Schinus terebinthifolius Leaf Lectin (SteLL) Reduces the Bacterial and Inflammatory Burden of Wounds Infected by Staphylococcus aureus Promoting Skin Repair
Abstract
:1. Introduction
2. Results
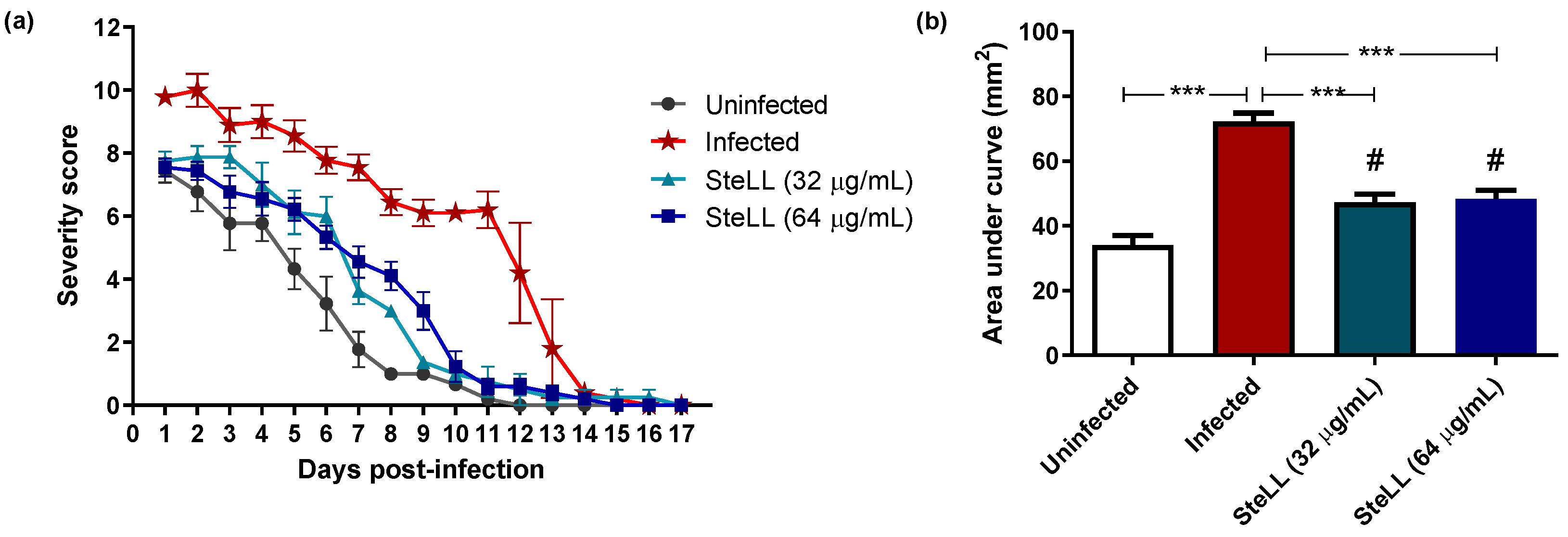
2.1. Topical Treatment with SteLL Reduced the Severity of S. aureus-Infected Skin Wounds
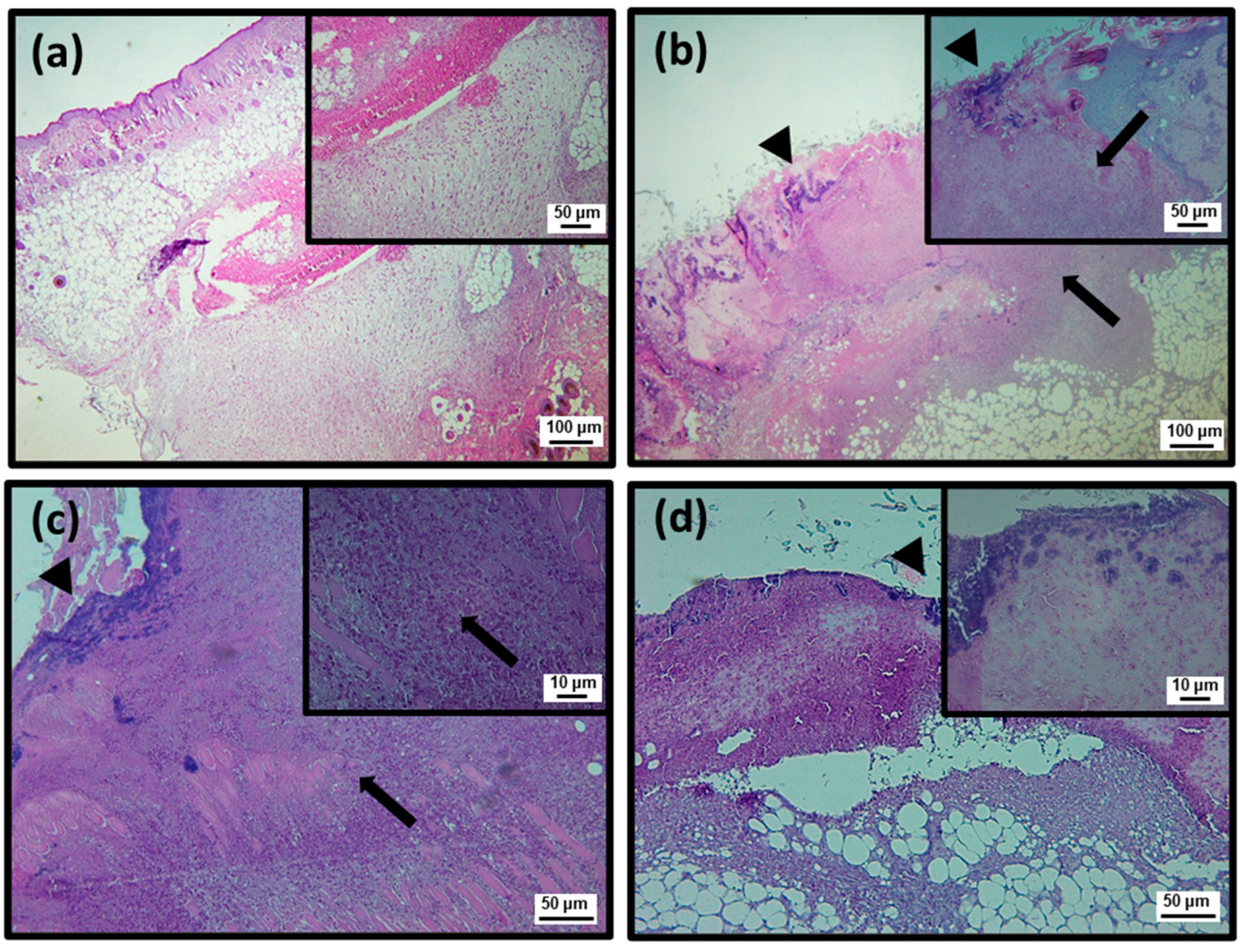
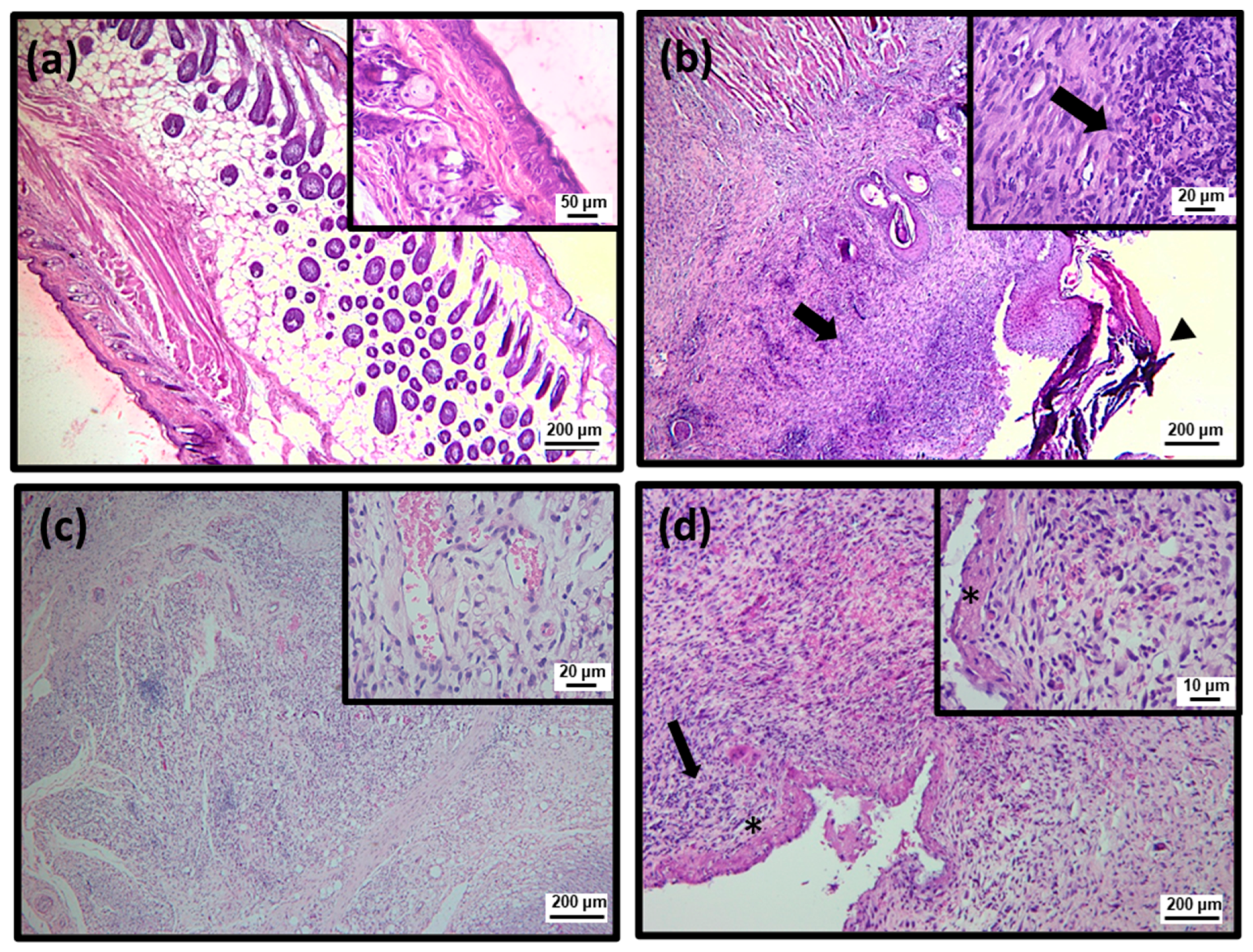
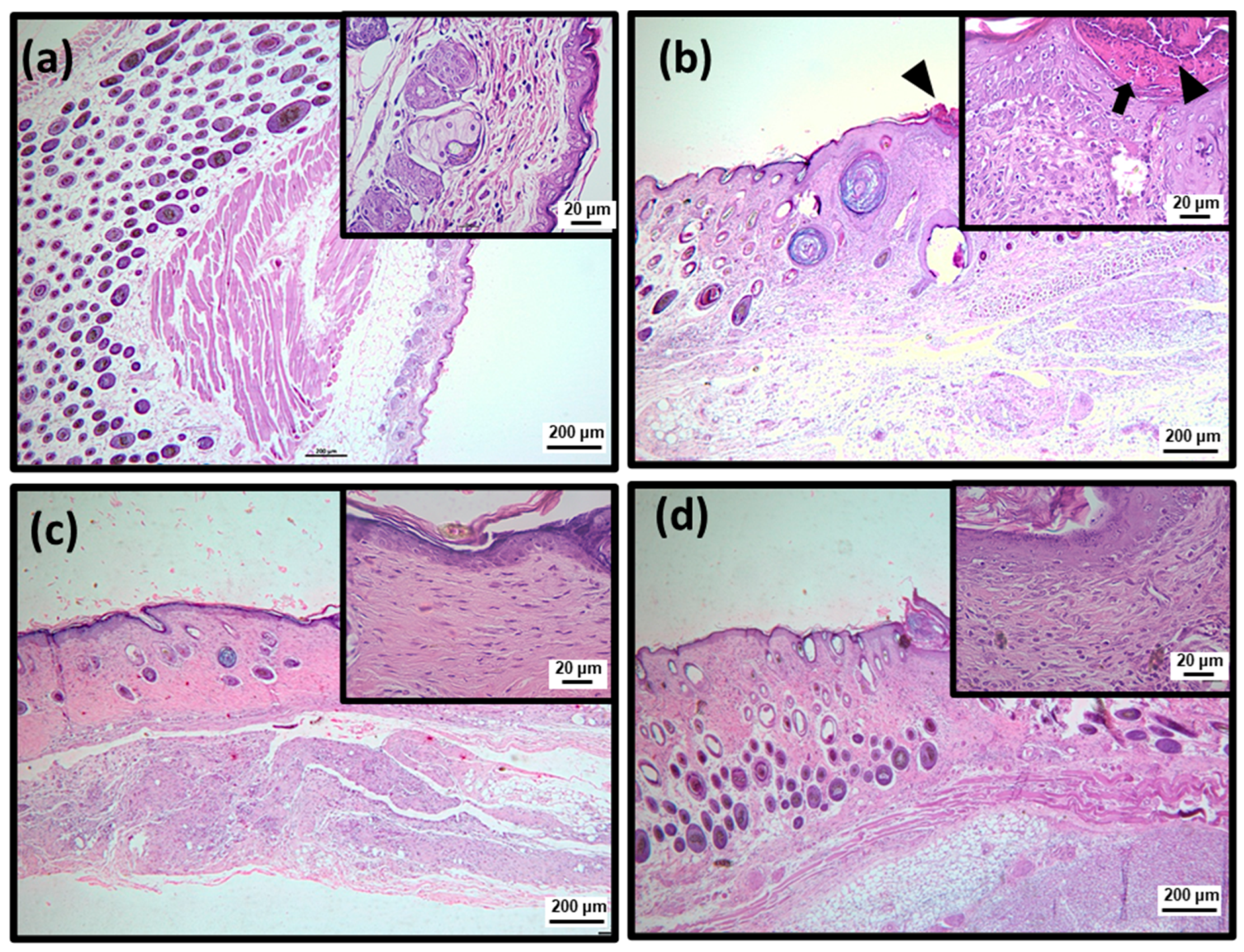
2.2. Topical Treatment with SteLL Accelerated the Contraction of S. aureus-Infected Skin Wounds
2.3. Topical Treatment with SteLL Reduced the Bacterial Load of Skin Lesions Infected by S. aureus
2.4. Topical Treatment with SteLL Modulated the Levels of Inflammatory Markers at Skin Lesions Infected by S. aureus
3. Discussion
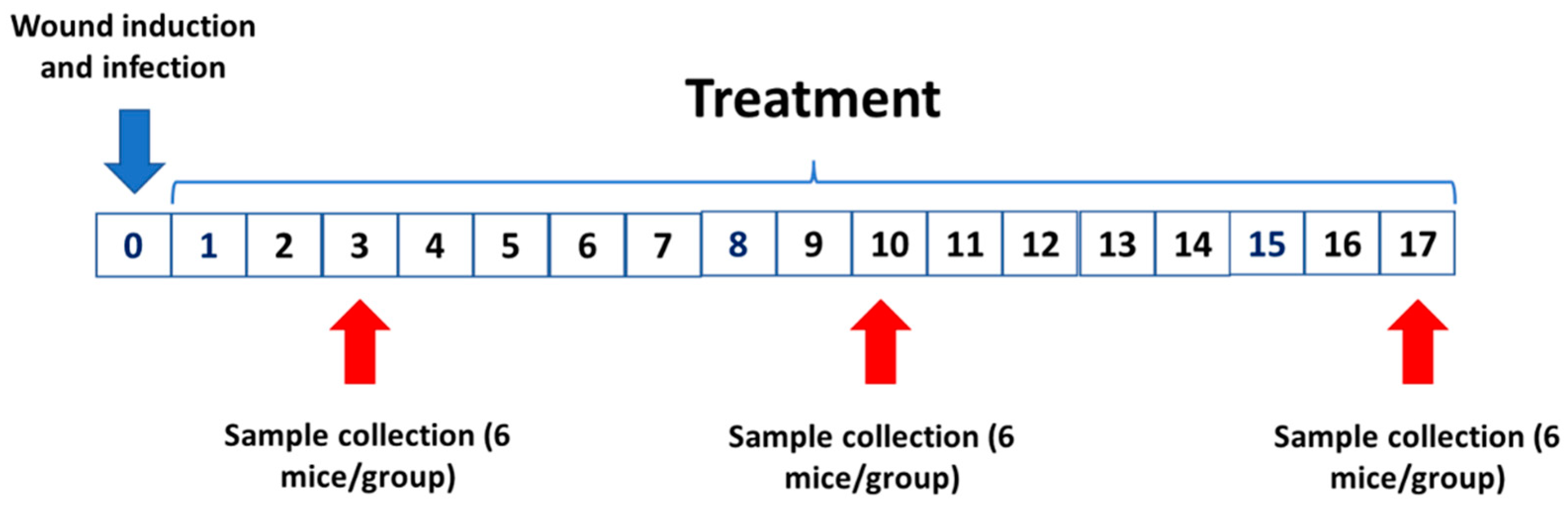
4. Materials and Methods
4.1. SteLL Purification
4.2. Animals and Ethical Conditions
4.3. Induction of Experimental Skin Injuries and Treatment
4.4. Analysis of Macroscopic Aspects
4.5. Histological Evaluation
4.6. Bacterial Quantification
4.7. Quantification of Inflammatory Markers
4.8. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lindholm, C.; Searle, R. Wound Management for the 21st Century: Combining Effectiveness and Efficiency. Int. Wound J. 2016, 13, 5–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beyene, R.T.; Derryberry, S.L.; Barbul, A. The Effect of Comorbidities on Wound Healing. Surg. Clin. N. Am. 2020, 100, 695–705. [Google Scholar] [CrossRef] [PubMed]
- Chopra, H.; Kumar, S.; Singh, I. Strategies and Therapies for Wound Healing: A Review. Curr. Drug Targets 2022, 23, 87–98. [Google Scholar] [CrossRef] [PubMed]
- Kaplani, K.; Koutsi, S.; Armenis, V.; Skondra, F.G.; Karantzelis, N.; Champeris Tsaniras, S.; Taraviras, S. Wound Healing Related Agents: Ongoing Research and Perspectives. Adv. Drug Deliv. Rev. 2018, 129, 242–253. [Google Scholar] [CrossRef] [PubMed]
- Lux, C.N. Wound Healing in Animals: A Review of Physiology and Clinical Evaluation. Vet. Dermatol. 2022, 33, 91-e27. [Google Scholar] [CrossRef]
- Rodrigues, M.; Kosaric, N.; Bonham, C.A.; Gurtner, G.C. Wound Healing: A Cellular Perspective. Physiol. Rev. 2019, 99, 665–706. [Google Scholar] [CrossRef]
