Evaluating the Role of Neddylation Modifications in Kidney Renal Clear Cell Carcinoma: An Integrated Approach Using Bioinformatics, MLN4924 Dosing Experiments, and RNA Sequencing
Abstract
:1. Introduction
- Maturation: The maturation of NEDD8, a crucial process in cellular regulation, begins with the decarboxylation and removal of the C-terminal precursor sequence from NEDD8 precursors. This step is mediated by two key enzymes, NEDD8-specific protease 1 (NEDP1) and ubiquitin C-terminal hydrolase L3 (UCHL3) [2]. NEDP1 plays a specific role in cleaving the C-terminal sequence of NEDD8 precursors, thereby producing active NEDD8 [16]. Concurrently, UCHL3 assists in the elimination of the C-terminal precursor sequence and also contributes to the decarboxylation process during maturation [17]. The activities of these enzymes are vital, as they ensure the proper maturation of NEDD8.
- Activation: The activation of NEDD8 is carried out by the NEDD8 activating enzyme (NAE), which is composed of two subunits: NAE1 and ubiquitin-like modifier-activating enzyme 3 (UBA3) [18]. In this step, the mature NEDD8 forms a high-energy thioester bond with a cysteine residue within NAE’s active site [19]. This activation of NEDD8 is a critical juncture, as the now active NEDD8 can bind to neddylation substrates [20]. This binding plays a pivotal role in the recognition of CRLs and the ubiquitination of tumor-related proteins [20]. In recent years, MLN4924 has become well-known as a small molecule inhibitor specifically targeting the neddylation pathway [21]. It inhibits the NAE, which is essential for the neddylation process [21]. By inhibiting NAE, MLN4924 effectively blocks the neddylation of cullin proteins, leading to the inactivation of CRLs [22]. This approach highlights the potential of targeting post-translational modification systems in the development of new cancer treatments.
