Searching for Effective Treatments in HFpEF: Implications for Modeling the Disease in Rodents
Abstract
:1. Introduction
2. Results
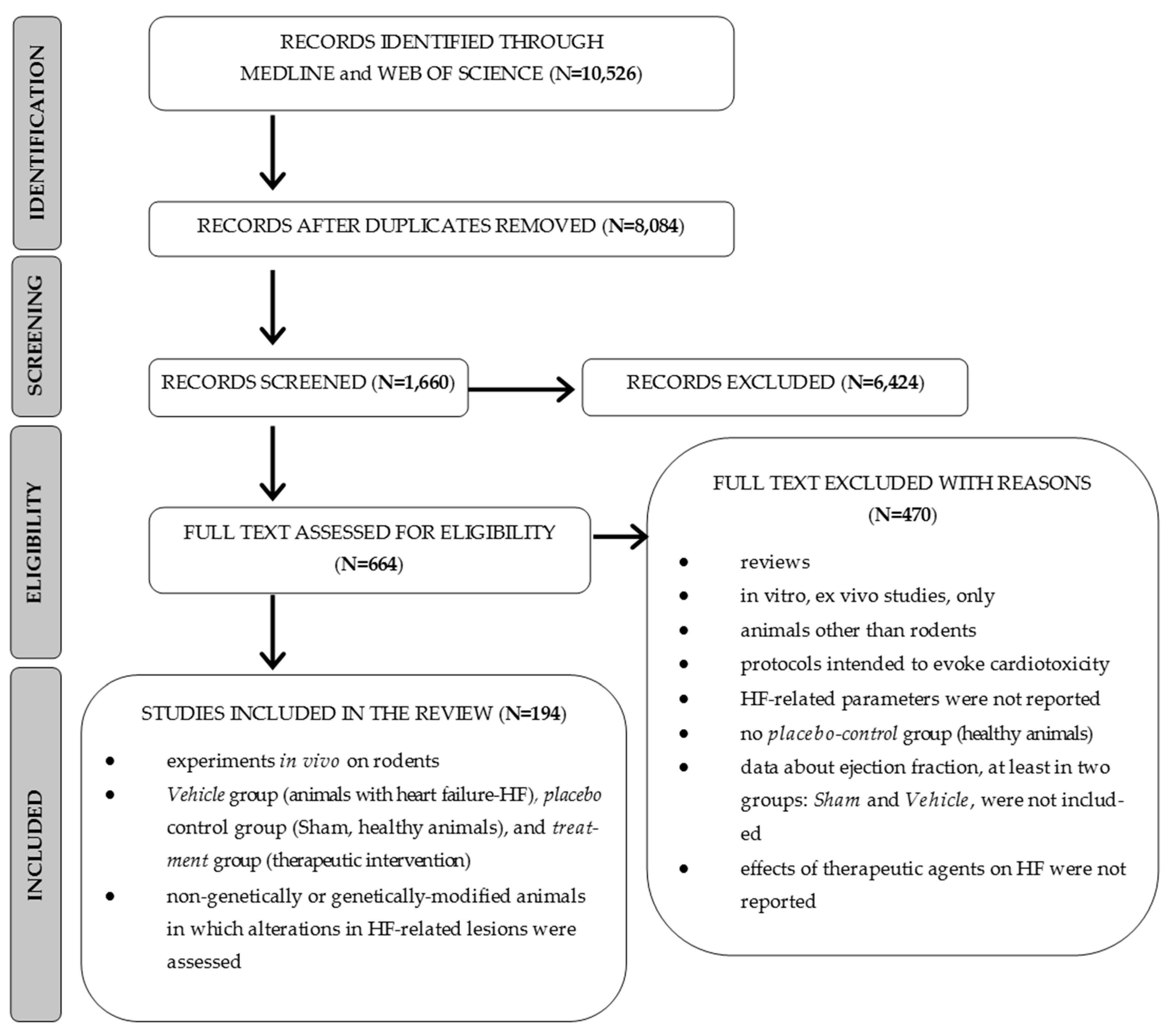
2.1. Selection of Studies
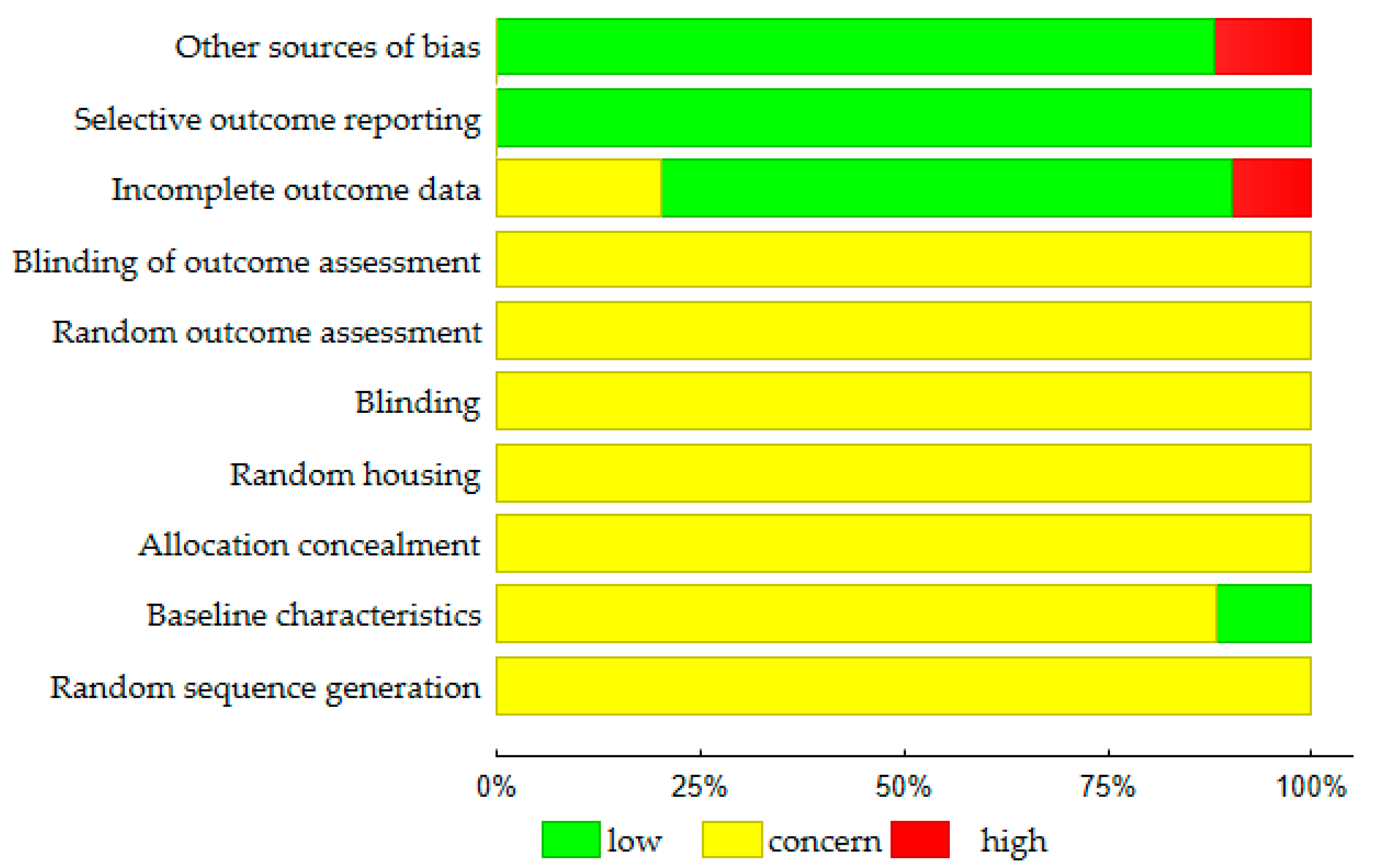
2.2. Quality Assessments
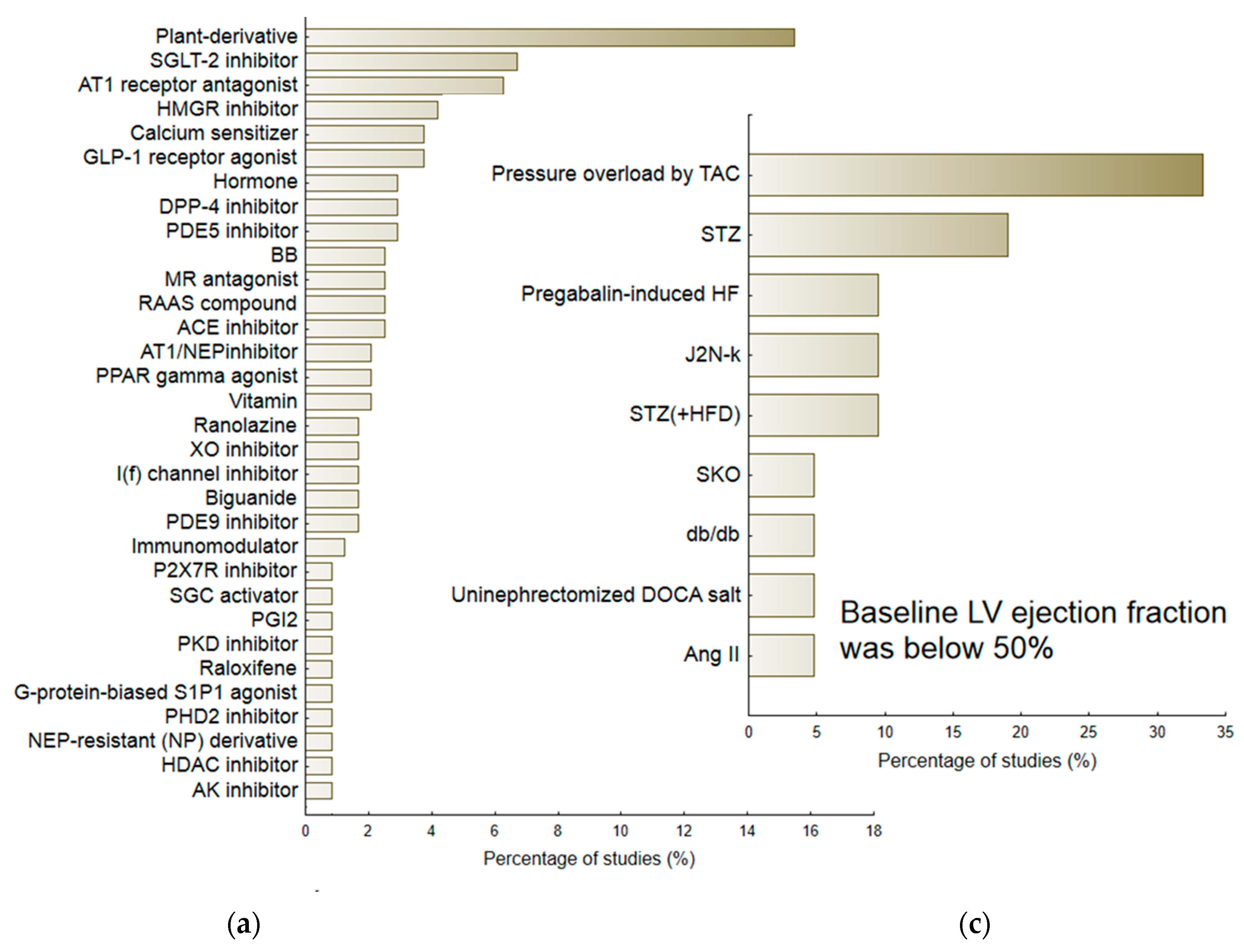
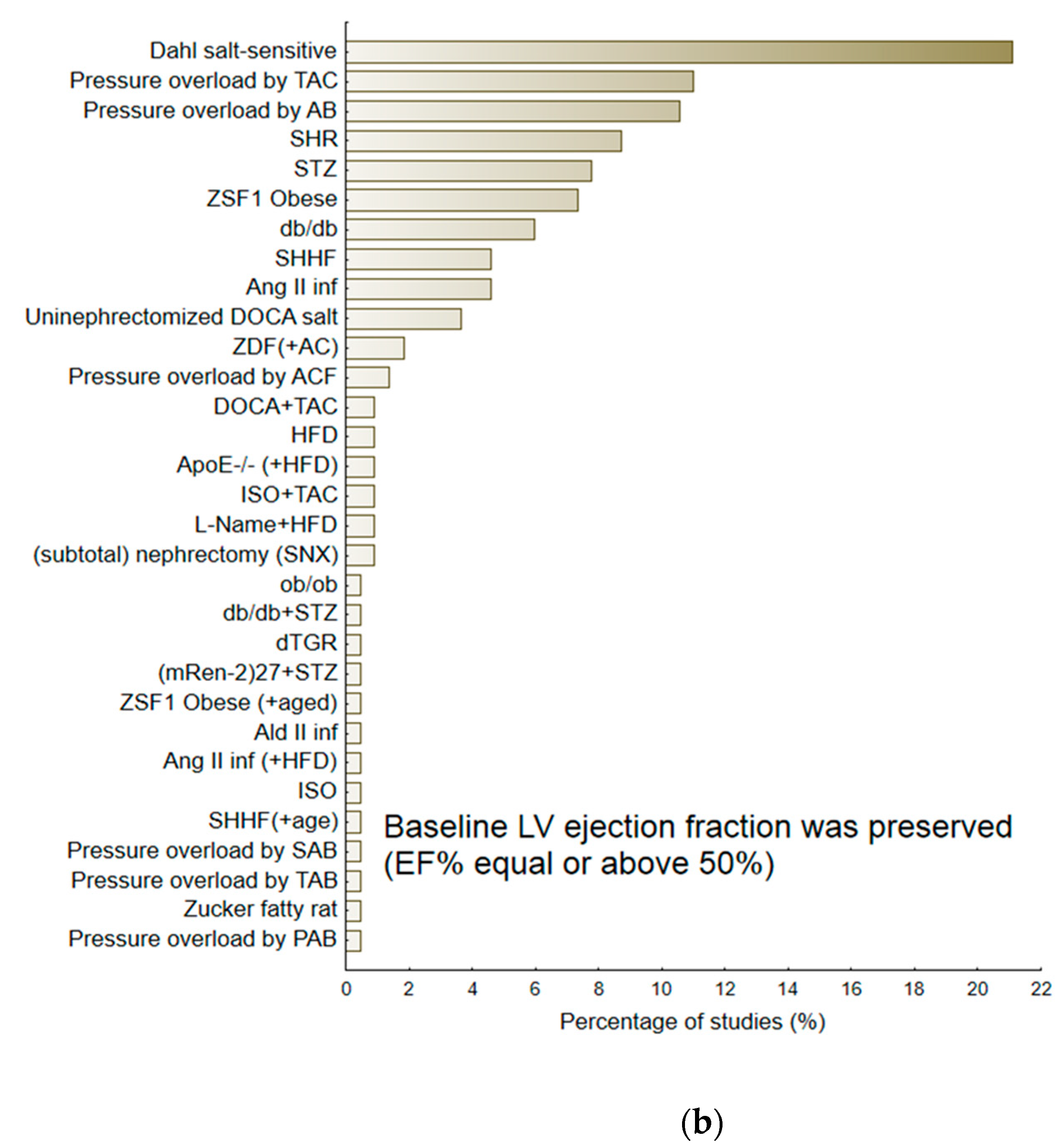
2.3. Animal Models and Therapeutic Agents
2.4. Efficacy of Treatments for HF
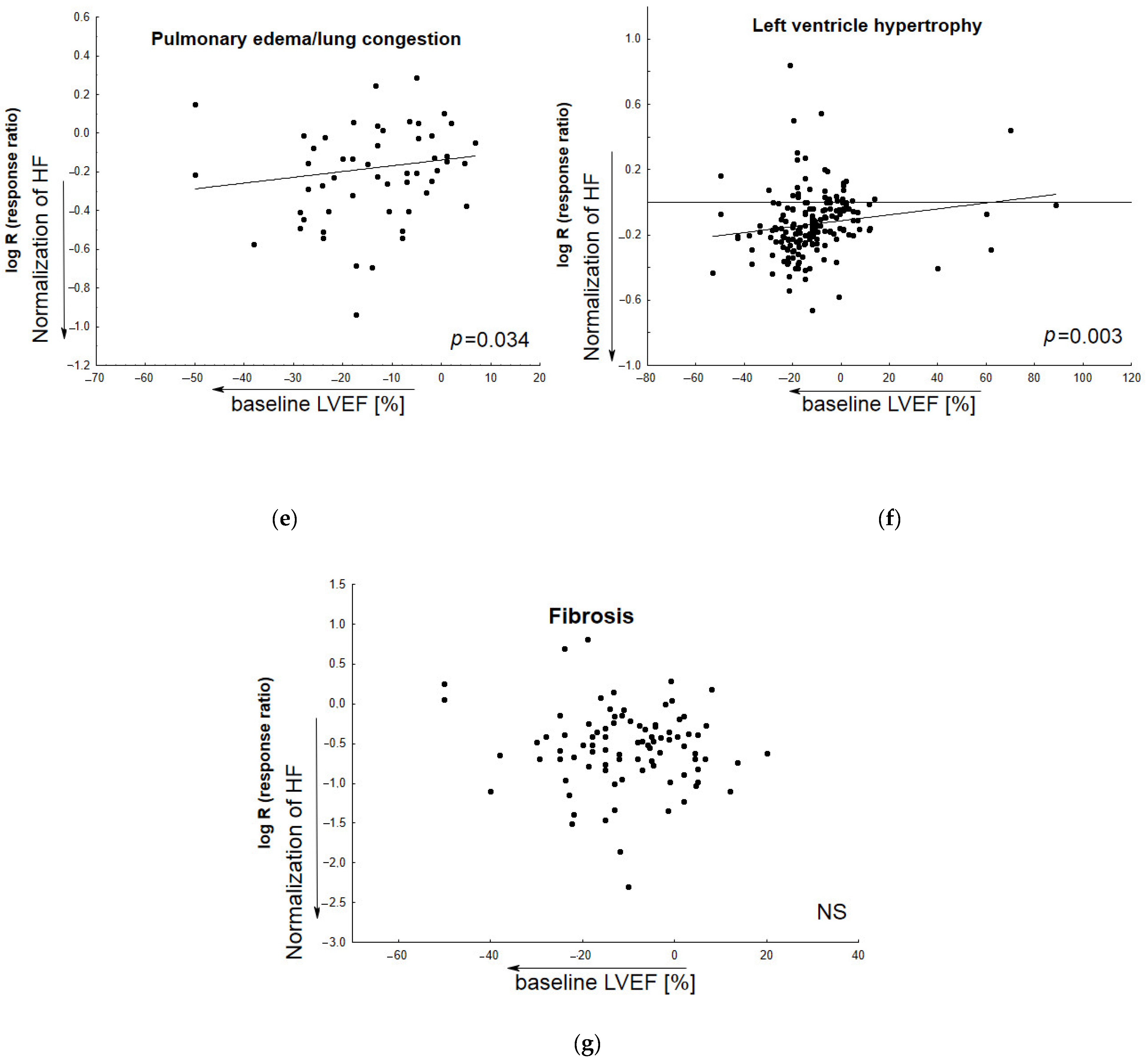
2.5. The Resultant Efficacy of Treatments for HF in Relation to the Baseline LVEF
3. Discussion
3.1. The Selection of Animal Models for Pre-Clinical Evaluations of Candidate Drugs
3.2. Treatment Goals in Pre- and Clinical Studies
3.3. Comorbid Conditions
3.4. The Role of the LVEF Parameter
3.5. Molecular Aspects of HFpEF Models
3.6. Study Limitations
4. Materials and Methods
4.1. Article Search and Data Extraction
4.2. Quality Assessments
4.3. Data Synthesis
5. Conclusions
- (a)
- Experimental approaches are characterized with varying degrees of effectiveness regarding their ability to develop the disease by the most common comorbidities associated with human HFpEF (hypertension, hyperglycemia, and/or obesity). The ZSF1 model is able to develop disease by a similar set of conditions to humans; as such, it appears suitable for identifying candidate medications.
- (b)
- The minority of experiments concerned drug-related normalization of pulmonary congestion, and even fewer entailed the improvement of animal exercise capacity. Both features represent treatment goals for patients with HF, and this phenomenon can make it difficult to comprehensively evaluate effective treatments for human HFpEF.
- (c)
- The baseline ejection fraction can play a key role in determining the extent to which particular medicine agents normalized the disease according to diastolic dysfunction, LV hypertrophy, or pulmonary congestion. In a particular model, preserving LVEF seems to favor the acquisition of reproducible and repeatable results for individual medicines.
- (d)
- The mortality associated with a candidate agent can be determined based on the likelihood of an individual experimental model to worsen animal survival. This should be taken into consideration in studies comparing different therapeutic agents.
- (e)
- Animal models of HFpEF might represent a promising approach for evaluating the deleterious functional and structural consequences of the disease at the molecular level, and for identifying future specific drug therapies. However, these effects were reported in only a small number of papers.
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Van Riet, E.E.; Hoes, A.W.; Wagenaar, K.P.; Limburg, A.; Landman, M.A.; Rutten, F.H. Epidemiology of heart failure: The prevalence of heart failure and ventricular dysfunction in older adults over time. A systematic review. Eur. J. Heart Fail. 2016, 18, 242–252. [Google Scholar] [CrossRef]
- Owan, T.E.; Hodge, D.O.; Herges, R.M.; Jacobsen, S.J.; Roger, V.L.; Redfield, M.M. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N. Engl. J. Med. 2006, 355, 251–259. [Google Scholar] [CrossRef]
- Del Buono, M.G.; Iannaccone, G.; Scacciavillani, R.; Carbone, S.; Camilli, M.; Niccoli, G.; Borlaug, B.A.; Lavie, C.J.; Arena, R.; Crea, F.; et al. Heart failure with preserved ejection fraction diagnosis and treatment: An updated review of the evidence. Prog. Cardiovasc. Dis. 2020, 63, 570–584. [Google Scholar] [CrossRef] [PubMed]
- Borlaug, B.A. The pathophysiology of heart failure with preserved ejection fraction. Nat. Rev. Cardiol. 2014, 11, 507–515. [Google Scholar] [CrossRef]
- Conceição, G.; Heinonen, I.; Lourenço, A.P.; Duncker, D.J.; Falcão-Pires, I. Animal models of heart failure with preserved ejection fraction. Neth. Heart J. 2016, 24, 275–286. [Google Scholar] [CrossRef]
- Valero-Muñoz, M.; Backman, W.; Sam, F. Murine Models of Heart Failure with Preserved Ejection Fraction: A “Fishing Expedition”. JACC Basic Transl. Sci. 2017, 2, 770–789. [Google Scholar] [CrossRef] [PubMed]
- Jasińska-Stroschein, M. Searching for an experimental rodent model of heart failure with preserved ejection fraction: Revisited. Biomed. Pharmacother. 2022, 152, 113251. [Google Scholar] [CrossRef] [PubMed]
- Barandiarán Aizpurua, A.; Schroen, B.; van Bilsen, M.; van Empel, V. Targeted HFpEF therapy based on matchmaking of human and animal models. Am. J. Physiol.-Heart Circ. Physiol. 2018, 315, H1670–H1683. [Google Scholar] [CrossRef]
- Abdellatif, M.; Trummer-Herbst, V.; Koser, F.; Durand, S.; Adão, R.; Vasques-Nóvoa, F.; Freundt, J.K.; Voglhuber, J.; Pricolo, M.R.; Kasa, M.; et al. Nicotinamide for the treatment of heart failure with preserved ejection fraction. Sci. Transl. Med. 2021, 13, eabd7064. [Google Scholar] [CrossRef]
- Abdurrachim, D.; Teo, X.Q.; Woo, C.C.; Chan, W.X.; Lalic, J.; Lam, C.S.P.; Lee, P.T.H. Empagliflozin reduces myocardial ketone utilization while preserving glucose utilization in diabetic hypertensive heart disease: A hyperpolarized 13 C magnetic resonance spectroscopy study. Diabetes Obes. Metab. 2019, 21, 357–365. [Google Scholar] [CrossRef] [PubMed]
- Adams, V.; Schauer, A.; Augstein, A.; Kirchhoff, V.; Draskowski, R.; Jannasch, A.; Goto, K.; Lyall, G.; Männel, A.; Barthel, P.; et al. Targeting MuRF1 by small molecules in a HFpEF rat model improves myocardial diastolic function and skeletal muscle contractility. J. Cachexia Sarcopenia Muscle 2022, 13, 1565–1581. [Google Scholar] [CrossRef]
- Akahori, H.; Tsujino, T.; Naito, Y.; Matsumoto, M.; Sasaki, N.; Iwasaku, T.; Eguchi, A.; Sawada, H.; Hirotani, S.; Masuyama, T. Atorvastatin ameliorates cardiac fibrosis and improves left ventricular diastolic function in hypertensive diastolic heart failure model rats. J. Hypertens. 2014, 32, 1534–1541. [Google Scholar] [CrossRef]
- Akinwumi, B.C.; Raj, P.; Lee, D.I.; Acosta, C.; Yu, L.; Thomas, S.M.; Nagabhushanam, K.; Majeed, M.; Davies, N.M.; Netticadan, T.; et al. Disparate Effects of Stilbenoid Polyphenols on Hypertrophic Cardiomyocytes In Vitro vs. in the Spontaneously Hypertensive Heart Failure Rat. Molecules 2017, 22, 204. [Google Scholar] [CrossRef] [PubMed]
- Altara, R.; da Silva, G.J.J.; Frisk, M.; Spelta, F.; Zouein, F.A.; Louch, W.E.; Booz, G.W.; Cataliotti, A. Cardioprotective Effects of the Novel Compound Vastiras in a Preclinical Model of End-Organ Damage. Hypertension 2020, 75, 1195–1204. [Google Scholar] [CrossRef] [PubMed]
- Aroor, A.R.; Mummidi, S.; Lopez-Alvarenga, J.C.; Das, N.; Habibi, J.; Jia, G.; Lastra, G.; Chandrasekar, B.; DeMarco, V.G. Sacubitril/valsartan inhibits obesity-associated diastolic dysfunction through suppression of ventricular-vascular stiffness. Cardiovasc. Diabetol. 2021, 20, 80. [Google Scholar] [CrossRef]
- Asensio Lopez, M.D.C.; Lax, A.; Hernandez Vicente, A.; Saura Guillen, E.; Hernandez-Martinez, A.; Fernandez Del Palacio, M.J.; Bayes-Genis, A.; Pascual Figal, D.A. Empagliflozin improves post-infarction cardiac remodeling through GTP enzyme cyclohydrolase 1 and irrespective of diabetes status. Sci. Rep. 2020, 10, 13553. [Google Scholar] [CrossRef]
- Awwad, Z.M.; El-Ganainy, S.O.; ElMallah, A.I.; Khattab, M.M.; El-Khatib, A.S. Telmisartan and captopril ameliorate pregabalin-induced heart failure in rats. Toxicology 2019, 428, 152310. [Google Scholar] [CrossRef]
- Bai, X.J.; Hao, J.T.; Zheng, R.H.; Yan, C.P.; Wang, J.; Yang, C.H.; Zhang, W.F.; Zhao, Z.Q. Glucagon-Like Peptide-1 Analog Liraglutide Attenuates Pressure-Overload Induced Cardiac Hypertrophy and Apoptosis through Activating ATP Sensitive Potassium Channels. Cardiovasc. Drugs Ther. 2021, 35, 87–101. [Google Scholar] [CrossRef] [PubMed]
- Bartoli, F.; Bailey, M.A.; Rode, B.; Mateo, P.; Antigny, F.; Bedouet, K.; Gerbaud, P.; Gosain, R.; Plante, J.; Norman, K.; et al. Orai1 Channel Inhibition Preserves Left Ventricular Systolic Function and Normal Ca2+ Handling After Pressure Overload. Circulation 2020, 141, 199–216. [Google Scholar] [CrossRef]
- Benes, J.; Kazdova, L.; Drahota, Z.; Houstek, J.; Medrikova, D.; Kopecky, J.; Kovarova, N.; Vrbacky, M.; Sedmera, D.; Strnad, H.; et al. Effect of metformin therapy on cardiac function and survival in a volume-overload model of heart failure in rats. Clin. Sci. 2011, 121, 29–41. [Google Scholar] [CrossRef]
- Biala, A.; Finckenberg, P.; Korpi, A.; Loytainen, M.; Martonen, E.; Levijoki, J.; Mervaala, E. Cardiovascular effects of the combination of levosimendan and valsartan in hypertensive Dahl/Rapp rats. J. Physiol. Pharmacol. 2011, 62, 275–285. [Google Scholar]
- Bryson, T.D.; Pandrangi, T.S.; Khan, S.Z.; Xu, J.; Pavlov, T.S.; Ortiz, P.A.; Peterson, E.; Harding, P. The deleterious role of the prostaglandin E2 EP3 receptor in angiotensin II hypertension. Am. J. Physiol. Heart Circ. Physiol. 2020, 318, H867–H882. [Google Scholar] [CrossRef] [PubMed]
- Bugyei-Twum, A.; Ford, C.; Civitarese, R.; Seegobin, J.; Advani, S.L.; Desjardins, J.F.; Kabir, G.; Zhang, Y.; Mitchell, M.; Switzer, J.; et al. Sirtuin 1 activation attenuates cardiac fibrosis in a rodent pressure overload model by modifying Smad2/3 transactivation. Cardiovasc. Res. 2018, 114, 1629–1641. [Google Scholar] [CrossRef] [PubMed]
- Burke, R.M.; Lighthouse, J.K.; Mickelsen, D.M.; Small, E.M. Sacubitril/Valsartan Decreases Cardiac Fibrosis in Left Ventricle Pressure Overload by Restoring PKG Signaling in Cardiac Fibroblasts. Circ. Heart Fail. 2019, 12, e005565. [Google Scholar] [CrossRef]
