Mannose-Functionalized Isoniazid-Loaded Nanostructured Lipid Carriers for Pulmonary Delivery: In Vitro Prospects and In Vivo Therapeutic Efficacy Assessment
Abstract
:1. Introduction
2. Results and Discussion
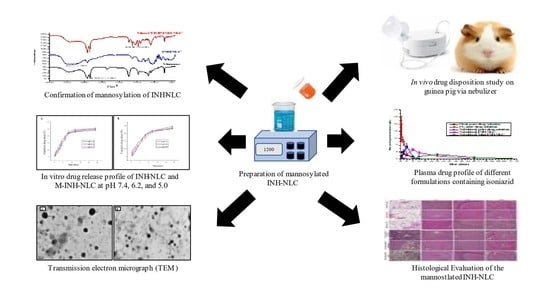
2.1. Investigation of Mannose-Functionalized NLC
2.2. Encapsulation Efficiency and Drug Loading
2.3. Average Particle Size, Polydispersity Index, and Zeta Potential Measurements
2.4. In Vitro Drug Release Analysis
2.5. In Vitro Release Kinetics
2.6. Transmission Electron Microscopy
2.7. In Vitro Evaluation of Inhalation Behavior of Nebulized Mist
2.8. In Vivo Pharmacokinetic Analysis
2.9. Histological Evaluation
2.10. Hepatotoxic and Nephrotoxic Evaluation
3. Materials and Methods
3.1. Material and Components
3.2. Method of Preparation of NLC
3.3. Mannosylation of Nanostructured Lipid Carriers
3.4. Fourier-Transform Infrared Spectroscopy
3.5. Encapsulation Efficiency and Drug Loading Analysis
3.6. Average Particle Size, Polydispersity Index, and Zeta Potential Analysis
3.7. In Vitro Drug Release Analysis
3.8. In Vitro Drug Release Kinetics
3.9. Transmission Electron Microscopy
3.10. In Vitro Evaluation of Inhalation Behavior of Nebulized Mist
3.11. Experimental Animal Model
3.11.1. Animals
3.11.2. Nebulization Conditions
3.11.3. In Vivo Pharmacokinetic Analysis
3.12. Reverse-Phase High-Performance Liquid Chromatographic Condition
3.13. Method Validation and Preparation of Calibration Curve
3.14. Preparation of Plasma Samples
3.15. Histological Evaluation
3.16. Hepatotoxic and Nephrotoxic Evaluation
3.17. Statistical Analysis
4. Conclusions
Future Prospects
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fogel, N. Tuberculosis: A Disease without Boundaries. Tuberculosis 2015, 95, 527–531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miggiano, R.; Rizzi, M.; Ferraris, D.M. Mycobacterium tuberculosis Pathogenesis, Infection Prevention and Treatment. Pathogens 2020, 9, 385. [Google Scholar] [CrossRef] [PubMed]
- Seung, K.J.; Keshavjee, S.; Rich, M.L. Multidrug-Resistant Tuberculosis and Extensively Drug-Resistant Tuberculosis. Cold Spring Harb. Perspect. Med. 2015, 5, a017863. [Google Scholar] [CrossRef] [Green Version]
- Kebede, B. Tuberculosis Epidemiology, Pathogenesis, Drugs and Drug Resistance Development: A Review. J. Biomed. Sci. 2019, 8, 1–10. [Google Scholar]
- Agyeman, A.A.; Ofori-Asenso, R. Tuberculosis—An Overview. J. Public Health Emerg. 2017, 1, 7. [Google Scholar] [CrossRef]
- Zumla, A.; Nahid, P.; Cole, S.T. Advances in the Development of New Tuberculosis Drugs and Treatment Regimens. Nat. Rev. Drug Discov. 2013, 12, 388–404. [Google Scholar] [CrossRef]
- Franzblau, S.G.; DeGroote, M.A.; Cho, S.H.; Andries, K.; Nuermberger, E.; Orme, I.M.; Mdluli, K.; Angulo-Barturen, I.; Dick, T.; Dartois, V.; et al. Comprehensive Analysis of Methods Used for the Evaluation of Compounds against Mycobacterium tuberculosis. Tuberculosis 2012, 92, 453–488. [Google Scholar] [CrossRef] [Green Version]
