Biomechanical Analysis Suggests Myosuit Reduces Knee Extensor Demand during Level and Incline Gait
Abstract
1. Introduction
2. Materials and Methods
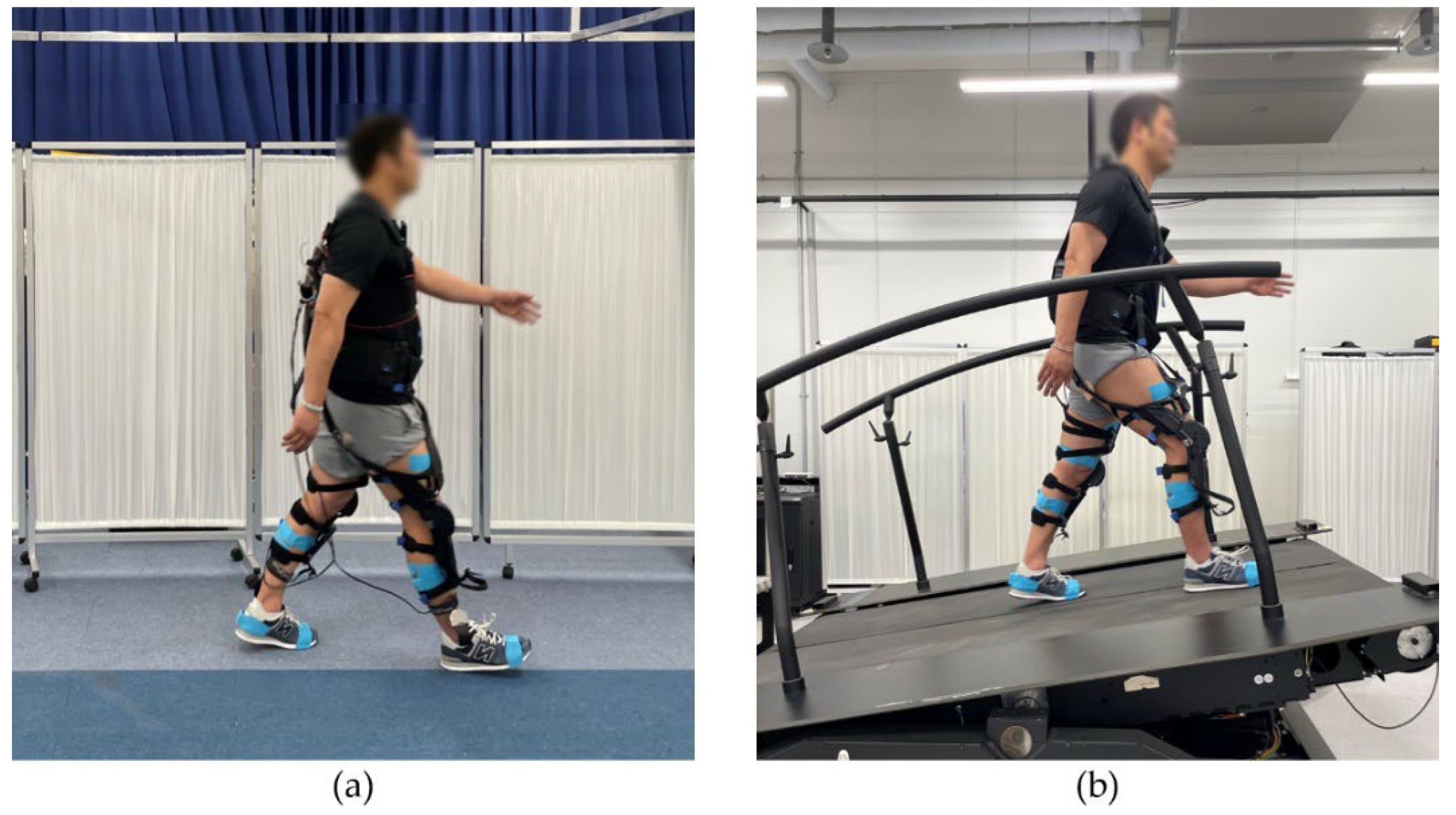
2.1. Experimental Setup
2.1.1. Myosuit
2.1.2. Level Overground Gait Sessions
2.1.3. Incline Treadmill Gait Sessions
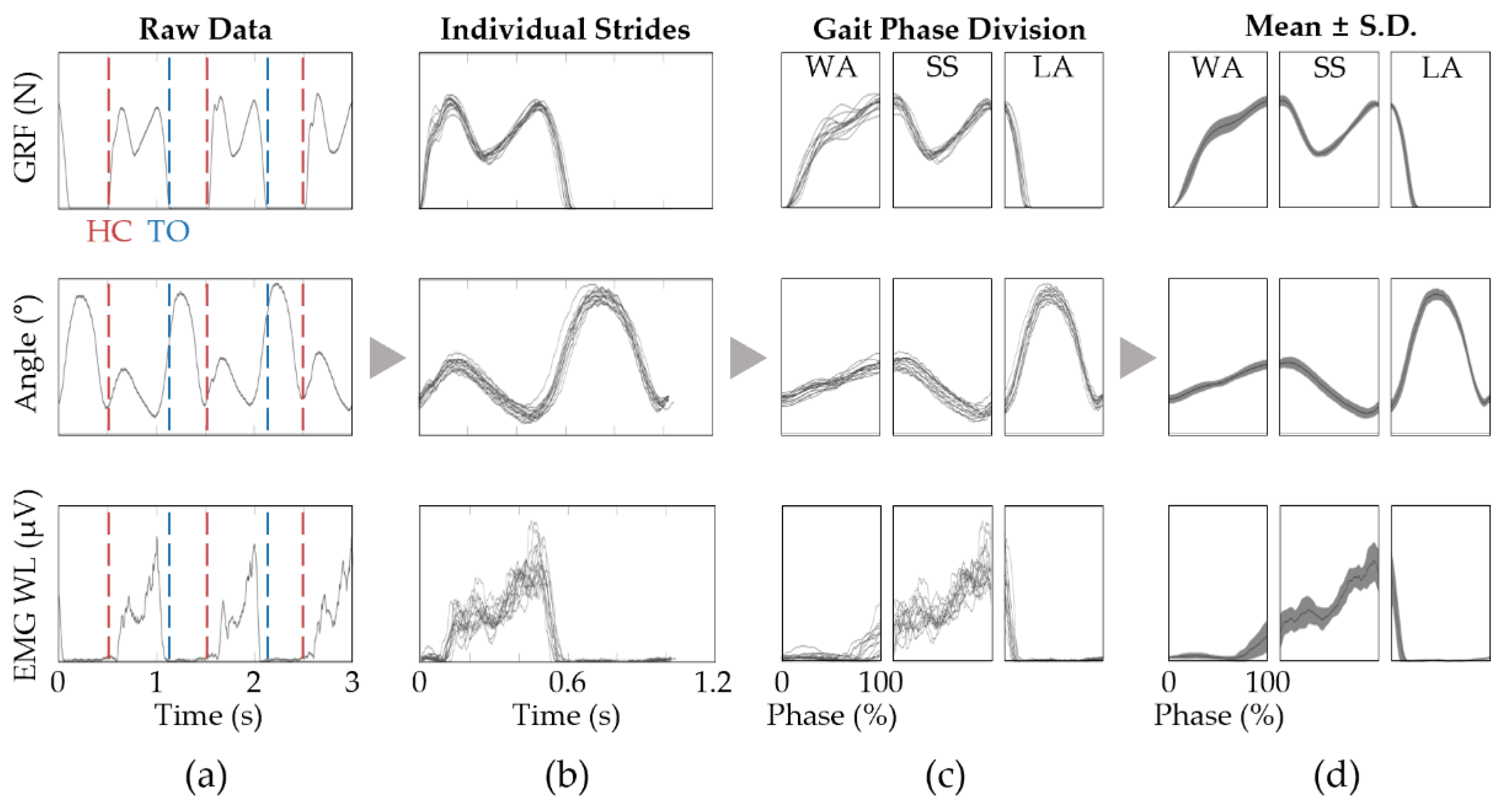
2.2. Signal Processing
2.2.1. EMG Pre-Processing
2.2.2. Joint Angle Estimation
2.2.3. Gait-Related Task Phase Segmentation
3. Results
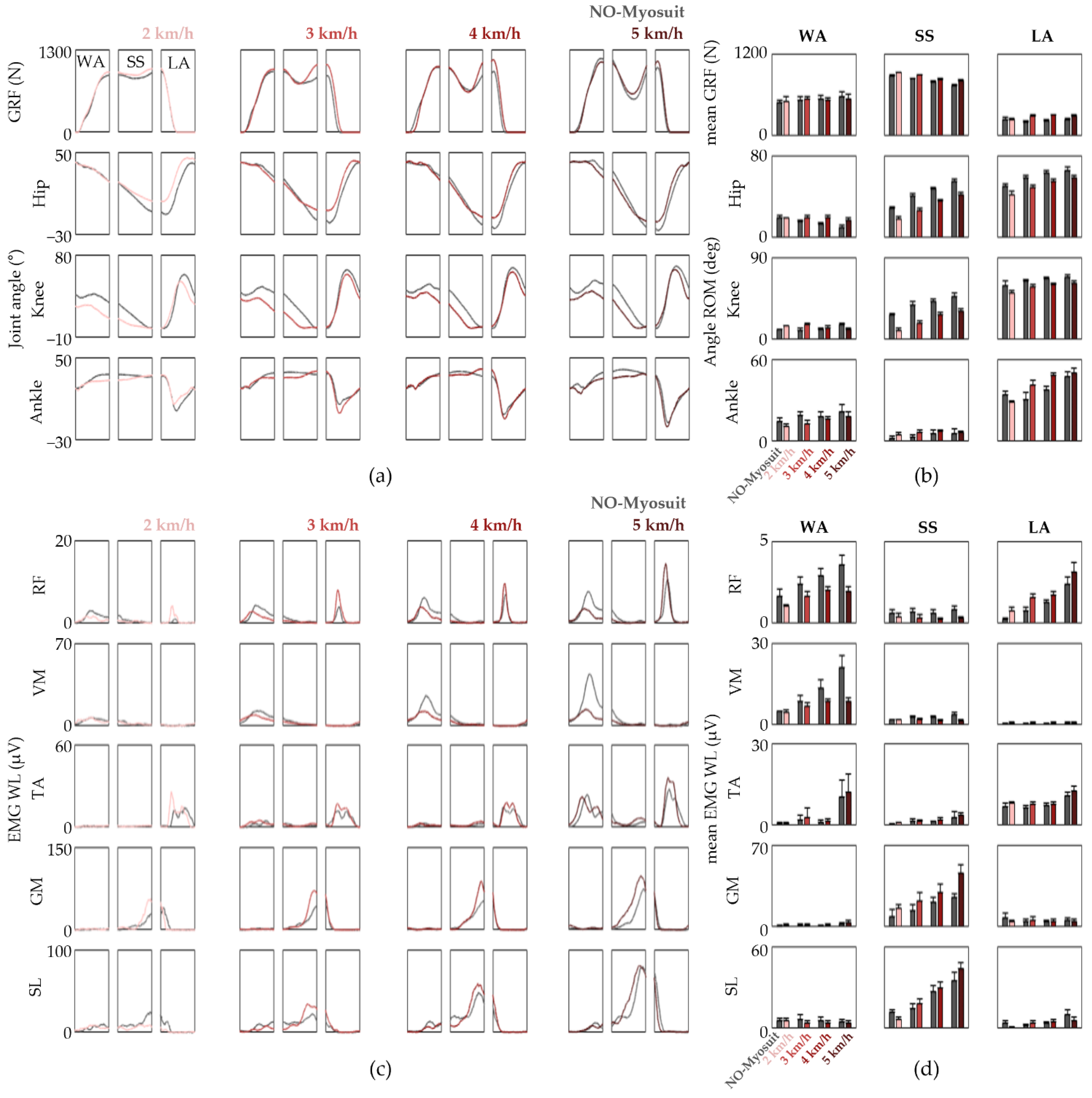
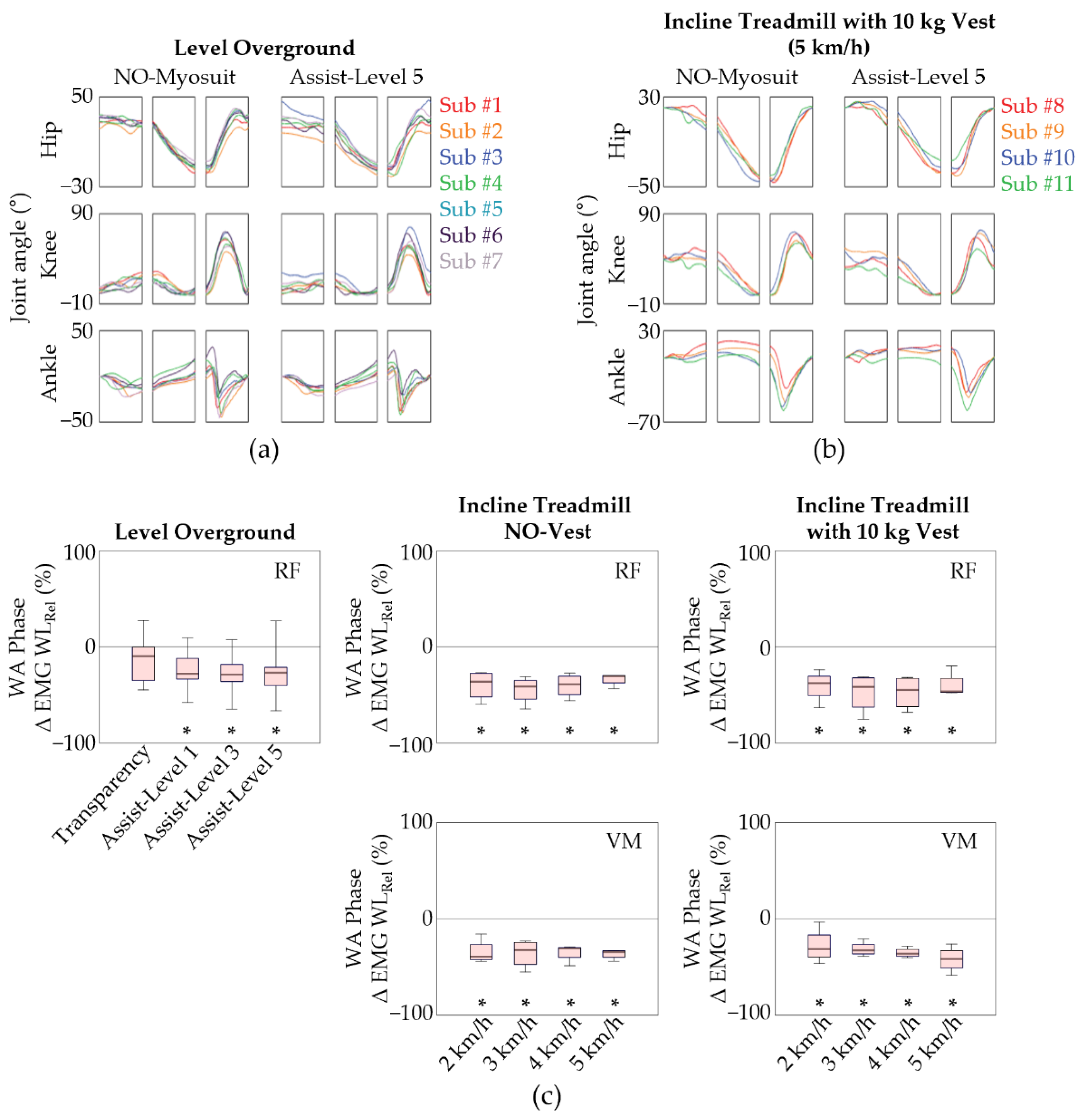
3.1. Level Overground Gait Sessions
3.2. Incline Treadmill Gait Sessions
3.3. Group Analysis
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 Guidelines on Physical Activity and Sedentary Behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide Trends in Insufficient Physical Activity from 2001 to 2016: A Pooled Analysis of 358 Population-Based Surveys with 1.9 Million Participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef]
- Colberg, S.R.; Sigal, R.J.; Yardley, J.E.; Riddell, M.C.; Dunstan, D.W.; Dempsey, P.C.; Horton, E.S.; Castorino, K.; Tate, D.F. Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care 2016, 39, 2065–2079. [Google Scholar] [CrossRef] [PubMed]
- Savela, S.; Koistinen, P.; Tilvis, R.S.; Strandberg, A.Y.; Pitkälä, K.H.; Salomaa, V.V.; Miettinen, T.A.; Strandberg, T.E. Leisure-Time Physical Activity, Cardiovascular Risk Factors and Mortality during a 34-Year Follow-Up in Men. Eur. J. Epidemiol. 2010, 25, 619–625. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Brown, J.C.; Winters-Stone, K.; Lee, A.; Schmitz, K.H. Cancer, Physical Activity, and Exercise. Compr. Physiol. 2012, 2, 2775–2809. [Google Scholar]
