Colorectal Cancer Diagnosis through Breath Test Using a Portable Breath Analyzer—Preliminary Data
Abstract
1. Introduction
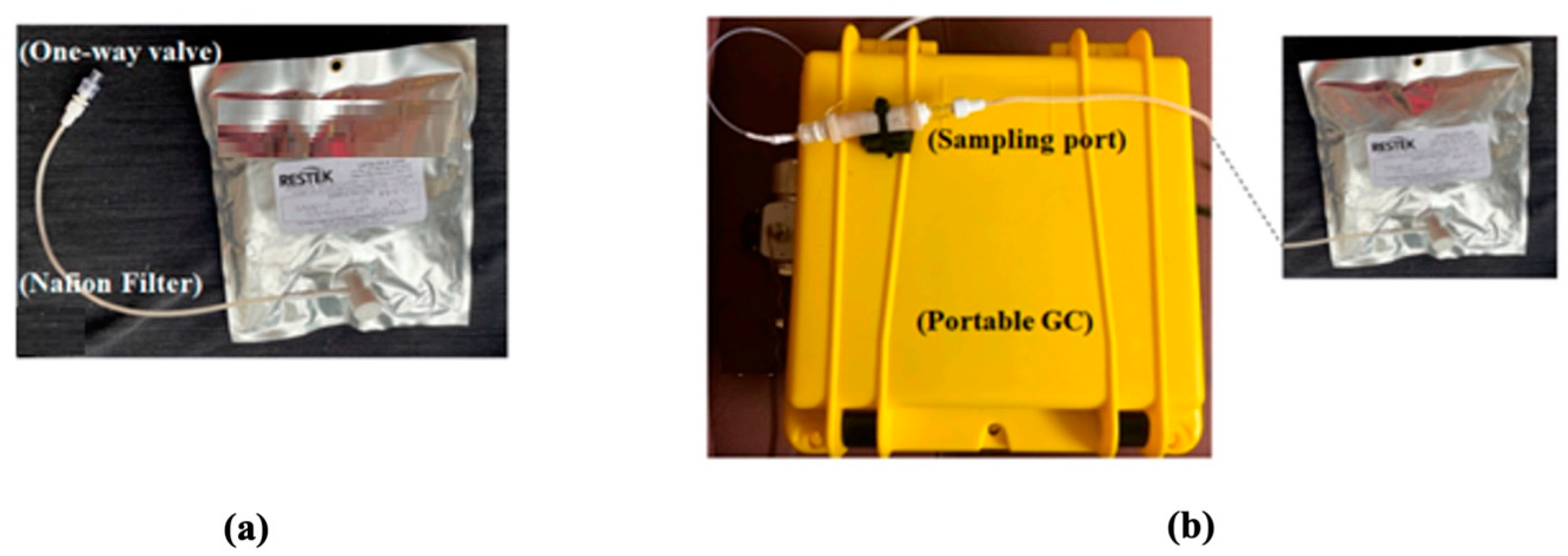
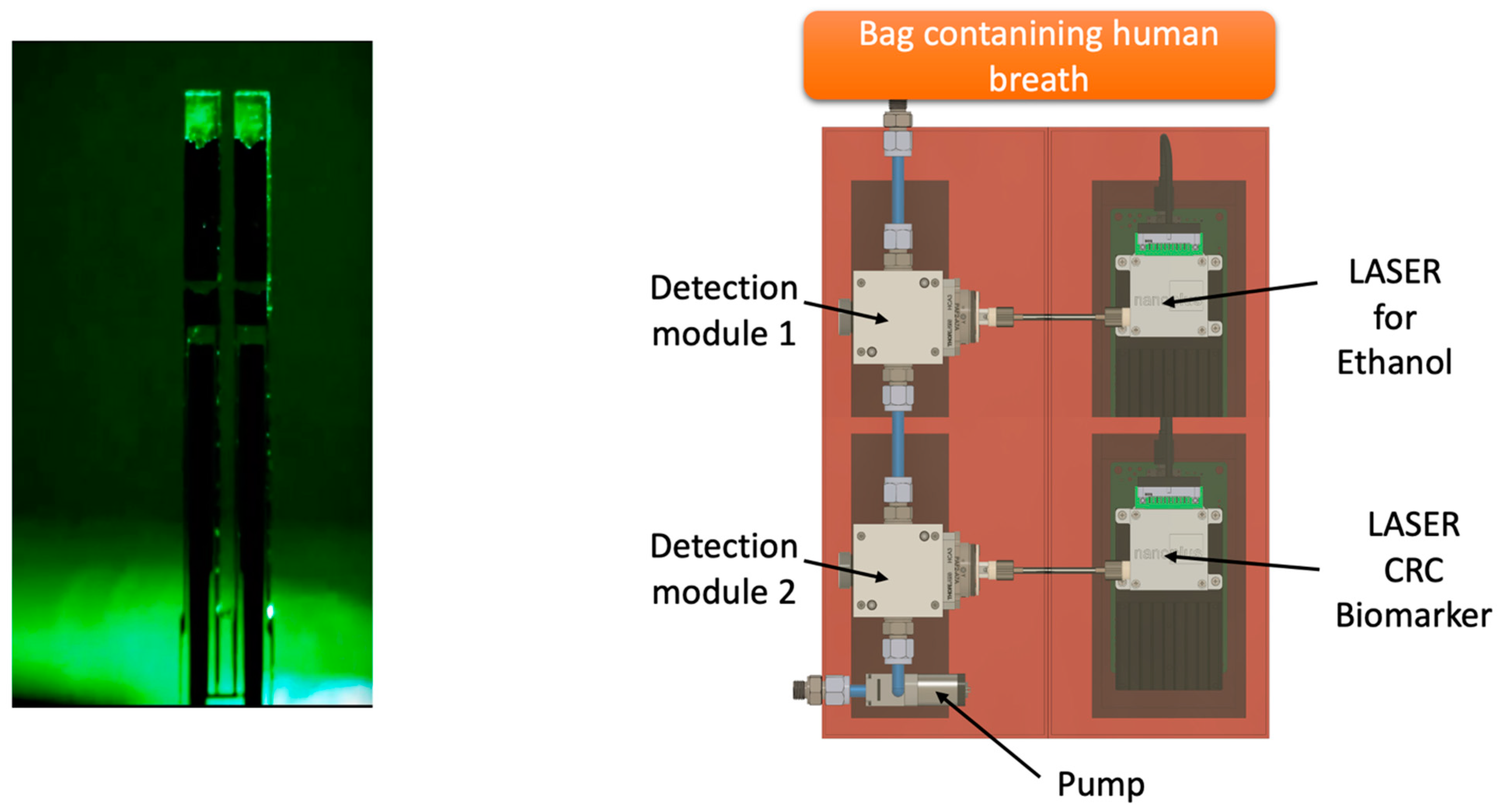
2. Methods
3. Breath Analysis
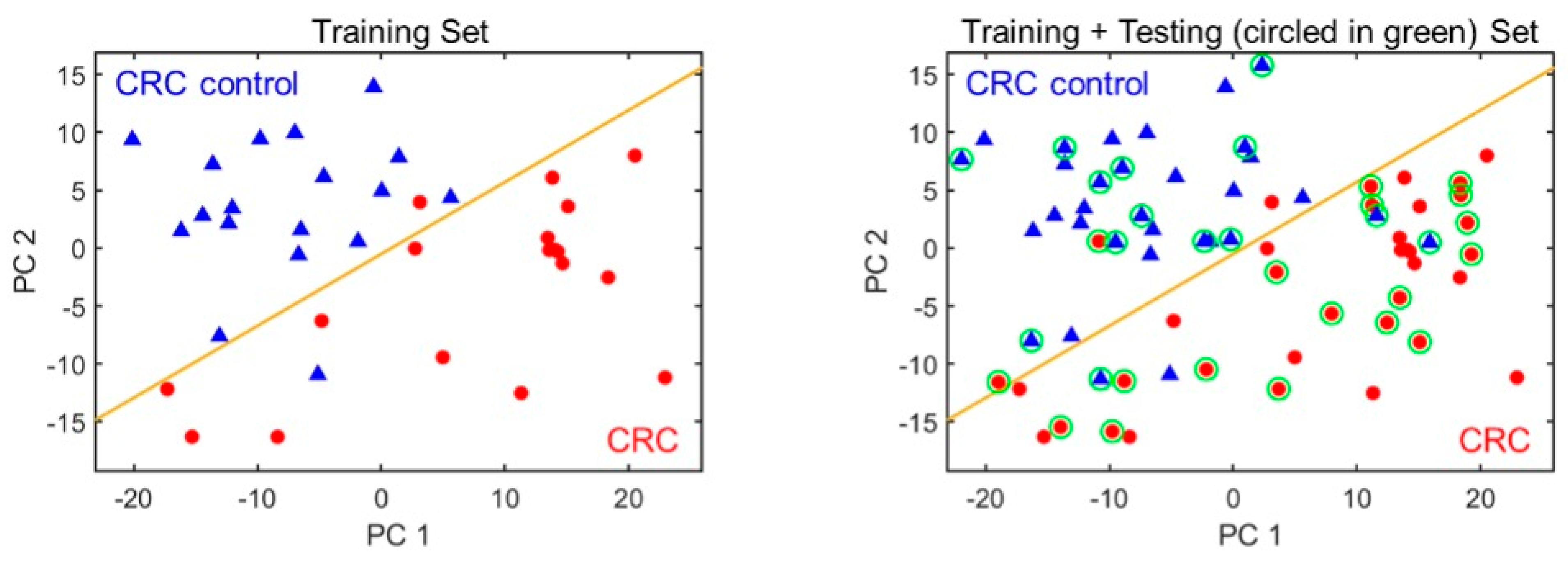
4. Statistical Analysis
5. Results
6. Discussion
- Selection of Carbopack X and B.
- Maximum working temperature of SSTI (250 °C).
- Short column length.
- Low maximum column operating temperature (120 °C).
- Some compounds with ionization potential higher than 10.6 eV cannot be detected.
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arnold, M.; Sierra, M.S.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global patterns and trends in colorectal cancer incidence and mortality. Gut 2017, 66, 683–691. [Google Scholar] [CrossRef] [PubMed]
- Jideh, B.; Bourke, M.J. Colorectal cancer screening reduces incidence, mortality and morbidity. Med. J. Aust. 2018, 208, 483–484. [Google Scholar] [CrossRef] [PubMed]
- Kanth, P.; Inadomi, J.M. Screening and prevention of colorectal cancer. BMJ 2021, 374, n1855. [Google Scholar] [CrossRef] [PubMed]
- Li, J.N.; Yuan, S.Y. Fecal occult blood test in colorectal cancer screening. J. Dig. Dis. 2019, 20, 62–64. [Google Scholar] [CrossRef] [PubMed]
- Lauby-Secretan, B.; Vilahur, N.; Bianchini, F.; Guha, N.; Straif, K.; International Agency for Research on Cancer Handbook Working Group. The IARC Perspective on Colorectal Cancer Screening. N. Engl. J. Med. 2018, 378, 1734–1740. [Google Scholar] [CrossRef] [PubMed]
- Deng, X.; Nakamura, Y. Cancer Precision Medicine: From Cancer Screening to Drug Selection and Personalized Immunotherapy. Trends Pharmacol. Sci. 2017, 38, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.; Zang, W.; Tabartehfarahani, A.; Lam, A.; Huang, X.; Sivakumar, A.D.; Thota, C.; Yang, S.; Dickson, R.P.; Sjoding, M.W.; et al. Portable Breath-Based Volatile Organic Compound Monitoring for the Detection of COVID-19 During the Circulation of the SARS-CoV-2 Delta Variant and the Transition to the SARS-CoV-2 Omicron Variant. JAMA Netw. Open 2023, 6, e230982. [Google Scholar] [CrossRef] [PubMed]
