Monoclonal Antibodies in Pregnancy and Breastfeeding in Patients with Multiple Sclerosis: A Review and an Updated Clinical Guide
Abstract
:1. Introduction
2. Monoclonal Antibodies and Family Planning in MS
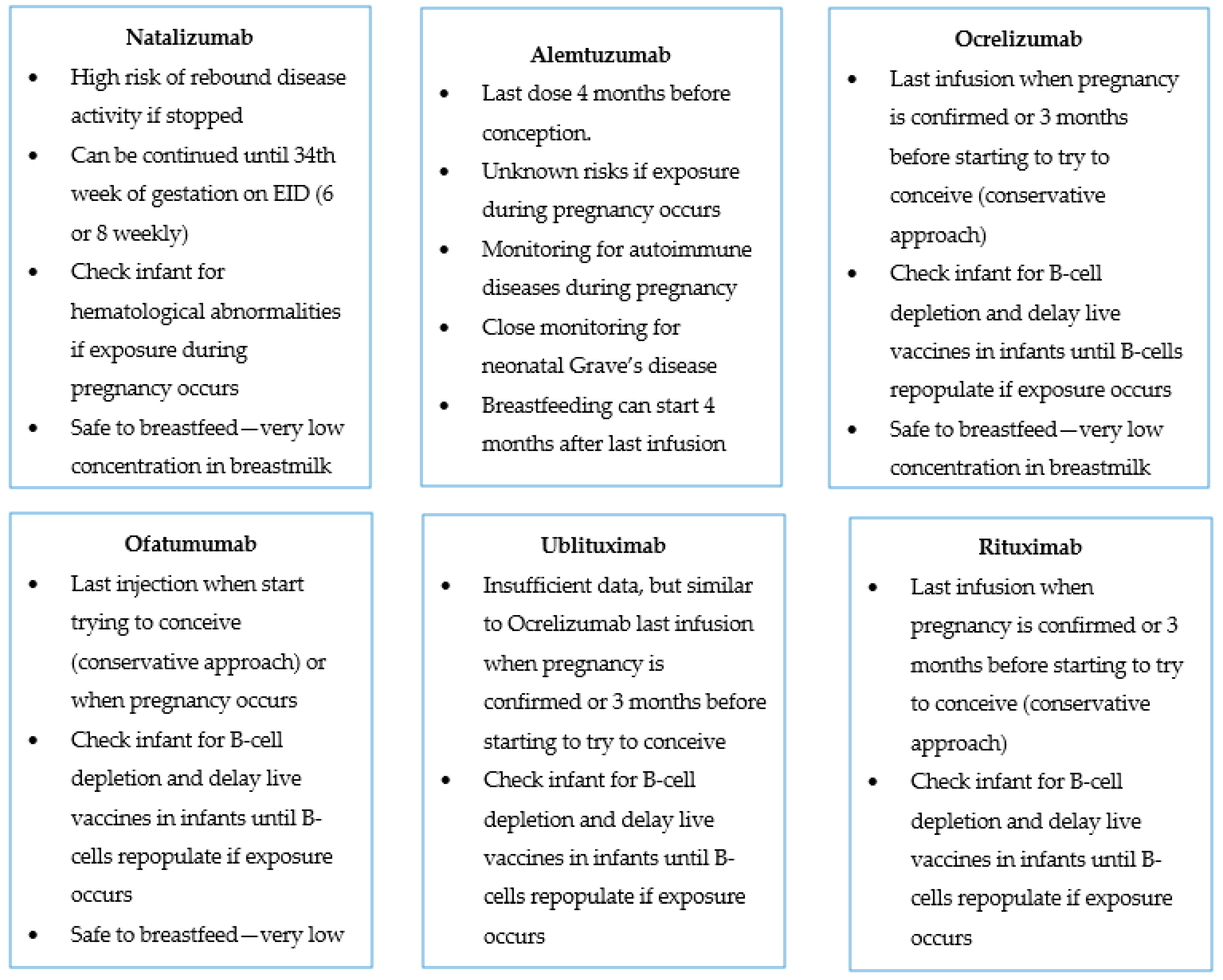
2.1. Natalizumab
2.2. Alemtuzumab
2.3. Ocrelizumab
2.4. Ofatumumab
2.5. Ublituximab
2.6. Rituximab
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dobson, R.; Giovannoni, G. Multiple sclerosis—A review. Eur. J. Neurol. 2018, 26, 27–40. [Google Scholar] [CrossRef] [PubMed]
- Harding, K.; Williams, O.; Willis, M.; Hrastelj, J.; Rimmer, A.; Joseph, F.; Tomassini, V.; Wardle, M.; Pickersgill, T.; Robertson, N.; et al. Clinical Outcomes of Escalation vs Early Intensive Disease-Modifying Therapy in Patients with Multiple Sclerosis. JAMA Neurol. 2019, 76, 536–541. [Google Scholar] [CrossRef]
- Brown, J.W.L.; Coles, A.; Horakova, D.; Havrdova, E.; Izquierdo, G.; Prat, A.; Girard, M.; Duquette, P.; Trojano, M.; Lugaresi, A.; et al. Association of Initial Disease-Modifying Therapy with Later Conversion to Secondary Progressive Multiple Sclerosis. JAMA 2019, 321, 175–187, Erratum in: JAMA 2020, 323, 1318. [Google Scholar] [CrossRef] [PubMed]
- He, A.; Merkel, B.; Brown, J.W.L.; Ryerson, L.Z.; Kister, I.; Malpas, C.B.; Sharmin, S.; Horakova, D.; Havrdova, E.K.; Spelman, T.; et al. Timing of high-efficacy therapy for multiple sclerosis: A retrospective observational cohort study. Lancet Neurol. 2020, 19, 307–316. [Google Scholar] [CrossRef]
- Spelman, T.; Magyari, M.; Piehl, F.; Svenningsson, A.; Rasmussen, P.V.; Kant, M.; Sellebjerg, F.; Joensen, H.; Hillert, J.; Lycke, J. Treatment Escalation vs Immediate Initiation of Highly Effective Treatment for Patients with Relapsing-Remitting Multiple Sclerosis: Data From 2 Different National Strategies. JAMA Neurol. 2021, 78, 1197–1204. [Google Scholar] [CrossRef] [PubMed]
- Fink, K.; Gorczyca, A.; Alping, P.; Englund, S.; Farmand, S.; Langer-Gould, A.M.; Piehl, F.; McKay, K.; Frisell, T.; Razaz, N. Multiple sclerosis, disease-modifying drugs and risk for adverse perinatal and pregnancy outcomes: Results from a population-based cohort study. Mult. Scler. J. 2023, 29, 731–740. [Google Scholar] [CrossRef] [PubMed]
- Moccia, M.; Affinito, G.; Fumo, M.G.; Giordana, R.; Di Gennaro, M.; Mercogliano, M.; Carotenuto, A.; Petracca, M.; Lanzillo, R.; Triassi, M.; et al. Fertility, pregnancy and childbirth in women with multiple sclerosis: A population-based study from 2018 to 2020. J. Neurol. Neurosurg. Psychiatry 2023, jnnp-2022-330883. [Google Scholar] [CrossRef]
- Kopp, T.I.; Pinborg, A.; Glazer, C.H.; Magyari, M. Women with female infertility seeking medically assisted reproduction are not at increased risk of developing multiple sclerosis. Hum. Reprod. 2022, 37, 1324–1333. [Google Scholar] [CrossRef] [PubMed]