- Byrne, N.J.; Matsumura, N.; Maayah, Z.H.; Ferdaoussi, M.; Takahara, S.; Darwesh, A.M.; Levasseur, J.L.; Jahng, J.W.S.; Vos, D.; Parajuli, N.; et al. Empagliflozin Blunts Worsening Cardiac Dysfunction Associated With Reduced NLRP3 (Nucleotide-Binding Domain-Like Receptor Protein 3) Inflammasome Activation in Heart Failure. Circ. Heart Fail. 2020, 13, e006277. [Google Scholar] [CrossRef]
- Cao, H.J.; Fang, J.; Zhang, Y.L.; Zou, L.X.; Han, X.; Yang, J.; Yan, X.; Li, P.B.; Wang, H.X.; Guo, S.-B.; et al. Genetic ablation and pharmacological inhibition of immunosubunit β5i attenuates cardiac remodeling in deoxycorticosterone-acetate (DOCA)-salt hypertensive mice. J. Mol. Cell. Cardiol. 2019, 137, 34–45. [Google Scholar] [CrossRef] [PubMed]
- Cappetta, D.; De Angelis, A.; Ciuffreda, L.P.; Coppini, R.; Cozzolino, A.; Miccichè, A.; Dell’Aversana, C.; D’Amario, D.; Cianflone, E.; Scavone, C.; et al. Amelioration of diastolic dysfunction by dapagliflozin in a non-diabetic model involves coronary endothelium. Pharmacol. Res. 2020, 157, 104781. [Google Scholar] [CrossRef]
- Cezar, M.D.; Damatto, R.L.; Pagan, L.U.; Lima, A.R.; Martinez, P.F.; Bonomo, C.; Rosa, C.M.; Campos, D.H.; Cicogna, A.C.; Gomes, M.J.; et al. Early Spironolactone Treatment Attenuates Heart Failure Development by Improving Myocardial Function and Reducing Fibrosis in Spontaneously Hypertensive Rats. Cell. Physiol. Biochem. 2015, 36, 1453–1466. [Google Scholar] [CrossRef]
- Chan, V.; Hoey, A.; Brown, L. Improved cardiovascular function with aminoguanidine in DOCA-salt hypertensive rats. Br. J. Pharmacol. 2006, 148, 902–908. [Google Scholar] [CrossRef]
- Chang, D.; Xu, T.T.; Zhang, S.J.; Cai, Y.; Min, S.D.; Zhao, Z.; Lu, C.Q.; Wang, Y.C.; Ju, S. Telmisartan ameliorates cardiac fibrosis and diastolic function in cardiorenal heart failure with preserved ejection fraction. Exp. Biol. Med. 2021, 246, 2511–2521. [Google Scholar] [CrossRef]
- Chang, S.A.; Kim, Y.J.; Lee, H.W.; Kim, D.H.; Kim, H.K.; Chang, H.J.; Sohn, D.W.; Oh, B.H.; Park, Y.B. Effect of rosuvastatin on cardiac remodeling. function. and progression to heart failure in hypertensive heart with established left ventricular hypertrophy. Hypertension 2009, 54, 591–597. [Google Scholar] [CrossRef]
- Chang, X.; Zhang, T.; Wang, J.; Liu, Y.; Yan, P.; Meng, Q.; Yin, Y.; Wang, S. SIRT5-Related Desuccinylation Modification Contributes to Quercetin-Induced Protection against Heart Failure and High-Glucose-Prompted Cardiomyocytes Injured through Regulation of Mitochondrial Quality Surveillance. Oxid. Med. Cell. Longev. 2021, 2021, 5876841. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Zou, L.X.; Lin, Q.Y.; Yan, X.; Bi, H.L.; Xie, X.; Wang, S.; Wang, Q.S.; Zhang, Y.L.; Li, H.H. Resveratrol as a new inhibitor of immunoproteasome prevents PTEN degradation and attenuates cardiac hypertrophy after pressure overload. Redox Biol. 2019, 20, 390–401. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; Wu, J.L.; Fu, G.S.; Mou, Y.; Hu, S.J. Chronic treatment with qiliqiangxin ameliorates aortic endothelial cell dysfunction in diabetic rats. J. Cardiovasc. Pharmacol. Ther. 2015, 20, 230–240. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Zhuo, C.; Zu, A.; Yuan, S.; Zhang, H.; Zhao, J.; Zheng, L. Thymoquinone ameliorates pressure overload-induced cardiac hypertrophy by activating the AMPK signalling pathway. J. Cell. Mol. Med. 2022, 26, 855–867. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhang, Z.; Zhang, X.; Jia, Z.; Liu, J.; Chen, X.; Xu, A.; Liang, X.; Li, G. Paeonol attenuates heart failure induced by transverse aortic constriction via ERK1/2 signalling. Pharm. Biol. 2022, 60, 562–569. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Wang, L.; Huang, S.; Ke, J.; Wang, Q.; Zhou, Z.; Chang, W. Lutein attenuates angiotensin II-induced cardiac remodeling by inhibiting AP-1/IL-11 signaling. Redox. Biol. 2021, 44, 102020. [Google Scholar] [CrossRef]
- Chi, L.; Belardinelli, L.; Zeng, A.; Hirakawa, R.; Rajamani, S.; Ling, H.; Dhalla, A.K. Inhibition of late Na+ current. a novel target to improve diastolic function and electrical abnormalities in Dahl salt-sensitive rats. Am. J. Physiol. Heart Circ. Physiol. 2016, 310, H1313–H1320. [Google Scholar] [CrossRef]
- Chinnakkannu, P.; Reese, C.; Gaspar, J.A.; Panneerselvam, S.; Pleasant-Jenkins, D.; Mukherjee, R.; Baicu, C.; Tourkina, E.; Hoffman, S.; Kuppuswamy, D. Suppression of angiotensin II-induced pathological changes in heart and kidney by the caveolin-1 scaffolding domain peptide. PLoS ONE 2018, 13, e0207844. [Google Scholar] [CrossRef]
- Choudhary, R.; Palm-Leis, A.; Scott, R.C., 3rd; Guleria, R.S.; Rachut, E.; Baker, K.M.; Pan, J. All-trans retinoic acid prevents development of cardiac remodeling in aortic banded rats by inhibiting the renin-angiotensin system. Am. J. Physiol. Heart Circ. Physiol. 2008, 294, H633–H644. [Google Scholar] [CrossRef]
- Davila, A.; Tian, Y.; Czikora, I.; Li, J.; Su, H.; Huo, Y.; Patel, V.; Robinson, V.; Kapuku, G.; Weintraub, N.; et al. Adenosine Kinase Inhibition Augments Conducted Vasodilation and Prevents Left Ventricle Diastolic Dysfunction in Heart Failure With Preserved Ejection Fraction. Circ. Heart Fail. 2019, 12, e005762. [Google Scholar] [CrossRef] [PubMed]
- De Angelis, A.; Cappetta, D.; Piegari, E.; Rinaldi, B.; Ciuffreda, L.P.; Esposito, G.; Ferraiolo, F.A.; Rivellino, A.; Russo, R.; Donniacuo, M.; et al. Long-term administration of ranolazine attenuates diastolic dysfunction and adverse myocardial remodeling in a model of heart failure with preserved ejection fraction. Int. J. Cardiol. 2016, 217, 69–79. [Google Scholar] [CrossRef]
- Duda, M.K.; O’Shea, K.M.; Tintinu, A.; Xu, W.; Khairallah, R.J.; Barrows, B.R.; Chess, D.J.; Azimzadeh, A.M.; Harris, W.S.; Sharov, V.G.; et al. Fish oil. but not flaxseed oil. decreases inflammation and prevents pressure overload-induced cardiac dysfunction. Cardiovasc. Res. 2009, 81, 319–327. [Google Scholar] [CrossRef] [PubMed]
- Dulce, R.A.; Kanashiro-Takeuchi, R.M.; Takeuchi, L.M.; Salerno, A.G.; Wanschel, A.C.B.A.; Kulandavelu, S.; Balkan, W.; Zuttion, M.S.S.R.; Cai, R.; Schally, A.V.; et al. Synthetic growth hormone-releasing hormone agonist ameliorates the myocardial pathophysiology characteristic of HFpEF. Cardiovasc. Res. 2022, 118, 3586–3601. [Google Scholar]
- Esposito, G.; Cappetta, D.; Russo, R.; Rivellino, A.; Ciuffreda, L.P.; Roviezzo, F.; Piegari, E.; Berrino, L.; Rossi, F.; De Angelis, A.; et al. Sitagliptin reduces inflammation. fibrosis and preserves diastolic function in a rat model of heart failure with preserved ejection fraction. Br. J. Pharmacol. 2017, 174, 4070–4086. [Google Scholar] [CrossRef]
- Evaristi, M.F.; Poirier, B.; Chénedé, X.; Lefebvre, A.M.; Roccon, A.; Gillot, F.; Beeské, S.; Corbier, A.; Pruniaux-Harnist, M.P.; Janiak, P.; et al. A G-protein-biased S1P1 agonist. SAR247799. improved LVH and diastolic function in a rat model of metabolic syndrome. PLoS ONE 2022, 17, e0257929. [Google Scholar] [CrossRef] [PubMed]
- Fenning, A.; Harrison, G.; Rose’meyer, R.; Hoey, A.; Brown, L. l-Arginine attenuates cardiovascular impairment in DOCA-salt hypertensive rats. Am. J. Physiol. Heart Circ. Physiol. 2005, 289, H1408–H1416. [Google Scholar] [CrossRef]
- Ge, Q.; Zhao, L.; Liu, C.; Ren, X.; Yu, Y.H.; Pan, C.; Hu, Z. LCZ696. an Angiotensin Receptor-Neprilysin inhibitor. Improves Cardiac Hypertrophy and Fibrosis and Cardiac Lymphatic Remodeling in Transverse Aortic Constriction Model Mice. BioMed Res. Int. 2020, 2020, 7256862. [Google Scholar] [CrossRef]
- Gimenes, R.; Gimenes, C.; Rosa, C.M.; Xavier, N.P.; Campos, D.H.S.; Fernandes, A.A.H.; Cezar, M.D.M.; Guirado, G.N.; Pagan, L.U.; Chaer, I.D.; et al. Influence of apocynin on cardiac remodeling in rats with streptozotocin-induced diabetes mellitus. Cardiovasc. Diabetol. 2018, 17, 15. [Google Scholar] [CrossRef]
- Giri, S.R.; Bhoi, B.; Jain, M.R.; Gatne, M.M. Cardioprotective role of peroxisome proliferator-activated receptor-γ agonist. rosiglitazone in a unique murine model of diabetic cardiopathy. Life Sci. 2016, 162, 1–13. [Google Scholar] [CrossRef]
- Gladden, J.D.; Zelickson, B.R.; Guichard, J.L.; Ahmed, M.I.; Yancey, D.M.; Ballinger, S.; Shanmugam, M.; Babu, G.J.; Johnson, M.S.; Darley-Usmar, V.; et al. Xanthine oxidase inhibition preserves left ventricular systolic but not diastolic function in cardiac volume overload. Am. J. Physiol. Heart Circ. Physiol. 2013, 305, H1440–H1450. [Google Scholar] [CrossRef] [PubMed]
- Goltsman, I.; Khoury, E.E.; Aronson, D.; Nativ, O.; Feuerstein, G.Z.; Winaver, J.; Abassi, Z. Rosiglitazone treatment restores renal responsiveness to atrial natriuretic peptide in rats with congestive heart failure. J. Cell. Mol. Med. 2019, 7, 4779–4794. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Garre, D.; González-Rubio, M.L.; Muñoz-Pacheco, P.; Caro-Vadillo, A.; Aragoncillo, P.; Fernández-Cruz, A. Rosuvastatin added to standard heart failure therapy improves cardiac remodelling in heart failure rats with preserved ejection fraction. Eur. J. Heart Fail. 2010, 12, 903–912. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Hurtado, N.; Domínguez-Rodríguez, A.; Mateo, P.; Fernández-Velasco, M.; Val-Blasco, A.; Aizpún, R.; Sabourin, J.; Gómez, A.M.; Benitah, J.P.; Delgado, C. Beneficial effects of leptin treatment in a setting of cardiac dysfunction induced by transverse aortic constriction in mouse. J. Physiol. 2017, 595, 4227–4243. [Google Scholar] [CrossRef] [PubMed]