- Shekhawat, J.K.; Banerjee, M. Role of Breath Biopsy in COVID-19. J. Appl. Lab. Med. 2022, 7, 1175–1188. [Google Scholar] [CrossRef]
- Boots, A.W.; Bos, L.D.; van der Schee, M.P.; van Schooten, F.J.; Sterk, P.J. Exhaled Molecular Fingerprinting in Diagnosis and Monitoring: Validating Volatile Promises. Trends Mol. Med. 2015, 21, 633–644. [Google Scholar] [CrossRef]
- Bond, A.; Greenwood, R.; Lewis, S.; Corfe, B.; Sarkar, S.; O’Toole, P.; Rooney, P.; Burkitt, M.; Hold, G.; Probert, C. Volatile organic compounds emitted from faeces as a biomarker for colorectal cancer. Aliment. Pharmacol. Ther. 2019, 49, 1005–1012. [Google Scholar] [CrossRef]
- McFarlane, M.; Millard, A.; Hall, H.; Savage, R.; Constantinidou, C.; Arasaradnam, R.; Nwokolo, C. Urinary volatile organic compounds and faecal microbiome profiles in colorectal cancer. Color. Dis. 2019, 21, 1259–1269. [Google Scholar] [CrossRef] [PubMed]
- Altomare, D.F.; Di Lena, M.; Porcelli, F.; Trizio, L.; Travaglio, E.; Tutino, M.; Dragonieri, S.; Memeo, V.; de Gennaro, G. Exhaled volatile organic compounds identify patients with colorectal cancer. Br. J. Surg. 2013, 100, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Wen, Q.; Boshier, P.; Myridakis, A.; Belluomo, I.; Hanna, G.B. Urinary Volatile Organic Compound Analysis for the Diagnosis of Cancer: A Systematic Literature Review and Quality Assessment. Metabolites 2020, 11, 17. [Google Scholar] [CrossRef] [PubMed]
- Kneepkens, C.M.; Lepage, G.; Roy, C.C. The potential of the hydrocarbon breath test as a measure of lipid peroxidation. Free Radic. Biol. Med. 1994, 17, 127–160. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, P.; Loeseken, C.; Schubert, J.K.; Miekisch, W. Breath gas aldehydes as biomarkers of lung cancer. Int. J. Cancer 2010, 126, 2663–2670. [Google Scholar] [CrossRef] [PubMed]
- Phillips, M.; Cataneo, R.N.; Saunders, C.; Hope, P.; Schmitt, P.; Wai, J. Volatile biomarkers in the breath of women with breast cancer. J. Breath Res. 2010, 4, 026003. [Google Scholar] [CrossRef] [PubMed]