- Franklin, G.M.; Tremlett, H. Multiple sclerosis and pregnancy: What should we be telling our patients? Neurology 2009, 73, 1820–1822. [Google Scholar] [CrossRef]
- Filippi, M.; Amato, M.P.; Centonze, D.; Gallo, P.; Gasperini, C.; Inglese, M.; Patti, F.; Pozzilli, C.; Preziosa, P.; Trojano, M. Early use of high-efficacy disease-modifying therapies makes the difference in people with multiple sclerosis: An expert opinion. J. Neurol. 2022, 269, 5382–5394, Erratum in J. Neurol. 2022, 269, 6690–6691. [Google Scholar] [CrossRef]
- LaHue, S.C.; Gelfand, A.A.; Bove, R.M. Navigating monoclonal antibody use in breastfeeding women: Do no harm or do little good? Neurology 2019, 93, 668–672. [Google Scholar] [CrossRef] [PubMed]
- Schubert, C.; Steinberg, L.; Peper, J.; Ramien, C.; Hellwig, K.; Köpke, S.; Solari, A.; Giordano, A.; Gold, S.M.; Friede, T.; et al. Postpartum relapse risk in multiple sclerosis: A systematic review and meta-analysis. J. Neurol. Neurosurg. Psychiatry 2023, jnnp-2022-330533. [Google Scholar] [CrossRef] [PubMed]
- Voskuhl, R.; Momtazee, C. Pregnancy: Effect on Multiple Sclerosis, Treatment Considerations, and Breastfeeding. Neurotherapeutics 2017, 14, 974–984. [Google Scholar] [CrossRef] [PubMed]
- Vukusic, S.; Hutchinson, M.; Hours, M.; Moreau, T.; Cortinovis-Tourniaire, P.; Adeleine, P.; Confavreux, C. Pregnancy and multiple sclerosis (the PRIMS study): Clinical predictors of post-partum relapse. Brain 2004, 127, 1353–1360, Erratum in Brain 2004, 127, 1912. [Google Scholar] [CrossRef] [PubMed]
- Confavreux, C.; Hutchinson, M.; Hours, M.M.; Cortinovis-Tourniaire, P.; Moreau, T. Rate of Pregnancy-Related Relapse in Multiple Sclerosis. Pregnancy in Multiple Sclerosis Group. N. Engl. J. Med. 1998, 339, 285–291. [Google Scholar] [CrossRef]
- Dobson, R.; Jokubaitis, V.G.; Giovannoni, G. Change in pregnancy- associated multiple sclerosis relapse rates over time: A meta-analysis. Mult. Scler. Relat. Disord. 2020, 44, 102241. [Google Scholar] [CrossRef]
- Portaccio, E.; Annovazzi, P.; Ghezzi, A.; Zaffaroni, M.; Moiola, L.; Martinelli, V.; Lanzillo, R.; Morra, V.B.; Rinaldi, F.; Gallo, P.; et al. Pregnancy decision- making in women with multiple sclerosis treated with natalizumab: II: Maternal risks. Neurology 2018, 90, e832–e839. [Google Scholar] [CrossRef]
- Anderson, A.; Krysko, K.M.; Rutatangwa, A.; Krishnakumar, T.; Chen, C.; Rowles, W.; Zhao, C.; Houtchens, M.K.; Bove, R. Clinical and Radiologic Disease Activity in Pregnancy and Postpartum in MS. Neurol. Neuroimmunol. Neuroinflamm. 2021, 8, e959. [Google Scholar] [CrossRef]