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T.; Alkandari, J.R.; Andersen, L.B.; Bauman, A.E.; Brownson, R.C.; et al. Effect of Physical Inactivity on Major Non-Communicable Diseases Worldwide: An Analysis of Burden of Disease and Life Expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef]
- Hollmann, W.; Strüder, H.K.; Tagarakis, C.V.; King, G. Physical activity and the elderly. Eur. J. Prev. Cardiol. 2007, 14, 730–739. [Google Scholar] [CrossRef]
- Dumith, S.C.; Hallal, P.C.; Reis, R.S.; Kohl, H.W. Worldwide Prevalence of Physical Inactivity and Its Association with Human Development Index in 76 Countries. Prev. Med. 2011, 53, 24–28. [Google Scholar] [CrossRef]
- Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report, 2008; US Department of Health and Human Services: Washington, DC, USA, 2008.
- Landi, F.; Marzetti, E.; Martone, A.M.; Bernabei, R.; Onder, G. Exercise as a Remedy for Sarcopenia. Curr. Opin. Clin. Nutr. Metab. Care 2014, 17, 25–31. [Google Scholar] [CrossRef]
- Steffl, M.; Bohannon, R.W.; Sontakova, L.; Tufano, J.J.; Shiells, K.; Holmerova, I. Relationship between Sarcopenia and Physical Activity in Older People: A Systematic Review and Meta-Analysis. Clin. Interv. Aging 2017, 12, 835–845. [Google Scholar] [CrossRef]
- Puetz, T.W. Physical activity and feelings of energy and fatigue. Sports Med. 2006, 36, 767–780. [Google Scholar] [CrossRef]