- Conjugation: Once NEDD8 is activated, it is loaded onto the NAE, setting the stage for its transfer to the neddylation E2-conjugating enzymes, specifically ubiquitin-conjugating enzyme E2 M (UBE2M) and UBE2F [23]. This transfer is facilitated by a trans-thiolation reaction, a critical biochemical mechanism that effectively moves NEDD8 from NAE to the E2 enzyme [24,25]. This step ensures the proper positioning and readiness of NEDD8 for subsequent steps in the protein modification process.
- Ligation: In the substrate neddylation phase, the final step involves a substrate-specific E3 ligase (either RING-box protein 1/2 (RBX1/2) or DCN1), which plays a crucial role in transferring NEDD8 from the E2 enzyme to the substrate protein [5,26]. This intricate process leads to the formation of a covalent bond between NEDD8 and a lysine residue on the target protein, effectively completing the neddylation process [26]. This step is essential for the regulation of protein function and stability within the cell.
2. Results
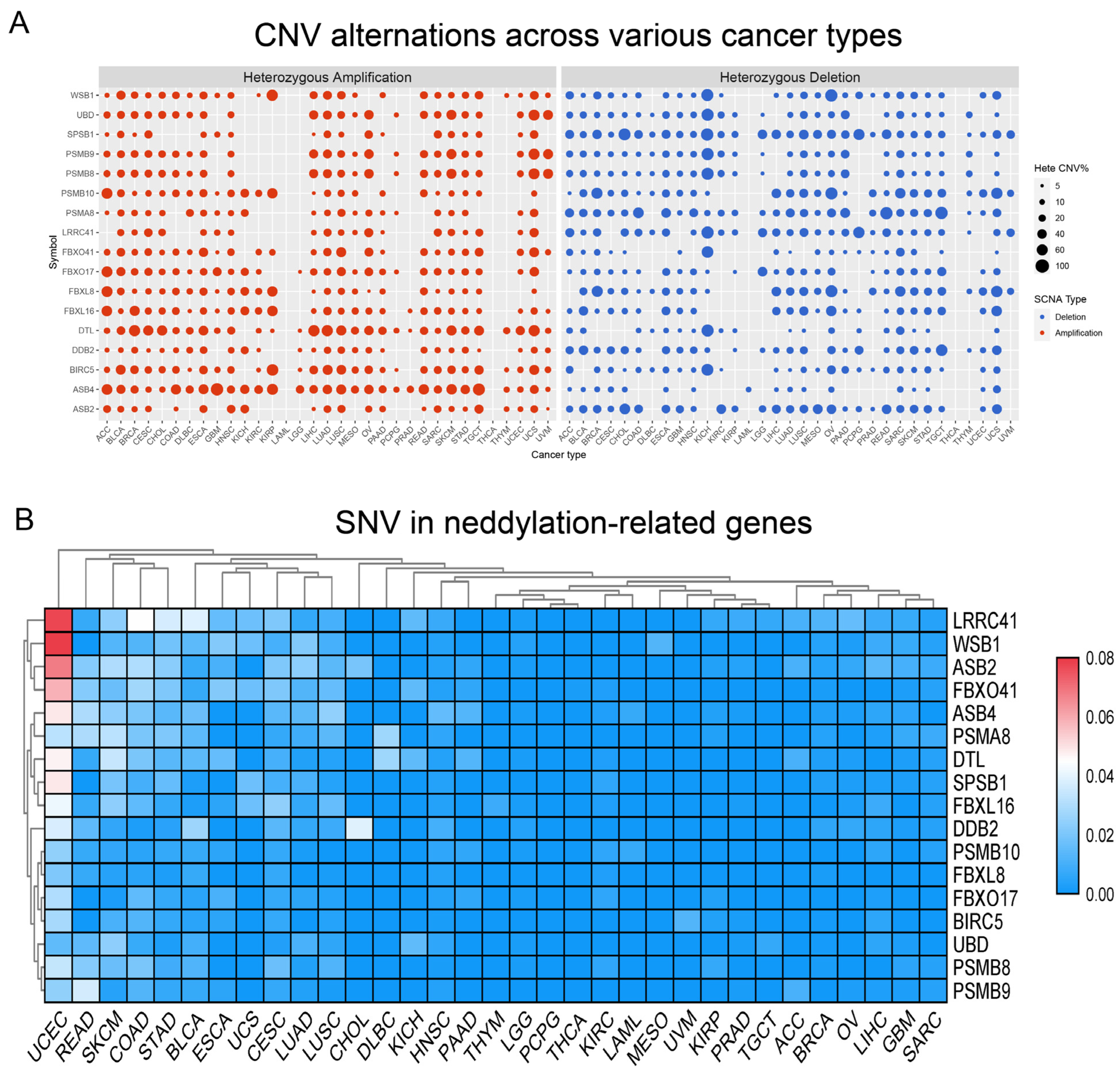
2.1. Prevalent Mutations in Neddylation-Related Genes
2.2. Neddylation-Related Genes: The Association and Clinical Significance between Methylation and KIRC
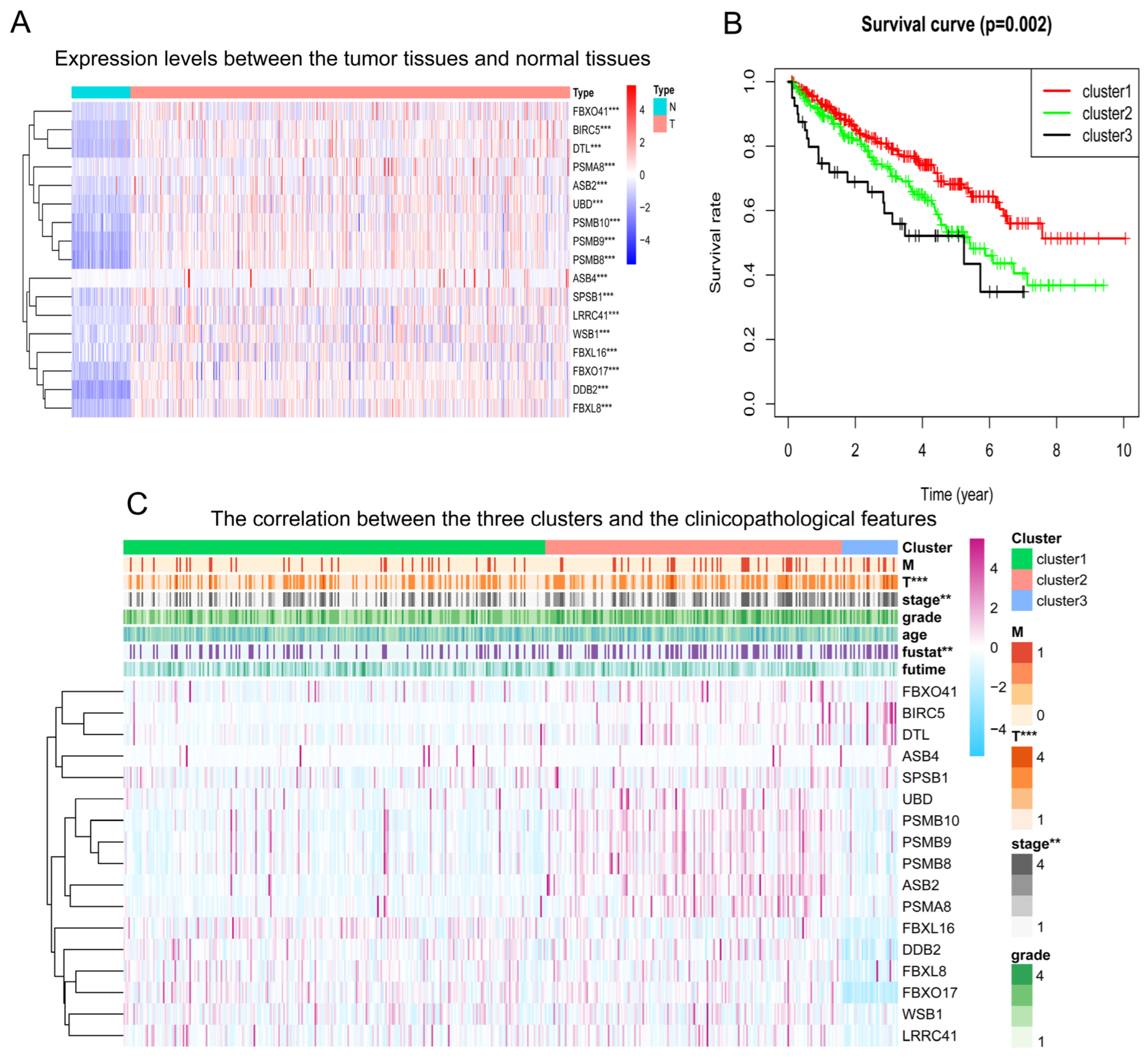
2.3. Impact of Neddylation Pathway Scores on Prognosis in KIRC
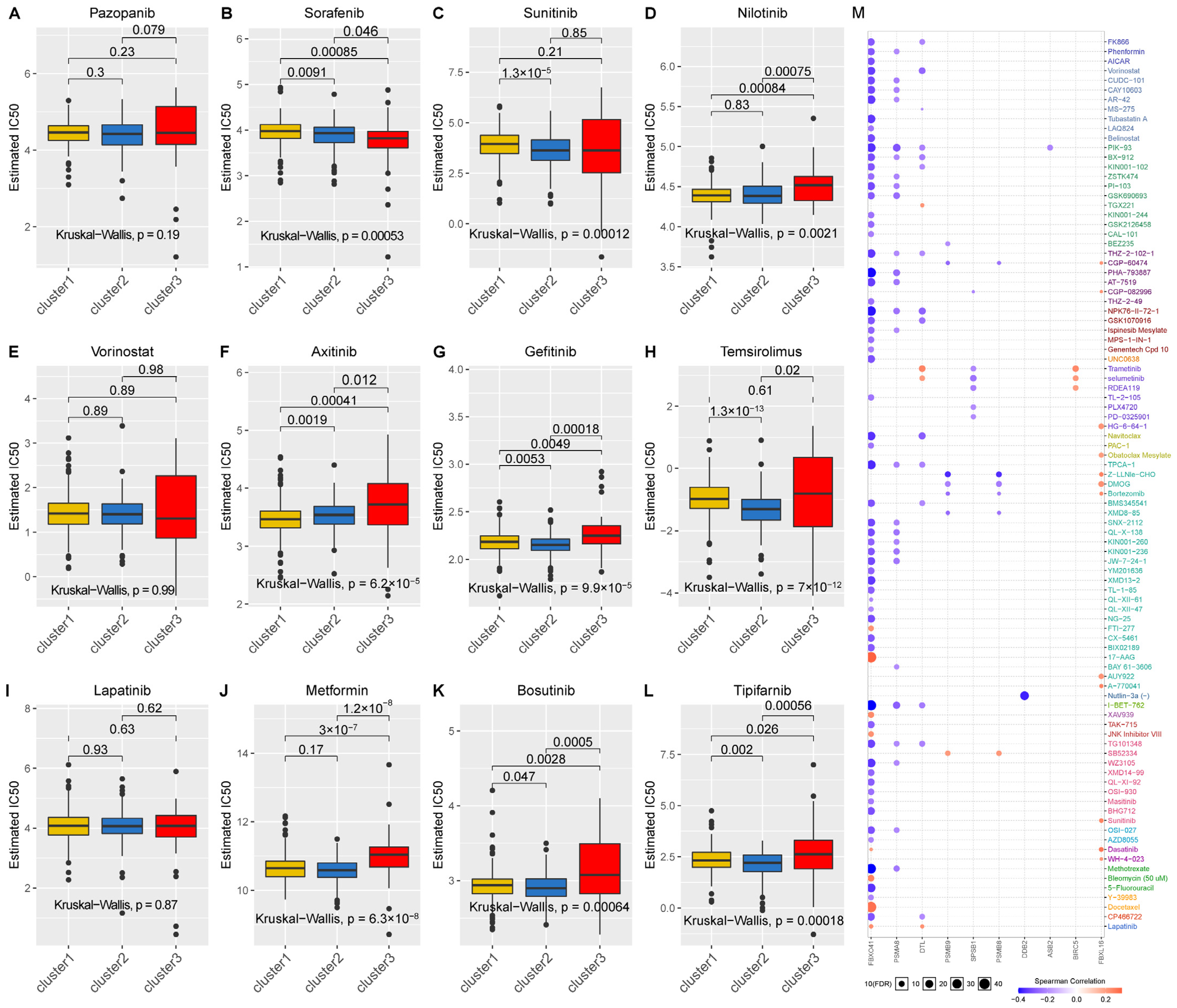
2.4. Relationship between Neddylation Clusters and Drug Sensitivity
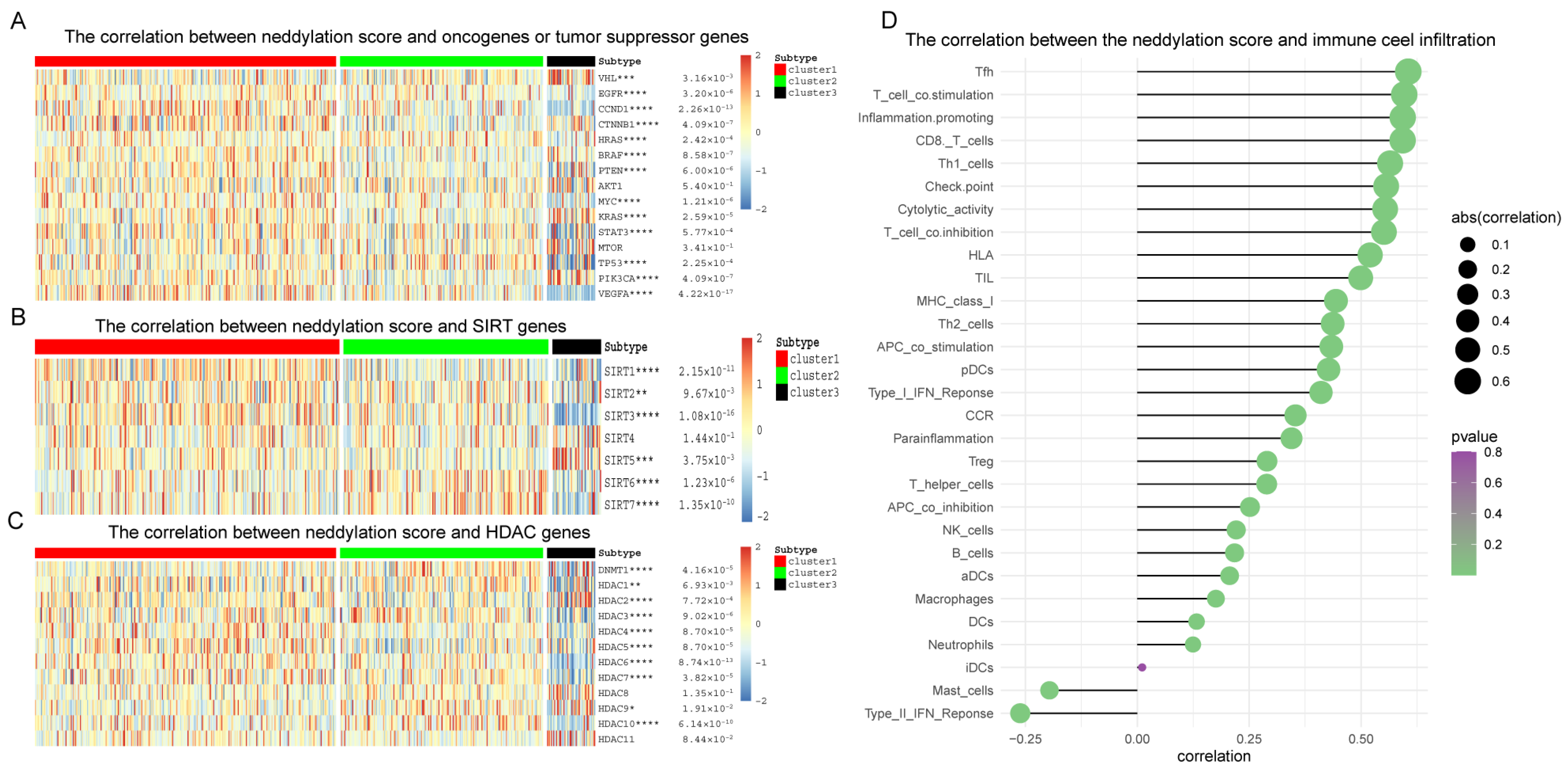
2.5. The Impact of the Neddylation Score on Classical Oncogenes and Immune Infiltration
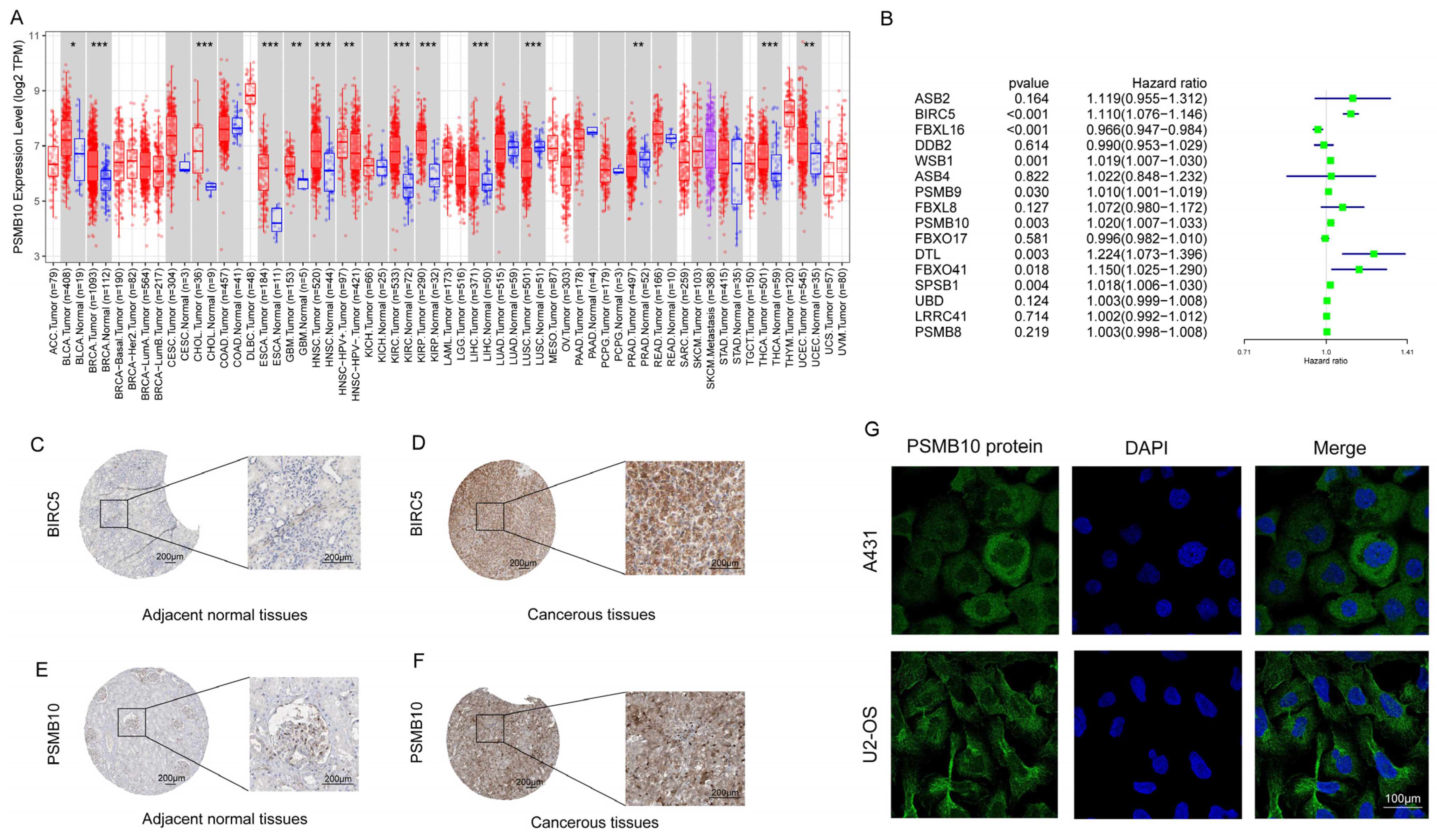
2.6. Screening for Neddylation-Related Genes with Specific Effects on KIRC
2.7. In Vitro Dosing Experiments Elucidate the Pivotal Role of Neddylation Modification in Determining the Phenotype of KIRC