- Timmins, G.S.; Deretic, V. Mechanisms of Action of Isoniazid. Mol. Microbiol. 2006, 62, 1220–1227. [Google Scholar] [CrossRef]
- Khatak, S.; Mehta, M.; Awasthi, R.; Paudel, K.R.; Singh, S.K.; Gulati, M.; Hansbro, N.G.; Hansbro, P.M.; Dua, K.; Dureja, H. Solid Lipid Nanoparticles Containing Anti-Tubercular Drugs Attenuate the Mycobacterium marinum Infection. Tuberculosis 2020, 125, 102008. [Google Scholar] [CrossRef]
- Weber, W.W.; Hein, D.W. Clinical Pharmacokinetics of Isoniazid. Clin. Pharmacokinet. 1979, 4, 401–422. [Google Scholar] [CrossRef]
- Diallo, T.; Adjobimey, M.; Ruslami, R.; Trajman, A.; Sow, O.; Obeng Baah, J.; Marks, G.B.; Long, R.; Elwood, K.; Zielinski, D.; et al. Safety and Side Effects of Rifampin versus Isoniazid in Children. N. Engl. J. Med. 2018, 379, 454–463. [Google Scholar] [CrossRef] [PubMed]
- Stagg, H.R.; Lipman, M.C.; Mchugh, T.D.; Jenkins, H.E. Isoniazid-Resistant Tuberculosis: A Cause for Concern? Int. J. Tuberc. Lung Dis. 2017, 21, 129–139. [Google Scholar] [CrossRef]
- Pardeshi, C.V.; Agnihotri, V.V.; Patil, K.Y.; Pardeshi, S.R.; Surana, S.J. Mannose-Anchored N,N,N-Trimethyl Chitosan Nanoparticles for Pulmonary Administration of Etofylline. Int. J. Biol. Macromol. 2020, 165, 445–459. [Google Scholar] [CrossRef] [PubMed]
- Patil, T.S.; Deshpande, A.S. Mannosylated Nanocarriers Mediated Site-Specific Drug Delivery for the Treatment of Cancer and Other Infectious Diseases: A State of the Art Review. J. Control. Release 2020, 320, 239–252. [Google Scholar] [CrossRef] [PubMed]
- Rojanarat, W.; Nakpheng, T.; Thawithong, E.; Yanyium, N.; Srichana, T. Inhaled Pyrazinamide Proliposome for Targeting Alveolar Macrophages. Drug Deliv. 2012, 19, 334–345. [Google Scholar] [CrossRef]
- Wijagkanalan, W.; Kawakami, S.; Takenaga, M.; Igarashi, R.; Yamashita, F.; Hashida, M. Efficient Targeting to Alveolar Macrophages by Intratracheal Administration of Mannosylated Liposomes in Rats. J. Control. Release 2008, 125, 121–130. [Google Scholar] [CrossRef]
- Saraogi, G.K.; Sharma, B.; Joshi, B.; Gupta, P.; Gupta, U.D.; Jain, N.K.; Agrawal, G.P. Mannosylated Gelatin Nanoparticles Bearing Isoniazid for Effective Management of Tuberculosis. J. Drug Target. 2011, 19, 219–227. [Google Scholar] [CrossRef]
- Filatova, L.Y.; Klyachko, N.L.; Kudryashova, E.V. Targeted Delivery of Anti-Tuberculosis Drugs to Macrophages: Targeting Mannose Receptors. Russ. Chem. Rev. 2018, 87, 374. [Google Scholar] [CrossRef]
- Tiwari, S.; Chaturvedi, A.P.; Tripathi, Y.B.; Mishra, B. Macrophage-Specific Targeting of Isoniazid Through Mannosylated Gelatin Microspheres. AAPS PharmSciTech 2011, 12, 900–908. [Google Scholar] [CrossRef] [Green Version]
- Virmani, T.; Kumar, G.; Sharma, A.; Pathak, K.; Akhtar, M.S.; Afzal, O.; Altamimi, A.S.A. Amelioration of Cancer Employing Chitosan, Its Derivatives, and Chitosan-Based Nanoparticles: Recent Updates. Polymers 2023, 15, 2928. [Google Scholar] [CrossRef]