- Beaudart, C.; Dawson, A.; Shaw, S.C.; Harvey, N.C.; Kanis, J.A.; Binkley, N.; Reginster, J.Y.; Chapurlat, R.; Chan, D.C.; Bruyère, O.; et al. Nutrition and Physical Activity in the Prevention and Treatment of Sarcopenia: Systematic Review. Osteoporos. Int. 2017, 28, 1817–1833. [Google Scholar] [CrossRef]
- Xiong, H.; Diao, X. A Review of Cable-Driven Rehabilitation Devices. Disabil. Rehabil. Assist. Technol. 2020, 15, 885–897. [Google Scholar] [CrossRef]
- Fazekas, G.; Horvath, M.; Troznai, T.; Toth, A. Robot-Mediated Upper Limb Physiotherapy for Patients with Spastic Hemiparesis: A Preliminary Study. J. Rehabil. Med. 2007, 39, 580–582. [Google Scholar] [CrossRef]
- Prange, G.B.; Jannink, M.J.A.; Groothuis-Oudshoorn, C.G.M.; Hermens, H.J.; Ijzerman, M.J. Systematic Review of the Effect of Robot-Aided Therapy on Recovery of the Hemiparetic Arm after Stroke. J. Rehabil. Res. Dev. 2006, 43, 171–183. [Google Scholar] [CrossRef]
- Kwakkel, G.; Kollen, B.J.; Krebs, H.I. Effects of Robot-Assisted Therapy on Upper Limb Recovery after Stroke: A Systematic Review. Neurorehabilit. Neural Repair 2008, 22, 111–121. [Google Scholar] [CrossRef]
- Schmidt, K.; Duarte, J.E.; Grimmer, M.; Sancho-Puchades, A.; Wei, H.; Easthope, C.S.; Riener, R. The Myosuit: Bi-Articular Anti-Gravity Exosuit That Reduces Hip Extensor Activity in Sitting Transfers. Front. Neurorobot. 2017, 11, 57. [Google Scholar] [CrossRef]
- Haufe, F.L.; Kober, A.M.; Schmidt, K.; Sancho-Puchades, A.; Duarte, J.E.; Wolf, P.; Riener, R. User-driven walking assistance: First experimental results using the MyoSuit. In Proceedings of the 2019 IEEE 16th International Conference on Rehabilitation Robotics (ICORR), Toronto, ON, Canada, 24–28 June 2019. [Google Scholar]