- Han, G.; Ceilley, R. Chronic Wound Healing: A Review of Current Management and Treatments. Adv. Ther. 2017, 34, 599–610. [Google Scholar] [CrossRef] [Green Version]
- Darby, I.A.; Laverdet, B.; Bonté, F.; Desmoulière, A. Fibroblasts and Myofibroblasts in Wound Healing. Clin. Cosmet. Investig. Dermatol. 2014, 7, 301–311. [Google Scholar] [CrossRef] [Green Version]
- Kovtun, A.; Messerer, D.A.C.; Scharffetter-Kochanek, K.; Huber-Lang, M.; Ignatius, A. Neutrophils in Tissue Trauma of the Skin, Bone, and Lung: Two Sides of the Same Coin. J. Immunol. Res. 2018, 2018, 8173983. [Google Scholar] [CrossRef]
- Adib, Y.; Bensussan, A.; Michel, L. Cutaneous Wound Healing: A Review about Innate Immune Response and Current Therapeutic Applications. Mediat. Inflamm. 2022, 2022, 5344085. [Google Scholar] [CrossRef]
- Williams, H.; Campbell, L.; Crompton, R.A.; Singh, G.; McHugh, B.J.; Davidson, D.J.; McBain, A.J.; Cruickshank, S.M.; Hardman, M.J. Microbial Host Interactions and Impaired Wound Healing in Mice and Humans: Defining a Role for BD14 and NOD2. J. Investig. Dermatol. 2018, 138, 2264–2274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sen, C.K.; Roy, S.; Mathew-Steiner, S.S.; Gordillo, G.M. Biofilm Management in Wound Care. Plast. Reconstr. Surg. 2021, 148, 275E–288E. [Google Scholar] [CrossRef] [PubMed]
- Holzer-Geissler, J.C.J.; Schwingenschuh, S.; Zacharias, M.; Einsiedler, J.; Kainz, S.; Reisenegger, P.; Holecek, C.; Hofmann, E.; Wolff-Winiski, B.; Fahrngruber, H.; et al. The Impact of Prolonged Inflammation on Wound Healing. Biomedicines 2022, 10, 856. [Google Scholar] [CrossRef] [PubMed]
- Bessa, L.J.; Fazii, P.; di Giulio, M.; Cellini, L. Bacterial Isolates from Infected Wounds and Their Antibiotic Susceptibility Pattern: Some Remarks about Wound Infection. Int. Wound J. 2015, 12, 47–52. [Google Scholar] [CrossRef]
- Pastar, I.; Sawaya, A.P.; Marjanovic, J.; Burgess, J.L.; Strbo, N.; Rivas, K.E.; Wikramanayake, T.C.; Head, C.R.; Stone, R.C.; Jozic, I.; et al. Intracellular Staphylococcus Aureus Triggers Pyroptosis and Contributes to Inhibition of Healing Due to Perforin-2 Suppression. J. Clin. Investig. 2021, 131, e133727. [Google Scholar] [CrossRef]
