Intravitreal Anti-Vascular Endothelial Growth Factor Therapies for Retinal Disorders
Abstract
:1. Introduction
2. Retinal Disorders That Benefit from Anti-VEGF Therapies
2.1. Choroidal Neovascularization
2.1.1. Exudative Age-Related Macular Degeneration
2.1.2. Polypoidal Choroidal Vasculopathy
2.1.3. Other Retinal Entities Associated with Choroidal Neovascularization
2.2. Retinal Neovascularization
2.2.1. Proliferative Diabetic Retinopathy
2.2.2. Retinal Vein Occlusion
2.2.3. Iris Neovascularization/Neovascular Glaucoma
2.2.4. Retinopathy of Prematurity
2.3. Macular Edema
2.3.1. Diabetic Macular Edema
2.3.2. Retinal Vein Occlusion
2.3.3. Radiation Retinopathy
2.4. Other Indications
2.4.1. Retinal Artery Macroaneurysm
2.4.2. Peripheral Exudative Hemorrhagic Chorioretinopathy
3. Intravitreal Anti-VEGF Therapies for Retinal Disorders
3.1. Pegaptanib
3.2. Bevacizumab
3.3. Ranibizumab
3.4. Aflibercept
3.5. Brolucizumab
3.6. Faricimab
4. Discussion
5. Future Directions: Emerging Anti-VEGF Therapies
5.1. Port Delivery System
5.2. Anti-VEGF Biosimilars
5.3. DARPins
5.4. Thermosensitive Hydrogels
5.5. Tyrosine Kinase Inhibitors
5.6. Adjuvant Radiotherapy
5.7. Gene Therapy
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AMD | Age-related macular degeneration |
| Anti-VEGF | Drugs that inhibit vascular endothelial growth factor |
| BRVO | Branch retinal vein occlusion |
| CRVO | Central retinal vein occlusion |
| DARPins | Designed ankyrin repeat proteins |
| DME | diabetic macular edema |
| DR | Diabetic retinopathy |
| EG-VEGF | Endocrine gland-derived vascular endothelial growth factor |
| IOI | Intraocular inflammation |
| IOP | Intraocular pressure |
| ME | Macular edema |
| NP-1 | Neuropilin-1 |
| NP-2 | Neurophilin-2 |
| NPDR | Non-proliferative diabetic retinopathy |
| PCV | Polypoidal choroidal vasculopathy |
| PDR | Proliferative diabetic retinopathy |
| PDT | Photodynamic therapy |
| PlGF | Placental growth factor |
| POHS | Presumed ocular histoplasmosis syndrome |
| PRP | Panretinal laser photocoagulation |
| RPE | Retinal pigment epithelium |
| RVO | Retinal vein occlusion |
| VEGF | Vascular endothelial growth factor |
| VEGFR | Vascular endothelial growth factor receptor |
References
- Ide, A. Vascularization of the Brown-Pearce rabbit epithelioma transplant as seen in the transparent ear chamber. Am. J. Roentgenol. 1939, 42, 891. [Google Scholar]
- Ferrara, N. From the discovery of vascular endothelial growth factor to the introduction of avastin in clinical trials—An interview with Napoleone Ferrara by Domenico Ribatti. Int. J. Dev. Biol. 2011, 55, 383–388. [Google Scholar] [PubMed] [Green Version]
- Melincovici, C.S.; Boşca, A.B.; Şuşman, S.; Mărginean, M.; Mihu, C.; Istrate, M.; Moldovan, I.M.; Roman, A.L.; Mihu, C.M. Vascular endothelial growth factor (VEGF)—Key factor in normal and pathological angiogenesis. Rom. J. Morphol. Embryol. 2018, 59, 455–467. [Google Scholar] [PubMed]
- Shibuya, M. Vascular Endothelial Growth Factor (VEGF) and Its Receptor (VEGFR) Signaling in Angiogenesis: A Crucial Target for Anti- and Pro-Angiogenic Therapies. Genes Cancer 2011, 2, 1097–1105. [Google Scholar] [CrossRef]
- Yonekura, H.; Sakurai, S.; Liu, X.; Migita, H.; Wang, H.; Yamagishi, S.; Nomura, M.; Abedin, M.J.; Unoki, H.; Yamamoto, Y.; et al. Placenta growth factor and vascular endothelial growth factor B and C expression in microvascular endothelial cells and pericytes. Implication in autocrine and paracrine regulation of angiogenesis. J. Biol. Chem. 1999, 274, 35172–35178. [Google Scholar] [CrossRef] [Green Version]
- Ferrara, N. VEGF-A: A critical regulator of blood vessel growth. Eur. Cytokine Netw. 2009, 20, 158–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferrara, N.; Gerber, H.P.; LeCouter, J. The biology of VEGF and its receptors. Nat. Med. 2003, 9, 669–676. [Google Scholar] [CrossRef]
- Penn, J.S.; Madan, A.; Caldwell, R.B.; Bartoli, M.; Caldwell, R.W.; Hartnett, M.E. Vascular endothelial growth factor in eye disease. Prog. Retin. Eye Res. 2008, 27, 331–371. [Google Scholar] [CrossRef] [Green Version]
- Bhisitkul, R.B. Vascular endothelial growth factor biology: Clinical implications for ocular treatments. Br. J. Ophthalmol. 2006, 90, 1542–1547. [Google Scholar] [CrossRef]
- Senger, D.R.; Galli, S.J.; Dvorak, A.M.; Perruzzi, C.A.; Harvey, V.S.; Dvorak, H.F. Tumor cells secrete a vascular permeability factor that promotes accumulation of ascites fluid. Science 1983, 219, 983–985. [Google Scholar] [CrossRef]
- Leung, D.W.; Cachianes, G.; Kuang, W.J.; Goeddel, D.V.; Ferrara, N. Vascular endothelial growth factor is a secreted angiogenic mitogen. Science 1989, 246, 1306–1309. [Google Scholar] [CrossRef]
