Attempt to Make the Upper-Limb Item of Objective Fugl–Meyer Assessment Using 9-Axis Motion Sensors
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Design
2.2. Participants
2.3. Ethical Considerations
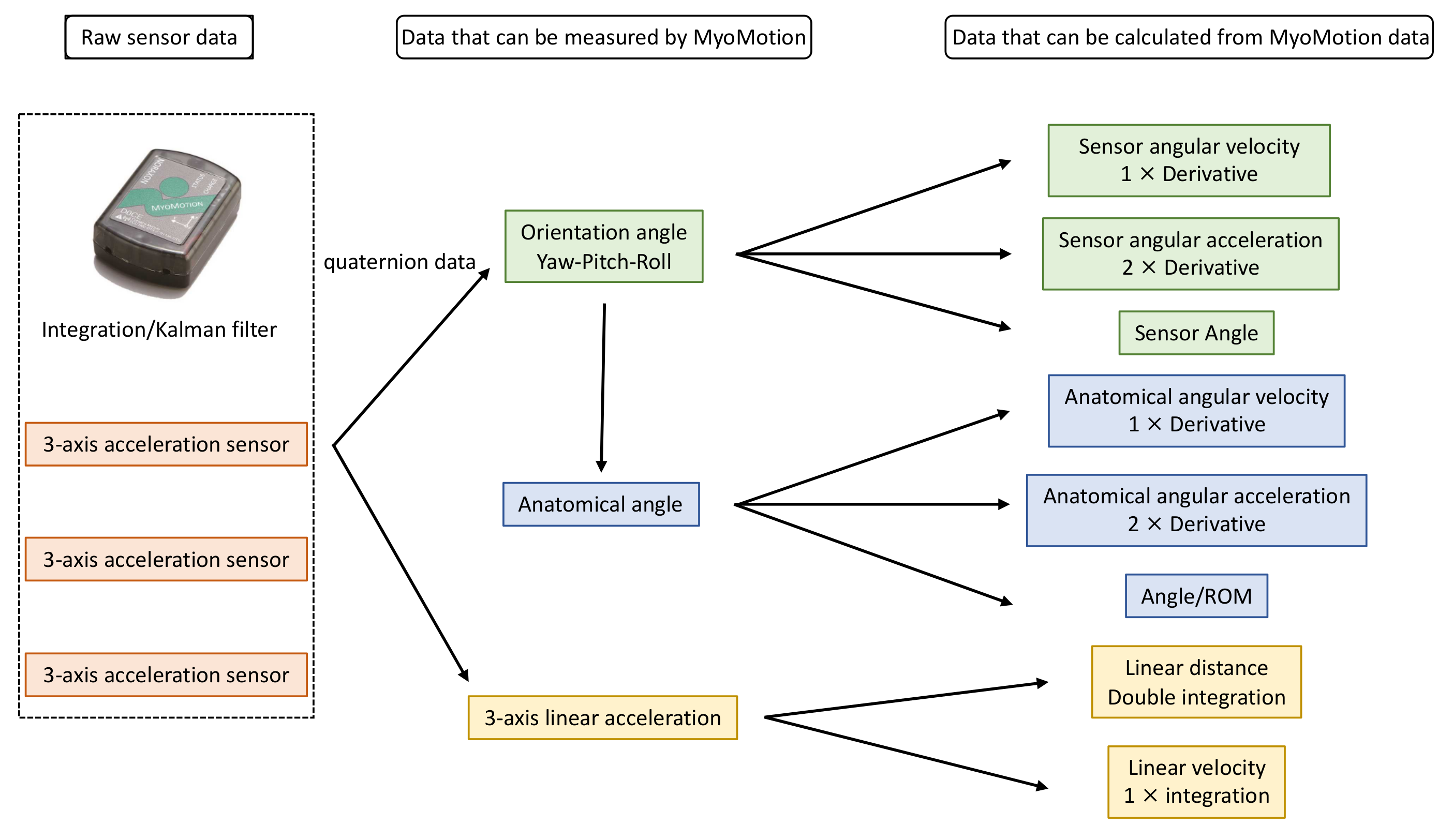
2.4. Measurement Equipment
2.5. Experimental Procedure
2.6. Extraction of Data
2.7. Analysis Method
3. Results
3.1. Participants
3.2. Analysis of Time Series Data of Movements
3.3. Correlation between Joint Angles of Each Part
3.4. Relationship between FMA (Continuous Variable) and Joint Angle
3.5. Construction of Discriminant Equation and Misjudgment Rate Using a Joint Angle of Final Limb Position
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Winstein, C.J.; Stein, J.; Arena, R.; Bates, B.; Cherney, L.R.; Cramer, S.C.; Deruyter, F.; Eng, J.J.; Fisher, B.; Harvey, R.L.; et al. Guidelines for Adult Stroke Rehabilitation and Recovery: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 2016, 47, e98–e169. [Google Scholar] [CrossRef] [PubMed]
- Fugl-Meyer, A.R.; Jääskö, L.; Leyman, I.; Olsson, S.; Steglind, S. The Post-Stroke Hemiplegic Patient. 1. A Method for Evaluation of Physical Performance. Scand. J. Rehabil. Med. 1975, 7, 13–31. [Google Scholar] [PubMed]
- Baker, K.; Cano, S.J.; Playford, E.D. Outcome Measurement in Stroke: A Scale Selection Strategy. Stroke 2011, 42, 1787–1794. [Google Scholar] [CrossRef] [PubMed]
- Platz, T.; Pinkowski, C.; van Wijck, F.; Johnson, G. Arm Rehabilitation Measurement: ARM; Manual for Performance and Scoring of the Fugl-Meyer Test (arm Section), Action Research Arm Test and the Box-and-Block Test; Deutscher Wissenschafts-Verlag (DWV): Kapperlrodeck, Germany, 2005; pp. 1–144. [Google Scholar]
- Duncan, P.W.; Propst, M.; Nelson, S.G. Reliability of the Fugl-Meyer Assessment of Sensorimotor Recovery Following Cerebrovascular Accident. Phys. Ther. 1983, 63, 1606–1610. [Google Scholar] [CrossRef]
- Wood-Dauphinee, S.L.; Williams, J.I.; Shapiro, S.H. Examining Outcome Measures in a Clinical Study of Stroke. Stroke 1990, 21, 731–739. [Google Scholar] [CrossRef]
- Sanford, J.; Moreland, J.; Swanson, L.R.; Stratford, P.W.; Gowland, C. Reliability of the Fugl-Meyer Assessment for Testing Motor Performance in Patients Following Stroke. Phys. Ther. 1993, 73, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Malouin, F.; Pichard, L.; Bonneau, C.; Durand, A.; Corriveau, D. Evaluating Motor Recovery Early After Stroke: Comparison of the Fugl-Meyer Assessment and the Motor Assessment Scale. Arch. Phys. Med. Rehabil. 1994, 75, 1206–1212. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.H.; Hsueh, I.P.; Sheu, C.F.; Hsieh, C.L. Psychometric Properties of the Sensory Scale of the Fugl-Meyer Assessment in Stroke Patients. Clin. Rehabil. 