- Gong, W.; Yan, M.; Chen, J.; Chaugai, S.; Chen, C.; Wang, D. Chronic inhibition of cyclic guanosine monophosphate-specific phosphodiesterase 5 prevented cardiac fibrosis through inhibition of transforming growth factor β-induced Smad signaling. Front. Med. 2014, 8, 445–455. [Google Scholar] [CrossRef]
- Gong, W.; Duan, Q.; Cai, Z.; Chen, C.; Ni, L.; Yan, M.; Wang, X.; Cianflone, K.; Wang, D.W. Chronic inhibition of cGMP-specific phosphodiesterase 5 suppresses endoplasmic reticulum stress in heart failure. Br. J. Pharmacol. 2013, 170, 1396–1409. [Google Scholar] [CrossRef]
- Gonzalez, L.; Novoa, U.; Moya, J.; Gabrielli, L.; Jalil, J.E.; García, L.; Chiong, M.; Lavandero, S.; Ocaranza, M.P. Angiotensin-(1-9) reduces cardiovascular and renal inflammation in experimental renin-independent hypertension. Biochem. Pharmacol. 2018, 156, 357–370. [Google Scholar] [CrossRef] [PubMed]
- Grune, J.; Benz, V.; Brix, S.; Salatzki, J.; Blumrich, A.; Höft, B.; Klopfleisch, R.; Foryst-Ludwig, A.; Kolkhof, P.; Kintscher, U. Steroidal and Nonsteroidal Mineralocorticoid Receptor Antagonists Cause Differential Cardiac Gene Expression in Pressure Overload-induced Cardiac Hypertrophy. J. Cardiovasc. Pharmacol. 2016, 67, 402–411. [Google Scholar] [CrossRef] [PubMed]
- Guan, X.; Guan, X.; Lu, C.; Shang, B.; Zhao, Y.; Meng, Y.; Zhang, Z. Nebivolol combined with tetrahydrobiopterin affects diastolic function in spontaneously hypertensive rats via the nitric oxide/cyclic guanosine monophosphate signalling pathway. BMC Pharmacol. Toxicol. 2020, 21, 84. [Google Scholar] [CrossRef]
- Habibi, J.; Aroor, A.R.; Sowers, J.R.; Jia, G.; Hayden, M.R.; Garro, M.; Barron, B.; Mayoux, E.; Rector, R.S.; Whaley-Connell, A.; et al. Sodium glucose transporter 2 (SGLT2) inhibition with empagliflozin improves cardiac diastolic function in a female rodent model of diabetes. Cardiovasc. Diabetol. 2017, 16, 9. [Google Scholar] [CrossRef]
- Hamdani, N.; Hervent, A.S.; Vandekerckhove, L.; Matheeussen, V.; Demolder, M.; Baerts, L.; De Meester, I.; Linke, W.A.; Paulus, W.J.; De Keulenaer, G.W. Left ventricular diastolic dysfunction and myocardial stiffness in diabetic mice is attenuated by inhibition of dipeptidyl peptidase 4. Cardiovasc. Res. 2014, 104, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Hammoudi, N.; Jeong, D.; Singh, R.; Farhat, A.; Komajda, M.; Mayoux, E.; Hajjar, R.; Lebeche, D. Empagliflozin Improves Left Ventricular Diastolic Dysfunction in a Genetic Model of Type 2 Diabetes. Cardiovasc. Drugs Ther. 2017, 31, 233–246. [Google Scholar] [CrossRef]
- Han, X.; Peng, C.; Huang, L.; Luo, X.; Mao, Q.; Wu, S.; Zhang, H. EGCG prevents pressure overload-induced myocardial remodeling by downregulating overexpression of HDAC5 in mice. Int. J. Mol. Med. 2022, 49, 11. [Google Scholar] [CrossRef] [PubMed]
- Henderson, B.C.; Sen, U.; Reynolds, C.; Moshal, K.S.; Ovechkin, A.; Tyagi, N.; Kartha, G.K.; Rodriguez, W.E.; Tyagi, S.C. Reversal of systemic hypertension-associated cardiac remodeling in chronic pressure overload myocardium by ciglitazone. Int. J. Biol. Sci. 2007, 3, 385–392. [Google Scholar] [CrossRef] [PubMed]
- Horvath, O.; Ordog, K.; Bruszt, K.; Deres, L.; Gallyas, F.; Sumegi, B.; Toth, K.; Halmosi, R. BGP-15 Protects against Heart Failure by Enhanced Mitochondrial Biogenesis and Decreased Fibrotic Remodelling in Spontaneously Hypertensive Rats. Oxid. Med. Cell. Longev. 2021, 2021, 1250858. [Google Scholar] [CrossRef] [PubMed]
- Hou, N.; Mai, Y.; Qiu, X.; Yuan, W.; Li, Y.; Luo, C.; Liu, Y.; Zhang, G.; Zhao, G.; Luo, J.D. Carvacrol Attenuates Diabetic Cardiomyopathy by Modulating the PI3K/AKT/GLUT4 Pathway in Diabetic Mice. Front. Pharmacol. 2019, 10, 998. [Google Scholar] [CrossRef]
- Huang, J.P.; Huang, S.S.; Deng, J.Y.; Chang, C.C.; Day, Y.J.; Hung, L.M. Insulin and resveratrol act synergistically preventing cardiac dysfunction in diabetes, but the advantage of resveratrol in diabetics with acute heart attack is antagonized by insulin. Free Radic. Biol. Med. 2010, 49, 1710–1721. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Wang, W.; Li, L.; Wang, T.; Zhao, Y.; Lin, Y.; Huang, W.; Wang, Y.; Huang, Z. P2X7 Receptor Deficiency Ameliorates STZ-induced Cardiac Damage and Remodeling Through PKCβ and ERK. Front. Cell. Dev. Biol. 2021, 9, 692028. [Google Scholar]
- Huang, Y.; Zhang, K.; Jiang, M.; Ni, J.; Chen, J.; Li, L.; Deng, J.; Zhu, Y.; Mao, J.; Gao, X.; et al. Regulation of energy metabolism by combination therapy attenuates cardiac metabolic remodeling in heart failure. Int. J. Biol. Sci. 2020, 16, 3133–3148. [Google Scholar] [CrossRef]
- Huang, Y.; Zhang, K.; Liu, M.; Su, J.; Qin, X.; Wang, X.; Zhang, J.; Li, S.; Fan, G. An herbal preparation ameliorates heart failure with preserved ejection fraction by alleviating microvascular endothelial inflammation and activating NO-cGMP-PKG pathway. Phytomedicine 2021, 91, 153633. [Google Scholar] [CrossRef]
- Huc, T.; Drapala, A.; Gawrys, M.; Konop, M.; Bielinska, K.; Zaorska, E.; Samborowska, E.; Wyczalkowska-Tomasik, A.; Pączek, L.; Dadlez, M.; et al. Chronic, low-dose TMAO treatment reduces diastolic dysfunction and heart fibrosis in hypertensive rats. Am. J. Physiol. Heart Circ. Physiol. 2018, 315, H1805–H1820. [Google Scholar] [CrossRef]
- Huo, S.; Shi, W.; Ma, H.; Yan, D.; Luo, P.; Guo, J.; Li, C.; Lin, J.; Zhang, C.; Li, S.; et al. Alleviation of Inflammation and Oxidative Stress in Pressure Overload-Induced Cardiac Remodeling and Heart Failure via IL-6/STAT3 Inhibition by Raloxifene. Oxid. Med. Cell. Longev. 2021, 2021, 6699054. [Google Scholar] [CrossRef]
- Ikeda, J.; Kimoto, N.; Kitayama, T.; Kunori, S. Cardiac DPP-4 inhibition by saxagliptin ameliorates isoproterenol-induced myocardial remodeling and cardiac diastolic dysfunction in rats. J. Pharmacol. Sci. 2016, 132, 65–70. [Google Scholar] [CrossRef]
- Jackson, M.R.; Cox, K.D.; Baugh, S.D.P.; Wakeen, L.; Rashad, A.A.; Lam, P.Y.S.; Polyak, B.; Jorns, M.S. Discovery of a first-in-class inhibitor of sulfide:quinone oxidoreductase that protects against adverse cardiac remodelling and heart failure. Cardiovasc. Res. 2022, 118, 1771–1784. [Google Scholar] [CrossRef]
- Jeong, E.M.; Monasky, M.M.; Gu, L.; Taglieri, D.M.; Patel, B.G.; Liu, H.; Wang, Q.; Greener, I.; Dudley, S.C., Jr.; Solaro, R.J. Tetrahydrobiopterin improves diastolic dysfunction by reversing changes in myofilament properties. J. Mol. Cell. Cardiol. 2013, 56, 44–54. [Google Scholar] [CrossRef]
- Jeong, M.Y.; Lin, Y.H.; Wennersten, S.A.; Demos-Davies, K.M.; Cavasin, M.A.; Mahaffey, J.H.; Monzani, V.; Saripalli, C.; Mascagni, P.; Reece, T.B.; et al. Histone deacetylase activity governs diastolic dysfunction through a nongenomic mechanism. Sci. Transl. Med. 2018, 10, eaao0144. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Yang, F.; Ou, D.; Huang, L.; Li, H.; Lang, M. MCC950 ameliorates ventricular arrhythmia vulnerability induced by heart failure. Bioengineered. 2022, 13, 8593–8604. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.A.; West, J.; Maynard, K.B.; Hemnes, A.R. ACE2 improves right ventricular function in a pressure overload model. PLoS ONE 2011, 6, e20828. [Google Scholar] [CrossRef]
- Joubert, M.; Jagu, B.; Montaigne, D.; Marechal, X.; Tesse, A.; Ayer, A.; Dollet, L.; Le May, C.; Toumaniantz, G.; Manrique, A.; et al. The Sodium-Glucose Cotransporter 2 inhibitor Dapagliflozin Prevents Cardiomyopathy in a Diabetic Lipodystrophic Mouse Model. Diabetes 2017, 66, 1030–1040. [Google Scholar] [CrossRef]
- Juric, D.; Wojciechowski, P.; Das, D.K.; Netticadan, T. Prevention of concentric hypertrophy and diastolic impairment in aortic-banded rats treated with resveratrol. Am. J. Physiol. Heart Circ. Physiol. 2007, 292, H2138–H2143. [Google Scholar] [CrossRef] [PubMed]
- Kakehi, K.; Iwanaga, Y.; Watanabe, H.; Sonobe, T.; Akiyama, T.; Shimizu, S.; Yamamoto, H.; Miyazaki, S. Modulation of Sympathetic Activity and Innervation With Chronic Ivabradine and β-Blocker Therapies: Analysis of Hypertensive Rats with Heart Failure. J. Cardiovasc. Pharmacol. Ther. 2019, 24, 387–396. [Google Scholar] [CrossRef] [PubMed]
- Kamiya, M.; Asai, K.; Maejima, Y.; Shirakabe, A.; Murai, K.; Noma, S.; Komiyama, H.; Sato, N.; Mizuno, K.; Shimizu, W. β3-Adrenergic Receptor Agonist Prevents Diastolic Dysfunction in an Angiotensin II-Induced Cardiomyopathy Mouse Model. J. Pharmacol. Exp. Ther. 2021, 376, 473–481. [Google Scholar] [CrossRef] [PubMed]
- Katare, R.G.; Caporali, A.; Oikawa, A.; Meloni, M.; Emanueli, C.; Madeddu, P. Vitamin B1 analog benfotiamine prevents diabetes-induced diastolic dysfunction and heart failure through Akt/Pim-1-mediated survival pathway. Circ. Heart Fail. 2010, 3, 294–305. [Google Scholar] [CrossRef]
- Khong, F.L.; Zhang, Y.; Edgley, A.J.; Qi, W.; Connelly, K.A.; Woodman, O.L.; Krum, H.; Kelly, D.J. 3′,4′-Dihydroxyflavonol antioxidant attenuates diastolic dysfunction and cardiac remodeling in streptozotocin-induced diabetic m(Ren2)27 rats. PLoS ONE 2011, 6, e22777. [Google Scholar] [CrossRef]
- Kim, S.; Yoshiyama, M.; Izumi, Y.; Kawano, H.; Kimoto, M.; Zhan, Y.; Iwao, H. Effects of combination of ACE inhibitor and angiotensin receptor blocker on cardiac remodeling, cardiac function, and survival in rat heart failure. Circulation 2001, 103, 148–154. [Google Scholar] [CrossRef]
- Kim-Mitsuyama, S.; Izumi, Y.; Izumiya, Y.; Yoshida, K.; Yoshiyama, M.; Iwao, H. Additive beneficial effects of the combination of a calcium channel blocker and an angiotensin blocker on a hypertensive rat-heart failure model. Hypertens. Res. 2004, 27, 771–779. [Google Scholar] [CrossRef]