- Abaffy, T.; Duncan, R.; Riemer, D.D.; Tietje, O.; Elgart, G.; Milikowski, C.; DeFazio, R.A. Differential volatile signatures from skin, naevi and melanoma: A novel approach to detect a pathological process. PLoS ONE 2010, 5, e13813. [Google Scholar] [CrossRef]
- Tsou, P.H.; Lin, Z.L.; Pan, Y.C.; Yang, H.C.; Chang, C.J.; Liang, S.K.; Wen, Y.F.; Chang, C.H.; Chang, L.Y.; Yu, K.L.; et al. Exploring Volatile Organic Compounds in Breath for High-Accuracy Prediction of Lung Cancer. Cancers 2021, 13, 1431. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Tian, Y.; Luo, Z.; Qian, C.; Li, W.; Duan, Y. Breath volatile organic compound analysis: An emerging method for gastric cancer detection. J. Breath Res. 2021, 15, 044002. [Google Scholar] [CrossRef]
- Altomare, D.F.; Picciariello, A.; Rotelli, M.T.; De Fazio, M.; Aresta, A.; Zambonin, C.G.; Vincenti, L.; Trerotoli, P.; De Vietro, N. Chemical signature of colorectal cancer: Case-control study for profiling the breath print. BJS Open 2020, 4, 1189–1199. [Google Scholar] [CrossRef]
- Zhou, M.; Sharma, R.; Zhu, H.; Li, Z.; Li, J.; Wang, S.; Bisco, E.; Massey, J.; Pennington, A.; Sjoding, M.; et al. Rapid breath analysis for acute respiratory distress syndrome diagnostics using a portable two-dimensional gas chromatography device. Anal. Bioanal. Chem. 2019, 411, 6435–6447. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.; Zang, W.; Zhou, M.; Schafer, N.; Begley, L.A.; Huang, Y.J.; Fan, X. Real Time Breath Analysis Using Portable Gas Chromatography for Adult Asthma Phenotypes. Metabolites 2021, 11, 265. [Google Scholar] [CrossRef] [PubMed]
- Gillies, C.E.; Jennaro, T.S.; Puskarich, M.A.; Sharma, R.; Ward, K.R.; Fan, X.; Jones, A.E.; Stringer, K.A. A Multilevel Bayesian Approach to Improve Effect Size Estimation in Regression Modeling of Metabolomics Data Utilizing Imputation with Uncertainty. Metabolites 2020, 10, 319. [Google Scholar] [CrossRef] [PubMed]
- Blanchet, L.; Smolinska, A.; Baranska, A.; Tigchelaar, E.; Swertz, M.; Zhernakova, A.; Dallinga, J.W.; Wijmenga, C.; van Schooten, F.J. Factors that influence the volatile organic compound content in human breath. J. Breath Res. 2017, 11, 016013. [Google Scholar] [CrossRef] [PubMed]