2004, 18, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Shelton, F.N.; Reding, M.J. Effect of Lesion Location on Upper Limb Motor Recovery after Stroke. Stroke 2001, 32, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Gladstone, D.J.; Danells, C.J.; Black, S.E. The Fugl-Meyer Assessment of Motor Recovery after Stroke: A Critical Review of Its Measurement Properties. Neurorehabil. Neural Repair 2002, 16, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Santisteban, L.; Térémetz, M.; Bleton, J.P.; Baron, J.C.; Maier, M.A.; Lindberg, P.G. Upper Limb Outcome Measures Used in Stroke Rehabilitation Studies: A Systematic Literature Review. PLoS ONE 2016, 11, e0154792. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, K.J.; Tilson, J.K.; Cen, S.Y.; Rose, D.K.; Hershberg, J.; Correa, A.; Gallichio, J.; McLeod, M.; Moore, C.; Wu, S.S.; et al. Fugl-Meyer Assessment on Sensorimotor Function after Stroke: Standardized Training Procedure for Clinical Practice and Clinical Trials. Stroke 2011, 42, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Del Din, S.; Patel, S.; Cobelli, C.; Bonato, P. Estimating Fugl-Meyer Clinical Scores in Stroke Survivors Using Wearable Sensors. In Proceedings of the 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Boston, MA, USA, 30 August–3 September 2011; pp. 5839–5842. [Google Scholar]
- Yu, L.; Xiong, D.; Guo, L.; Wang, J. A Remote Quantitative Fugl-Meyer Assessment Framework for Stroke Patients Based on Wearable Sensor Networks. Comput. Methods Programs Biomed. 2016, 128, 100–110. [Google Scholar] [CrossRef] [PubMed]
- Otten, P.; Kim, J.; Son, S.H. A Framework to Automate Assessment of Upper-Limb Motor Function Impairment: A Feasibility Study. Sensors 2015, 15, 20097–20114. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.S.; Cho, S.; Baek, D.; Bang, H.; Pain, N.J. Upper Extremity Functional Evaluation by Fugl-Meyer Assessment Scoring Using Depth-Sensing Camera in Hemiplegic Stroke Patients. PLoS ONE 2016, 11, e0158640. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Lee, Y.S.; Kim, J. Automated Evaluation of Upper-Limb Motor Function Impairment Using Fugl-Meyer Assessment. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Formstone, L.; Pucek, M.; Wilson, S.; Bentley, P.; McGregor, A.; Vaidyanathan, R. Myographic Information Enables Hand Function Classification in Automated Fugl-Meyer Assessment. In Proceedings of the 9th International IEEE EMBS Conference on Neural Engineering, San Francisco, CA, USA, 20–23 March 2019; pp. 239–242. [Google Scholar]
- Ryan, L.K.; Carr, C.E.; Meyen, F.; Domingues, A.R.; Dava, P.; Newman, J.; Jacobs, S.E. Using Inertial Measurement Units for Measuring Spacesuit Mobility and Work Envelope Capability for Intravehicular and Extravehicular Activities. In Proceedings of the 63rd International Astronautical Congress, Space Life Sciences Symposium, Life Support and EVA Systems Session, Naples, Italy, 1–5 October 2012; pp. 1–9. [Google Scholar]