- Houtchens, M.; Bove, R.; Healy, B.; Houtchens, S.; Kaplan, T.B.; Mahlanza, T.; Chitnis, T.; Bakshi, R. MRI activity in MS and completed pregnancy: Data from a tertiary academic center. Neurol. Neuroimmunol. Neuroinflamm. 2020, 7, e890. [Google Scholar] [CrossRef]
- Laplaud, D.; Leray, E.; Barrière, P.; Wiertlewski, S.; Moreau, T. Increase in multiple sclerosis relapse rate following in vitro fertilization. Neurology 2006, 66, 1280–1281. [Google Scholar] [CrossRef]
- Hellwig, K.; Beste, C.; Brune, N.; Haghikia, A.; Müller, T.; Schimrigk, S.; Gold, R. Increased MS relapse rate during assisted reproduction technique. J. Neurol. 2008, 255, 592–593. [Google Scholar] [CrossRef] [PubMed]
- Hellwig, K.; Schimrigk, S.; Beste, C.; Müller, T.; Gold, R. Increase in Relapse Rate during Assisted Reproduction Technique in Patients with Multiple Sclerosis. Eur. Neurol. 2008, 61, 65–68. [Google Scholar] [CrossRef] [PubMed]
- Michel, L.; Foucher, Y.; Vukusic, S.; Confavreux, C.; de Sèze, J.; Brassat, D.; Clanet, M.; Clavelou, P.; Ouallet, J.-C.; Brochet, B.; et al. Increased risk of multiple sclerosis relapse after in vitro fertilisation. J. Neurol. Neurosurg. Psychiatry 2012, 83, 796–802. [Google Scholar] [CrossRef] [PubMed]
- Correale, J.; Farez, M.F.; Ysrraelit, M.C. Increase in multiple sclerosis activity after assisted reproduction technology. Ann. Neurol. 2012, 72, 682–694. [Google Scholar] [CrossRef] [PubMed]
- Bove, R.; Rankin, K.; Lin, C.; Zhao, C.; Correale, J.; Hellwig, K.; Michel, L.; Laplaud, D.A.; Chitnis, T. Effect of assisted reproductive technology on multiple sclerosis relapses: Case series and meta-analysis. Mult. Scler. J. 2019, 26, 1410–1419. [Google Scholar] [CrossRef] [PubMed]
- Mainguy, M.; Tillaut, H.; Degremont, A.; Le Page, E.; Mainguy, C.; Duros, S.; Polard, E.; Leray, E. Assessing the Risk of Relapse Requiring Corticosteroids After In Vitro Fertilization in Women with Multiple Sclerosis. Neurology 2022, 99, e1916–e1925. [Google Scholar] [CrossRef]
- Graham, E.L.; Bakkensen, J.B.; Anderson, A.; Lancki, N.; Davidson, A.; Giraldo, G.P.; Jungheim, E.S.; Vanderhoff, A.C.; Ostrem, B.; Mok-Lin, E.; et al. Inflammatory Activity After Diverse Fertility Treatments. Neurol. Neuroimmunol. Neuroinflamm. 2023, 10, e200106. [Google Scholar] [CrossRef]
- Uher, T.; Havrdova, E.K.; Vodehnalova, K.; Krasensky, J.; Capek, V.; Vaneckova, M.; Horakova, D. Pregnancy-induced brain magnetic resonance imaging changes in women with multiple sclerosis. Eur. J. Neurol. 2022, 29, 1446–1456. [Google Scholar] [CrossRef]
- Lehmann, H.; Zveik, O.; Levin, N.; Brill, L.; Imbar, T.; Vaknin-Dembinsky, A. Brain MRI activity during the year before pregnancy can predict post-partum clinical relapses. Mult. Scler. J. 2021, 27, 2232–2239. [Google Scholar] [CrossRef]