- Allegretti, M.; Cottone, G.; Carboni, F.; Cotroneo, E.; Casini, B.; Giordani, E.; Amoreo, C.A.; Buglioni, S.; Diodoro, M.; Pescarmona, E.; et al. Cross-sectional analysis of circulating tumor DNA in primary colorectal cancer at surgery and during post-surgery follow-up by liquid biopsy. J. Exp. Clin. Cancer Res. 2020, 39, 69. [Google Scholar] [CrossRef] [PubMed]
- Loktionov, A. Biomarkers for detecting colorectal cancer non-invasively: DNA, RNA or proteins? World J. Gastrointest. Oncol. 2020, 12, 124–148. [Google Scholar] [CrossRef] [PubMed]
- Pardini, B.; Ferrero, G.; Tarallo, S.; Gallo, G.; Francavilla, A.; Licheri, N.; Trompetto, M.; Clerico, G.; Senore, C.; Peyre, S.; et al. A Fecal MicroRNA Signature by Small RNA Sequencing Accurately Distinguishes Colorectal Cancers: Results from a Multicenter Study. Gastroenterology 2023, 165, 582–599e8. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Xu, L.; Wang, M.; An, G.; Feng, G. The accuracy of circulating microRNA-21 in the diagnosis of colorectal cancer: A systematic review and meta-analysis. Color. Dis. 2015, 17, O100–O107. [Google Scholar] [CrossRef]
- Chung, J.; Akter, S.; Han, S.; Shin, Y.; Choi, T.G.; Kang, I.; Kim, S.S. Diagnosis by Volatile Organic Compounds in Exhaled Breath in Exhaled Breath from Patients with Gastric and Colorectal Cancers. Int. J. Mol. Sci. 2022, 24, 129. [Google Scholar] [CrossRef]
- Amal, H.; Leja, M.; Funka, K.; Lasina, I.; Skapars, R.; Sivins, A.; Ancans, G.; Kikuste, I.; Vanags, A.; Tolmanis, I.; et al. Breath testing as potential colorectal cancer screening tool. Int. J. Cancer 2016, 138, 229–236. [Google Scholar] [CrossRef]
- Markar, S.R.; Chin, S.T.; Romano, A.; Wiggins, T.; Antonowicz, S.; Paraskeva, P.; Ziprin, P.; Darzi, A.; Hanna, G.B. Breath Volatile Organic Compound Profiling of Colorectal Cancer Using Selected Ion Flow-tube Mass Spectrometry. Ann. Surg. 2019, 269, 903–910. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Ke, C.; Wang, X.; Chi, C.; Guo, L.; Luo, S.; Guo, Z.; Xu, G.; Zhang, F.; Li, E. Noninvasive detection of colorectal cancer by analysis of exhaled breath. Anal. Bioanal. Chem. 2014, 406, 4757–4763. [Google Scholar] [CrossRef]