- Alhalmi, A.; Beg, S.; Almalki, W.H.; Alghamdi, S.; Kohli, K. Recent Advances in Nanotechnology-Based Targeted Therapeutics for Breast Cancer Management. Curr. Drug Metab. 2022, 14, 35657282. [Google Scholar] [CrossRef]
- Nandvikar, N.Y.; Lala, R.R.; Shinde, A.S. Nanostructured Lipid Carrier: The Advanced Lipid Carriers. Int. J. Pharm. Sci. Res. 2019, 10, 5252–5265. [Google Scholar] [CrossRef]
- Virmani, T.; Kumar, G.; Virmani, R.; Sharma, A.; Pathak, K. Nanocarrier-Based Approaches to Combat Chronic Obstructive Pulmonary Disease. Nanomedicine 2022, 17, 1833–1854. [Google Scholar] [CrossRef] [PubMed]
- Kumar, G.; Virmani, T.; Sharma, A.; Pathak, K. Codelivery of Phytochemicals with Conventional Anticancer Drugs in Form of Nanocarriers. Pharmaceutics 2023, 15, 889. [Google Scholar] [CrossRef]
- Vieira, R.; Severino, P.; Nalone, L.A.; Souto, S.B.; Silva, A.M.; Lucarini, M.; Durazzo, A.; Santini, A.; Souto, E.B. Sucupira Oil-Loaded Nanostructured Lipid Carriers (NLC): Lipid Screening, Factorial Design, Release Profile, and Cytotoxicity. Molecules 2020, 25, 685. [Google Scholar] [CrossRef] [Green Version]
- Subramaniam, B.; Siddik, Z.H.; Nagoor, N.H. Optimization of Nanostructured Lipid Carriers: Understanding the Types, Designs, and Parameters in the Process of Formulations. J. Nanoparticle Res. 2020, 22, 141. [Google Scholar] [CrossRef]
- Haider, M.; Abdin, S.M.; Kamal, L.; Orive, G. Nanostructured Lipid Carriers for Delivery of Chemotherapeutics: A Review. Pharmaceutics 2020, 12, 288. [Google Scholar] [CrossRef] [Green Version]
- Pinheiro, M.; Ribeiro, R.; Vieira, A.; Andrade, F.; Reis, S. Design of a Nanostructured Lipid Carrier Intended to Improve the Treatment of Tuberculosis. Drug Des. Devel. Ther. 2016, 10, 2467–2475. [Google Scholar] [CrossRef] [Green Version]
- Sahu, P.K.; Mishra, D.K.; Jain, N.; Rajoriya, V.; Jain, A.K. Mannosylated Solid Lipid Nanoparticles for Lung-Targeted Delivery of Paclitaxel. Drug Dev. Ind. Pharm. 2015, 41, 640–649. [Google Scholar] [CrossRef]
- Jain, A.; Agarwal, A.; Majumder, S.; Lariya, N.; Khaya, A.; Agrawal, H.; Majumdar, S.; Agrawal, G.P. Mannosylated Solid Lipid Nanoparticles as Vectors for Site-Specific Delivery of an Anti-Cancer Drug. J. Control. Release 2010, 148, 359–367. [Google Scholar] [CrossRef]
- Sharma, P.R.; Dravid, A.A.; Kalapala, Y.C.; Gupta, V.K.; Jeyasankar, S.; Goswami, A.; Agarwal, R. Cationic Inhalable Particles for Enhanced Drug Delivery to M. tuberculosis Infected Macrophages. Biomater. Adv. 2022, 133, 112612. [Google Scholar] [CrossRef]
- Vieira, A.C.C.; Magalhães, J.; Rocha, S.; Cardoso, M.S.; Santos, S.G.; Borges, M.; Pinheiro, M.; Reis, S. Targeted Macrophages Delivery of Rifampicin-Loaded Lipid Nanoparticles to Improve Tuberculosis Treatment. Nanomedicine 2017, 12, 2721–2736. [Google Scholar] [CrossRef] [PubMed]
- Zainab; Ahmad, S.; Khan, I.; Saeed, K.; Ahmad, H.; Alam, A.; Almehmadi, M.; Alsaiari, A.A.; Haitao, Y.; Ahmad, M. A Study on Green Synthesis, Characterization of Chromium Oxide Nanoparticles and Their Enzyme Inhibitory Potential. Front. Pharmacol. 2022, 13, 1008182. [Google Scholar] [CrossRef]