- Lapinskas, T.; Kelle, S.; Grune, J.; Foryst-Ludwig, A.; Meyborg, H.; Jeuthe, S.; Wellnhofer, E.; Elsanhoury, A.; Pieske, B.; Gebker, R.; et al. Serelaxin Improves Regional Myocardial Function in Experimental Heart Failure: An In Vivo Cardiac Magnetic Resonance Study. J. Am. Heart. Assoc. 2020, 9, e013702. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.C.; Shiou, Y.L.; Jhuo, S.J.; Chang, C.Y.; Liu, P.L.; Jhuang, W.J.; Dai, Z.K.; Chen, W.Y.; Chen, Y.F.; Lee, A.S. The sodium-glucose co-transporter 2 inhibitor empagliflozin attenuates cardiac fibrosis and improves ventricular hemodynamics in hypertensive heart failure rats. Cardiovasc. Diabetol. 2019, 18, 45. [Google Scholar] [CrossRef]
- Leite, S.; Moreira-Costa, L.; Cerqueira, R.; Sousa-Mendes, C.; Angélico-Gonçalves, A.; Fontoura, D.; Vasques-Nóvoa, F.; Leite-Moreira, A.F.; Lourenço, A.P. Chronic Sildenafil Therapy in the ZSF1 Obese Rat Model of Metabolic Syndrome and Heart Failure With Preserved Ejection Fraction. J. Cardiovasc. Pharmacol. Ther. 2021, 26, 690–701. [Google Scholar] [CrossRef]
- Li, L.; Luo, W.; Qian, Y.; Zhu, W.; Qian, J.; Li, J.; Jin, Y.; Xu, X.; Liang, G. Luteolin protects against diabetic cardiomyopathy by inhibiting NF-κB-mediated inflammation and activating the Nrf2-mediated antioxidant responses. Phytomedicine 2019, 59, 152774. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Lu, Q.; Qiu, Y.; do Carmo, J.M.; Wang, Z.; da Silva, A.A.; Mouton, A.; Omoto, A.C.M.; Hall, M.E.; Li, J.; et al. Direct Cardiac Actions of the Sodium Glucose Co-Transporter 2 inhibitor Empagliflozin Improve Myocardial Oxidative Phosphorylation and Attenuate Pressure-Overload Heart Failure. J. Am. Heart Assoc. 2021, 10, e018298. [Google Scholar] [CrossRef]
- Li, Z.; Wang, Y.; Jiang, Y.; Ma, D.; Jiang, P.; Zhou, G.; Yang, J.; Dong, F.; Zhao, H.; Zhang, Y.; et al. Xiao-Qing-Long-Tang Maintains Cardiac Function during Heart Failure with Reduced Ejection Fraction in Salt-Sensitive Rats by Regulating the Imbalance of Cardiac Sympathetic Innervation. Evid.-Based Complement. Alternat. Med. 2020, 2020, 9467271. [Google Scholar] [CrossRef] [PubMed]
- Liao, H.H.; Zhang, N.; Feng, H.; Zhang, N.; Ma, Z.G.; Yang, Z.; Yuan, Y.; Bian, Z.Y.; Tang, Q.Z. Oleanolic acid alleviated pressure overload-induced cardiac remodeling. Mol. Cell. Biochem. 2015, 409, 145–154. [Google Scholar] [CrossRef]
- Liao, Y.; Zhao, H.; Ogai, A.; Kato, H.; Asakura, M.; Kim, J.; Asanuma, H.; Minamino, T.; Takashima, S.; Kitakaze, M. Atorvastatin slows the progression of cardiac remodeling in mice with pressure overload and inhibits epidermal growth factor receptor activation. Hypertens. Res. 2008, 31, 335–344. [Google Scholar] [CrossRef]
- Liu, L.; Wang, W.; Meng, X.; Gao, J.; Wu, H.; Wang, P.; Wu, W.; Wang, L.; Ma, L.; Zhang, W. Left ventricular hypertrophy induced by abdominal aortic banding and its prevention by angiotensin receptor blocker telmisartan--a proteomic analysis. J. Physiol. Biochem. 2010, 66, 329–338. [Google Scholar] [CrossRef]
- Liu, L.; Zhao, W.; Liu, J.; Gan, Y.; Liu, L.; Tian, J. Epigallocatechin-3 gallate prevents pressure overload-induced heart failure by up-regulating SERCA2a via histone acetylation modification in mice. PLoS ONE 2018, 13, e0205123. [Google Scholar] [CrossRef]
- Liu, W.; Zi, M.; Tsui, H.; Chowdhury, S.K.; Zeef, L.; Meng, Q.J.; Travis, M.; Prehar, S.; Berry, A.; Hanley, N.A.; et al. A novel immunomodulatory, FTY-720 reverses existing cardiac hypertrophy and fibrosis from pressure overload by targeting NFAT (nuclear factor of activated T-cells) signaling and periostin. Circ. Heart Fail. 2013, 6, 833–844. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.Y.; Liao, H.H.; Feng, H.; Zhang, N.; Yang, J.J.; Li, W.J.; Chen, S.; Deng, W.; Tang, Q.Z. Icariside II attenuates cardiac remodeling via AMPKα2/mTORC1 in vivo and in vitro. J. Pharmacol. Sci. 2018, 138, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Li, S.; Zhang, Z.; Lv, Z.; Jiang, H.; Tan, X.; Liu, F. Effects of valproic acid on sympathetic activity and left ventricularmyocardial remodelling in rats during pressure overload. Turk. J. Med. Sci. 2017, 47, 1651–1660. [Google Scholar] [CrossRef]
- Loch, D.; Chan, V.; Hoey, A.; Brown, L. Rosuvastatin attenuates heart failure and cardiac remodelling in the ageing spontaneously hypertensive rat. Basic Clin. Pharmacol. Toxicol. 2009, 105, 262–270. [Google Scholar] [CrossRef]
- Lou, T.; Ma, J.; Xie, Y.; Yao, G.; Fan, Y.; Ma, S.; Zou, X. Nuanxin capsule enhances cardiac function by inhibiting oxidative stress-induced mitochondrial dependent apoptosis through AMPK/JNK signaling pathway. Biomed. Pharmacother. 2021, 135, 111188. [Google Scholar] [CrossRef]
- Louhelainen, M.; Merasto, S.; Finckenberg, P.; Vahtola, E.; Kaheinen, P.; Leskinen, H.; Levijoki, J.; Pollesello, P.; Haikala, H.; Mervaala, E.M. Effects of calcium sensitizer OR-1986 on a cardiovascular mortality and myocardial remodelling in hypertensive Dahl/Rapp rats. J. Physiol. Pharmacol. 2009, 60, 41–47. [Google Scholar] [PubMed]
- Louhelainen, M.; Vahtola, E.; Kaheinen, P.; Leskinen, H.; Merasto, S.; Kytö, V.; Finckenberg, P.; Colucci, W.S.; Levijoki, J.; Pollesello, P.; et al. Effects of levosimendan on cardiac remodeling and cardiomyocyte apoptosis in hypertensive Dahl/Rapp rats. Br. J. Pharmacol. 2007, 150, 851–861. [Google Scholar] [CrossRef]
- Lovelock, J.D.; Monasky, M.M.; Jeong, E.M.; Lardin, H.A.; Liu, H.; Patel, B.G.; Taglieri, D.M.; Gu, L.; Kumar, P.; Pokhrel, N.; et al. Ranolazine improves cardiac diastolic dysfunction through modulation of myofilament calcium sensitivity. Circ. Res. 2012, 110, 841–850. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.; Pontré, B.; Pickup, S.; Choong, S.Y.; Li, M.; Xu, H.; Gamble, G.D.; Phillips, A.R.; Cowan, B.R.; Young, A.A.; et al. Treatment with a copper-selective chelator causes substantive improvement in cardiac function of diabetic rats with left-ventricular impairment. Cardiovasc. Diabetol. 2013, 12, 28. [Google Scholar] [CrossRef] [PubMed]
- Luk, F.S.; Kim, R.Y.; Li, K.; Ching, D.; Wong, D.K.; Joshi, S.K.; Imhof, I.; Honbo, N.; Hoover, H.; Zhu, B.Q.; et al. Immunosuppression With FTY720 Reverses Cardiac Dysfunction in Hypomorphic ApoE Mice Deficient in SR-BI Expression That Survive Myocardial Infarction Caused by Coronary Atherosclerosis. J. Cardiovasc. Pharmacol. 2016, 67, 47–56. [Google Scholar] [CrossRef]
- Ma, S.; Feng, J.; Lin, X.; Liu, J.; Tang, Y.; Nie, S.; Gong, J.; Wang, L. Nicotinamide Riboside Alleviates Cardiac Dysfunction and Remodeling in Pressure Overload Cardiac Hypertrophy. Oxid. Med. Cell. Longev. 2021, 2021, 5546867. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.L.; Lin, Q.Y.; Wang, L.; Xie, X.; Zhang, Y.L.; Li, H.H. Rituximab prevents and reverses cardiac remodeling by depressing B cell function in mice. Biomed. Pharmacother. 2019, 114, 108804. [Google Scholar] [CrossRef]
- Ma, Y.; Huang, H.; Jiang, J.; Wu, L.; Lin, C.; Tang, A.; Dai, G.; He, J.; Chen, Y. AVE 0991 attenuates cardiac hypertrophy through reducing oxidative stress. Biochem. Biophys. Res. Commun. 2016, 474, 621–625. [Google Scholar] [CrossRef]
- Madonna, R.; Doria, V.; Minnucci, I.; Pucci, A.; Pierdomenico, D.S.; De Caterina, R. Empagliflozin reduces the senescence of cardiac stromal cells and improves cardiac function in a murine model of diabetes. J. Cell. Mol. Med. 2020, 24, 12331–12340. [Google Scholar] [CrossRef]
- Mátyás, C.; Németh, B.T.; Oláh, A.; Török, M.; Ruppert, M.; Kellermayer, D.; Barta, B.A.; Szabó, G.; Kökény, G.; Horváth, E.M.; et al. Prevention of the development of heart failure with preserved ejection fraction by the phosphodiesterase-5A inhibitor vardenafil in rats with type 2 diabetes. Eur. J. Heart Fail. 2017, 19, 326–336. [Google Scholar] [CrossRef] [PubMed]
- Methatham, T.; Tomida, S.; Kimura, N.; Imai, Y.; Aizawa, K. Inhibition of the canonical Wnt signaling pathway by a β-catenin/CBP inhibitor prevents heart failure by ameliorating cardiac hypertrophy and fibrosis. Sci. Rep. 2021, 11, 14886. [Google Scholar] [CrossRef]
- Methawasin, M.; Strom, J.; Borkowski, T.; Hourani, Z.; Runyan, R.; Smith, J.E., 3rd; Granzier, H. Phosphodiesterase 9a Inhibition in Mouse Models of Diastolic Dysfunction. Circ. Heart Fail. 2020, 13, e006609. [Google Scholar] [CrossRef] [PubMed]
- Minhas, K.M.; Saraiva, R.M.; Schuleri, K.H.; Lehrke, S.; Zheng, M.; Saliaris, A.P.; Berry, C.E.; Barouch, L.A.; Vandegaer, K.M.; Li, D.; et al. Xanthine oxidoreductase inhibition causes reverse remodeling in rats with dilated cardiomyopathy. Circ. Res. 2006, 98, 271–279. [Google Scholar] [CrossRef]
- Mishra, M.; Muthuramu, I.; Aboumsallem, J.P.; Kempen, H.; De Geest, B. Reconstituted HDL (Milano) Treatment Efficaciously Reverses Heart Failure with Preserved Ejection Fraction in Mice. Int. J. Mol. Sci. 2018, 19, 3399. [Google Scholar] [CrossRef]
- Mishra, M.; Muthuramu, I.; Kempen, H.; De Geest, B. Administration of apo A-I (Milano) nanoparticles reverses pathological remodelling cardiac dysfunction and heart failure in a murine model of HFpEF associated with hypertension. Sci. Rep. 2020, 10, 8382. [Google Scholar] [CrossRef]
- Morgan, L.A.; Olzinski, A.R.; Upson, J.J.; Zhao, S.; Wang, T.; Eisennagel, S.H.; Hoang, B.; Tunstead, J.R.; Marino, J.P., Jr.; Willette, R.N.; et al. Soluble epoxide hydrolase inhibition does not prevent cardiac remodeling and dysfunction after aortic constriction in rats and mice. J. Cardiovasc. Pharmacol. 2013, 61, 291–301. [Google Scholar] [CrossRef] [PubMed]