- Roy, S.; Santra, S.; Das, A.; Dixith, S.; Sinha, M.; Ghatak, S.; Ghosh, N.; Banerjee, P.; Khanna, S.; Mathew-Steiner, S.; et al. Staphylococcus Aureus Biofilm Infection Compromises Wound Healing by Causing Deficiencies in Granulation Tissue Collagen. Ann. Surg. 2020, 271, 1174–1185. [Google Scholar] [CrossRef]
- Macedo, G.H.R.V.; Costa, G.D.E.; Oliveira, E.R.; Damasceno, G.V.; Mendonça, J.S.P.; Silva, L.D.S.; Chagas, V.L.; Bazán, J.M.N.; Aliança, A.S.D.S.; de Miranda, R.D.C.M.; et al. Interplay between Eskape Pathogens and Immunity in Skin Infections: An Overview of the Major Determinants of Virulence and Antibiotic Resistance. Pathogens 2021, 10, 148. [Google Scholar] [CrossRef]
- Ramalingam, S.; Chandrasekar, M.J.N.; Nanjan, M.J. Plant-Based Natural Products for Wound Healing: A Critical Review. Curr. Drug Res. Rev. 2022, 14, 37–60. [Google Scholar] [CrossRef]
- Coelho, L.C.B.B.; Silva, P.M.d.S.; de Oliveira, W.F.; de Moura, M.C.; Pontual, E.V.; Gomes, F.S.; Paiva, P.M.G.; Napoleão, T.H.; Correia, M.T.d.S. Lectins as Antimicrobial Agents. J. Appl. Microbiol. 2018, 125, 1238–1252. [Google Scholar] [CrossRef] [Green Version]
- Jandú, J.J.B.; Moraes Neto, R.N.; Zagmignan, A.; de Sousa, E.M.; Brelaz-de-Castro, M.C.A.; dos Santos Correia, M.T.; da Silva, L.C.N. Targeting the Immune System with Plant Lectins to Combat Microbial Infections. Front. Pharmacol. 2017, 8, 671. [Google Scholar] [CrossRef]
- Dias, R.d.O.; Machado, L.d.S.; Migliolo, L.; Franco, O.L. Insights into Animal and Plant Lectins with Antimicrobial Activities. Molecules 2015, 20, 519–541. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feriani, A.; Tir, M.; Arafah, M.; Gómez-Caravaca, A.M.; Contreras, M.d.M.; Nahdi, S.; Taamalli, A.; Allagui, M.S.; Alwasel, S.; Segura-Carretero, A.; et al. Schinus Terebinthifolius Fruits Intake Ameliorates Metabolic Disorders, Inflammation, Oxidative Stress, and Related Vascular Dysfunction, in Atherogenic Diet-Induced Obese Rats. Insight of Their Chemical Characterization Using HPLC-ESI-QTOF-MS/MS. J. Ethnopharmacol. 2021, 269, 113701. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, V.S.; Augusta, I.M.; Braz, M.V.d.C.; Riger, C.J.; Prudêncio, E.R.; Sawaya, A.C.H.F.; Sampaio, G.R.; Torres, E.A.F.d.S.; Saldanha, T. Aroeira Fruit (Schinus Terebinthifolius Raddi) as a Natural Antioxidant: Chemical Constituents, Bioactive Compounds and in Vitro and in Vivo Antioxidant Capacity. Food Chem. 2020, 315, 126274. [Google Scholar] [CrossRef] [PubMed]