- Gklinos, P.; Papadopoulou, M.; Stanulovic, V.; Mitsikostas, D.; Papadopoulos, D. Monoclonal Antibodies as Neurological Therapeutics. Pharmaceuticals 2021, 14, 92. [Google Scholar] [CrossRef]
- Schneider, H.; Miller, R.K. Receptor-mediated uptake and transport of macromolecules in the human placenta. Int. J. Dev. Biol. 2010, 54, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Malek, A.; Sager, R.; Kuhn, P.; Nicolaides, K.H.; Schneider, H. Evolution of Maternofetal Transport of Immunoglobulins During Human Pregnancy. Am. J. Reprod. Immunol. 1996, 36, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.H.; Soon, D.; Fernando, K.T.; MacManus, D.G.; Barker, G.J.; Yousry, T.A.; Fisher, E.; O’Connor, P.W.; Phillips, J.T.; Polman, C.H.; et al. MRI outcomes in a placebo-controlled trial of natalizumab in relapsing MS. Neurology 2007, 68, 1390–1401. [Google Scholar] [CrossRef] [PubMed]
- Polman, C.H.; O’Connor, P.W.; Havrdova, E.; Hutchinson, M.; Kappos, L.; Miller, D.H.; Phillips, J.T.; Lublin, F.D.; Giovannoni, G.; Wajgt, A.; et al. A Randomized, Placebo-Controlled Trial of Natalizumab for Relapsing Multiple Sclerosis. N. Engl. J. Med. 2006, 354, 899–910. [Google Scholar] [CrossRef] [PubMed]
- Rudick, R.A.; Stuart, W.H.; Calabresi, P.A.; Confavreux, C.; Galetta, S.L.; Radue, E.-W.; Lublin, F.D.; Weinstock-Guttman, B.; Wynn, D.R.; Lynn, F.; et al. Natalizumab plus Interferon Beta-1a for Relapsing Multiple Sclerosis. N. Engl. J. Med. 2006, 354, 911–923. [Google Scholar] [CrossRef]
- Kapoor, R.; Ho, P.R.; Campbell, N.; Chang, I.; Deykin, A.; Forrestal, F.; Lucas, N.; Yu, B.; Arnold, D.L.; Freedman, M.S.; et al. Effect of natalizumab on disease progression in secondary progressive multiple sclerosis (ASCEND): A phase 3, randomised, double-blind, placebo-controlled trial with an open-label extension. Lancet Neurol. 2018, 17, 405–415. [Google Scholar] [CrossRef]
- Friend, S.; Richman, S.; Bloomgren, G.; Cristiano, L.M.; Wenten, M. Evaluation of pregnancy outcomes from the Tysabri® (natalizumab) pregnancy exposure registry: A global, observational, follow-up study. BMC Neurol. 2016, 16, 150. [Google Scholar] [CrossRef]
- Portaccio, E.; Annovazzi, P.; Ghezzi, A.; Zaffaroni, M.; Moiola, L.; Martinelli, V.; Lanzillo, R.; Morra, V.B.; Rinaldi, F.; Gallo, P.; et al. Pregnancy decision-making in women with multiple sclerosis treated with natalizumab: I: Fetal risks. Neurology 2018, 90, e823–e831. [Google Scholar] [CrossRef]
- Ebrahimi, N.; Herbstritt, S.; Gold, R.; Amezcua, L.; Koren, G.; Hellwig, K. Pregnancy and fetal outcomes following natalizumab exposure in pregnancy. A prospective, controlled observational study. Mult. Scler. J. 2014, 21, 198–205. [Google Scholar] [CrossRef]