- Muñoz-Pacheco, P.; Ortega-Hernández, A.; Caro-Vadillo, A.; Casanueva-Eliceiry, S.; Aragoncillo, P.; Egido, J.; Fernández-Cruz, A.; Gómez-Garre, D. Eplerenone enhances cardioprotective effects of standard heart failure therapy through matricellular proteins in hypertensive heart failure. J. Hypertens. 2013, 31, 2309–2318. [Google Scholar] [CrossRef] [PubMed]
- Naruse, G.; Kanamori, H.; Yoshida, A.; Minatoguchi, S.; Kawaguchi, T.; Iwasa, M.; Yamada, Y.; Mikami, A.; Kawasaki, M.; Nishigaki, K.; et al. The intestine responds to heart failure by enhanced mitochondrial fusion through glucagon-like peptide-1 signalling. Cardiovasc. Res. 2019, 115, 1873–1885. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.D.; Shingu, Y.; Amorim, P.A.; Schenkl, C.; Schwarzer, M.; Doenst, T. GLP-1 Improves Diastolic Function and Survival in Heart Failure with Preserved Ejection Fraction. J. Cardiovasc. Transl. Res. 2018, 11, 259–267. [Google Scholar] [CrossRef]
- Nie, J.; Duan, Q.; He, M.; Li, X.; Wang, B.; Zhou, C.; Wu, L.; Wen, Z.; Chen, C.; Wang, D.W.; et al. Ranolazine prevents pressure overload-induced cardiac hypertrophy and heart failure by restoring aberrant Na+ and Ca2+ handling. J. Cell. Physiol. 2019, 234, 11587–11601. [Google Scholar] [CrossRef]
- Nordén, E.S.; Bendiksen, B.A.; Andresen, H.; Bergo, K.K.; Espe, E.K.; Hasic, A.; Hauge-Iversen, I.M.; Veras, I.; Hussain, R.I.; Sjaastad, I.; et al. Sacubitril/valsartan ameliorates cardiac hypertrophy and preserves diastolic function in cardiac pressure overload. ESC Heart Fail. 2021, 8, 918–927. [Google Scholar] [CrossRef] [PubMed]
- Ohtani, T.; Ohta, M.; Yamamoto, K.; Mano, T.; Sakata, Y.; Nishio, M.; Takeda, Y.; Yoshida, J.; Miwa, T.; Okamoto, M.; et al. Elevated cardiac tissue level of aldosterone and mineralocorticoid receptor in diastolic heart failure: Beneficial effects of mineralocorticoid receptor blocker. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2007, 292, R946–R954. [Google Scholar] [CrossRef] [PubMed]
- Oishi, S.; Suzuki, N.; Hasui, Y.; Homma, T.; Obana, M.; Nagayama, T.; Fujio, Y. Sustained Activation of Guanylate Cyclase-A with TDT a Natriuretic Peptide Derivative Exhibits Cardiorenal Protection in Dahl Salt-Sensitive Hypertensive Rats. J. Pharmacol. Exp. Ther. 2017, 363, 402–410. [Google Scholar] [CrossRef] [PubMed]
- O’Shea, K.M.; Chess, D.J.; Khairallah, R.J.; Hecker, P.A.; Lei, B.; Walsh, K.; Des Rosiers, C.; Stanley, W.C. ω-3 Polyunsaturated fatty acids prevent pressure overload-induced ventricular dilation and decrease in mitochondrial enzymes despite no change in adiponectin. Lipids Health Dis. 2010, 9, 95. [Google Scholar] [CrossRef]
- Park, S.H.; Farooq, M.A.; Gaertner, S.; Bruckert, C.; Qureshi, A.W.; Lee, H.H.; Benrahla, D.; Pollet, B.; Stephan, D.; Ohlmann, P.; et al. Empagliflozin improved systolic blood pressure, endothelial dysfunction and heart remodeling in the metabolic syndrome ZSF1 rat. Cardiovasc. Diabetol. 2020, 19, 19. [Google Scholar] [CrossRef]
- Perlini, S.; Ferrero, I.; Palladini, G.; Tozzi, R.; Gatti, C.; Vezzoli, M.; Cesana, F.; Janetti, M.B.; Clari, F.; Busca, G.; et al. Survival benefits of different antiadrenergic interventions in pressure overload left ventricular hypertrophy/failure. Hypertension 2006, 48, 93–97. [Google Scholar] [CrossRef]
- Plante, E.; Menaouar, A.; Danalache, B.A.; Broderick, T.L.; Jankowski, M.; Gutkowska, J. Treatment with brain natriuretic peptide prevents the development of cardiac dysfunction in obese diabetic db/db mice. Diabetologia 2014, 57, 1257–1267. [Google Scholar] [CrossRef]
- Pozder Geb Gehlken, C.; Rogier van der Velde, A.; Meijers, W.C.; Silljé, H.H.W.; Muntendam, P.; Dokter, M.M.; van Gilst, W.H.; Schols, H.A.; de Boer, R.A. Pectins from various sources inhibit galectin-3-related cardiac fibrosis. Curr. Res. Transl. Med. 2022, 70, 103321. [Google Scholar] [CrossRef]
- Primessnig, U.; Bracic, T.; Levijoki, J.; Otsomaa, L.; Pollesello, P.; Falcke, M.; Pieske, B.; Heinzel, F.R. Long-term effects of Na+/Ca2+ exchanger inhibition with ORM-11035 improves cardiac function and remodelling without lowering blood pressure in a model of heart failure with preserved ejection fraction. Eur. J. Heart Fail. 2019, 21, 1543–1552. [Google Scholar] [CrossRef]
- Qiu, Z.; Zhang, W.; Fan, F.; Li, H.; Wu, C.; Ye, Y.; Du, Q.; Li, Z.; Hu, X.; Zhao, G.; et al. Rosuvastatin-attenuated heart failure in aged spontaneously hypertensive rats via PKCα/β2 signal pathway. J. Cell. Mol. Med. 2012, 16, 3052–3061. [Google Scholar] [CrossRef]
- Randriamboavonjy, J.I.; Loirand, G.; Vaillant, N.; Lauzier, B.; Derbré, S.; Michalet, S.; Pacaud, P.; Tesse, A. Cardiac Protective Effects of Moringa oleifera Seeds in Spontaneous Hypertensive Rats. Am. J. Hypertens. 2016, 29, 873–881. [Google Scholar] [CrossRef]
- Reddy, S.S.; Agarwal, H.; Barthwal, M.K. Cilostazol ameliorates heart failure with preserved ejection fraction and diastolic dysfunction in obese and non-obese hypertensive mice. J. Mol. Cell. Cardiol. 2018, 123, 46–57. [Google Scholar] [CrossRef]
- Richards, D.A.; Aronovitz, M.J.; Liu, P.; Martin, G.L.; Tam, K.; Pande, S.; Karas, R.H.; Bloomfield, D.M.; Mendelsohn, M.E.; Blanton, R.M. CRD-733, a Novel PDE9 (Phosphodiesterase 9) inhibitor, Reverses Pressure Overload-Induced Heart Failure. Circ. Heart Fail. 2021, 14, e007300. [Google Scholar] [CrossRef] [PubMed]
- Rimbaud, S.; Ruiz, M.; Piquereau, J.; Mateo, P.; Fortin, D.; Veksler, V.; Garnier, A.; Ventura-Clapier, R. Resveratrol improves survival, hemodynamics and energetics in a rat model of hypertension leading to heart failure. PLoS ONE 2011, 6, e26391. [Google Scholar] [CrossRef] [PubMed]
- Russell-Hallinan, A.; Neary, R.; Watson, C.J.; Baugh, J.A. Repurposing From Oncology to Cardiology: Low-Dose 5-Azacytidine Attenuates Pathological Cardiac Remodeling in Response to Pressure Overload Injury. J. Cardiovasc. Pharmacol. Ther. 2021, 26, 375–385. [Google Scholar] [CrossRef]
- Salah, E.M.; Bastacky, S.I.; Jackson, E.K.; Tofovic, S.P. Captopril Attenuates Cardiovascular and Renal Disease in a Rat Model of Heart Failure With Preserved Ejection Fraction. J. Cardiovasc. Pharmacol. 2018, 71, 205–214. [Google Scholar] [CrossRef]
- Satoh, S.; Ueda, Y.; Koyanagi, M.; Kadokami, T.; Sugano, M.; Yoshikawa, Y.; Makino, N. Chronic inhibition of Rho kinase blunts the process of left ventricular hypertrophy leading to cardiac contractile dysfunction in hypertension-induced heart failure. J. Mol. Cell. Cardiol. 2003, 35, 59–70. [Google Scholar] [CrossRef] [PubMed]
- Satoh, S.; Ueda, Y.; Suematsu, N.; Oyama, J.; Kadokami, T.; Sugano, M.; Yoshikawa, Y.; Makino, N. Beneficial effects of angiotensin-converting enzyme inhibition on sarcoplasmic reticulum function in the failing heart of the Dahl rat. Circ. J. 2003, 67, 705–711. [Google Scholar] [CrossRef]
- Schauer, A.; Adams, V.; Augstein, A.; Jannasch, A.; Draskowski, R.; Kirchhoff, V.; Goto, K.; Mittag, J.; Galli, R.; Männel, A.; et al. Sacubitril/Valsartan Improves Diastolic Function But Not Skeletal Muscle Function in a Rat Model of HFpEF. Int. J. Mol. Sci. 2021, 22, 3570. [Google Scholar] [CrossRef] [PubMed]
- Seymour, E.M.; Singer, A.A.; Bennink, M.R.; Parikh, R.V.; Kirakosyan, A.; Kaufman, P.B.; Bolling, S.F. Chronic intake of a phytochemical-enriched diet reduces cardiac fibrosis and diastolic dysfunction caused by prolonged salt-sensitive hypertension. J. Gerontol. A Biol. Sci. Med. Sci. 2008, 63, 1034–1042. [Google Scholar] [CrossRef]
- Shang, L.; Weng, X.; Wang, D.; Yue, W.; Mernaugh, R.; Amarnath, V.; Weir, E.K.; Dudley, S.C.; Xu, Y.; Hou, M.; et al. Isolevuglandin scavenger attenuates pressure overload-induced cardiac oxidative stress, cardiac hypertrophy, heart failure and lung remodeling. Free Radic. Biol. Med. 2019, 141, 291–298. [Google Scholar] [CrossRef]
- Shao, S.; Zhang, Y.; Gong, M.; Yang, Q.; Yuan, M.; Yuan, M.; Suo, Y.; Wang, X.; Li, Y.; Bao, Q.; et al. Ivabradine Ameliorates Cardiac Function in Heart Failure with Preserved and Reduced Ejection Fraction via Upregulation of miR-133a. Oxid. Med. Cell. Longev. 2021, 2021, 1257283. [Google Scholar] [CrossRef]
- Shea, C.M.; Price, G.M.; Liu, G.; Sarno, R.; Buys, E.S.; Currie, M.G.; Masferrer, J.L. Soluble guanylate cyclase stimulator praliciguat attenuates inflammation, fibrosis, and end-organ damage in the Dahl model of cardiorenal failure. Am. J. Physiol.-Renal Physiol. 2020, 318, F148–F159. [Google Scholar] [CrossRef]
- Shiraki, A.; Oyama, J.I.; Nishikido, T.; Node, K. GLP-1 analog liraglutide-induced cardiac dysfunction due to energetic starvation in heart failure with non-diabetic dilated cardiomyopathy. Cardiovasc. Diabetol. 2019, 18, 164. [Google Scholar]
- Signore, P.E.; Guo, G.; Wei, Z.; Zhang, W.; Lin, A.; Del Balzo, U. A small-molecule inhibitor of hypoxia-inducible factor prolyl hydroxylase improves obesity, nephropathy and cardiomyopathy in obese ZSF1 rats. PLoS ONE 2021, 16, e0255022. [Google Scholar] [CrossRef]
- Stolina, M.; Luo, X.; Dwyer, D.; Han, C.Y.; Chen, R.; Zhang, Y.; Xiong, Y.; Chen, Y.; Yin, J.; Shkumatov, A.; et al. The evolving systemic biomarker milieu in obese ZSF1 rat model of human cardiometabolic syndrome: Characterization of the model and cardioprotective effect of GDF15. PLoS ONE 2020, 15, e0231234. [Google Scholar] [CrossRef] [PubMed]
- Sukumaran, V.; Tsuchimochi, H.; Sonobe, T.; Waddingham, M.T.; Shirai, M.; Pearson, J.T. Liraglutide treatment improves the coronary microcirculation in insulin resistant Zucker obese rats on a high salt diet. Cardiovasc. Diabetol. 2020, 19, 24. [Google Scholar] [CrossRef] [PubMed]