- Haufe, F.L.; Schmidt, K.; Duarte, J.E.; Wolf, P.; Riener, R.; Xiloyannis, M. Activity-Based Training with the Myosuit: A Safety and Feasibility Study across Diverse Gait Disorders. J. NeuroEng. Rehabil. 2020, 17, 135. [Google Scholar] [CrossRef]
- Haufe, F.L.; Wolf, P.; Duarte, J.E.; Riener, R.; Xiloyannis, M. Increasing exercise intensity during outside walking training with a wearable robot. In Proceedings of the 2020 8th IEEE RAS/EMBS International Conference for Biomedical Robotics and Biomechatronics (BioRob), New York, NY, USA, 29 November–1 December 2020. [Google Scholar]
- Gui, K.; Liu, H.; Zhang, D. Toward Multimodal Human-Robot Interaction to Enhance Active Participation of Users in Gait Rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 2054–2066. [Google Scholar] [CrossRef]
- Edgerton, V.R.; Roy, R.R. Robotic Training and Spinal Cord Plasticity. Brain Res. Bull. 2009, 78, 4–12. [Google Scholar] [CrossRef][Green Version]
- Cao, J.; Xie, S.Q.; Das, R.; Zhu, G.L. Control Strategies for Effective Robot Assisted Gait Rehabilitation: The State of Art and Future Prospects. Med. Eng. Phys. 2014, 36, 1555–1566. [Google Scholar] [CrossRef]
- Carr, J.H.; Shepherd, R.B. A Motor Learning Model for Stroke Rehabilitation. Physiotherapy 1989, 75, 372–380. [Google Scholar] [CrossRef]
- Bowles, A.O.; Kevorkian, C.G.; Rintala, D.H. Gender differences regarding career issues and promotion in ac-ademic physical medicine and rehabilitation. Am. J. Phys. Med. Rehabil. 2007, 86, 918–925. [Google Scholar] [CrossRef]