- Hellwig, K.; Tokic, M.; Thiel, S.; Esters, N.; Spicher, C.; Timmesfeld, N.; Ciplea, A.I.; Gold, R.; Langer-Gould, A. Multiple Sclerosis Disease Activity and Disability Following Discontinuation of Natalizumab for Pregnancy. JAMA Netw. Open 2022, 5, e2144750. [Google Scholar] [CrossRef]
- Haghikia, A.; Langer-Gould, A.; Rellensmann, G.; Schneider, H.; Tenenbaum, T.; Elias-Hamp, B.; Menck, S.; Zimmermann, J.; Herbstritt, S.; Marziniak, M.; et al. Natalizumab Use During the Third Trimester of Pregnancy. JAMA Neurol. 2014, 71, 891–895. [Google Scholar] [CrossRef] [PubMed]
- Thiel, S.; Litvin, N.; Haben, S.; Ciplea, A.; Gold, R.; Hellwig, K. Disease activity and pregnancy outcomes after long-term exposure to natalizumab during pregnancy. In Proceedings of the 39th Congress of the European Committee for Treatment and Research In Multiple Sclerosis, Amsterdam, The Netherlands, 26–28 October 2022. [Google Scholar]
- Krysko, K.M.; Dobson, R.; Alroughani, R.; Amato, M.P.; Bove, R.; Ciplea, A.I.; Fragoso, Y.; Houtchens, M.; Jokubaitis, V.G.; Magyari, M.; et al. Family planning considerations in people with multiple sclerosis. Lancet Neurol. 2023, 22, 350–366. [Google Scholar] [CrossRef] [PubMed]
- Foley, J.F.; Defer, G.; Ryerson, L.Z.; Cohen, J.A.; Arnold, D.L.; Butzkueven, H.; Cutter, G.; Giovannoni, G.; Killestein, J.; Wiendl, H.; et al. Comparison of switching to 6-week dosing of natalizumab versus continuing with 4-week dosing in patients with relapsing-remitting multiple sclerosis (NOVA): A randomised, controlled, open-label, phase 3b trial. Lancet Neurol. 2022, 21, 608–619. [Google Scholar] [CrossRef] [PubMed]
- Dobson, R.; Dassan, P.; Roberts, M.; Giovannoni, G.; Nelson-Piercy, C.; Brex, P.A. UK consensus on pregnancy in multiple sclerosis: ‘Association of British Neurologists’ guidelines. Pract. Neurol. 2019, 19, 106–114. [Google Scholar] [CrossRef]
- Coles, A.J.; Cohen, J.A.; Fox, E.J.; Giovannoni, G.; Hartung, H.P.; Havrdova, E.; Schippling, S.; Selmaj, K.W.; Traboulsee, A.; Compston, D.A.S.; et al. Alemtuzumab CARE- MS II 5-year follow-up: Efficacy and safety findings. Neurology 2017, 89, 1117–1126. [Google Scholar] [CrossRef]
- Oh, J.; Achiron, A.; Celius, E.G.; Chambers, C.; Derwenskus, J.; Devonshire, V.; Hellwig, K.; Hutton, G.J.; McCombe, P.; Moore, M.; et al. Pregnancy outcomes and postpartum relapse rates in women with RRMS treated with alemtuzumab in the phase 2 and 3 clinical development program over 16 years. Mult. Scler. Relat. Disord. 2020, 43, 102146. [Google Scholar] [CrossRef]