- Gomes, F.S.; Procópio, T.F.; Napoleão, T.H.; Coelho, L.C.B.B.; Paiva, P.M.G. Antimicrobial Lectin from Schinus Terebinthifolius Leaf. J. Appl. Microbiol. 2013, 114, 672–679. [Google Scholar] [CrossRef] [PubMed]
- Lima, I.M.d.S.F.; Zagmignan, A.; Santos, D.M.; Maia, H.S.; dos Santos Silva, L.; da Silva Cutrim, B.; Vieira, S.L.; Bezerra Filho, C.M.; de Sousa, E.M.; Napoleão, T.H.; et al. Schinus Terebinthifolia Leaf Lectin (SteLL) Has Anti-Infective Action and Modulates the Response of Staphylococcus Aureus-Infected Macrophages. Sci. Rep. 2019, 9, 18159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brito Marques Ramos, D.; de Moura Fontes Araújo, M.T.; de Lima Araújo, T.C.; dos Santos Neto, O.G.; e Silva, M.G.; Silva, Y.A.; Lira Torres, D.J.; de Siqueira Patriota, L.L.; de Melo, C.M.L.; de Lorena, V.M.B.; et al. Evaluation of Antitumor Activity and Toxicity of Schinus Terebinthifolia Leaf Extract and Lectin (SteLL) in Sarcoma 180-Bearing Mice. J. Ethnopharmacol. 2019, 233, 148–157. [Google Scholar] [CrossRef]
- Ramos, D.B.M.; Araújo, M.T.M.F.; Araújo, T.C.L.; Silva, Y.A.; Santos, A.C.L.A.; Silva, M.G.; Paiva, P.M.G.; Mendes, R.L.; Napoleão, T.H. Antinociceptive Activity of Schinus Terebinthifolia Leaf Lectin (SteLL) in Sarcoma 180-Bearing Mice. J. Ethnopharmacol. 2020, 259, 112952. [Google Scholar] [CrossRef]
- Lima, B.R.F.; Patriota, L.L.d.S.; Marinho, A.d.O.; Costa, J.A.; Napoleão, T.H.; Rosa, M.M.; Paiva, P.M.G. The Anxiolytic Activity of Schinus Terebinthifolia Leaf Lectin (SteLL) Is Dependent on Monoaminergic Signaling Although Independent of the Carbohydrate-Binding Domain of the Lectin. Pharmaceuticals 2022, 15, 1364. [Google Scholar] [CrossRef]
- Marinho, A.O.; Brito, J.S.; Costa, J.A.; Silva, A.R.; Silva, S.P.; Amorim, L.C.; Correia, M.T.d.S.; Paiva, P.M.G.; Oliveira, A.M.; Patriota, L.L.d.S.; et al. Schinus Terebinthifolia Leaf Lectin Has Central and Peripheral Antinociceptive Action Mediated by Its Carbohydrate-Recognition Domain and Delta-Opioid Receptors. J. Ethnopharmacol. 2023, 301, 115817. [Google Scholar] [CrossRef]