- Ferrara, N.; Henzel, W.J. Pituitary follicular cells secrete a novel heparin-binding growth factor specific for vascular endothelial cells. Biochem. Biophys. Res. Commun. 1989, 161, 851–858. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, K.; Khosrof, S.; Bursell, S.E.; Moromizato, Y.; Aiello, L.P.; Ogura, Y.; Adamis, A.P. Vascular endothelial growth factor (VEGF)-induced retinal vascular permeability is mediated by intercellular adhesion molecule-1 (ICAM-1). Am. J. Pathol. 2000, 156, 1733–1739. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azzouz, M.; Ralph, G.S.; Storkebaum, E.; Walmsley, L.E.; Mitrophanous, K.A.; Kingsman, S.M.; Carmeliet, P.; Mazarakis, N.D. VEGF delivery with retrogradely transported lentivector prolongs survival in a mouse ALS model. Nature 2004, 429, 413–417. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.M.; Mao, B.Y.; Jiang, S.; Li, S.F.; Deng, Y.L. Neuroprotective effect of exogenous vascular endothelial growth factor on rat spinal cord neurons in vitro hypoxia. Chin. Med. J. 2005, 118, 1644–1650. [Google Scholar]
- Marneros, A.G.; Fan, J.; Yokoyama, Y.; Gerber, H.P.; Ferrara, N.; Crouch, R.K.; Olsen, B.R. Vascular endothelial growth factor expression in the retinal pigment epithelium is essential for choriocapillaris development and visual function. Am. J. Pathol. 2005, 167, 1451–1459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martin, A.C.; Thornton, J.D.; Liu, J.; Wang, X.; Zuo, J.; Jablonski, M.M.; Chaum, E.; Zindy, F.; Skapek, S.X. Pathogenesis of persistent hyperplastic primary vitreous in mice lacking the arf tumor suppressor gene. Investig. Ophthalmol. Vis. Sci. 2004, 45, 3387–3396. [Google Scholar] [CrossRef] [Green Version]
- Spaide, R.F.; Curcio, C.A. Drusen characterization with multimodal imaging. Retina 2010, 30, 1441–1454. [Google Scholar] [CrossRef] [Green Version]
- Yang, S.; Zhou, J.; Li, D. Functions and Diseases of the Retinal Pigment Epithelium. Front. Pharmacol. 2021, 12, 727870. [Google Scholar] [CrossRef]
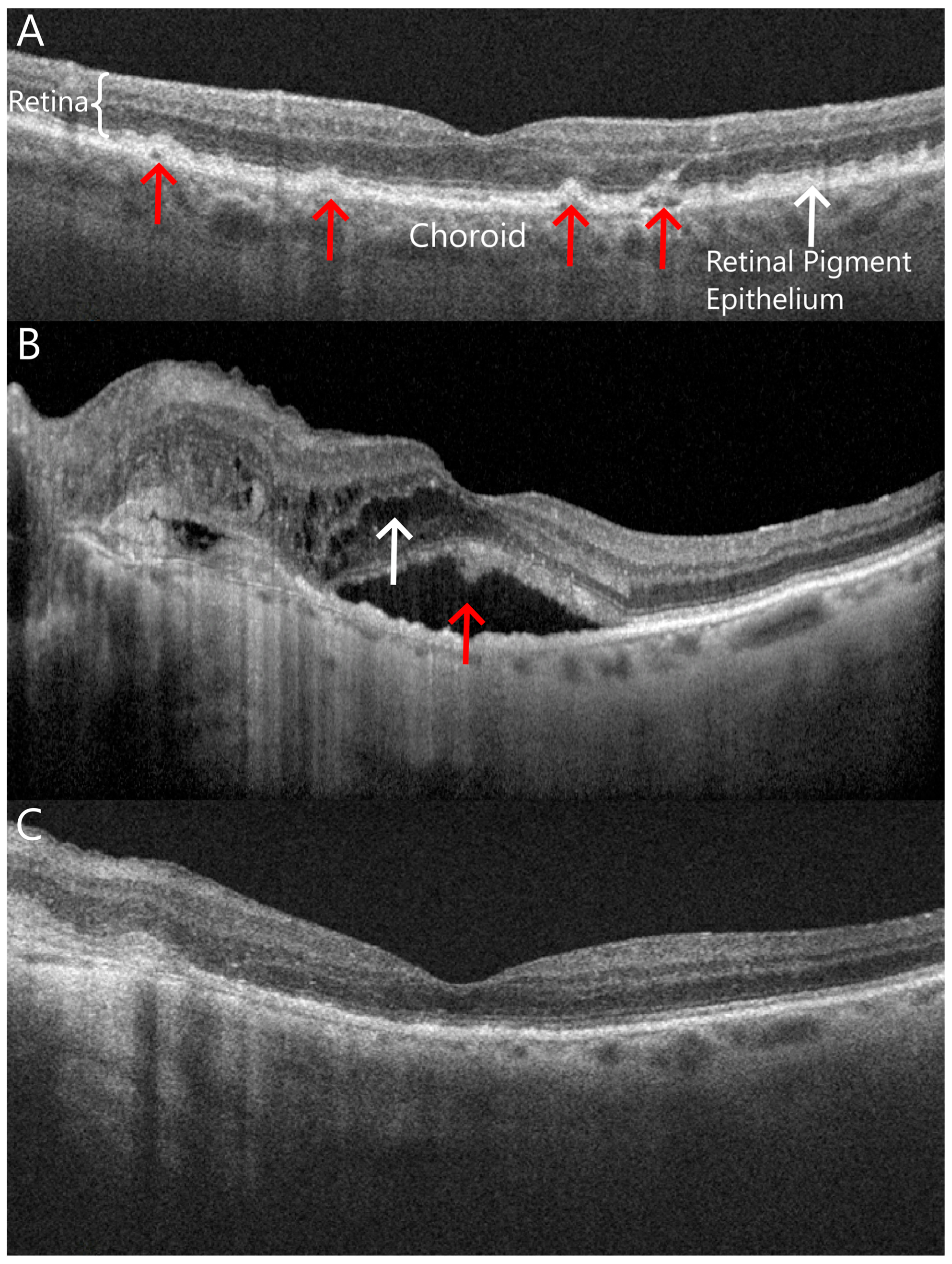
- Tagawa, M.; Ooto, S.; Yamashiro, K.; Tamura, H.; Oishi, A.; Miyata, M.; Hata, M.; Yoshikawa, M.; Yoshimura, N.; Tsujikawa, A. Characteristics of pachychoroid neovasculopathy. Sci. Rep. 2020, 10, 16248. [Google Scholar] [CrossRef]
- Yamashiro, K.; Yanagi, Y.; Koizumi, H.; Matsumoto, H.; Cheung, C.M.G.; Gomi, F.; Iida, T.; Tsujikawa, A. Relationship between Pachychoroid and Polypoidal Choroidal Vasculopathy. J. Clin. Med. 2022, 11, 4614. [Google Scholar] [CrossRef]
- Cheung, C.M.G.; Lai, T.Y.Y.; Ruamviboonsuk, P.; Chen, S.J.; Chen, Y.; Freund, K.B.; Gomi, F.; Koh, A.H.; Lee, W.K.; Wong, T.Y. Polypoidal Choroidal Vasculopathy: Definition, Pathogenesis, Diagnosis, and Management. Ophthalmology 2018, 125, 708–724. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koh, A.; Lee, W.K.; Chen, L.J.; Chen, S.J.; Hashad, Y.; Kim, H.; Lai, T.Y.; Pilz, S.; Ruamviboonsuk, P.; Tokaji, E.; et al. EVEREST study: Efficacy and safety of verteporfin photodynamic therapy in combination with ranibizumab or alone versus ranibizumab monotherapy in patients with symptomatic macular polypoidal choroidal vasculopathy. Retina 2012, 32, 1453–1464. [Google Scholar] [CrossRef]
- Lim, T.H.; Lai, T.Y.Y.; Takahashi, K.; Wong, T.Y.; Chen, L.J.; Ruamviboonsuk, P.; Tan, C.S.; Lee, W.K.; Cheung, C.M.G.; Ngah, N.F.; et al. Comparison of Ranibizumab With or Without Verteporfin Photodynamic Therapy for Polypoidal Choroidal Vasculopathy: The EVEREST II Randomized Clinical Trial. JAMA Ophthalmol. 2020, 138, 935–942. [Google Scholar] [CrossRef]
- Oishi, A.; Miyamoto, N.; Mandai, M.; Honda, S.; Matsuoka, T.; Oh, H.; Kita, M.; Nagai, T.; Bessho, N.; Uenishi, M.; et al. LAPTOP study: A 24-month trial of verteporfin versus ranibizumab for polypoidal choroidal vasculopathy. Ophthalmology 2014, 121, 1151–1152. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.K.; Iida, T.; Ogura, Y.; Chen, S.J.; Wong, T.Y.; Mitchell, P.; Cheung, G.C.M.; Zhang, Z.; Leal, S.; Ishibashi, T. Efficacy and Safety of Intravitreal Aflibercept for Polypoidal Choroidal Vasculopathy in the PLANET Study: A Randomized Clinical Trial. JAMA Ophthalmol. 2018, 136, 786–793. [Google Scholar] [CrossRef] [PubMed]
- Kokame, G.T.; Lai, J.C.; Wee, R.; Yanagihara, R.; Shantha, J.G.; Ayabe, J.; Hirai, K. Prospective clinical trial of Intravitreal aflibercept treatment for PolypoIdal choroidal vasculopathy with hemorrhage or exudation (EPIC study): 6 month results. BMC Ophthalmol. 2016, 16, 127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seko, Y.; Seko, Y.; Fujikura, H.; Pang, J.; Tokoro, T.; Shimokawa, H. Induction of vascular endothelial growth factor after application of mechanical stress to retinal pigment epithelium of the rat in vitro. Investig. Ophthalmol. Vis. Sci. 1999, 40, 3287–3291. [Google Scholar]
- Tan, C.S.; Sadda, S.R. Anti-vascular endothelial growth factor therapy for the treatment of myopic choroidal neovascularization. Clin. Ophthalmol. 2017, 11, 1741–1746. [Google Scholar] [CrossRef] [Green Version]
- Barth, T.; Zeman, F.; Helbig, H.; Gamulescu, M.A. Intravitreal anti-VEGF treatment for choroidal neovascularization secondary to traumatic choroidal rupture. BMC Ophthalmol. 2019, 19, 239. [Google Scholar] [CrossRef] [Green Version]
- Wong, T.Y.; Sun, J.; Kawasaki, R.; Ruamviboonsuk, P.; Gupta, N.; Lansingh, V.C.; Maia, M.; Mathenge, W.; Moreker, S.; Muqit, M.M.K.; et al. Guidelines on Diabetic Eye Care: The International Council of Ophthalmology Recommendations for Screening, Follow-up, Referral, and Treatment Based on Resource Settings. Ophthalmology 2018, 125, 1608–1622. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Evans, J.R.; Michelessi, M.; Virgili, G. Laser photocoagulation for proliferative diabetic retinopathy. Cochrane Database Syst. Rev. 2014, 2014, Cd011234. [Google Scholar] [CrossRef]