- Kappos, L.; Li, D.; Calabresi, P.A.; O’Connor, P.; Bar-Or, A.; Barkhof, F.; Yin, M.; Leppert, D.; Glanzman, R.; Tinbergen, J.; et al. Ocrelizumab in relapsing-remitting multiple sclerosis: A phase 2, randomised, placebo-controlled, multicentre trial. Lancet 2011, 378, 1779–1787. [Google Scholar] [CrossRef]
- van Lierop, Z.Y.; Toorop, A.A.; van Ballegoij, W.J.; Dubbelink, T.B.O.; Strijbis, E.M.; de Jong, B.A.; van Oosten, B.W.; Moraal, B.; Teunissen, C.E.; Uitdehaag, B.M.; et al. Personalized B-cell tailored dosing of ocrelizumab in patients with multiple sclerosis during the COVID-19 pandemic. Mult. Scler. J. 2021, 28, 1121–1125. [Google Scholar] [CrossRef]
- Rolfes, L.; Pawlitzki, M.; Pfeuffer, S.; Nelke, C.; Lux, A.; Pul, R.; Kleinschnitz, C.; Kleinschnitz, K.; Rogall, R.; Pape, K.; et al. Ocrelizumab Extended Interval Dosing in Multiple Sclerosis in Times of COVID-19. Neurol. Neuroimmunol. Neuroinflamm. 2021, 8, e1035. [Google Scholar] [CrossRef]
- Oreja-Guevara, C.; Vukusic, S.; Pietrasanta, C.; McElrath, T.; Hellwig, K.; Bove, R.; Craveiro, L.; Ferreira, G.; Lin, C.-J.; Pasquarelli, N.; et al. Pregnancy and infant outcomes in women receiving ocrelizumab for the treatment of multiple sclerosis. In Proceedings of the 39th Congress of The European Committee for Treatment and Research in Multiple Sclerosis, Amsterdam, The Netherlands, 26–28 October 2022. [Google Scholar]
- Kümpfel, T.; Thiel, S.; Meinl, I.; Ciplea, A.I.; Bayas, A.; Hoffmann, F.; Oy, U.H.-V.; Hoshi, M.; Kluge, J.; Ringelstein, M.; et al. Anti-CD20 therapies and pregnancy in neuroimmunologic disorders: A cohort study from Germany. Neurol. Neuroimmunol. Neuroinflamm. 2020, 8, e913. [Google Scholar] [CrossRef]
- Rolfes, M.; Rutatangwa, A.; Waubant, E.; Krysko, K.M. Ocrelizumab exposure in the second trimester of pregnancy without neonatal B-cell depletion. Mult. Scler. Relat. Disord. 2020, 45, 102398. [Google Scholar] [CrossRef] [PubMed]
- Schwake, C.; Steinle, J.; Thiel, S.; Ciplea, A.; Gold, R.; Hellwig, K. Effects of anti-CD20 therapies on infant health and physiological B-cell development if administered before or during pregnancy and/or lactation. In Proceedings of the 39th Congress of the European Committee for Treatment and Research In Multiple Sclerosis, Amsterdam, The Netherlands, 26–28 October 2022. [Google Scholar]
- Anderson, A.; Poole, S.; Rowle, W.; Jacobs, D.; Bevan, C.; Brandstadter, R.; Ciplea, A.I.; Cooper, A.C.J.; Fabian, M.; Kakara, M.; et al. Anti-CD20 monoclonal antibody therapy after 59 pregnancies in women with neurological conditions: Low breastmilk transfer and normal infant development in a multicenter cohort. In Proceedings of the 39th Congress of The European Committee For Treatment And Research In Multiple Sclerosis, Amsterdam, The Netherlands, 26–28 October 2022. [Google Scholar]