- Perry, J. Gait Analysis: Normal and Pathological Function; SLACK Incorporated: Thorofare, NJ, USA, 1992; pp. 3–16. [Google Scholar]
- Kharb, A.; Saini, V.; Jain, Y.K.; Dhiman, S. A review of gait cycle and its parameters. Int. J. Comput. Eng. Manag. 2011, 13, 78–83. [Google Scholar]
- Vu, H.T.T.; Dong, D.; Cao, H.L.; Verstraten, T.; Lefeber, D.; Vanderborght, B.; Geeroms, J. A Review of Gait Phase Detection Algorithms for Lower Limb Prostheses. Sensors 2020, 20, 3972. [Google Scholar] [CrossRef] [PubMed]
- Gaffney, C.J.; Cunnington, J.; Rattley, K.; Wrench, E.; Dyche, C.; Bampouras, T.M. Weighted Vests in CrossFit Increase Physiological Stress during Walking and Running without Changes in Spatiotemporal Gait Parameters. Ergonomics 2022, 65, 147–158. [Google Scholar] [CrossRef]
- Englehart, K.; Hudgins, B. A Robust, Real-Time Control Scheme for Multifunction Myoelectric Control. IEEE Trans. Biomed. Eng. 2003, 50, 848–854. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Chung, S.H.; Choi, J.; Lee, J.M.; Kim, S.J. Practical Method for Predicting Intended Gait Speed via Soleus Surface EMG Signals. Electron. Lett. 2020, 56, 528–531. [Google Scholar] [CrossRef]
- Saito, A.; Kizawa, S.; Kobayashi, Y.; Miyawaki, K. Pose Estimation by Extended Kalman Filter Using Noise Covariance Matrices Based on Sensor Output. ROBOMECH J. 2020, 7, 36. [Google Scholar] [CrossRef]