- Gross, J.G.; Glassman, A.R.; Liu, D.; Sun, J.K.; Antoszyk, A.N.; Baker, C.W.; Bressler, N.M.; Elman, M.J.; Ferris, F.L., 3rd; Gardner, T.W.; et al. Five-Year Outcomes of Panretinal Photocoagulation vs Intravitreous Ranibizumab for Proliferative Diabetic Retinopathy: A Randomized Clinical Trial. JAMA Ophthalmol. 2018, 136, 1138–1148. [Google Scholar] [CrossRef] [Green Version]
- Maturi, R.K.; Glassman, A.R.; Josic, K.; Antoszyk, A.N.; Blodi, B.A.; Jampol, L.M.; Marcus, D.M.; Martin, D.F.; Melia, M.; Salehi-Had, H.; et al. Effect of Intravitreous Anti-Vascular Endothelial Growth Factor vs Sham Treatment for Prevention of Vision-Threatening Complications of Diabetic Retinopathy: The Protocol W Randomized Clinical Trial. JAMA Ophthalmol. 2021, 139, 701–712. [Google Scholar] [CrossRef]
- Maturi, R.K.; Glassman, A.R.; Josic, K.; Baker, C.W.; Gerstenblith, A.T.; Jampol, L.M.; Meleth, A.; Martin, D.F.; Melia, M.; Punjabi, O.S.; et al. Four-Year Visual Outcomes in the Protocol W Randomized Trial of Intravitreous Aflibercept for Prevention of Vision-Threatening Complications of Diabetic Retinopathy. JAMA 2023, 329, 376–385. [Google Scholar] [CrossRef]
- Nicholson, L.; Talks, S.J.; Amoaku, W.; Talks, K.; Sivaprasad, S. Retinal vein occlusion (RVO) guideline: Executive summary. Eye 2022, 36, 909–912. [Google Scholar] [CrossRef]
- The Eye Disease Case-Control Study Group. Risk Factors for Central Retinal Vein Occlusion. Arch. Ophthalmol. 1996, 114, 545–554. [Google Scholar]
- Karia, N. Retinal vein occlusion: Pathophysiology and treatment options. Clin. Ophthalmol. 2010, 4, 809–816. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garweg, J.G.; Zandi, S. Retinal vein occlusion and the use of a dexamethasone intravitreal implant (Ozurdex®) in its treatment. Graefes Arch. Clin. Exp. Ophthalmol. 2016, 254, 1257–1265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heier, J.S.; Campochiaro, P.A.; Yau, L.; Li, Z.; Saroj, N.; Rubio, R.G.; Lai, P. Ranibizumab for macular edema due to retinal vein occlusions: Long-term follow-up in the HORIZON trial. Ophthalmology 2012, 119, 802–809. [Google Scholar] [CrossRef]
- Brown, D.M.; Campochiaro, P.A.; Singh, R.P.; Li, Z.; Gray, S.; Saroj, N.; Rundle, A.C.; Rubio, R.G.; Murahashi, W.Y. Ranibizumab for macular edema following central retinal vein occlusion: Six-month primary end point results of a phase III study. Ophthalmology 2010, 117, 1124–1133.e1121. [Google Scholar] [CrossRef]
- Senthil, S.; Dada, T.; Das, T.; Kaushik, S.; Puthuran, G.V.; Philip, R.; Rani, P.K.; Rao, H.; Singla, S.; Vijaya, L. Neovascular glaucoma—A review. Indian J. Ophthalmol. 2021, 69, 525–534. [Google Scholar] [CrossRef] [PubMed]
- Bhatnagar, A.; Skrehot, H.C.; Bhatt, A.; Herce, H.; Weng, C.Y. Epidemiology of Retinopathy of Prematurity in the US From 2003 to 2019. JAMA Ophthalmol. 2023, 141, 479–485. [Google Scholar] [CrossRef] [PubMed]
- Hellström, A.; Smith, L.E.; Dammann, O. Retinopathy of prematurity. Lancet 2013, 382, 1445–1457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mintz-Hittner, H.A.; Kennedy, K.A.; Chuang, A.Z. Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N. Engl. J. Med. 2011, 364, 603–615. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tran, K.D.; Cernichiaro-Espinosa, L.A.; Berrocal, A.M. Management of Retinopathy of Prematurity—Use of Anti-VEGF Therapy. Asia Pac. J. Ophthalmol. 2018, 7, 56–62. [Google Scholar]
- Brownlee, M. The pathobiology of diabetic complications: A unifying mechanism. Diabetes 2005, 54, 1615–1625. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, Q.D.; Brown, D.M.; Marcus, D.M.; Boyer, D.S.; Patel, S.; Feiner, L.; Gibson, A.; Sy, J.; Rundle, A.C.; Hopkins, J.J.; et al. Ranibizumab for diabetic macular edema: Results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology 2012, 119, 789–801. [Google Scholar] [CrossRef]
- Wells, J.A.; Glassman, A.R.; Ayala, A.R.; Jampol, L.M.; Aiello, L.P.; Antoszyk, A.N.; Arnold-Bush, B.; Baker, C.W.; Bressler, N.M.; Browning, D.J.; et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N. Engl. J. Med. 2015, 372, 1193–1203. [Google Scholar] [CrossRef] [Green Version]
- Noma, H.; Yasuda, K.; Shimura, M. Cytokines and Pathogenesis of Central Retinal Vein Occlusion. J. Clin. Med. 2020, 9, 3457. [Google Scholar] [CrossRef]
- Varma, R.; Bressler, N.M.; Suñer, I.; Lee, P.; Dolan, C.M.; Ward, J.; Colman, S.; Rubio, R.G. Improved vision-related function after ranibizumab for macular edema after retinal vein occlusion: Results from the BRAVO and CRUISE trials. Ophthalmology 2012, 119, 2108–2118. [Google Scholar] [CrossRef] [PubMed]
- Heier, J.S.; Clark, W.L.; Boyer, D.S.; Brown, D.M.; Vitti, R.; Berliner, A.J.; Kazmi, H.; Ma, Y.; Stemper, B.; Zeitz, O.; et al. Intravitreal aflibercept injection for macular edema due to central retinal vein occlusion: Two-year results from the COPERNICUS study. Ophthalmology 2014, 121, 1414–1420.e1411. [Google Scholar] [CrossRef] [PubMed]