- Hellwig, K.; Yamout, B.; Bove, R.; Gummuluri, K.S.; Schulze-Topphoff, U.; Fantaccini, S.; Zielman, R.; Sullivan, R.; Amato, M.P.; Dobson, R.; et al. Pregnancy outcomes in ofatumumab-treated patients with multiple sclerosis. In Proceedings of the Consortium of Multiple Sclerosis Centers Annual Meeting, National Harbor, MD, USA, 1–4 June 2022. [Google Scholar]
- Babiker, H.M.; Glode, A.E.; Cooke, L.S.; Mahadevan, D. Ublituximab for the treatment of CD20 positive B-cell malignancies. Expert Opin. Investig. Drugs 2018, 27, 407–412. [Google Scholar] [CrossRef]
- Le Garff-Tavernier, M.; Herbi, L.; de Romeuf, C.; Nguyen-Khac, F.; Davi, F.; Grelier, A.; Boudjoghra, M.; Maloum, K.; Choquet, S.; Urbain, R.; et al. Antibody-dependent cellular cytotoxicity of the optimized anti-CD20 monoclonal antibody ublituximab on chronic lymphocytic leukemia cells with the 17p deletion. Leukemia 2013, 28, 230–233. [Google Scholar] [CrossRef]
- Smith, J.B.; Hellwig, K.; Fink, K.; Lyell, D.J.; Piehl, F.; Langer-Gould, A. Rituximab, MS, and pregnancy. Neurol. Neuroimmunol. Neuroinflamm. 2020, 7, e734. [Google Scholar] [CrossRef] [PubMed]
- Das, G.; Damotte, V.; Gelfand, J.M.; Bevan, C.; Cree, B.A.; Do, L.; Green, A.J.; Hauser, S.L.; Bove, R. Rituximab before and during pregnancy: A systematic review, and a case series in MS and NMOSD. Neurol. Neuroimmunol. Neuroinflamm. 2018, 5, e453. [Google Scholar] [CrossRef] [PubMed]
- Perrotta, K.; Kiernan, E.; Bandoli, G.; Manaster, R.; Chambers, C. Pregnancy outcomes following maternal treatment with rituximab prior to or during pregnancy: A case series. Rheumatol. Adv. Pract. 2021, 5, rkaa074. [Google Scholar] [CrossRef] [PubMed]
- Dehghanimahmoudabadi, A.; Kianfar, N.M.; Akhdar, M.; Dasdar, S.M.; Balighi, K.; Mahmoudi, H.; Daneshpazhooh, M. Pregnancy outcomes in women with pemphigus exposed to rituximab before or during pregnancy. Int. J. Women’s Dermatol. 2022, 8, e038. [Google Scholar] [CrossRef] [PubMed]
| Natalizumab | Alemtuzumab | Ocrelizumab | Ofatumumab | Ublituximab | Rituximab | |
|---|---|---|---|---|---|---|
| IgG subclass | IgG4 | IgG1 | IgG1 | IgG1 | IgG1 | IgG1 |
| Route of administration and dosing intervals | IV *—4 weekly | IV *—2 courses 1 year apart | IV *—6 monthly | SC *—monthly | IV *—6 monthly | IV *—6 monthly |
| Use in pregnancy | Can be used | No | Not routinely | Not routinely | Not routinely | Not routinely |
| Mechanism of action | Anti-trafficking, binds to α4-integrin expressed on lymphocytes | Immune reconstitution therapy, anti-CD52 | Anti-CD20, B-cell depletion | Anti-CD20, B-cell depletion | Anti-CD20, B-cell depletion | Anti-CD20, B-cell depletion |
| Risk of rebound activity if stopped | High | No | No | Unknown | Unknown | No |