- Diniz, R.M.; Fernandes, T.G.F.; Mendonça, J.S.P.; Silva, L.d.S.; Saminez, W.F.d.S.; Oliveira, P.V.; Amorim, E.A.F.; Figueiredo, C.S.S.S.; Bezerra Filho, C.M.; Correia, M.T.S.; et al. Antimicrobial and Anti-Inflammatory Effects of Eugenia Brejoensis Essential Oil in Mice Wounds Infected by Staphylococcus Aureus. Front. Pharmacol. 2022, 14, 4349. [Google Scholar] [CrossRef]
- Ribeiro, D.M.L.; Júnior, A.R.C.; Macedo, G.H.R.V.; Chagas, V.L.; Silva, L.S.; Cutrim, B.S.; Santos, D.M.; Soares, B.L.L.; Zagmignan, A.; Miranda, R.C.M.; et al. Polysaccharide-Based Formulations for Healing of Skin-Related Wound Infections: Lessons from Animal Models and Clinical Trials. Biomolecules 2020, 10, 63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carneiro, M.A.M.S.; Silva, L.S.; Diniz, R.M.; Saminez, W.F.d.S.; Oliveira, P.V.; Pereira Mendonça, J.S.; Colasso, A.H.M.; Soeiro Silva, I.S.; Jandú, J.J.B.; Sá, J.C.; et al. Immunomodulatory and Anti-Infective Effects of Cratylia Mollis Lectin (Cramoll) in a Model of Wound Infection Induced by Staphylococcus Aureus. Int. Immunopharmacol. 2021, 100, 108094. [Google Scholar] [CrossRef] [PubMed]
- Silva, V.; Peirone, C.; Amaral, J.S.; Capita, R.; Alonso-Calleja, C.; Marques-Magallanes, J.A.; Martins, Â.; Carvalho, Á.; Maltez, L.; Pereira, J.E.; et al. High Efficacy of Ozonated Oils on the Removal of Biofilms Produced by Methicillin-Resistant Staphylococcus Aureus (MRSA) from Infected Diabetic Foot Ulcers. Molecules 2020, 25, 3601. [Google Scholar] [CrossRef] [PubMed]
- Kakkar, H.; Chaudhary, N.; Mehta, D.; Saini, V.; Maheshwari, S.; Singh, J.; Walia, P.; Bajaj, A. N-Methyl Benzimidazole Tethered Cholic Acid Amphiphiles Can Eradicate S. Aureus-Mediated Biofilms and Wound Infections. Molecules 2022, 27, 3501. [Google Scholar] [CrossRef] [PubMed]
- Coriolano, M.C.; de Melo, C.M.L.; Silva, F.D.O.; Schirato, G.V.; Porto, C.S.; dos Santos, P.J.P.; Correia, M.T.D.S.; Porto, A.L.F.; Carneiro-Leão, A.M.D.A.; Coelho, L.C.B.B. Parkia Pendula Seed Lectin: Potential Use to Treat Cutaneous Wounds in Healthy and Immunocompromised Mice. Appl. Biochem. Biotechnol. 2014, 172, 2682–2693. [Google Scholar] [CrossRef]