- Clark, W.L.; Boyer, D.S.; Heier, J.S.; Brown, D.M.; Haller, J.A.; Vitti, R.; Kazmi, H.; Berliner, A.J.; Erickson, K.; Chu, K.W.; et al. Intravitreal Aflibercept for Macular Edema Following Branch Retinal Vein Occlusion: 52-Week Results of the VIBRANT Study. Ophthalmology 2016, 123, 330–336. [Google Scholar] [CrossRef]
- Archer, D.B.; Amoaku, W.M.; Gardiner, T.A. Radiation retinopathy--clinical, histopathological, ultrastructural and experimental correlations. Eye 1991, 5 Pt 2, 239–251. [Google Scholar] [CrossRef]
- Mason, J.O.; Albert, M.A.; Persaud, T.O.; Vail, R.S. Intravitreal bevacizumab treatment for radiation macular edema after plaque radiotherapy for choroidal melanoma. Retina 2007, 27, 903–907. [Google Scholar] [CrossRef]
- Rabb, M.F.; Gagliano, D.A.; Teske, M.P. Retinal arterial macroaneurysms. Surv. Ophthalmol. 1988, 33, 73–96. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.Y.; Lin, L.Y.; Chang, P.Y.; Chen, F.T.; Mai, E.L.C.; Wang, J.K. Laser and Anti-Vascular Endothelial Growth Factor Agent Treatments for Retinal Arterial Macroaneurysm. Asia Pac. J. Ophthalmol. 2017, 6, 444–449. [Google Scholar]
- Takkar, B.; Roy, S.; Sodhi, P.K.; Azad, S.; Bajwa, G.S. Peripheral choroidal neovascular membrane in a case of peripheral exudative hemorrhagic chorioretinopathy managed with combination therapy. Int. Ophthalmol. 2017, 37, 429–431. [Google Scholar] [CrossRef]
- Vinores, S.A. Pegaptanib in the treatment of wet, age-related macular degeneration. Int. J. Nanomed. 2006, 1, 263–268. [Google Scholar]
- Preclinical and phase 1A clinical evaluation of an anti-VEGF pegylated aptamer (EYE001) for the treatment of exudative age-related macular degeneration. Retina 2002, 22, 143–152. [CrossRef]
- Patel, M.; Whitfield, L.; Hutmacher, M.; Kowalski, K.; Burger, P.; Dessalegn, B.; Modi, M.; Group, M.S. Population Pharmacokinetics/Pharmacodynamics (PK/PD) of Pegaptanib Sodium (Macugen®) in Patients with Age–Related Macular Degeneration (AMD). Investig. Ophthalmol. Vis. Sci. 2006, 47, 2623. [Google Scholar]
- Gragoudas, E.S.; Adamis, A.P.; Cunningham, E.T.; Jr Feinsod, M.; Guyer, D.R. Pegaptanib for neovascular age-related macular degeneration. N. Engl. J. Med. 2004, 351, 2805–2816. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stewart, M.W. Vascular Endothelial Growth Factor Inhibitor Use in Ophthalmology: The Revolution Continues. Curr. Drug Ther. 2012, 7, 77–79. [Google Scholar] [CrossRef]
- Ferrara, N.; Hillan, K.J.; Gerber, H.P.; Novotny, W. Discovery and development of bevacizumab, an anti-VEGF antibody for treating cancer. Nat. Rev. Drug Discov. 2004, 3, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Grisanti, S.; Ziemssen, F. Bevacizumab: Off-label use in ophthalmology. Indian J. Ophthalmol. 2007, 55, 417–420. [Google Scholar] [CrossRef]
- Michels, S.; Rosenfeld, P.J.; Puliafito, C.A.; Marcus, E.N.; Venkatraman, A.S. Systemic bevacizumab (Avastin) therapy for neovascular age-related macular degeneration twelve-week results of an uncontrolled open-label clinical study. Ophthalmology 2005, 112, 1035–1047. [Google Scholar] [CrossRef]
- Rosenfeld, P.J.; Fung, A.E.; Puliafito, C.A. Optical coherence tomography findings after an intravitreal injection of bevacizumab (avastin) for macular edema from central retinal vein occlusion. Ophthalmic Surg. Lasers Imaging 2005, 36, 336–339. [Google Scholar] [CrossRef]
- Rosenfeld, P.J.; Moshfeghi, A.A.; Puliafito, C.A. Optical coherence tomography findings after an intravitreal injection of bevacizumab (avastin) for neovascular age-related macular degeneration. Ophthalmic Surg. Lasers Imaging 2005, 36, 331–335. [Google Scholar] [CrossRef]
- Michaelides, M.; Kaines, A.; Hamilton, R.D.; Fraser-Bell, S.; Rajendram, R.; Quhill, F.; Boos, C.J.; Xing, W.; Egan, C.; Peto, T.; et al. A prospective randomized trial of intravitreal bevacizumab or laser therapy in the management of diabetic macular edema (BOLT study) 12-month data: Report 2. Ophthalmology 2010, 117, 1078–1086.e2. [Google Scholar] [CrossRef]
- Gillies, M.C.; Lim, L.L.; Campain, A.; Quin, G.J.; Salem, W.; Li, J.; Goodwin, S.; Aroney, C.; McAllister, I.L.; Fraser-Bell, S. A randomized clinical trial of intravitreal bevacizumab versus intravitreal dexamethasone for diabetic macular edema: The BEVORDEX study. Ophthalmology 2014, 121, 2473–2481. [Google Scholar] [CrossRef]
- Martin, D.F.; Maguire, M.G.; Ying, G.S.; Grunwald, J.E.; Fine, S.L.; Jaffe, G.J. Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N. Engl. J. Med. 2011, 364, 1897–1908. [Google Scholar] [PubMed] [Green Version]
- Afarid, M.; Sadegi Sarvestani, A.; Rahat, F.; Azimi, A. Intravitreal Injection of Bevacizumab: Review of our previous Experience. Iran. J. Pharm. Res. 2018, 17, 1093–1098. [Google Scholar] [PubMed]
- Modarreszadeh, M.; Naseripour, M.; Ghasemi-Falavarjani, K.; Nikeghbali, A.; Hashemi, M.; Parvaresh, M.M. Two Different Doses of Intravitreal Bevacizumab for Treatment of Choroidal Neovascularization Associated with Age-related Macular Degeneration. J. Ophthalmic Vis. Res. 2008, 3, 102–107. [Google Scholar] [PubMed]