| Last dose | Last infusion no later than 34 weeks of gestation. | Last infusion no later than 4 months before starting to try to conceive. | Last infusion 3 months before starting to try to conceive (conservative approach) or stopping when pregnancy is confirmed. | Last injection when starting to try to conceive (conservative approach) or stopping when pregnancy is confirmed. | Last infusion 3 months before starting to try to conceive (conservative approach) or stopping when pregnancy is confirmed. | Last infusion 3 months before starting to try to conceive (conservative approach) or stopping when pregnancy is confirmed. |
| Risk of miscarriage | No | Insufficient data | No | Not enough data | Not enough data | Probably not; there is a study with high rate of miscarriage, though it was attributed to pre-existing infertility |
| Fetal exposure during pregnancy risks | Hematological abnormalities | Unknown | Neonatal B-cell depletion | No data | No data | Neonatal B-cell depletion |
| Other considerations | - | Neonatal Grave’s disease | - | - | - | - |
| Breastfeeding (≥2 weeks post-partum) | Yes | Wait 4 months after last infusion | Yes | Yes | No data | Yes |
| Vaccinations | Avoid live vaccines in mother. Postpone in neonates exposed during third trimester. | Avoid live vaccines in mother. Exclude hematological abnormalities in neonates before live vaccines | Avoid live vaccines in mother. Exclude low B-cell counts in neonates before live vaccines | Avoid live vaccines in mother. Exclude low B-cell counts in neonates before live vaccines | Avoid live vaccines in mother. Exclude low B-cell counts in neonates before live vaccines | Avoid live vaccines in mother. Exclude low B-cell counts in neonates before live vaccines |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gklinos, P.; Dobson, R. Monoclonal Antibodies in Pregnancy and Breastfeeding in Patients with Multiple Sclerosis: A Review and an Updated Clinical Guide. Pharmaceuticals 2023, 16, 770. https://doi.org/10.3390/ph16050770
Gklinos P, Dobson R. Monoclonal Antibodies in Pregnancy and Breastfeeding in Patients with Multiple Sclerosis: A Review and an Updated Clinical Guide. Pharmaceuticals. 2023; 16(5):770. https://doi.org/10.3390/ph16050770
Chicago/Turabian StyleGklinos, Panagiotis, and Ruth Dobson. 2023. "Monoclonal Antibodies in Pregnancy and Breastfeeding in Patients with Multiple Sclerosis: A Review and an Updated Clinical Guide" Pharmaceuticals 16, no. 5: 770. https://doi.org/10.3390/ph16050770
APA StyleGklinos, P., & Dobson, R. (2023). Monoclonal Antibodies in Pregnancy and Breastfeeding in Patients with Multiple Sclerosis: A Review and an Updated Clinical Guide. Pharmaceuticals, 16(5), 770. https://doi.org/10.3390/ph16050770