- van Keulen, K.E.; Jansen, M.E.; Schrauwen, R.W.M.; Kolkman, J.J.; Siersema, P.D. Volatile organic compounds in breath can serve as a non-invasive diagnostic biomarker for the detection of advanced adenomas and colorectal cancer. Aliment. Pharmacol. Ther. 2020, 51, 334–346. [Google Scholar] [CrossRef] [PubMed]
- Wilson, A.D. Application of Electronic-Nose Technologies and VOC-Biomarkers for the Noninvasive Early Diagnosis of Gastrointestinal Diseases (dagger). Sensors 2018, 18, 2613. [Google Scholar] [CrossRef] [PubMed]
- Steenhuis, E.G.M.; Schoenaker, I.J.H.; de Groot, J.W.B.; Fiebrich, H.B.; de Graaf, J.C.; Brohet, R.M.; van Dijk, J.D.; van Westreenen, H.L.; Siersema, P.D.; de Vos Tot Nederveen Cappel, W.H. Feasibility of volatile organic compound in breath analysis in the follow-up of colorectal cancer: A pilot study. Eur. J. Surg. Oncol. 2020, 46, 2068–2073. [Google Scholar] [CrossRef] [PubMed]
- De Vietro, N.; Aresta, A.; Rotelli, M.T.; Zambonin, C.; Lippolis, C.; Picciariello, A.; Altomare, D.F. Relationship between cancer tissue derived and exhaled volatile organic compound from colorectal cancer patients. Preliminary results. J. Pharm. Biomed. Anal. 2020, 180, 113055. [Google Scholar] [CrossRef] [PubMed]
- Altomare, D.F.; Di Lena, M.; Porcelli, F.; Travaglio, E.; Longobardi, F.; Tutino, M.; Depalma, N.; Tedesco, G.; Sardaro, A.; Memeo, R.; et al. Effects of Curative Colorectal Cancer Surgery on Exhaled Volatile Organic Compounds and Potential Implications in Clinical Follow-up. Ann. Surg. 2015, 262, 862–866, discussion 866–867. [Google Scholar] [CrossRef] [PubMed]
- Fisher, D.A.; Princic, N.; Miller-Wilson, L.A.; Wilson, K.; DeYoung, K.; Ozbay, A.B.; Limburg, P. Adherence to fecal immunochemical test screening among adults at average risk for colorectal cancer. Int. J. Color. Dis. 2022, 37, 719–721. [Google Scholar] [CrossRef] [PubMed]