- Wu, L.; Arevalo, J.F.; Roca, J.A.; Maia, M.; Berrocal, M.H.; Rodriguez, F.J.; Evans, T.; Costa, R.A.; Cardillo, J. Comparison of two doses of intravitreal bevacizumab (Avastin) for treatment of macular edema secondary to branch retinal vein occlusion: Results from the Pan-American Collaborative Retina Study Group at 6 months of follow-up. Retina 2008, 28, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Jan, S.; Nazim, M.; Karim, S.; Hussain, Z. Intravitreal Bevacizumab: Indications And Complications. J. Ayub Med. Coll. Abbottabad 2016, 28, 364–368. [Google Scholar]
- Fasih, U.; Shaikh, N.; Rahman, A.; Sultan, S.; Fehmi, M.S.; Shaikh, A. A one-year follow-up study of ocular and systemic complications of intravitreal injection of bevacizumab (Avastin). J. Pak. Med. Assoc. 2013, 63, 707–710. [Google Scholar]
- VanderBeek, B.L.; Bonaffini, S.G.; Ma, L. Association of compounded bevacizumab with postinjection endophthalmitis. JAMA Ophthalmol. 2015, 133, 1159–1164. [Google Scholar] [CrossRef] [Green Version]
- Kim, L.A.; D’Amore, P.A. A brief history of anti-VEGF for the treatment of ocular angiogenesis. Am. J. Pathol. 2012, 181, 376–379. [Google Scholar] [CrossRef] [Green Version]
- Lien, S.; Lowman, H.B. Therapeutic anti-VEGF antibodies. Handb. Exp. Pharmacol. 2008, 181, 131–150. [Google Scholar]
- Joo, K.; Park, S.J.; Choi, Y.; Lee, J.E.; Na, Y.M.; Hong, H.K.; Park, K.H.; Kim, H.M.; Chung, J.Y.; Woo, S.J. Role of the Fc Region in the Vitreous Half-Life of Anti-VEGF Drugs. Investig. Ophthalmol. Vis. Sci. 2017, 58, 4261–4267. [Google Scholar] [CrossRef] [Green Version]
- Rosenfeld, P.J.; Brown, D.M.; Heier, J.S.; Boyer, D.S.; Kaiser, P.K.; Chung, C.Y.; Kim, R.Y. Ranibizumab for neovascular age-related macular degeneration. N. Engl. J. Med. 2006, 355, 1419–1431. [Google Scholar] [CrossRef] [Green Version]
- Brown, D.M.; Kaiser, P.K.; Michels, M.; Soubrane, G.; Heier, J.S.; Kim, R.Y.; Sy, J.P.; Schneider, S. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N. Engl. J. Med. 2006, 355, 1432–1444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boyer, D.S.; Heier, J.S.; Brown, D.M.; Francom, S.F.; Ianchulev, T.; Rubio, R.G. A Phase IIIb study to evaluate the safety of ranibizumab in subjects with neovascular age-related macular degeneration. Ophthalmology 2009, 116, 1731–1739. [Google Scholar] [CrossRef] [PubMed]
- Vaidyanathan, U.; Moshirfar, M. Ranibizumab. In StatPearls; StatPearls Publishing LLC: Treasure Island, FL, USA, 2023. [Google Scholar]
- Adams, B.S.; Sorhaitz, W.; Stringham, J. Aflibercept. In StatPearls; StatPearls Publishing LLC: Treasure Island, FL, USA, 2023. [Google Scholar]
- Papadopoulos, N.; Martin, J.; Ruan, Q.; Rafique, A.; Rosconi, M.P.; Shi, E.; Pyles, E.A.; Yancopoulos, G.D.; Stahl, N.; Wiegand, S.J. Binding and neutralization of vascular endothelial growth factor (VEGF) and related ligands by VEGF Trap, ranibizumab and bevacizumab. Angiogenesis 2012, 15, 171–185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stewart, M.W.; Rosenfeld, P.J. Predicted biological activity of intravitreal VEGF Trap. Br. J. Ophthalmol. 2008, 92, 667–668. [Google Scholar] [CrossRef] [PubMed]
- Autiero, M.; Waltenberger, J.; Communi, D.; Kranz, A.; Moons, L.; Lambrechts, D.; Kroll, J.; Plaisance, S.; De Mol, M.; Bono, F.; et al. Role of PlGF in the intra- and intermolecular cross talk between the VEGF receptors Flt1 and Flk1. Nat. Med. 2003, 9, 936–943. [Google Scholar] [CrossRef]
- Heier, J.S.; Brown, D.M.; Chong, V.; Korobelnik, J.F.; Kaiser, P.K.; Nguyen, Q.D.; Kirchhof, B.; Ho, A.; Ogura, Y.; Yancopoulos, G.D.; et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology 2012, 119, 2537–2548. [Google Scholar] [CrossRef]
- Schmidt-Erfurth, U.; Kaiser, P.K.; Korobelnik, J.F.; Brown, D.M.; Chong, V.; Nguyen, Q.D.; Ho, A.C.; Ogura, Y.; Simader, C.; Jaffe, G.J.; et al. Intravitreal aflibercept injection for neovascular age-related macular degeneration: Ninety-six-week results of the VIEW studies. Ophthalmology 2014, 121, 193–201. [Google Scholar] [CrossRef]
- Heier, J.S.; Korobelnik, J.F.; Brown, D.M.; Schmidt-Erfurth, U.; Do, D.V.; Midena, E.; Boyer, D.S.; Terasaki, H.; Kaiser, P.K.; Marcus, D.M.; et al. Intravitreal Aflibercept for Diabetic Macular Edema: 148-Week Results from the VISTA and VIVID Studies. Ophthalmology 2016, 123, 2376–2385. [Google Scholar] [CrossRef]
- Pielen, A.; Clark, W.L.; Boyer, D.S.; Ogura, Y.; Holz, F.G.; Korobelnik, J.F.; Stemper, B.; Asmus, F.; Rittenhouse, K.D.; Ahlers, C.; et al. Integrated results from the COPERNICUS and GALILEO studies. Clin. Ophthalmol. 2017, 11, 1533–1540. [Google Scholar] [CrossRef] [Green Version]
- Wells, J.A.; Glassman, A.R.; Ayala, A.R.; Jampol, L.M.; Bressler, N.M.; Bressler, S.B.; Brucker, A.J.; Ferris, F.L.; Hampton, G.R.; Jhaveri, C.; et al. Aflibercept, Bevacizumab, or Ranibizumab for Diabetic Macular Edema: Two-Year Results from a Comparative Effectiveness Randomized Clinical Trial. Ophthalmology 2016, 123, 1351–1359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wykoff, C.C.; Brown, D.M.; Reed, K.; Berliner, A.J.; Gerstenblith, A.T.; Breazna, A.; Abraham, P.; Fein, J.G.; Chu, K.W.; Clark, W.L.; et al. Effect of High-Dose Intravitreal Aflibercept, 8 mg, in Patients With Neovascular Age-Related Macular Degeneration: The Phase 2 CANDELA Randomized Clinical Trial. JAMA Ophthalmol. 2023. [CrossRef]