- Kumar, G.; Virmani, T.; Pathak, K.; Al Kamaly, O.; Saleh, A. Central Composite Design Implemented Azilsartan Medoxomil Loaded Nanoemulsion to Improve Its Aqueous Solubility and Intestinal Permeability: In Vitro and Ex Vivo Evaluation. Pharmaceuticals 2022, 15, 1343. [Google Scholar] [CrossRef]
- Zhou, Y.; Ahuja, A.; Irvin, C.M.; Kracko, D.A.; McDonald, J.D.; Cheng, Y.-S. Medical Nebulizer Performance: Effects of Cascade Impactor Temperature. Respir. Care 2005, 50, 1077–1082. [Google Scholar]
- Al Ayoub, Y.; Gopalan, R.C.; Najafzadeh, M.; Mohammad, M.A.; Anderson, D.; Paradkar, A.; Assi, K.H. Development and Evaluation of Nanoemulsion and Microsuspension Formulations of Curcuminoids for Lung Delivery with a Novel Approach to Understanding the Aerosol Performance of Nanoparticles. Int. J. Pharm. 2019, 557, 254–263. [Google Scholar] [CrossRef] [Green Version]
- Sharma, A.; Sharma, S.; Khuller, G.K. Lectin-Functionalized Poly (Lactide-Co-Glycolide) Nanoparticles as Oral/Aerosolized Antitubercular Drug Carriers for Treatment of Tuberculosis. J. Antimicrob. Chemother. 2004, 54, 761–766. [Google Scholar] [CrossRef]
- Alhalmi, A.; Amin, S.; Beg, S.; Al-Salahi, R.; Mir, S.R.; Kohli, K. Formulation and Optimization of Naringin Loaded Nanostructured Lipid Carriers Using Box-Behnken Based Design: In Vitro and Ex Vivo Evaluation. J. Drug Deliv. Sci. Technol. 2022, 74, 103590. [Google Scholar] [CrossRef]
- Patil, T.S.; Deshpande, A.S. Design, Development, and Characterisation of Clofazimine-Loaded Mannosylated Nanostructured Lipid Carriers: 33-Box-Behnken Design Approach. Mater. Technol. 2021, 36, 460–475. [Google Scholar] [CrossRef]
- Alhalmi, A.; Amin, S.; Khan, Z.; Beg, S.; Al, O.; Saleh, A.; Kohli, K. Nanostructured Lipid Carrier-Based Codelivery of Raloxifene and Naringin: Formulation, Optimization, In Vitro, Ex Vivo, In Vivo Assessment, and Acute Toxicity Studies. Pharmaceutics 2022, 14, 1771. [Google Scholar] [CrossRef]
- Shah, N.V.; Seth, A.K.; Balaraman, R.; Aundhia, C.J.; Maheshwari, R.A.; Parmar, G.R. Nanostructured Lipid Carriers for Oral Bioavailability Enhancement of Raloxifene: Design and in Vivo Study. J. Adv. Res. 2016, 7, 423–434. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rahman, M.; Almalki, W.H.; Afzal, O.; Altamimi, A.S.A.; Kazmi, I.; Al-Abbasi, F.A.; Choudhry, H.; Alenezi, S.K.; Barkat, M.A.; Beg, S.; et al. Cationic Solid Lipid Nanoparticles of Resveratrol for Hepatocellular Carcinoma Treatment: Systematic Optimization, in Vitro Characterization and Preclinical Investigation. Int. J. Nanomed. 2020, 15, 9283–9299. [Google Scholar] [CrossRef] [PubMed]
- Patil-Gadhe, A.; Pokharkar, V. Montelukast-Loaded Nanostructured Lipid Carriers: Part I Oral Bioavailability Improvement. Eur. J. Pharm. Biopharm. 2014, 88, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, A.V.; Pydi, C.R.; Verma, R.; Jose, J.; Kumar, L. Design, Preparation and In Vitro Characterizations of Fluconazole Loaded Nanostructured Lipid Carriers. Braz. J. Pharm. Sci. 2020, 56, e18069. [Google Scholar] [CrossRef]