- Sung, Y.L.; Lin, T.T.; Syu, J.Y.; Hsu, H.J.; Lin, K.Y.; Liu, Y.B.; Lin, S.F. Reverse electromechanical modelling of diastolic dysfunction in spontaneous hypertensive rat after sacubitril/valsartan therapy. ESC Heart Fail. 2020, 7, 4040–4050. [Google Scholar] [CrossRef]
- Tamayo, M.; Martín-Nunes, L.; Val-Blasco, A.; G.M-Piedras, M.J.; Navarro-García, J.A.; Lage, E.; Prieto, P.; Ruiz-Hurtado, G.; Fernández-Velasco, M.; Delgado, C. Beneficial effects of paricalcitol on cardiac dysfunction and remodelling in a model of established heart failure. Br. J. Pharmacol. 2020, 177, 3273–3290. [Google Scholar] [CrossRef] [PubMed]
- Tang, X.; Chen, X.F.; Wang, N.Y.; Wang, X.M.; Liang, S.T.; Zheng, W.; Lu, Y.B.; Zhao, X.; Hao, D.L.; Zhang, Z.Q.; et al. SIRT2 Acts as a Cardioprotective Deacetylase in Pathological Cardiac Hypertrophy. Circulation 2017, 136, 2051–2067. [Google Scholar] [CrossRef] [PubMed]
- Thandapilly, S.J.; Wojciechowski, P.; Behbahani, J.; Louis, X.L.; Yu, L.; Juric, D.; Kopilas, M.A.; Anderson, H.D.; Netticadan, T. Resveratrol prevents the development of pathological cardiac hypertrophy and contractile dysfunction in the SHR without lowering blood pressure. Am. J. Hypertens. 2010, 23, 192–196. [Google Scholar] [CrossRef] [PubMed]
- Thomas, T.A.; Kuzman, J.A.; Anderson, B.E.; Andersen, S.M.; Schlenker, E.H.; Holder, M.S.; Gerdes, A.M. Thyroid hormones induce unique and potentially beneficial changes in cardiac myocyte shape in hypertensive rats near heart failure. Am. J. Physiol. Heart Circ. Physiol. 2005, 288, H2118–H2122. [Google Scholar] [CrossRef]
- Tian, J.; Zhang, M.; Suo, M.; Liu, D.; Wang, X.; Liu, M.; Pan, J.; Jin, T.; An, F. Dapagliflozin alleviates cardiac fibrosis through suppressing EndMT and fibroblast activation via AMPKα/TGF-β/Smad signalling in type 2 diabetic rats. J. Cell. Mol. Med. 2021, 25, 7642–7659. [Google Scholar] [CrossRef]
- Travers, J.G.; Wennersten, S.A.; Peña, B.; Bagchi, R.A.; Smith, H.E.; Hirsch, R.A.; Vanderlinden, L.A.; Lin, Y.H.; Dobrinskikh, E.; Demos-Davies, K.M.; et al. HDAC Inhibition Reverses Preexisting Diastolic Dysfunction and Blocks Covert Extracellular Matrix Remodeling. Circulation 2021, 143, 1874–1890. [Google Scholar] [CrossRef] [PubMed]
- Valero-Munoz, M.; Li, S.; Wilson, R.M.; Boldbaatar, B.; Iglarz, M.; Sam, F. Dual Endothelin-A/Endothelin-B Receptor Blockade and Cardiac Remodeling in Heart Failure With Preserved Ejection Fraction. Circ. Heart Fail. 2016, 9, e003381. [Google Scholar] [CrossRef]
- Venardos, K.; De Jong, K.A.; Elkamie, M.; Connor, T.; McGee, S.L. The PKD inhibitor CID755673 enhances cardiac function in diabetic db/db mice. PLoS ONE 2015, 10, e0120934. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.; Rawat, S.; Ho, K.L.; Wagg, C.S.; Zhang, L.; Teoh, H.; Dyck, J.E.; Uddin, G.M.; Oudit, G.Y.; Mayoux, E. Empagliflozin Increases Cardiac Energy Production in Diabetes: Novel Translational Insights Into the Heart Failure Benefits of SGLT2 inhibitors. JACC Basic Transl. Sci. 2018, 3, 575–587. [Google Scholar] [CrossRef]
- Wang, D.; Luo, Y.; Myakala, K.; Orlicky, D.J.; Dobrinskikh, E.; Wang, X.; Levi, M. Serelaxin improves cardiac and renal function in DOCA-salt hypertensive rats. Sci. Rep. 2017, 7, 9793. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Li, Z.; Wang, Y.; Zhang, J.; Zhao, W.; Fu, M.; Han, X.; Zhou, J.; Ge, J. Qiliqiangxin Enhances Cardiac Glucose Metabolism and Improves Diastolic Function in Spontaneously Hypertensive Rats. Evid.-Based Complement. Alternat. Med. 2017, 2017, 3197320. [Google Scholar] [CrossRef]
- Wang, L.; Halliday, G.; Huot, J.R.; Satoh, T.; Baust, J.J.; Fisher, A.; Cook, T.; Hu, J.; Avolio, T.; Goncharov, D.A.; et al. Treatment With Treprostinil and Metformin Normalizes Hyperglycemia and Improves Cardiac Function in Pulmonary Hypertension Associated With Heart Failure With Preserved Ejection Fraction. Arterioscler. Thromb. Vasc. Biol. 2020, 40, 1543–1558. [Google Scholar] [CrossRef] [PubMed]
- Wei, H.; Qu, H.; Wang, H.; Ji, B.; Ding, Y.; Liu, D.; Duan, Y.; Liang, H.; Peng, C.; Xiao, X. 1,25-Dihydroxyvitamin-D3 prevents the development of diabetic cardiomyopathy in type 1 diabetic rats by enhancing autophagy via inhibiting the β-catenin/TCF4/GSK-3β/mTOR pathway. J. Steroid Biochem. Mol. Biol. 2017, 168, 71–90. [Google Scholar] [CrossRef] [PubMed]
- Westermann, D.; Becher, P.M.; Lindner, D.; Savvatis, K.; Xia, Y.; Fröhlich, M.; Hoffmann, S.; Schultheiss, H.P.; Tschöpe, C. Selective PDE5A inhibition with sildenafil rescues left ventricular dysfunction, inflammatory immune response and cardiac remodeling in angiotensin II-induced heart failure in vivo. Basic Res. Cardiol. 2012, 107, 308. [Google Scholar] [CrossRef]
- Westermann, D.; Riad, A.; Richter, U.; Jäger, S.; Savvatis, K.; Schuchardt, M.; Bergmann, N.; Tölle, M.; Nagorsen, D.; Gotthardt, M.; et al. Enhancement of the endothelial NO synthase attenuates experimental diastolic heart failure. Basic Res. Cardiol. 2009, 104, 499–509. [Google Scholar] [CrossRef] [PubMed]
- Westermann, D.; Rutschow, S.; Jäger, S.; Linderer, A.; Anker, S.; Riad, A.; Unger, T.; Schultheiss, H.P.; Pauschinger, M.; Tschöpe, C. Contributions of inflammation and cardiac matrix metalloproteinase activity to cardiac failure in diabetic cardiomyopathy: The role of angiotensin type 1 receptor antagonism. Diabetes 2007, 56, 641–646. [Google Scholar] [CrossRef]
- Wilck, N.; Markó, L.; Balogh, A.; Kräker, K.; Herse, F.; Bartolomaeus, H.; Szijártó, I.A.; Gollasch, M.; Reichhart, N.; Strauss, O.; et al. Nitric oxide-sensitive guanylyl cyclase stimulation improves experimental heart failure with preserved ejection fraction. JCI Insight 2018, 3, e96006. [Google Scholar] [CrossRef]
- Williams, S.; Pourrier, M.; McAfee, D.; Lin, S.; Fedida, D. Ranolazine improves diastolic function in spontaneously hypertensive rats. Am. J. Physiol. Heart Circ. Physiol. 2014, 306, H867–H881. [Google Scholar] [CrossRef] [PubMed]
- Wu, B.; Lin, J.; Luo, J.; Han, D.; Fan, M.; Guo, T.; Tao, L.; Yuan, M.; Yi, F. Dihydromyricetin Protects against Diabetic Cardiomyopathy in Streptozotocin-Induced Diabetic Mice. BioMed Res. Int. 2017, 2017, 3764370. [Google Scholar] [CrossRef]
- Wu, F.; Qiu, Y.; Ye, G.; Luo, H.; Jiang, J.; Yu, F.; Zhou, W.; Zhang, S.; Feng, J. Treatment with hydrogen molecule attenuates cardiac dysfunction in streptozotocin-induced diabetic mice. Cardiovasc. Pathol. 2015, 24, 294–303. [Google Scholar] [CrossRef]
- Wu, L.; Mei, L.; Chong, L.; Huang, Y.; Li, Y.; Chu, M.; Yang, X. Olmesartan ameliorates pressure overload-induced cardiac remodeling through inhibition of TAK1/p38 signaling in mice. Life Sci. 2016, 145, 121–126. [Google Scholar] [CrossRef]
- Wu, X.; Zhang, T.; Lyu, P.; Chen, M.; Ni, G.; Cheng, H.; Xu, G.; Li, X.; Wang, L.; Shang, H. Traditional Chinese Medication Qiliqiangxin Attenuates Diabetic Cardiomyopathy via Activating PPARγ. Front. Cardiovasc. Med. 2021, 8, 698056. [Google Scholar] [CrossRef]
- Xiao, L.; Gu, Y.; Gao, L.; Shangguan, J.; Chen, Y.; Zhang, Y.; Li, L. Sanggenon C protects against pressure overload-induced cardiac hypertrophy via the calcineurin/NFAT2 pathway. Mol. Med. Rep. 2017, 16, 5338–5346. [Google Scholar] [CrossRef]
- Xiao, Y.; Yang, Z.; Wu, Q.Q.; Jiang, X.H.; Yuan, Y.; Chang, W.; Bian, Z.Y.; Zhu, J.X.; Tang, Q.Z. Cucurbitacin B Protects Against Pressure Overload Induced Cardiac Hypertrophy. J. Cell. Biochem. 2017, 118, 3899–3910. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.N.; Kong, L.H.; Ding, P.; Liu, Y.; Fan, Z.G.; Gao, E.H.; Yang, J.; Yang, L.F. Melatonin ameliorates pressure overload-induced cardiac hypertrophy by attenuating Atg5-dependent autophagy and activating the Akt/mTOR pathway. Biochim. Biophys. Acta Mol. Basis Dis. 2020, 1866, 165848. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Hu, X.; Lu, Z.; Zhang, P.; Zhao, L.; Wessale, J.L.; Bache, R.J.; Chen, Y. Xanthine oxidase inhibition with febuxostat attenuates systolic overload-induced left ventricular hypertrophy and dysfunction in mice. J. Card. Fail. 2008, 14, 746–753. [Google Scholar] [CrossRef]
- Xu, X.; Zhang, L.; Liang, J. Rosuvastatin prevents pressure overload-induced myocardial hypertrophy via inactivation of the Akt, ERK1/2 and GATA4 signaling pathways in rats. Mol. Med. Rep. 2013, 8, 385–392. [Google Scholar] [CrossRef]
- Xu, X.; Zhao, L.; Hu, X.; Zhang, P.; Wessale, J.; Bache, R.; Chen, Y. Delayed treatment effects of xanthine oxidase inhibition on systolic overload-induced left ventricular hypertrophy and dysfunction. Nucleosides Nucleotides Nucleic Acids 2010, 29, 306–313. [Google Scholar] [CrossRef] [PubMed]
- Xue, M.; Li, T.; Wang, Y.; Chang, Y.; Cheng, Y.; Lu, Y.; Liu, X.; Xu, L.; Li, X.; Yu, X.; et al. Empagliflozin prevents cardiomyopathy via sGC-cGMP-PKG pathway in type 2 diabetes mice. Clin. Sci. 2019, 133, 1705–1720. [Google Scholar] [CrossRef]
- Yamamoto, M.; Ishizu, T.; Seo, Y.; Suto, Y.; Sai, S.; Xu, D.; Murakoshi, N.; Kimura, T.; Kawakami, Y.; Aonuma, K. Teneligliptin Prevents Cardiomyocyte Hypertrophy, Fibrosis and Development of Hypertensive Heart Failure in Dahl Salt-Sensitive Rats. J. Card. Fail. 2018, 24, 53–60. [Google Scholar] [CrossRef]
- Yan, P.; Mao, W.; Jin, L.; Fang, M.; Liu, X.; Lang, J.; Jin, L.; Cao, B.; Shou, Q.; Fu, H. Crude Radix Aconiti Lateralis Preparata (Fuzi) with Glycyrrhiza Reduces Inflammation and Ventricular Remodeling in Mice through the TLR4/NF-κB Pathway. Mediators Inflamm. 2020, 2020, 5270508. [Google Scholar] [CrossRef]