- Iyer, P.G.; Albini, T.A. Drug-related adverse effects of antivascular endothelial growth factor agents. Curr. Opin. Ophthalmol. 2021, 32, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Markham, A. Brolucizumab: First Approval. Drugs 2019, 79, 1997–2000. [Google Scholar] [CrossRef] [PubMed]
- Gaudreault, J.; Gunde, T.; Floyd, H.S.; Ellis, J.; Tietz, J.; Binggeli, D.; Keller, B.; Schmidt, A.; Escher, D. Preclinical pharmacology and safety of ESBA1008, a single-chain antibody fragment, investigated as potential treatment for age related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2012, 53, 3025. [Google Scholar]
- Dugel, P.U.; Koh, A.; Ogura, Y.; Jaffe, G.J.; Schmidt-Erfurth, U.; Brown, D.M.; Gomes, A.V.; Warburton, J.; Weichselberger, A.; Holz, F.G. HAWK and HARRIER: Phase 3, Multicenter, Randomized, Double-Masked Trials of Brolucizumab for Neovascular Age-Related Macular Degeneration. Ophthalmology 2020, 127, 72–84. [Google Scholar] [CrossRef]
- Tietz, J.; Spohn, G.; Schmid, G.; Konrad, J.; Jampen, S.; Maurer, P.; Schmidt, A.; Escher, D. Affinity and potency of RTH258 (ESBA1008), a novel inhibitor of vascular endothelial growth factor a for the treatment of retinal disorders. Investig. Ophthalmol. Vis. Sci. 2015, 56, 1501. [Google Scholar]
- Dugel, P.U.; Singh, R.P.; Koh, A.; Ogura, Y.; Weissgerber, G.; Gedif, K.; Jaffe, G.J.; Tadayoni, R.; Schmidt-Erfurth, U.; Holz, F.G. HAWK and HARRIER: Ninety-Six-Week Outcomes from the Phase 3 Trials of Brolucizumab for Neovascular Age-Related Macular Degeneration. Ophthalmology 2021, 128, 89–99. [Google Scholar] [CrossRef]
- Mehta, N.; Fong, R.D.; Wilson, M.; Moussa, K.; Emami-Naeini, P.; Moshiri, A.; Yiu, G.; Park, S.S. Real-World Experience Using Intravitreal Brolucizumab Alone or in Combination with Aflibercept in the Management of Neovascular Age-Related Macular Degeneration. Clin. Ophthalmol. 2023, 17, 657–665. [Google Scholar] [CrossRef]
- Brown, D.M.; Emanuelli, A.; Bandello, F.; Barranco, J.J.E.; Figueira, J.; Souied, E.; Wolf, S.; Gupta, V.; Ngah, N.F.; Liew, G.; et al. KESTREL and KITE: 52-Week Results From Two Phase III Pivotal Trials of Brolucizumab for Diabetic Macular Edema. Am. J. Ophthalmol. 2022, 238, 157–172. [Google Scholar] [CrossRef]
- Baumal, C.R.; Spaide, R.F.; Vajzovic, L.; Freund, K.B.; Walter, S.D.; John, V.; Rich, R.; Chaudhry, N.; Lakhanpal, R.R.; Oellers, P.R.; et al. Retinal Vasculitis and Intraocular Inflammation after Intravitreal Injection of Brolucizumab. Ophthalmology 2020, 127, 1345–1359. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.; Chea, S.; Matsumiya, W.; Halim, M.S.; Yaşar, Ç.; Kuang, G.; Sepah, Y.J.; Khanani, A.M.; Do, D.V.; Nguyen, Q.D. Severe vision loss secondary to retinal arteriolar occlusions after multiple intravitreal brolucizumab administrations. Am. J. Ophthalmol. Case Rep. 2020, 18, 100687. [Google Scholar] [CrossRef] [PubMed]
- Singer, M.; Albini, T.A.; Seres, A.; Baumal, C.R.; Parikh, S.; Gale, R.; Kaiser, P.K.; Lobach, I.; Feltgen, N.; Joshi, M.R.; et al. Clinical Characteristics and Outcomes of Eyes with Intraocular Inflammation after Brolucizumab: Post Hoc Analysis of HAWK and HARRIER. Ophthalmol. Retin. 2022, 6, 97–108. [Google Scholar] [CrossRef]
- Shirley, M. Faricimab: First Approval. Drugs 2022, 82, 825–830. [Google Scholar] [CrossRef] [PubMed]
- Khanani, A.M.; Russell, M.W.; Aziz, A.A.; Danzig, C.J.; Weng, C.Y.; Eichenbaum, D.A.; Singh, R.P. Angiopoietins as Potential Targets in Management of Retinal Disease. Clin. Ophthalmol. 2021, 15, 3747–3755. [Google Scholar] [CrossRef]
- Heier, J.S.; Khanani, A.M.; Quezada Ruiz, C.; Basu, K.; Ferrone, P.J.; Brittain, C.; Figueroa, M.S.; Lin, H.; Holz, F.G.; Patel, V.; et al. Efficacy, durability, and safety of intravitreal faricimab up to every 16 weeks for neovascular age-related macular degeneration (TENAYA and LUCERNE): Two randomised, double-masked, phase 3, non-inferiority trials. Lancet 2022, 399, 729–740. [Google Scholar] [CrossRef]
- Wykoff, C.C.; Abreu, F.; Adamis, A.P.; Basu, K.; Eichenbaum, D.A.; Haskova, Z.; Lin, H.; Loewenstein, A.; Mohan, S.; Pearce, I.A.; et al. Efficacy, durability, and safety of intravitreal faricimab with extended dosing up to every 16 weeks in patients with diabetic macular oedema (YOSEMITE and RHINE): Two randomised, double-masked, phase 3 trials. Lancet 2022, 399, 741–755. [Google Scholar] [CrossRef]
- Rasier, R.; Artunay, O.; Yuzbasioglu, E.; Sengul, A.; Bahcecioglu, H. The effect of intravitreal bevacizumab (avastin) administration on systemic hypertension. Eye 2009, 23, 1714–1718. [Google Scholar] [CrossRef]
- Sengul, A.; Rasier, R.; Ciftci, C.; Artunay, O.; Kockar, A.; Bahcecioglu, H.; Yuzbasioglu, E. Short-term effects of intravitreal ranibizumab and bevacizumab administration on 24-h ambulatory blood pressure monitoring recordings in normotensive patients with age-related macular degeneration. Eye 2017, 31, 677–683. [Google Scholar] [CrossRef]
- Thulliez, M.; Angoulvant, D.; Le Lez, M.L.; Jonville-Bera, A.P.; Pisella, P.J.; Gueyffier, F.; Bejan-Angoulvant, T. Cardiovascular events and bleeding risk associated with intravitreal antivascular endothelial growth factor monoclonal antibodies: Systematic review and meta-analysis. JAMA Ophthalmol. 2014, 132, 1317–1326. [Google Scholar] [CrossRef]