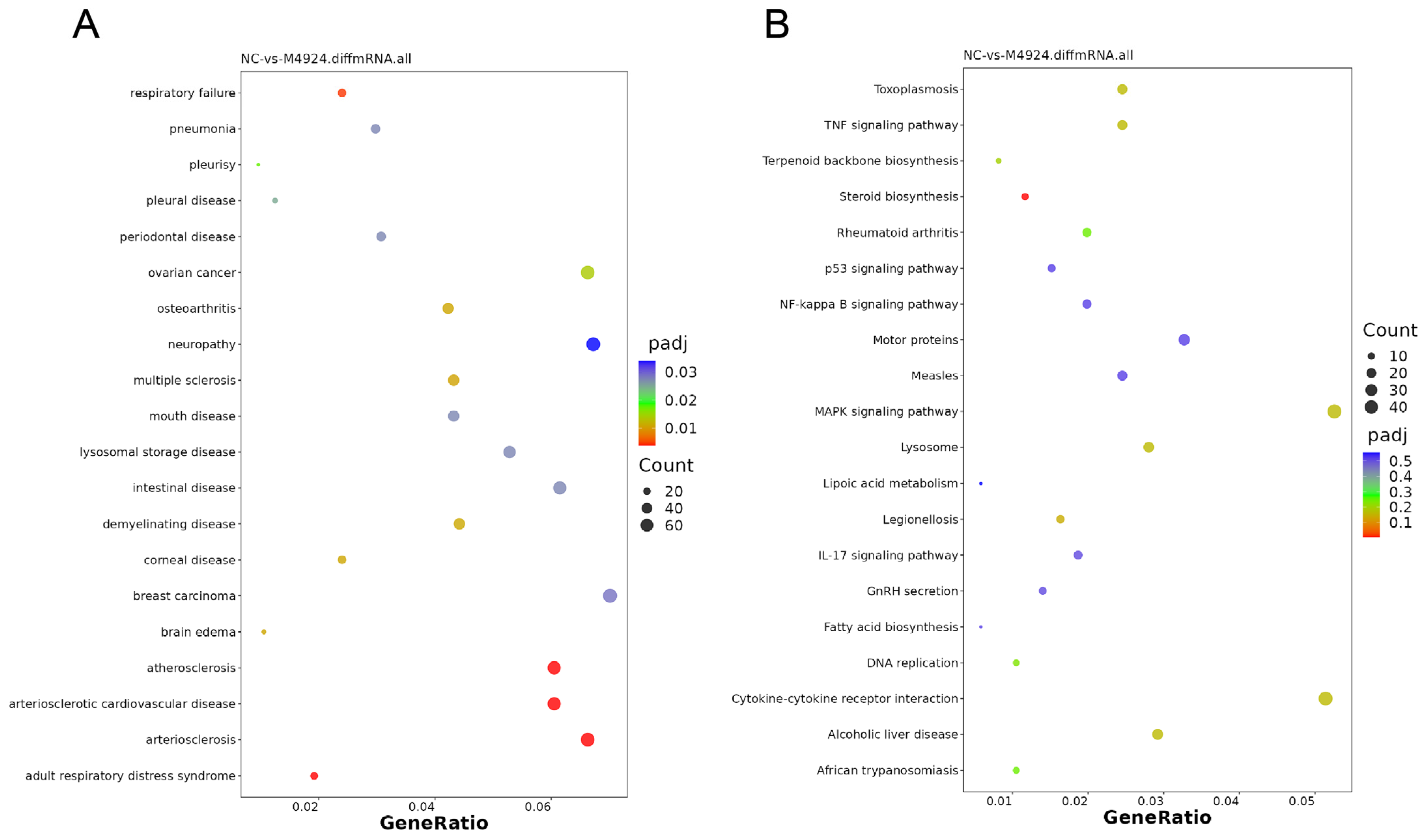
2.8. Deciphering the Impact and Underlying Mechanisms of MLN4924 Treatment on KIRC Cell Lines through RNA Sequencing Analysis
2.9. In Vitro Analysis Reveals the Targeted Therapeutic Potential of PSMB10 in KIRC
3. Discussion
4. Materials and Methods
4.1. Date Extraction Processing
4.2. Methylation
4.3. Cluster Analysis
4.4. Drug Sensitivity
4.5. Classic Cancer-Related Genes and Histone Modifications
4.6. Immune Cell Infiltration
4.7. Screening Specific Genes
4.8. Cell Culture
4.9. RNA Sequencing
4.10. Cell Transfection (Six-Well Plate as an Example)
4.11. Quantitative Real-Time PCR
4.12. Immunofluorescence
4.13. CCK-8 Cell Proliferation Assay
4.14. Colony Formation
4.15. Transwell Invasion Experiment
4.16. Cell Migration Experiment
4.17. Wound Healing Assay
4.18. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Glossary
| ASB | Ankyrin repeat and SOCS box protein |