- Elefante, A.; Menduni, G.; Rossmadl, H.; Mackowiak, V.; Giglio, M.; Sampaolo, A.; Patimisco, P.; Passaro, V.M.N.; Spagnolo, V. Environmental Monitoring of Methane with Quartz-Enhanced Photoacoustic Spectroscopy Exploiting an Electronic Hygrometer to Compensate the H2O Influence on the Sensor Signal. Sensors 2020, 20, 2935. [Google Scholar] [CrossRef]
- Patimisco, P.; Sampaolo, A.; Dong, L.; Tittel, F.K.; Spagnolo, V. Recent advances in quartz enhanced photoacoustic sensing. Appl. Phys. Rev. 2018, 5, 011106. [Google Scholar] [CrossRef]
- Patimisco, P.; Scamarcio, G.; Tittel, F.K.; Spagnolo, V. Quartz-enhanced photoacoustic spectroscopy: A review. Sensors 2014, 14, 6165–6206. [Google Scholar] [CrossRef] [PubMed]
- Viscaino, M.; Bustos, J.T.; Munoz, P.; Cheein, C.A.; Cheein, F.A. Artificial intelligence for the early detection of colorectal cancer: A comprehensive review of its advantages and misconceptions. World J. Gastroenterol. 2021, 27, 6399–6414. [Google Scholar] [CrossRef] [PubMed]
- Gallos, I.K.; Tryfonopoulos, D.; Shani, G.; Amditis, A.; Haick, H.; Dionysiou, D.D. Advancing Colorectal Cancer Diagnosis with AI-Powered Breathomics: Navigating Challenges and Future Directions. Diagnostics 2023, 13, 3673. [Google Scholar] [CrossRef] [PubMed]
- Mitsala, A.; Tsalikidis, C.; Pitiakoudis, M.; Simopoulos, C.; Tsaroucha, A.K. Artificial Intelligence in Colorectal Cancer Screening, Diagnosis and Treatment. A New Era. Curr. Oncol. 2021, 28, 1581–1607. [Google Scholar] [CrossRef] [PubMed]

| CRC Group | HC Group | p | ||
|---|---|---|---|---|
| n | 36 | 32 | ||
| Gender | Male | 26 (72.20%) | 19 (59.40%) | 0.74 |
| Female | 10 (27.80%) | 13 (40.60%) | ||
| Age | 67 (64–77.25) | 65 (54–68.75) | 0.07 | |
| BMI * | 27.50 (25.15–30.12) | 25 (23.42–27.90) | 0.03 | |
| Comorbidities | Cardiovascular | 27 (75%) | 11 (34.30%) | <0.01 |
| Pulmonary | 6 (16%) | 0 | 0.06 | |
| Diabetes | 7 (19.40%) | 4 (12.50%) | 0.40 | |
| Drugs | Antihypertensive | 26 (72.20%) | 9 (28.10%) | <0.01 |
| Antidiabetic | 5 (13.80%) | 4 (12.50%) | 0.80 | |
| Weight Loss | yes | 3 (8.30%) | 1 (3.10%) | 0.36 |
| no | 33(91.60%) | 31 (96.80%) | ||
| Family history of CRC | yes | 3 (8.30%) | 2 (6.20%) | 0.74 |
| no | 33(91.60%) | 30 (93.70%) |
| Pathological T | T1 | 0 |
| T2 | 4 (11.10%) | |