- Lee, H.S.; Ryu, H.; Lee, S.U.; Cho, J.S.; You, S.; Park, J.H.; Jang, S.H. Analysis of Gait Characteristics Using Hip-Knee Cyclograms in Patients with Hemiplegic Stroke. Sensors 2021, 21, 7685. [Google Scholar] [CrossRef] [PubMed]
- Francis, C.A.; Lenz, A.L.; Lenhart, R.L.; Thelen, D.G. The Modulation of Forward Propulsion, Vertical Support, and Center of Pressure by the Plantarflexors during Human Walking. Gait Posture 2013, 38, 993–997. [Google Scholar] [CrossRef]
- Lim, M.R.; Huang, R.C.; Wu, A.; Girardi, F.P.; Cammisa, F.P., Jr. Evaluation of the elderly patient with an abnormal gait. J. Am. Acad. Orthop. Surg. 2007, 15, 107–117. [Google Scholar] [CrossRef]
- Swank, C.; Wang-Price, S.; Gao, F.; Almutairi, S. Walking with a Robotic Exoskeleton Does Not Mimic Natural Gait: A within-Subjects Study. JMIR Rehabil. Assist. Technol. 2019, 6, e11023. [Google Scholar] [CrossRef]
- Sylos-Labini, F.; la Scaleia, V.; d’Avella, A.; Pisotta, I.; Tamburella, F.; Scivoletto, G.; Molinari, M.; Wang, S.; Wang, L.; van Asseldonk, E.; et al. EMG Patterns during Assisted Walking in the Exoskeleton. Front. Hum. Neurosci. 2014, 8, 423. [Google Scholar] [CrossRef]
- Androwis, G.J.; Pilkar, R.; Ramanujam, A.; Nolan, K.J. Electromyography Assessment during Gait in a Robotic Exoskeleton for Acute Stroke. Front. Neurol. 2018, 9, 630. [Google Scholar] [CrossRef]
- Melton, L.J.; Khosla, S.; Crowson, C.S.; O’Connor, M.K.; O’Fallon, W.M.; Riggs, B.L. Epidemiology of Sarcopenia. J. Am. Geriatr. Soc. 2000, 48, 625–630. [Google Scholar] [CrossRef]
- Holloszy, J.O. The biology of aging. In Mayo Clinic Proceedings; Elsevier: Amsterdam, The Netherlands, 2000; pp. S3–S9. [Google Scholar]