- Yan, X.; Zhang, Y.L.; Zhang, L.; Zou, L.X.; Chen, C.; Liu, Y.; Xia, Y.L.; Li, H.H. Gallic Acid Suppresses Cardiac Hypertrophic Remodeling and Heart Failure. Mol. Nutr. Food Res. 2019, 63, e1800807. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Wu, Q.Q.; Liu, Y.; Hu, Z.F.; Bian, Z.Y.; Tang, Q.Z. Cinnamaldehyde attenuates pressure overload-induced cardiac hypertrophy. Int. J. Clin. Exp. Pathol. 2015, 8, 14345–14354. [Google Scholar] [PubMed]
- Yin, J.; Kukucka, M.; Hoffmann, J.; Sterner-Kock, A.; Burhenne, J.; Haefeli, W.E.; Kuppe, H.; Kuebler, W.M. Sildenafil preserves lung endothelial function and prevents pulmonary vascular remodeling in a rat model of diastolic heart failure. Circ. Heart Fail. 2011, 4, 198–206. [Google Scholar] [CrossRef]
- Youcef, G.; Olivier, A.; Nicot, N.; Muller, A.; Deng, C.; Labat, C.; Fay, R.; Rodriguez-Guéant, R.M.; Leroy, C.; Jaisser, F.; et al. Preventive and chronic mineralocorticoid receptor antagonism is highly beneficial in obese SHHF rats. Br. J. Pharmacol. 2016, 173, 1805–1819. [Google Scholar] [CrossRef]
- Yu, J.; Chen, R.; Tan, Y.; Wu, J.; Qi, J.; Zhang, M.; Gu, W. Salvianolic Acid B Alleviates Heart Failure by Inactivating ERK1/2/GATA4 Signaling Pathway after Pressure Overload in Mice. PLoS ONE 2016, 11, e0166560. [Google Scholar] [CrossRef]
- Yuan, X.; Xiao, Y.C.; Zhang, G.P.; Hou, N.; Wu, X.Q.; Chen, W.L.; Luo, J.D.; Zhang, G.S. Chloroquine improves left ventricle diastolic function in streptozotocin-induced diabetic mice. Drug. Des. Devel. Ther. 2016, 10, 2729–2737. [Google Scholar]
- Yuan, Y.; Zong, J.; Zhou, H.; Bian, Z.Y.; Deng, W.; Dai, J.; Gan, H.W.; Yang, Z.; Li, H.; Tang, Q.Z. Puerarin attenuates pressure overload-induced cardiac hypertrophy. J. Cardiol. 2014, 63, 73–81. [Google Scholar] [CrossRef]
- Zhang, B.; Zhang, J.; Zhang, C.; Zhang, X.; Ye, J.; Kuang, S.; Sun, G.; Sun, X. Notoginsenoside R1 Protects Against Diabetic Cardiomyopathy Through Activating Estrogen Receptor α and Its Downstream Signaling. Front. Pharmacol. 2018, 9, 1227. [Google Scholar] [CrossRef]
- Zhang, N.; Yang, Z.; Xiang, S.Z.; Jin, Y.G.; Wei, W.Y.; Bian, Z.Y.; Deng, W.; Tang, Q.Z. Nobiletin attenuates cardiac dysfunction, oxidative stress and inflammatory in streptozotocin: Induced diabetic cardiomyopathy. Mol. Cell. Biochem. 2016, 417, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.W.; Bai, F.; Wang, J.; Zheng, R.H.; Yang, L.W.; James, E.A.; Zhao, Z.Q. Edaravone inhibits pressure overload-induced cardiac fibrosis and dysfunction by reducing expression of angiotensin II AT1 receptor. Drug. Des. Devel. Ther. 2017, 11, 3019–3033. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Edgley, A.J.; Cox, A.J.; Powell, A.K.; Wang, B.; Kompa, A.R.; Stapleton, D.I.; Zammit, S.C.; Williams, S.J.; Krum, H.; et al. FT011, a new anti-fibrotic drug, attenuates fibrosis and chronic heart failure in experimental diabetic cardiomyopathy. Eur. J. Heart Fail. 2012, 14, 549–562. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Lin, X.; Chu, Y.; Chen, X.; Du, H.; Zhang, H.; Xu, C.; Xie, H.; Ruan, Q.; Lin, J.; et al. Dapagliflozin: A sodium-glucose cotransporter 2 inhibitor, attenuates angiotensin II-induced cardiac fibrotic remodeling by regulating TGFβ1/Smad signaling. Cardiovasc. Diabetol. 2021, 20, 121. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.; Liao, Y.; Minamino, T.; Asano, Y.; Asakura, M.; Kim, J.; Asanuma, H.; Takashima, S.; Hori, M.; Kitakaze, M. Inhibition of cardiac remodeling by pravastatin is associated with amelioration of endoplasmic reticulum stress. Hypertens. Res. 2008, 31, 1977–1987. [Google Scholar] [CrossRef]
- Zhao, M.; Zhang, J.; Xu, Y.; Liu, J.; Ye, J.; Wang, Z.; Ye, D.; Feng, Y.; Xu, S.; Pan, W.; et al. Selective Inhibition of NLRP3 Inflammasome Reverses Pressure Overload-Induced Pathological Cardiac Remodeling by Attenuating Hypertrophy, Fibrosis and Inflammation. Int. Immunopharmacol. 2021, 99, 108046. [Google Scholar] [CrossRef] [PubMed]
- Zhao, T.; Chen, H.; Xu, F.; Wang, J.; Liu, Y.; Xing, X.; Guo, L.; Zhang, M.; Lu, Q. Liraglutide alleviates cardiac fibrosis through inhibiting P4hα-1 expression in STZ-induced diabetic cardiomyopathy. Acta Biochim. Biophys. Sin. 2019, 51, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Zhao, T.; Kee, H.J.; Kee, S.J.; Jeong, M.H. Hdac8 inhibitor Alleviates Transverse Aortic Constriction-Induced Heart Failure in Mice by Downregulating Ace1. Oxid. Med. Cell. Longev. 2022, 2022, 6227330. [Google Scholar] [CrossRef]
- Zhao, Y.; Wang, C.; Wang, C.; Hong, X.; Miao, J.; Liao, Y.; Zhou, L.; Liu, Y. An essential role for Wnt/β-catenin signaling in mediating hypertensive heart disease. Sci. Rep. 2018, 8, 8996. [Google Scholar] [CrossRef]
- Zhao, Z.; Liu, H.; Li, Y.; Tian, J.; Deng, S. Wnt-C59 Attenuates Pressure Overload-Induced Cardiac Hypertrophy via Interruption of Wnt Pathway. Med. Sci. Monit. 2020, 26, e923025. [Google Scholar] [CrossRef]
- Zheng, H.; Pu, S.Y.; Fan, X.F.; Li, X.S.; Zhang, Y.; Yuan, J.; Zhang, Y.F.; Yang, J.L. Treatment with angiotensin-(1-9) alleviates the cardiomyopathy in streptozotocin-induced diabetic rats. Biochem. Pharmacol. 2015, 95, 38–45. [Google Scholar] [CrossRef]
- Zheng, R.H.; Bai, X.J.; Zhang, W.W.; Wang, J.; Bai, F.; Yan, C.P.; James, E.A.; Bose, H.S.; Wang, N.P.; Zhao, Z.Q. Liraglutide attenuates cardiac remodeling and improves heart function after abdominal aortic constriction through blocking angiotensin II type 1 receptor in rats. Drug Des. Devel. Ther. 2019, 13, 2745–2757. [Google Scholar] [CrossRef]
- Zhou, G.F.; Jiang, Y.H.; Ma, D.F.; Wang, Y.C.; Yang, J.L.; Chen, J.Y.; Chi, C.Y.; Han, X.W.; Li, Z.Y.; Li, X. Xiao-Qing-Long Tang Prevents Cardiomyocyte Hypertrophy, Fibrosis and the Development of Heart Failure with Preserved Ejection Faction in Rats by Modulating the Composition of the Gut Microbiota. BioMed Res. Int. 2019, 2019, 9637479. [Google Scholar] [CrossRef]
- Zuo, G.; Ren, X.; Qian, X.; Ye, P.; Luo, J.; Gao, X.; Zhang, J.; Chen, S. Inhibition of JNK and p38 MAPK-mediated inflammation and apoptosis by ivabrfoisadine improves cardiac function in streptozotocin-induced diabetic cardiomyopathy. J. Cell. Physiol. 2019, 234, 1925–1936. [Google Scholar] [CrossRef]
- Hooijmans, C.R.; Rovers, M.M.; de Vries, R.B.; Leenaars, M.; Ritskes-Hoitinga, M.; Langendam, M.W. SYRCLE’s risk of bias tool for animal studies. BMC Med. Res. Methodol. 2014, 14, 43. [Google Scholar] [CrossRef]
- Seferović, P.M.; Coats, A.; Ponikowski, P.; Filippatos, G.; Huelsmann, M.; Jhund, P.S.; Polovina, M.M.; Komajda, M.; Seferović, J.; Sari, I.; et al. European Society of Cardiology/Heart Failure Association position paper on the role and safety of new glucose-lowering drugs in patients with heart failure. Eur. J. Heart Fail. 2020, 22, 196–213. [Google Scholar] [CrossRef] [PubMed]
- Tofovic, S.P.; Kusaka, H.; Kost, C.K., Jr.; Bastacky, S. Renal function and structure in diabetic, hypertensive, obese ZDFxSHHF-hybrid rats. Ren. Fail. 2000, 22, 387–406. [Google Scholar] [CrossRef]
- Roh, J.; Rhee, J.; Chaudhari, V.; Rosenzweig, A. The Role of Exercise in Cardiac Aging: From Physiology to Molecular Mechanisms. Circ. Res. 2016, 118, 279–295. [Google Scholar] [CrossRef] [PubMed]
- Jasińska-Stroschein, M. Training programs in preclinical studies. The example of pulmonary hypertension. Systematic review and meta-analysis. PLoS ONE 2022, 17, e0276875. [Google Scholar] [CrossRef] [PubMed]
- Halliday, B.P.; Senior, R.; Pennell, D.J. Assessing left ventricular systolic function: From ejection fraction to strain analysis. Eur. Heart J. 2021, 42, 789–797. [Google Scholar] [CrossRef]
- Roh, J.; Houstis, N.; Rosenzweig, A. Why Don’t We Have Proven Treatments for HFpEF? Circ. Res. 2017, 120, 1243–1245. [Google Scholar] [CrossRef]
- Ciccarelli, M.; Dawson, D.; Falcao-Pires, I.; Giacca, M.; Hamdani, N.; Heymans, S.; Hooghiemstra, A.; Leeuwis, A.; Hermkens, D.; Tocchetti, C.G.; et al. Reciprocal organ interactions during heart failure: A position paper from the ESC Working Group on Myocardial Function. Cardiovasc. Res. 2021, 117, 2416–2433. [Google Scholar] [CrossRef]
- Withaar, C.; Lam, C.S.P.; Schiattarella, G.G.; de Boer, R.A.; Meems, L.M.G. Heart failure with preserved ejection fraction in humans and mice: Embracing clinical complexity in mouse models. Eur. Heart J. 2021, 42, 4420–4430. [Google Scholar] [CrossRef] [PubMed]



| Pharmacologic Class/Therapeutic Group | Active Substance | Species | Animal Model * | Systolic Function | Diastolic Function | LVH | LVEDd | Fibrosis | Pulmonary Edema/Lung Congestion | Other Parameters | Refs | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Active Relaxation | Passive Stiffness (LVEDP, Diastolic Stiff) | Hemodynamics, Renal Function, Exercise | Biochemical Markers | ||||||||||
| ACE inhibitor | Captopril, Benazepril, Temocapril | rat | Dahl salt sensitive, ZSF1 Obese | ↔LVEF [%]; ↑dP/dtmax | ↑E/A; ↑dP/dtmin | ↓ | ↔ | ↓ | ↓SBP; ↑Ccr | ↓NT-proBNP | [17,85,137,138] | ||
| AT1 receptor antagonist (ARB) | Irbesartan, Losartan, Olmesartan, Telmisartan, Valsartan | mouse/ rat | Ang II, Dahl salt sensitive, pressure-overload by AAB (TAC), SHR, STZ, ZSF1 Obese | ↑LVEF [%]; ↑LVSP | ↑dP/dtmin | ↔ | ↓ | ↔ | ↓ | ↓SBP; ↓Cr | ↓NT-proBNP (BNP); ↓Infl; ↑MF; ↓FA; ↓Apoptosis | [15,17,21,30,70,85,86,96,149,160,164,170,197,200] | |