| T3 | 27 (75%) | |
| T4 | 5 (13.80%) | |
| Pathological N | N0 | 26 (72.20%) |
| N1 | 7 (19.40%) | |
| N2 | 3 (8.30%) | |
| Tumor location | Right | 8 (22.20%) |
| Transverse | 2 (5.50%) | |
| Left | 2 (5.50%) | |
| Sigmoid | 16 (44.40%) | |
| Rectum | 8 (22.20%) | |
| CEA | ng/mL | 2.8 (6.20–1.70) |
| CA 19.9 | U/mL | 9.6 (22.20–6.90) |
| Retention Time TR (s) | Library Compound | Retention Time TR (s) | Library Compound | Retention Time TR (s) | Library Compound |
|---|---|---|---|---|---|
| 9 | 1,4-Dioxane-2,6-dione | 260 | 1-Octene | 470 | Hexane, 2,2,5,5- tetramethyl- |
| 38 | Butane, 2-methyl- | 266 | Tetrachloroethylene | 482 | Heptane, 2,3,6-trimethyl- |
| 42 | Isoprene | 267 | 4-Octene, (Z)- | 502 | a-Pinene |
| 47 | 4-Penten-1-ol | 271 | 4-Octene, (E)- | 504 | Cyclohexene, 4-methylene- 1-(1-methylethyl)- |
| 53 | Pentane, 2-methyl- | 276 | Octane | 527 | 4-Octene, 2,6-dimethyl-, [S-(E)]- |
| 62 | 1-Pentene, 2-methyl- | 283 | Heptane, 3,3-dimethyl- | 533 | 2-Undecanethiol, 2-methyl- |
| 65 | n-Hexane | 288 | 2-Heptene, 3-methyl- | 558 | Octane, 4-ethyl- |
| 72 | 1-Pentanol, 2-methyl- | 295 | 2-Octene | 565 | 5-Ethyldecane |
| 115 | Hexane, 3-methyl- | 304 | Hexane, 2,3,5-trimethyl- | 601 | Decyl octyl ether |
| 137 | Heptane | 316 | Heptane, 2,4-dimethyl- | 609 | Decane, 2,6,7-trimethyl- |
| 154 | Cyclohexane, methyl- | 327 | Octane, 2-methyl- | 616 | Decane, 2,4,6-trimethyl- |
| 158 | 1-Pentanol, 2-ethyl-4- methyl- | 341 | Heptane, 2,5-dimethyl- | 624 | Dodecane, 1-fluoro- |
| 175 | Pentane, 2,2,3-trimethyl- | 362 | Hexane, 2,3,4-trimethyl- | 630 | Decane, 2,2-dimethyl- |
| 197 | 2,4-dimethylhexane | 372 | 4,6-Octadiyn-3-one, 2- methyl- | 665 | 2,2,7,7-Tetramethyloctane |
| 209 | Pentane, 2,3,4-trimethyl- | 376 | Heptane, 2,3-dimethyl- | 656 | Decane, 2,6,8-trimethyl- |
| 214 | Pentane, 2,3,3-trimethyl- | 387 | Octane, 4-methyl- | 675 | Decane, 2,5,9-trimethyl- |
| 221 | Hexane, 2,3-dimethyl- | 394 | Cyclopentane, 2-ethyl-1,1- dimethyl- | 696 | Heptane, 5-ethyl-2,2,3- trimethyl- |
| 230 | Hexane, 2,3-dimethyl- | 412 | Heptane, 2,2,4-trimethyl- | 717 | Decane, 2,6,7-trimethyl- |