- Sousa, F.D.; Vasconselos, P.D.; Silva, A.F.B.; Mota, E.F.; Rocha Tomé, A.; Mendes, F.R.d.S.; Gomes, A.M.M.; Abraham, D.J.; Shiwen, X.; Owen, J.S.; et al. Hydrogel and Membrane Scaffold Formulations of Frutalin (Breadfruit Lectin) within a Polysaccharide Galactomannan Matrix Have Potential for Wound Healing. Int. J. Biol. Macromol. 2019, 121, 429–442. [Google Scholar] [CrossRef]
- Nascimento Neto, L.G.; Silva Pinto, L.; Bastos, R.M.; Evaristo, F.F.V.; Vasconcelos, M.A.; Carneiro, V.A.; Arruda, F.V.S.; Porto, A.L.F.; Leal, R.B.; Silva, V.A.; et al. Effect of the Lectin of Bauhinia Variegata and Its Recombinant Isoform on Surgically Induced Skin Wounds in a Murine Model. Molecules 2011, 16, 9298–9315. [Google Scholar] [CrossRef]
- Santos, A.J.C.A.; Silva Barros, B.R.; Souza Aguiar, L.M.; Siqueira Patriota, L.L.; Albuquerque Lima, T.; Zingali, R.B.; Paiva, P.M.G.; Napoleão, T.H.; Melo, C.M.L.; Pontual, E.V. Schinus Terebinthifolia Leaf Lectin (SteLL) Is an Immunomodulatory Agent by Altering Cytokine Release by Mice Splenocytes. 3 Biotech 2020, 10, 144. [Google Scholar] [CrossRef]
- Okonkwo, U.A.; Dipietro, L.A. Diabetes and Wound Angiogenesis. Int. J. Mol. Sci. 2017, 18, 1419. [Google Scholar] [CrossRef] [Green Version]
- DiPietro, L.A. Angiogenesis and Wound Repair: When Enough Is Enough. J. Leukoc. Biol. 2016, 100, 979–984. [Google Scholar] [CrossRef] [Green Version]
- Han, C.; Barakat, M.; DiPietro, L.A. Angiogenesis in Wound Repair: Too Much of a Good Thing? Cold Spring Harb. Perspect. Biol. 2022, 14, a041225. [Google Scholar] [CrossRef]
- Farahpour, M.R.; Pirkhezr, E.; Ashrafian, A.; Sonboli, A. Accelerated Healing by Topical Administration of Salvia Officinalis Essential Oil on Pseudomonas Aeruginosa and Staphylococcus Aureus Infected Wound Model. Biomed. Pharmacother. 2020, 128, 110120. [Google Scholar] [CrossRef] [PubMed]
- Farahpour, M.R.; Sheikh, S.; Kafshdooz, E.; Sonboli, A. Accelerative Effect of Topical Zataria Multiflora Essential Oil against Infected Wound Model by Modulating Inflammation, Angiogenesis, and Collagen Biosynthesis. Pharm. Biol. 2021, 59, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Lowry, O.H.; Rosebrough, N.J.; Farr, A.L.; Randall, R.J. Protein Measurement with the Folin Phenol Reagent. J. Biol. Chem. 1951, 193, 265–275. [Google Scholar] [CrossRef]