- Czajkowska-Kośnik, A.; Szymańska, E.; Czarnomysy, R.; Jacyna, J.; Markuszewski, M.; Basa, A.; Winnicka, K. Nanostructured Lipid Carriers Engineered as Topical Delivery of Etodolac: Optimization and Cytotoxicity Studies. Materials 2021, 14, 596. [Google Scholar] [CrossRef]
- Velmurugan, R.; Selvamuthukumar, S. Development and Optimization of Ifosfamide Nanostructured Lipid Carriers for Oral Delivery Using Response Surface Methodology. Appl. Nanosci. 2016, 6, 159–173. [Google Scholar] [CrossRef] [Green Version]
- Tyagi, N.; Gupta, P.; Khan, Z.; Neupane, Y.R.; Mangla, B.; Mehra, N.; Ralli, T.; Alhalmi, A.; Ali, A.; Al Kamaly, O. Superparamagnetic Iron-Oxide Nanoparticles Synthesized via Green Chemistry for the Potential Treatment of Breast Cancer. Molecules 2023, 28, 2343. [Google Scholar] [CrossRef]
- Yamamoto, H.; Kuno, Y.; Sugimoto, S.; Takeuchi, H.; Kawashima, Y. Surface-Modified PLGA Nanosphere with Chitosan Improved Pulmonary Delivery of Calcitonin by Mucoadhesion and Opening of the Intercellular Tight Junctions. J. Control. Release 2005, 102, 373–381. [Google Scholar] [CrossRef]
- Pandey, R.; Khuller, G.K. Solid Lipid Particle-Based Inhalable Sustained Drug Delivery System against Experimental Tuberculosis. Tuberculosis 2005, 85, 227–234. [Google Scholar] [CrossRef]
- Pandey, R.; Sharma, A.; Zahoor, A.; Sharma, S.; Khuller, G.K.; Prasad, B. Poly (Dl-Lactide-Co-Glycolide) Nanoparticle-Based Inhalable Sustained Drug Delivery System for Experimental Tuberculosis. J. Antimicrob. Chemother. 2003, 52, 981–986. [Google Scholar] [CrossRef] [Green Version]
- Dasht Bozorg, B.; Goodarzi, A.; Fahimi, F.; Tabarsi, P.; Shahsavari, N.; Kobarfard, F.; Dastan, F. Simultaneous Determination of Isoniazid, Pyrazinamide and Rifampin in Human Plasma by High-Performance Liquid Chromatography and UV Detection. Iran. J. Pharm. Res. IJPR 2019, 18, e124712. [Google Scholar] [CrossRef]
- Kar, R.; Nangpal, P.; Mathur, S.; Singh, S.; Tyagi, A.K. BioA Mutant of Mycobacterium tuberculosis Shows Severe Growth Defect and Imparts Protection against Tuberculosis in Guinea Pigs. PLoS ONE 2017, 12, e0179513. [Google Scholar] [CrossRef] [PubMed] [Green Version]





| S. No. | Formulation | Encapsulation Efficiency (%EE) | Drug Loading (%DL) |
|---|---|---|---|
| 1. | INH-NLC | 82.09 ± 3.60 ** | 18.39 ± 0.81 ** |
| 2. | Man-INH-NLC | 79.71 ± 1.65 ** | 17.86 ± 0.37 ** |
| S. No. | Formulation | Particle Size Analysis (nm) | The Polydispersity Index (PDI) | Zeta Potential (mV) |
|---|---|---|---|---|
| 1. | INH-NLC | 247.6 ± 4.05 | 0.289 ± 0.04 | +42.48 ± 1.86 |
| 2. | Man-INH-NLC | 273.4 ± 8.24 | 0.223 ± 0.02 | +24.18 ± 2.26 |
| S. No. | Formulation | Zero-Order | First-Order | Higuchi’s Square Root Model | Korsmeyer–Peppas Model |
|---|---|---|---|---|---|
| 1 | INH-NLC | 0.739 | 0.739 | 0.9019 | 0.9661 |