- Tomás, M.T.; Galán-Mercant, A.; Carnero, E.A.; Fernandes, B. Functional Capacity and Levels of Physical Activity in Aging: A 3-Year Follow-Up. Front. Med. 2017, 4, 244. [Google Scholar] [CrossRef]
- Faude, O.; Donath, L. Editorial: Neuromuscular Performance during Lifespan: Assessment Methods and Exercise Interventions. Front. Physiol. 2019, 10, 1348. [Google Scholar] [CrossRef]
- Palmio, J.; Udd, B. Borderlines between Sarcopenia and Mild Late-Onset Muscle Disease. Front. Aging Neurosci. 2014, 6, 267. [Google Scholar] [CrossRef][Green Version]
- Timothy, J.D. Physiology of aging invited review: Aging and sarcopenia. J. Appl. Physiol. 2003, 95, 1717–1727. [Google Scholar]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.; Kim, Y.; Kang, S.; Kim, S.-J. Biomechanical Analysis Suggests Myosuit Reduces Knee Extensor Demand during Level and Incline Gait. Sensors 2022, 22, 6127. https://doi.org/10.3390/s22166127
Kim J, Kim Y, Kang S, Kim S-J. Biomechanical Analysis Suggests Myosuit Reduces Knee Extensor Demand during Level and Incline Gait. Sensors. 2022; 22(16):6127. https://doi.org/10.3390/s22166127
Chicago/Turabian StyleKim, Jaewook, Yekwang Kim, Seonghyun Kang, and Seung-Jong Kim. 2022. "Biomechanical Analysis Suggests Myosuit Reduces Knee Extensor Demand during Level and Incline Gait" Sensors 22, no. 16: 6127. https://doi.org/10.3390/s22166127
APA StyleKim, J., Kim, Y., Kang, S., & Kim, S.-J. (2022). Biomechanical Analysis Suggests Myosuit Reduces Knee Extensor Demand during Level and Incline Gait. Sensors, 22(16), 6127. https://doi.org/10.3390/s22166127