- Procópio, T.F.; de Siqueira Patriota, L.L.; de Moura, M.C.; da Silva, P.M.; de Oliveira, A.P.S.; do Nascimento Carvalho, L.V.; de Albuquerque Lima, T.; Soares, T.; da Silva, T.D.; Breitenbach Barroso Coelho, L.C.; et al. CasuL: A New Lectin Isolated from Calliandra Surinamensis Leaf Pinnulae with Cytotoxicity to Cancer Cells, Antimicrobial Activity and Antibiofilm Effect. Int. J. Biol. Macromol. 2017, 98, 419–429. [Google Scholar] [CrossRef]
- Carvalho, A.R.; Martins, A.L.D.B.; Cutrim, B.D.S.; Santos, D.M.; Maia, H.S.; da Silva, M.S.M.; Zagmignan, A.; Silva, M.R.C.; Monteiro, C.D.A.; Guilhon, G.M.S.P.; et al. Betulinic Acid Prevents the Acquisition of Ciprofloxacin-Mediated Mutagenesis in Staphylococcus Aureus. Molecules 2019, 24, 1757. [Google Scholar] [CrossRef] [Green Version]
- Schneider, C.A.; Rasband, W.S.; Eliceiri, K.W. NIH Image to ImageJ: 25 Years of Image Analysis. Nat. Methods 2012, 9, 671–675. [Google Scholar] [CrossRef]
- Ferro, T.A.F.; Souza, E.B.; Suarez, M.A.M.; Rodrigues, J.F.S.; Pereira, D.M.S.; Mendes, S.J.F.; Gonzaga, L.F.; Machado, M.C.A.M.; Bomfim, M.R.Q.; Calixto, J.B.; et al. Topical Application of Cinnamaldehyde Promotes Faster Healing of Skin Wounds Infected with Pseudomonas Aeruginosa. Molecules 2019, 24, 1627. [Google Scholar] [CrossRef]


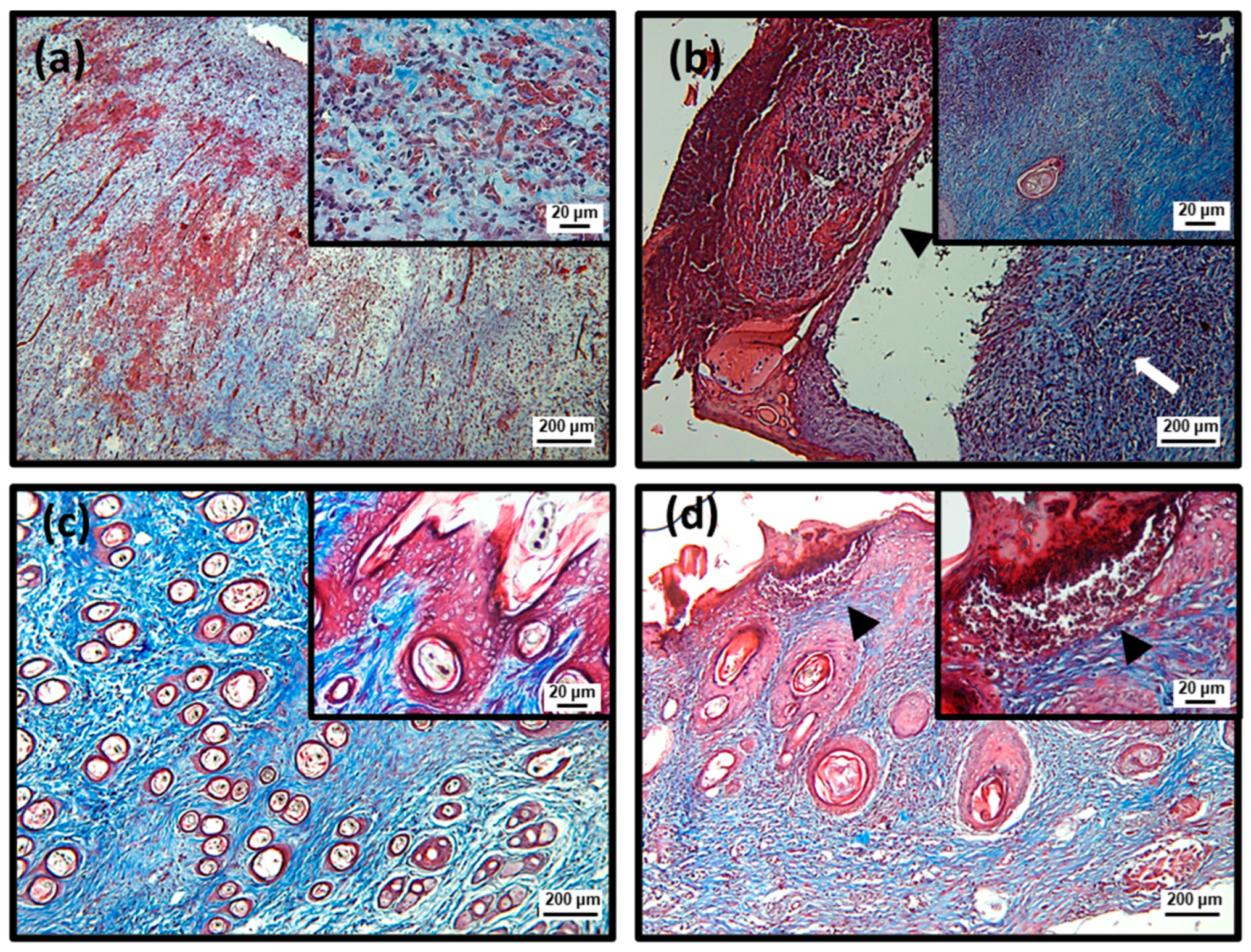



| Parameter | Uninfected | Infected | SteLL | ||
|---|---|---|---|---|---|
| 32 µg/mL | 64 µg/mL | ||||
| 3 days | Cell debris | 2 ± 0 a | 3 ± 0 b | 3 ± 0 b | 2.25 ± 0.5 a |
| Re-epithelization | 0 ± 0 a | 0 ± 0 a | 0 ± 0 a | 0 ± 0 a | |
| Inflammatory infiltrate | 1.25 ± 0.5 a | 3 ± 0 b | 3 ± 0 b | 2.5 ± 0.58 c | |
| Fibroblast proliferation | - | - | - | - | |
| 10 days | Cell debris | 0 ± 0 a | 1 ± 0 b | 0 ± 0 a | 1 ± 0.58 b |
| Re-epithelization | 3 ± 0 a | 2.5 ± 0.5 b | 3 ± 0 a | 2.0 ± 0.5 c | |
| Inflammatory infiltrate | 0 ± 0 a | 2 ± 0 b | 1 ± 0 c | 2 ± 0 b | |
| Fibroblast proliferation | 1.25 ± 0.5 a | 3 ± 0 b | 3 ± 0 b | 2.5 ± 0.58 c | |