| Beta-blocker (BB) | Bisoprolol, BRL 37,344, Metoprolol, Nebivolol, Propranolol | mouse/ rat | Ang II, Dahl salt sensitive, pressure-overload by AAB (TAC) | ↑LVEF [%] | ↑E/A; ↑tau | ↓ | ↓p = 0.0957 | ↓ | ↓ p = 0.0792 | ↓SBP; ↑Cr | [59,81,82,127] | ||
| MR antagonist (MRA) | Eplerenone, Finerenone, Spironolactone | mouse/ rat | Dahl salt sensitive, pressure overload by TAC, SHR, SHHF aged, SHHF cp/cp obese | ↑LVEF [%] | ↑E/A | ↓ | ↔ | ↓ | ↓ | ↓BNP; ↓Infl | [28,58,118,123,184] | ||
| NEP inhibitor/AT1 receptor antagonist (ARNI) | Sacubitril/Valsartan | mouse/ rat | Pressure-overload by AB (TAC), SHR, ZSF1 Obese | ↑LVEF [%] | ↓ | ↓ | ↓ | ↓ | ↓ | ↑Endothelium | [24,122,140,149] | ||
| Biguanide | Metformin | mouse/ rat | Ang II, db/db, pressure overload by ACF, STZ + HFD | ↑LVEF [%] | ↑tau | ↔ | ↓ | ↓ | ↓ | ↓ p = 0.0776 | ↓GLU; ↓Apoptosis | [20,151,154,188] | |
| DPP-4 inhibitor | Saxagliptin, Sitagliptin, Teneligliptin | mouse/rat/ | Dahl salt sensitive, db/db, Isoproterenol-induced HF | ↑LVEF [%]; ↑dP/dtmax; ↔LVSP | ↑E/A; ↑dP/dtmin ↑tau | ↓ | ↓ | ↔ | ↓ | ↓ | ↓Infl; ↓OX; ↑Endothelium | [45,61,73,179] | |
| GLP-1 receptor agonist | Exendin-4, GLP-1, Liraglutide | rat/ hamster | Dahl salt sensitive, pressure-overload by AAB, STZ, Zucker fatty rat | ↑LVEF [%]; ↑LVSP | ↑E/A p = 0.073 | ↓ | ↓ | ↓ | ↔ | ↔ | ↓Infl; ↓OX; ↓NT-proBNP; ↓Apoptosis | [18,119,120,145,148,196,200] | |
| PPAR-gamma agonist | Ciglitazone, Pioglitazone, Rosiglita-zone | mouse/ rat | Pressure-overload by AAB (ACF), ZDF + TAC | ↔LVEF [%]; ↔LVSP; ↑ dP/dtmax p = 0.06 | ↔ | ↓ | ↓ | ↓SBP | ↑Endothelium | [50,52,64,79] | |||
| SGLT-2 inhibitor | Dapagliflozin, Empagliflozin | mouse/ rat | Ang II, Dahl salt sensitive, db/db (ob/ob), L-Name + HFD, pressure-overload by TAC, SHHF, SHR, STZ (+HFD), ZSF1 Obese | ↑LVEF [%] | ↑dP/dtmin | ↔ | ↓ | ↔ | ↓ | ↔ | ↓SBP; ↑Exercise | ↑Endothelium; ↓OX;↓Infl; ↑GLU; ↓BNP | [10,16,25,27,60,62,69,79,88,91,110,126,154,158,178,191] |
| Calcium sensitizer | Levosi mendan, OR-1986 | rat | Dahl salt sensitive | ↑LVEF [%] | ↔ | ↓ | ↓SBP | ↓BNP; ↓Apoptosis | [21,102,103] | ||||
| HMGR inhibitor | Atorvastatin, Pravastatin, Rosuvastatin | mouse/ rat | Dahl salt sensitive, pressure overload by AAB (TAC), SHHF, SHR | ↑LVEF [%]; ↔LVSP; ↑dP/dtmax | ↓ | ↓ | ↓ | ↔ | ↓ | ↓Infl; ↑Endothelium; ↓OX; ↓Apoptosis; ↓NT-proBNP | [12,31,54,94,100,131,193] | ||
| I(f) current inhibitor | Ivabradin | mouse/ rat | Dahl salt sensitive, pressure overload by TAC | ↑LVEF [%] | ↑dP/dtmin | ↓ | ↓ p = 0.052 | ↓ | ↔ | ↓ | ↓Infl; ↓Apoptosis | [73,135,194] | |
| Immunomodulators | 5-azacytidine, Carvacrol, FTY-720, ITF2357/Givinostat, MCC950, PCI34051, Rituximab | mouse | Dahl salt sensi-tive, db/db + STZ, DOCA salt, TAC | ↑LVEF [%] | ↑dP/dtmin | ↓ | ↓ | ↓ | ↓BNP; ↓Infl | [66,76,97,108,136,155,194,196] | |||
| PDE3-i, PDE5-i, PDE9-i | Cilostazol, Sildenafil, Vardenafil, PF-4449613, CRD-733 | mouse/ rat | Ang II(+HFD), db/db, DOCA salt (+TAC), ISO + TAC, pressure overload by TAC, ZSF1, ZDF | ↔LVEF [%]; ↑dP/dtmax | ↓ | ↔ | ↓ | ↓ p = 0.0786 | ↑Exercise | ↓OX; ↓Apoptosis; ↓Infl | [55,56,89,111,113,133,134,163,183] | ||
| Plant-derivatives | See below # | mouse/ rat | Dahl salt sensitive, pressure overload by AAB (TAC), db/db (+STZ), L-Name + HFD, SHHF, SHR, STZ | ↑LVEF [%]; ↔LVSP | ↑dP/dtmin | ↓ | ↓ | ↓ | ↓ | ↓Apoptosis; ↑Endothelium; ↑MF; ↓OX | [13,32,33,34,35,36,49,67,80,84,92,98,101,135,152,171,173,180,181,182,185,188,201] | ||
| XO inhibitor | Allopurinol, Febuxostat, Oxypurinol | mouse/ rat | Pressure overload by ACF (TAC) | ↔LVEF [%] | ↓ | ↓ | ↓OX | [51,114,175,176] | |||||
| Pharmacologic Class/Therapeutic Group | Active Substance | Animal Model * | Effect | Diff in Means (95%CI) | Comparison ** | Arrhythmia; Mortality [Refs] |
|---|---|---|---|---|---|---|
| ACE inhibitor | Captopril, Benazepril, Temocapril | Dahl salt sensitive | ↔ | 4.28 (−5.39; 13.96); NS | - | |
| AT1 receptor antagonist (ARB) | Irbesartan, Losartan, Olmesartan, Telmisartan, Valsartan | Ang II | ↑ | 3.00 (0.52; 5.48); p < 0.0001 | Q = 126.88; df = 5; p < 0.0001 | |
| Dahl salt sensitive | ↔ | −1.52 (−4.24; 1.18); NS | ↓M [21,86] | |||
| Pressure−overload by AAB (TAC) | ↑ | 12.72 (7.86; 17.58); p < 0.0001 | ||||
| SHR | ↔ | 1.01 (−2.86; 4.87); NS | ||||
| STZ | ↓ | −6.70 (−9.44; −3.95); p < 0.0001 | ||||
| ZSF1 Obese | ↑ | 11.00 (8.76; 13.23); p < 0.0001 | ||||
| Beta-blocker (BB) | Bisoprolol, BRL 37344, Metoprolol, Nebivolol, Propranolol | Ang II | ↑ | 9.9 (8.23; 11.57); p < 0.0001 | Q = 76.04; df = 2; p < 0.0001 | |
| Dahl salt sensitive | ↔ | 5.79 (−0.75; 21.94); NS | ↓M [81,127] | |||
| Pressure-overload by AAB (TAC) | ↔ | 1.00 (−0.13; 2.13); NS | ||||
| MR antagonist (MRA) | Eplerenone, Finerenone, Spironolacto ne | Dahl salt sensitive | ↔ | −2.45 (−5.49; 0.59); NS | Q = 24.96; df = 2; p < 0.0001 | |
| SHR | ↑ | 2.00 (1.43; 2.57); p < 0.0001 | ||||
| SHHF aged (cp/cp obese) | ↑ | 10.15 (6.25; 14.06); p < 0.0001 | ↓M [183] | |||
| NEP inhibitor/AT1 receptor antagonist (ARNI) | Sacubitril/Valsartan | Pressure-overload by AB (TAC) | ↔ | 10.50 (−8.12; 29.12); NS | Q = 4.10; df = 2; NS | ↓M [24] |
| SHR | ↔ | −1.00 (−9.16; 7.16); NS | ↓A [149] | |||
| ZSF1 Obese | ↑ | 8.48 (3.79; 13.18); p = 0.0004 | ||||
| Biguanide | Metformin | Ang II inf | ↑ | 10.00 (7.27; 12.72); p < 0.0001 | Q = 136.59; df = 3; p < 0.0001 | |
| db/db | ↑ | 15.00 (13.04; 16.96); p < 0.0001 | ||||
| Pressure overload by ACF | ↑ | 6.2 (3.25; 9.15); p < 0.0001 | ||||
| STZ + HFD | ↑ | 26.00 (23.74; 28.26); p < 0.0001 | ||||
| DPP-4 inhibitor | Saxagliptin, Sitagliptin, Teneligliptin | Dahl salt sensitive | ↔ | −0.95 (−2.73; 0.83); NS | Q = 353.67; df = 2; p < 0.0001 | ↓M [45] |
| db/db | ↑ | 19.9 (14.05; 25.75); p < 0.0001 | ||||
| Isoproterenol-induced HF | ↑ | 18.7 (17.66; 19.74); p < 0.0001 | ||||
| GLP-1 receptor agonist | Exendin-4, GLP-1, Liraglutide | Dahl salt sensitive | ↔ | 0.01 (−1.76; 1.75); NS | Q = 21.24; df = 3; p < 0.0001 | ↔M [119] |
| Pressure-overload by AAB | ↔ | 7.08 (−2.32; 16.49); NS | ↓M [120] | |||
| STZ | ↑ | 5.32 (3.57; 7.07); p < 0.0001 | ↓A [195] | |||
| Zucker fatty rat | ↔ | 1.13 (−0.35; 2.61); NS | ||||
| PPAR-gamma agonist | Ciglitazone, Pioglitazone, Rosiglitazone | Pressure-overload by AAB (ACF) | ↔ | 9.18 (−4.53; 22.90); NS | Q = 1.48; df = 1; NS | |
| ZDF + TAC | ↔ | −0.22 (−6.69; 6.24); NS | ||||
| SGLT-2 inhibitor | Dapagliflozin, Empagliflozin | Ang II | ↓ | −2.98 (−4.69; −1.27); p = 0.0007 | Q = 1013.1; df = 8; p < 0.0001 | |
| Dahl salt sensitive | ↔ | −0.57 (−1.75; 0.60); NS | ||||
| db/db (ob/ob) | ↑ | 5.83 (0.01; 11.67); p = 0.049 | ||||
| L−Name + HFD | ↓ | −2.00 (−3.95; −0.04); p = 0.045 | ||||
| Pressure-overload by TAC | ↑ | 7.92 (3.73; 15.23); p = 0.035 | ↓M [91] | |||
| SHHF | ↔ | 0.01 (−2.27; 2.27): NS | ||||
| SHR | ↔ | −1.00 (−4.99; 2.99): NS | ||||
| STZ (+HFD) | ↑ | 13.19 (2.02; 24.37); p = 0.03 | ||||
| ZSF1 Obese | ↔ | 5.00 (−6.31; 16.32); NS | ||||
| Calcium sensitizer | Levosime ndan, OR-1986 | Dahl salt sensitive | ↑ | 7.58 (5.46; 9.70); p < 0.0001 | - | ↓M [102,103] |
| I(f) current inhibitor | Ivabradin | Dahl salt sensitive | ↑ | 15.9 (9.31; 22.49); p < 0.0001 | Q = 9.18; df = 1; p = 0.002 | ↓M [21,81] |
| Pressure overload by TAC | ↔ | 2.4 (−3.32; 8.13); NS | ||||
| Immunomodulators | FTY-720, MCC950 | Pressure overload by TAC | ↔ | 21.66 (−1.49; 44.81); p = 0.06 | - | [97,194] |
| HMGR inhibitor | Atorvastatin, Pravastatin, Rosuvastatin | Dahl salt sensitive | ↔ | −1.00 (−7.03; 5.03); NS | Q = 32.28; df = 3; p < 0.0001 | |
| Pressure overload by AAB (TAC) | ↑ | 18.82 (14.53; 23.10); p < 0.0001 | ||||
| SHHF | ↔ | 4.00 (−2.93; 10.93); NS | ||||
| SHR | ↔ | 7.67 (−0.08; 15.43); NS | ||||
| PDE3-i, PDE5-i, PDE9-i | Cilostazol, CRD-733, PF-4449613, Sildenafil, Vardenafil, | Ang II inf (+HFD) | ↔ | 1.00 (−2.73; 4.73); NS | Q = 65.22; df = 5; p < 0.0001 | |
| DOCA salt (+TAC) | ↓ | −8.5 (−11.44; −5.56): p < 0.0001 | ||||
| ISO + TAC | ↑ | 10.32 (6.74; 13.91): p < 0.0001 | ||||
| Pressure overload by TAC | ↔ | 6.40 (−14.87; 27.67); NS | ||||
| ZDF | ↔ | −2.00 (−5.14; 1.14): NS | ||||
| ZSF1 Obese | ↔ | 0.01 (−7.07; 7.06): NS | ||||
| Plant-derivatives | As listed below# | Dahl salt sensitive | ↑ | 9.28 (4.60; 13.96); p < 0.0001 | Q = 45.25; df = 6; p < 0.0001 | ↓M (RES) [119] |
| db/db (+STZ) | ↑ | 8.78 (4.95; 12.62); p < 0.0001 | ||||
| L-Name+ HFD | ↔ | 2.51 (−6.97; 12.00); NS | ||||
| Pressure overload by AAB (TAC) | ↓ | −2.00 (−3.96; −0.04); p = 0.046 | ||||
| SHHF | ↑ | 4.62 (2.41; 6.83); p < 0.0001 | ||||
| SHR | ↔ | 3.14 (−9.10; 15.38); NS | ||||
| STZ | ↑ | 6.96 (2.16; 11.77); p = 0.0044 | ||||
| XO inhibitor | Allopurinol, Febuxostat, Oxypurinol | Pressure overload by ACF (TAC) | ↔ | 3.97 (−3.73; 11.66); NS | - | ↑M (ALLO) [177] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jasińska-Stroschein, M. Searching for Effective Treatments in HFpEF: Implications for Modeling the Disease in Rodents. Pharmaceuticals 2023, 16, 1449. https://doi.org/10.3390/ph16101449
Jasińska-Stroschein M. Searching for Effective Treatments in HFpEF: Implications for Modeling the Disease in Rodents. Pharmaceuticals. 2023; 16(10):1449. https://doi.org/10.3390/ph16101449
Chicago/Turabian StyleJasińska-Stroschein, Magdalena. 2023. "Searching for Effective Treatments in HFpEF: Implications for Modeling the Disease in Rodents" Pharmaceuticals 16, no. 10: 1449. https://doi.org/10.3390/ph16101449
APA StyleJasińska-Stroschein, M. (2023). Searching for Effective Treatments in HFpEF: Implications for Modeling the Disease in Rodents. Pharmaceuticals, 16(10), 1449. https://doi.org/10.3390/ph16101449