| 239 | Heptane, 2,5-dimethyl- | 422 | Octane, 2,2-dimethyl- | 735 | Undecane, 3,6-dimethyl- |
| 249 | Hexane, 2,2,4-trimethyl- | 441 | Octane, 3,3-dimethyl- | 768 | Dodecane, 2,7,10- trimethyl- |
| 255 | Hexane, 2,2,5-trimethyl- |
| Training Set | Testing Set | Training + Testing Set | |||||||
|---|---|---|---|---|---|---|---|---|---|
| CRC | Non-CRC | Total | CRC | Non-CRC | Total | CRC | Non-CRC | Total | |
| Subject number | 18 | 18 | 36 | 18 | 14 | 32 | 36 | 32 | 68 |
| Positive | 17 | 1 | 18 | 17 | 3 | 20 | 34 | 4 | 38 |
| Negative | 1 | 17 | 18 | 1 | 11 | 12 | 2 | 28 | 30 |
| Specificity | 94.4% | 78.6% | 87.5% | ||||||
| Sensitivity | 94.4% | 94.5% | 94.4% | ||||||
| Positive predictive value | 94.4% | 85.0% | 89.5% | ||||||
| Negative predictive value | 94.4% | 91.7% | 93.3% | ||||||
| Total accuracy | 94.4% | 87.5% | 91.2% | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Picciariello, A.; Dezi, A.; Vincenti, L.; Spampinato, M.G.; Zang, W.; Riahi, P.; Scott, J.; Sharma, R.; Fan, X.; Altomare, D.F. Colorectal Cancer Diagnosis through Breath Test Using a Portable Breath Analyzer—Preliminary Data. Sensors 2024, 24, 2343. https://doi.org/10.3390/s24072343
Picciariello A, Dezi A, Vincenti L, Spampinato MG, Zang W, Riahi P, Scott J, Sharma R, Fan X, Altomare DF. Colorectal Cancer Diagnosis through Breath Test Using a Portable Breath Analyzer—Preliminary Data. Sensors. 2024; 24(7):2343. https://doi.org/10.3390/s24072343
Chicago/Turabian StylePicciariello, Arcangelo, Agnese Dezi, Leonardo Vincenti, Marcello Giuseppe Spampinato, Wenzhe Zang, Pamela Riahi, Jared Scott, Ruchi Sharma, Xudong Fan, and Donato F. Altomare. 2024. "Colorectal Cancer Diagnosis through Breath Test Using a Portable Breath Analyzer—Preliminary Data" Sensors 24, no. 7: 2343. https://doi.org/10.3390/s24072343
APA StylePicciariello, A., Dezi, A., Vincenti, L., Spampinato, M. G., Zang, W., Riahi, P., Scott, J., Sharma, R., Fan, X., & Altomare, D. F. (2024). Colorectal Cancer Diagnosis through Breath Test Using a Portable Breath Analyzer—Preliminary Data. Sensors, 24(7), 2343. https://doi.org/10.3390/s24072343