| 17 days | Cell debris | 0 ± 0 a | 0.5 ± 0 b | 0 ± 0 a | 0 ± 0 a |
| Re-epithelization | 3 ± 0 a | 3 ± 0 a | 3 ± 0 a | 3 ± 0 a | |
| Inflammatory infiltrate | 0 ± 0 a | 1 ± 0 b | 0 ± 0 a | 0 ± 0 a | |
| Fibroblast proliferation | 2.25 ± 0.5 a | 2 ± 0 a | 3 ± 0 b | 3 ± 0 b | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nunes, M.A.S.; Silva, L.d.S.; Santos, D.M.; Cutrim, B.d.S.; Vieira, S.L.; Silva, I.S.S.; Castelo Branco, S.J.d.S.; Nascimento, M.d.S.d.; Vale, A.A.M.; Santos-Azevedo, A.P.S.d.; et al. Schinus terebinthifolius Leaf Lectin (SteLL) Reduces the Bacterial and Inflammatory Burden of Wounds Infected by Staphylococcus aureus Promoting Skin Repair. Pharmaceuticals 2022, 15, 1441. https://doi.org/10.3390/ph15111441
Nunes MAS, Silva LdS, Santos DM, Cutrim BdS, Vieira SL, Silva ISS, Castelo Branco SJdS, Nascimento MdSd, Vale AAM, Santos-Azevedo APSd, et al. Schinus terebinthifolius Leaf Lectin (SteLL) Reduces the Bacterial and Inflammatory Burden of Wounds Infected by Staphylococcus aureus Promoting Skin Repair. Pharmaceuticals. 2022; 15(11):1441. https://doi.org/10.3390/ph15111441
Chicago/Turabian StyleNunes, Marcio Anderson Sousa, Lucas dos Santos Silva, Deivid Martins Santos, Brenda da Silva Cutrim, Silvamara Leite Vieira, Izadora Souza Soeiro Silva, Simeone Júlio dos Santos Castelo Branco, Mayara de Santana do Nascimento, André Alvares Marques Vale, Ana Paula Silva dos Santos-Azevedo, and et al. 2022. "Schinus terebinthifolius Leaf Lectin (SteLL) Reduces the Bacterial and Inflammatory Burden of Wounds Infected by Staphylococcus aureus Promoting Skin Repair" Pharmaceuticals 15, no. 11: 1441. https://doi.org/10.3390/ph15111441
APA StyleNunes, M. A. S., Silva, L. d. S., Santos, D. M., Cutrim, B. d. S., Vieira, S. L., Silva, I. S. S., Castelo Branco, S. J. d. S., Nascimento, M. d. S. d., Vale, A. A. M., Santos-Azevedo, A. P. S. d., Zagmignan, A., Sousa, J. C. d. S., Napoleão, T. H., Paiva, P. M. G., Monteiro-Neto, V., & Nascimento da Silva, L. C. (2022). Schinus terebinthifolius Leaf Lectin (SteLL) Reduces the Bacterial and Inflammatory Burden of Wounds Infected by Staphylococcus aureus Promoting Skin Repair. Pharmaceuticals, 15(11), 1441. https://doi.org/10.3390/ph15111441