| 2 | Man-INH-NLC | 0.7881 | 0.7881 | 0.9298 | 0.9717 |
| Formulations | Cmax, mg/L | Tmax, Hour | Kel | t1/2, Hour | MRT, Hour | AUC0–∞ (mg.h/L) | Relative Bioavailability | Absolute Bioavailability |
|---|---|---|---|---|---|---|---|---|
| Pure drug solution, Oral | 4.08 ± 0.42 | 1 | 0.16 ± 0.01 | 4.25 ± 0.34 | 4.87 ± 0.2 | 22.65 ± 2.55 | 1 | 0.49 |
| Pure drug solution, IV | 22.04 ± 2.21 | 0.25 | 0.66 ± 0.19 | 1.12 ± 0.3 ** | 1.88 ± 0.14 | 45.87 ± 3.97 | ns | 1 |
| Pure drug solution, Nebulized | 7.46 ± 1.55 | 4 | 0.093 ± 0.04 ** | 8.53 ± 3.33 ** | 7.43 ± 3.11 ** | 42.03 ± 9.70 | 1.86 | 0.92 |
| INH-NLC, Nebulized | 5.51 ± 0.4 ** | 8 | 0.027 ± 0.01 | 26.80 ± 6.39 | 18.81 ± 2.91 | 100.85 ± 3.83 | 4.45 | 2.10 |
| Man-INH-NLC, Nebulized | 2.72 ± 0.24 ** | 24 | −0.0174 ± 0.001 | 40.06 ± 3.78 | 51.11 ± 2.46 | 118.61 ± 8.28 | 5.24 | 2.89 |
| Formulation Code | Liver Function Test | Kidney Function Test | ||||
|---|---|---|---|---|---|---|
| ALT (IU/L) | ALP (IU/L) | AST (IU/L) | Urea (mg/dL) | Bilirubin (mg/dL) | Creatinine (mg/dL) | |
| Untreated control | 38.64 ± 5.33 | 153.51 ± 10.29 | 34.71 ± 3.62 | 15.17 ± 1.36 | 0.39 ± 0.07 | 1.13 ± 0.09 |
| The oral, pure drug solution | 103.77 ± 7.21 | 379.99 ± 13.47 | 96.52 ± 10.72 | 25.63 ± 2.68 | 0.62 ± 0.16 | 1.65 ± 0.10 |
| IV, the pure drug solution | 97.058 ± 5.64 | 371.66 ± 14.75 | 103.68 ± 3.38 | 27.69 ± 3.36 | 0.68 ± 0.15 | 1.75 ± 0.13 |
| The nebulized, pure drug solution | 98.47 ± 8.61 | 359.25 ± 5.73 | 87.27 ± 7.39 | 23.71 ± 2.91 | 0.61 ± 0.17 | 2.01 ± 0.24 |
| Nebulized, blank Man-NLC | 53.64 ± 2.81 ** | 171.12 ± 10.75 | 42.77 ± 7.87 | 16.43 ± 1.13 ** | 0.48 ± 0.03 ** | 1.25 ± 0.12 ** |
| Nebulized, Man-INH-NLC | 39.78 ± 6.26 | 193.64 ± 5.81 | 49.13 ± 9.44 ** | 18.98 ± 0.67 | 0.43 ± 0.09 ** | 1.31 ± 0.12 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahalwat, S.; Bhatt, D.C.; Rohilla, S.; Jogpal, V.; Sharma, K.; Virmani, T.; Kumar, G.; Alhalmi, A.; Alqahtani, A.S.; Noman, O.M.; et al. Mannose-Functionalized Isoniazid-Loaded Nanostructured Lipid Carriers for Pulmonary Delivery: In Vitro Prospects and In Vivo Therapeutic Efficacy Assessment. Pharmaceuticals 2023, 16, 1108. https://doi.org/10.3390/ph16081108
Ahalwat S, Bhatt DC, Rohilla S, Jogpal V, Sharma K, Virmani T, Kumar G, Alhalmi A, Alqahtani AS, Noman OM, et al. Mannose-Functionalized Isoniazid-Loaded Nanostructured Lipid Carriers for Pulmonary Delivery: In Vitro Prospects and In Vivo Therapeutic Efficacy Assessment. Pharmaceuticals. 2023; 16(8):1108. https://doi.org/10.3390/ph16081108
Chicago/Turabian StyleAhalwat, Shaveta, Dinesh Chandra Bhatt, Surbhi Rohilla, Vikas Jogpal, Kirti Sharma, Tarun Virmani, Girish Kumar, Abdulsalam Alhalmi, Ali S. Alqahtani, Omar M. Noman, and et al. 2023. "Mannose-Functionalized Isoniazid-Loaded Nanostructured Lipid Carriers for Pulmonary Delivery: In Vitro Prospects and In Vivo Therapeutic Efficacy Assessment" Pharmaceuticals 16, no. 8: 1108. https://doi.org/10.3390/ph16081108