- Holekamp, N.M.; Campochiaro, P.A.; Chang, M.A.; Miller, D.; Pieramici, D.; Adamis, A.P.; Brittain, C.; Evans, E.; Kaufman, D.; Maass, K.F. Archway randomized phase 3 trial of the port delivery system with ranibizumab for neovascular age-related macular degeneration. Ophthalmology 2022, 129, 295–307. [Google Scholar] [CrossRef] [PubMed]
- Regillo, C.; Berger, B.; Brooks, L.; Clark, W.L.; Mittra, R.; Wykoff, C.C.; Callaway, N.F.; DeGraaf, S.; Ding, H.T.; Fung, A.E.; et al. Archway Phase 3 Trial of the Port Delivery System with Ranibizumab for Neovascular Age-Related Macular Degeneration 2-Year Results. Ophthalmology 2023, 130, 735–747. [Google Scholar] [CrossRef]
- Sharma, A.; Khanani, A.M.; Parachuri, N.; Kumar, N.; Bandello, F.; Kuppermann, B.D. Port delivery system with ranibizumab (Susvimo) recall- What does it mean to the retina specialists. Int. J. Retina Vitr. 2023, 9, 6. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Ophthalmology; Academy Board of Trustees. The Use of Biosimilars in Ophthalmic Practice—2022. Available online: https://www.aao.org/education/clinical-statement/use-of-biosimilars-in-ophthalmic-practice (accessed on 30 June 2023).
- Sharma, A.; Kumar, N.; Kuppermann, B.D.; Francesco, B.; Lowenstein, A. Ophthalmic biosimilars: Lessons from India. Indian J. Ophthalmol. 2019, 67, 1384–1385. [Google Scholar] [CrossRef]
- Sharma, A.; Kumar, N.; Kuppermann, B.D.; Bandello, F.; Loewenstein, A. Ophthalmic biosimilars and biologics-role of endotoxins. Eye 2020, 34, 614–615. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, P.K.; Schmitz-Valckenberg, M.S.; Holz, F.G. Anti-Vascular Endothelial Growth Factor Biosimilars in Ophthalmology. Retina 2022, 42, 2243–2250. [Google Scholar] [CrossRef] [PubMed]
- Comparing the Efficacy and Safety of Biosimilar Candidate Xlucane Versus Lucentis® in Patients with nAMD (XPLORE). Available online: https://classic.clinicaltrials.gov/ct2/show/NCT03805100 (accessed on 30 June 2023).
- Kapur, M.; Nirula, S.; Naik, M.P. Future of anti-VEGF: Biosimilars and biobetters. Int. J. Retina Vitreous 2022, 8, 2. [Google Scholar] [CrossRef]
- Outlook Therapeutics Presents NORSE TWO Phase 3 Pivotal Safety and Efficacy Data for ONS-5010/LYTENAVA™ (Bevacizumab-Vikg) at the Retina Subspecialty Day, American Academy of Ophthalmology (AAO) 2021 Annual Conference. Available online: https://ir.outlooktherapeutics.com/news-releases/news-release-details/outlook-therapeutics-presents-norse-two-phase-3-pivotal-safety (accessed on 30 June 2023).
- Stumpp, M.T.; Binz, H.K.; Amstutz, P. DARPins: A new generation of protein therapeutics. Drug Discov. Today 2008, 13, 695–701. [Google Scholar] [CrossRef] [PubMed]
- Khurana, R.N.; Kunimoto, D.; Yoon, Y.H.; Wykoff, C.C.; Chang, A.; Maturi, R.K.; Agostini, H.; Souied, E.; Chow, D.R.; Lotery, A.J.; et al. Two-Year Results of the Phase 3 Randomized Controlled Study of Abicipar in Neovascular Age-Related Macular Degeneration. Ophthalmology 2021, 128, 1027–1038. [Google Scholar] [CrossRef]
- Kunimoto, D.; Yoon, Y.H.; Wykoff, C.C.; Chang, A.; Khurana, R.N.; Maturi, R.K.; Agostini, H.; Souied, E.; Chow, D.R.; Lotery, A.J.; et al. Efficacy and Safety of Abicipar in Neovascular Age-Related Macular Degeneration: 52-Week Results of Phase 3 Randomized Controlled Study. Ophthalmology 2020, 127, 1331–1344. [Google Scholar] [CrossRef]
- Sharma, A.; Kumar, N.; Kuppermann, B.D.; Bandello, F. Abicipar pegol: The non-monoclonal antibody anti-VEGF. Eye 2020, 34, 797–801. [Google Scholar] [CrossRef] [PubMed]
- Callanan, D.; Khurana, R.N.; Maturi, R.K.; Patel, S.; Wykoff, C.C.; Eichenbaum, D.; Khanani, A.M.; Hassan, T.; Badger, H.; Mehta, S.; et al. Impact of Modifying Abicipar Manufacturing Process in Patients with Neovascular Age-Related Macular Degeneration: MAPLE Study Results. Clin. Ophthalmol. 2023, 17, 1367–1384. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Mooney, D.J. Designing hydrogels for controlled drug delivery. Nat. Rev. Mater. 2016, 1, 16071. [Google Scholar] [CrossRef] [PubMed]
- Matanović, M.R.; Kristl, J.; Grabnar, P.A. Thermoresponsive polymers: Insights into decisive hydrogel characteristics, mechanisms of gelation, and promising biomedical applications. Int. J. Pharm. 2014, 472, 262–275. [Google Scholar] [CrossRef]
- Kim, S.; Kang-Mieler, J.J.; Liu, W.; Wang, Z.; Yiu, G.; Teixeira, L.B.C.; Mieler, W.F.; Thomasy, S.M. Safety and Biocompatibility of Aflibercept-Loaded Microsphere Thermo-Responsive Hydrogel Drug Delivery System in a Nonhuman Primate Model. Transl. Vis. Sci. Technol. 2020, 9, 30. [Google Scholar] [CrossRef] [Green Version]
- Hussain, R.M.; Shaukat, B.A.; Ciulla, L.M.; Berrocal, A.M.; Sridhar, J. Vascular Endothelial Growth Factor Antagonists: Promising Players in the Treatment of Neovascular Age-Related Macular Degeneration. Drug Des. Devel Ther. 2021, 15, 2653–2665. [Google Scholar] [CrossRef]
- Le Tourneau, C.; Raymond, E.; Faivre, S. Sunitinib: A novel tyrosine kinase inhibitor. A brief review of its therapeutic potential in the treatment of renal carcinoma and gastrointestinal stromal tumors (GIST). Ther. Clin. Risk Manag. 2007, 3, 341–348. [Google Scholar] [CrossRef] [Green Version]