- Balasubramanian, S.; Abbas, J. Comparison of Angle Measurements between Vicon and MyoMotion Systems; Arizona State University: Tempe, AZ, USA, 2013. [Google Scholar]
- Bonnechère, B.; Jansen, B.; Salvia, P.; Bouzahouene, H.; Omelina, L.; Moiseev, F.; Sholukha, V.; Cornelis, J.; Rooze, M.; Van Sint Jan, S. Validity and Reliability of the Kinect within Functional Assessment Activities: Comparison with Standard Stereophotogrammetry. Gait Posture 2014, 39, 593–598. [Google Scholar] [CrossRef] [PubMed]
- Nagata, S. Fugl-Meyer Assessment. Jpn. J. Occup. Ther. 2004, 38, 579–586. [Google Scholar]
- Yoon, T.L. Validity and Reliability of an Inertial Measurement Unit-Based 3D Angular Measurement of Shoulder Joint Motion. J. Korean Phys. Ther. 2017, 29, 145–151. [Google Scholar] [CrossRef]
- Yoon, T.L.; Kim, H.N.; Min, J.H. Validity and Reliability of an Inertial Measurement Unit–based 3-Dimensional Angular Measurement of Cervical Range of Motion. J. Manip. Physiol. Ther. 2019, 42, 75–81. [Google Scholar] [CrossRef] [PubMed]






| Target Test Symbol | |||
|---|---|---|---|---|
| Flexors | Data | N/A | |
| Extensors | Data | N/A | ||
| Flexor synergy | Shoulder | Retraction | T1 |
| Elevation | T2 | |||
| Abduction (90°) | T3 | |||
| External rotation | T4 | |||
| Elbow | Flexion | T5 | ||
| Forearm | Supination | T6 | ||
| Extensor synergy | Shoulder | Adduction/internal Rotation | T7 | |
| Elbow | Extension | T8 | ||
| Forearm | Pronation | T9 | ||
| Hand to lumbar spine | T10 | ||
| Shoulder flexion 0–90° | T11 | |||
| Pronation/supination of the forearm, with the elbow flexed to 90° | T12 | |||
| Shoulder abduction 0–90° | T13 | ||
| Shoulder flexion 90–180° | T14 | |||
| Pronation/supination of the forearm, with the elbow fully extended | T15 | |||
| Biceps, triceps, finger flexors | N/A | ||
| Wrist stability at 15° dorsiflexion with the elbow flexed at 90° | T16 | ||
| Repeated wrist flexion and extension with the elbow flexed to 90° | T17 | |||
| Wrist stability at 15° dorsiflexion with the elbow at 0° | T18 | |||
| Repeated wrist flexion and extension with the elbow at 0° | T19 | |||
| Circumduction of the wrist | T20 | |||
| Mass flexion | N/A | ||
| Mass extension | N/A | |||
| Grasp A: extension of the MCP, flexion of the PIP and DIP | N/A | |||
| Grasp B: extended index finger and thumb | N/A | |||
| Grasp C: pulp of the thumb against the pulp of the index finger | N/A | |||
| Grasp D: volar surface on the thumb and index finger against each other | N/A | |||
| Grasp E: spherical grasp | N/A | |||
| Tremor | T21 | ||
| Dysmetria | T22 | |||
| Time | T23 | |||
| Articular Point | Joint Angle |
|---|---|
| Neck | Flexion/extension |
| Lateral flexion (right/left) | |
| Rotation (right/left) | |
| Chest | Flexion/extension |
| Lateral flexion (right/left) | |
| Rotation (right/left) | |
| Waist | Flexion/extension |
| Lateral flexion (right/left) | |
| Rotation (right/left) | |
| Shoulder | Flexion/extension |
| Abduction/adduction | |
| External rotation/internal rotation | |
| Total flexion | |
| Elbow | Flexion/extension |
| Forearm | Pronation/supination |
| Hand | Palmar flexion/dorsiflexion |
| Radial flexion/ulnar flexion |
| Characteristic | Patients, N = 30 | Healthy Participants, N = 15 |
|---|---|---|
| Age | 67.5 (58.75–72.5) | 29 (24.5–44.5) |
| Female sex (%) | 30 | 60 |
| Left-handed (%) | 0 | 6.7 |
| Days since stroke | 64 (33.5–109.25) | - |
| Diagnosis of hemorrhage (%) | 33.3 | - |
| Somatosensory deficits presented (%) | 57 | - |
| Brunnstrom recovery stage *, proximal | 4 (3–5) | - |
| Brunnstrom recovery stage *, distal | 5 (3–5) | - |
| FMA Test | Dependent Variable | Coefficient | p-Value | R | R2 |
|---|---|---|---|---|---|
| Flexor synergy | (Intercept) | 2.037 | 0.233 | 0.907 | 0.823 |
| Elbow flexion/extension | 0.062 | <0.001 | |||
| Shoulder flexion/extension | 0.021 | 0.011 | |||
| Shoulder external/internal rotation | 0.052 | 0.001 | |||
| Extensor synergy | (Intercept) | 4.024 | <0.001 | 0.857 | 0.734 |
| Elbow flexion/extension | −0.079 | <0.001 | |||
| Neck rotation | −0.027 | 0.001 | |||
| shoulder total flexion | 0.157 | <0.001 | |||
| shoulder flexion/extension | −0.077 | 0.001 | |||
| shoulder abduction/adduction | 0.044 | 0.014 | |||
| Coordination/Speed | (Intercept) | 1.848 | 0.021 | 0.838 | 0.721 |
| Elbow flexion/extension | −0.036 | <0.001 | |||
| Shoulder total flexion | 0.05 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ueyama, Y.; Takebayashi, T.; Takeuchi, K.; Yamazaki, M.; Hanada, K.; Okita, Y.; Shimada, S. Attempt to Make the Upper-Limb Item of Objective Fugl–Meyer Assessment Using 9-Axis Motion Sensors. Sensors 2023, 23, 5213. https://doi.org/10.3390/s23115213
Ueyama Y, Takebayashi T, Takeuchi K, Yamazaki M, Hanada K, Okita Y, Shimada S. Attempt to Make the Upper-Limb Item of Objective Fugl–Meyer Assessment Using 9-Axis Motion Sensors. Sensors. 2023; 23(11):5213. https://doi.org/10.3390/s23115213
Chicago/Turabian StyleUeyama, Yusuke, Takashi Takebayashi, Kenta Takeuchi, Makoto Yamazaki, Keisuke Hanada, Yuho Okita, and Shinichi Shimada. 2023. "Attempt to Make the Upper-Limb Item of Objective Fugl–Meyer Assessment Using 9-Axis Motion Sensors" Sensors 23, no. 11: 5213. https://doi.org/10.3390/s23115213
APA StyleUeyama, Y., Takebayashi, T., Takeuchi, K., Yamazaki, M., Hanada, K., Okita, Y., & Shimada, S. (2023). Attempt to Make the Upper-Limb Item of Objective Fugl–Meyer Assessment Using 9-Axis Motion Sensors. Sensors, 23(11), 5213. https://doi.org/10.3390/s23115213