- Samanta, A.; Aziz, A.A.; Jhingan, M.; Singh, S.R.; Khanani, A.M.; Chhablani, J. Emerging Therapies in Neovascular Age-Related Macular Degeneration in 2020. Asia Pac. J. Ophthalmol. 2020, 9, 250–259. [Google Scholar] [CrossRef]
- Tolentino, M.J.; Tolentino, A.J. Investigational drugs in clinical trials for macular degeneration. Expert. Opin. Investig. Drugs 2022, 31, 1067–1085. [Google Scholar] [CrossRef]
- Osmanovic, S.; Moisseiev, E.; Mishra, K.K.; Daftari, I.; Moshiri, A.; Morse, L.; Park, S.S. Phase I/II Randomized Study of Proton Beam with Anti-Vascular Endothelial Growth Factor for Exudative Age-Related Macular Degeneration: One-Year Results. Ophthalmol. Retin. 2017, 1, 217–226. [Google Scholar] [CrossRef]
- Mukkamala, L.K.; Mishra, K.; Daftari, I.; Moshiri, A.; Park, S.S. Phase I/II randomized study of proton beam with anti-VEGF for exudative age-related macular degeneration: Long-term results. Eye 2020, 34, 2271–2279. [Google Scholar] [CrossRef]
- Dugel, P.U.; Bebchuk, J.D.; Nau, J.; Reichel, E.; Singer, M.; Barak, A.; Binder, S.; Jackson, T.L. Epimacular brachytherapy for neovascular age-related macular degeneration: A randomized, controlled trial (CABERNET). Ophthalmology 2013, 120, 317–327. [Google Scholar] [CrossRef] [PubMed]
- Maguire, A.M.; Bennett, J.; Aleman, E.M.; Leroy, B.P.; Aleman, T.S. Clinical Perspective: Treating RPE65-Associated Retinal Dystrophy. Mol. Ther. 2021, 29, 442–463. [Google Scholar] [CrossRef] [PubMed]
- Adverum Biotechnologies, Inc. Adverum Biotechnologies Announces First Subject Dosed with Ixo-Vec in the Phase 2 LUNA Trial for the Treatment of Wet Age-Related Macular Degeneration. Available online: https://investors.adverum.com/news/news-details/2022/Adverum-Biotechnologies-Announces-First-Subject-Dosed-with-Ixo-vec-in-the-Phase-2-LUNA-Trial-for-the-Treatment-of-Wet-Age-Related-Macular-Degeneration/default.aspx (accessed on 1 July 2023).
- Chung, S.H.; Frick, S.L.; Yiu, G. Targeting vascular endothelial growth factor using retinal gene therapy. Ann. Transl. Med. 2021, 9, 1277. [Google Scholar] [CrossRef]
- Grishanin, R.; Vuillemenot, B.; Sharma, P.; Keravala, A.; Greengard, J.; Gelfman, C.; Blumenkrantz, M.; Lawrence, M.; Hu, W.; Kiss, S.; et al. Preclinical Evaluation of ADVM-022, a Novel Gene Therapy Approach to Treating Wet Age-Related Macular Degeneration. Mol. Ther. 2019, 27, 118–129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khanani, A.M.; Kiss, S.; Turpcu, A.; Hoang, C.; Osborne, A. Phase 1 study of intravitreal gene therapy ADVM-022 for neovascular AMD (OPTIC Trial). Investig. Ophthalmol. Vis. Sci. 2020, 61, 1154. [Google Scholar]

| Drug | Structure | Target | Standard Dose | FDA-Approved Clinical Indications | Landmark Clinical Trials | FDA Approval Date |
|---|---|---|---|---|---|---|
| Pegaptanib | 28 nucleotide RNA aptamer with a 5’-attachment of polyethylene glycol | VEGF-A165 | 0.3 mg/0.09 mL | AMD | AMD: VISION [62] | 2004 |
| Bevacizumab | Recombinant humanized monoclonal IgG1 antibody | All isoforms of VEGF-A | 1.25 mg/0.05 mL | Off-label for ophthalmic use | AMD: CATT [71] DME: BOLT [69], BEVORDEX [70] | Off-label for ophthalmic use |
| Ranibizumab | Recombinant humanized monoclonal IgG1 kappa antibody fragment | All isoforms of VEGF-A | 0.3 mg/0.05 mL or 0.5 mg/0.05 mL | AMD, DR, DME, ME due to RVO, myopic choroidal neovascularization | AMD: MARINA [81], ANCHOR [82] DME: RISE, RIDE [48] RVO: BRAVO, CRUISE [51] | 2006 |
| Aflibercept | Soluble decoy receptor comprised of an Fc fragment of IgG1 fused to binding domains of VEGFR-1 and VEGFR-2 | All isoforms of VEGF-A, VEGF-B, and placental growth factor | 2.0 mg/0.05 mL | AMD, DR, DME, ME due to RVO, retinopathy of prematurity | AMD: VIEW 1, VIEW 2 [90] DME: VISTA, VIVID [91] RVO: COPERNICUS, GALILEO [92] | 2011 |
| Brolucizumab | Humanized monoclonal single-chain variable fragment (scFv) | All isoforms of VEGF-A | 6.0 mg/0.05 mL | AMD, DME | AMD: HAWK, HARRIER [98] DME: KESTREL, KITE [102] | 2019 |
| Faricimab | IgG1-derived bispecific monoclonal antibody | Angiopoietin-2 and all isoforms of VEGF-A | 6.0 mg/0.05 mL | AMD, DME | AMD: TENAYA, LUCERNE [108] DME: RHINE, YOSEMITE [109] | 2022 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hang, A.; Feldman, S.; Amin, A.P.; Ochoa, J.A.R.; Park, S.S. Intravitreal Anti-Vascular Endothelial Growth Factor Therapies for Retinal Disorders. Pharmaceuticals 2023, 16, 1140. https://doi.org/10.3390/ph16081140
Hang A, Feldman S, Amin AP, Ochoa JAR, Park SS. Intravitreal Anti-Vascular Endothelial Growth Factor Therapies for Retinal Disorders. Pharmaceuticals. 2023; 16(8):1140. https://doi.org/10.3390/ph16081140
Chicago/Turabian StyleHang, Abraham, Samuel Feldman, Aana P. Amin, Jorge A. Rivas Ochoa, and Susanna S. Park. 2023. "Intravitreal Anti-Vascular Endothelial Growth Factor Therapies for Retinal Disorders" Pharmaceuticals 16, no. 8: 1140. https://doi.org/10.3390/ph16081140
APA StyleHang, A., Feldman, S., Amin, A. P., Ochoa, J. A. R., & Park, S. S. (2023). Intravitreal Anti-Vascular Endothelial Growth Factor Therapies for Retinal Disorders. Pharmaceuticals, 16(8), 1140. https://doi.org/10.3390/ph16081140