| BCA3 | Breast cancer-associated protein 3 |
| BIRC5 | Baculoviral IAP repeat containing 5 |
| CCK-8 | Cell Counting Kit-8 |
| CNV | Copy number variation |
| CRLs | Cullin-RING ligases |
| CSN | COP9 signalosome |
| CTNNB1 | Catenin beta 1 |
| DDB2 | DNA damage-binding protein 2 |
| DMEM | Dulbecco’s modified Eagle medium |
| DNMT1 | DNA methyltransferase 1 |
| DTL | Denticleless E3 ubiquitin protein ligase homolog |
| EMT | Epithelial-mesenchymal transition |
| FBXL | F-box and leucine-rich repeat protein |
| FBXO | F-box protein |
| FBS | Fetal bovine serum |
| GAPDH | Glyceraldehyde-3-phosphate dehydrogenase |
| GDSC | Genomics of drug sensitivity in cancer |
| GSCALite | Gene Set Cancer Analysis Lite |
| GSVA | Gene Set Variation Analysis |
| HDACs | Histone deacetylases |
| HPA | Human protein atlas |
| IC50 | Half-maximal inhibitory concentration |
| IFN | Interferon |
| KIRC | Kidney renal clear cell carcinoma |
| LAML | Acute myeloid leukemia |
| LGG | Brain lower-grade glioma |
| LRRC41 | Leucine-rich repeat containing 41 |
| MEM | Minimum essential medium |
| NAE | NEDD8 activating enzyme |
| NEDD8 | Neuronal precursor cell-expressed developmentally down-regulated protein 8 |
| NEDP1 | NEDD8-specific protease 1 |
| PBS | Phosphate-buffered saline |
| PCPG | Pheochromocytoma and paraganglioma |
| PSMA | Proteasome 20S subunit alpha |
| PSMB | Proteasome 20S subunit beta |
| RBX1/2 | RING-box protein 1/2 |
| RCC | Renal cell carcinoma |
| SARC | Sarcoma |
| SIRT | Sirtuin |
| SNV | Single nucleotide variation |
| SPSB1 | SplA/Ryanodine receptor domain and SOCS box containing 1 |
| TCGA | The Cancer Genome Atlas |
| THCA | Thyroid carcinoma |
| TME | Tumor microenvironment |
| UBA3 | Ubiquitin-like modifier-activating enzyme 3 |
| UBD | Ubiquitin D |
| UBE2F/M | Ubiquitin-conjugating enzyme E2 F/M |
| UCHL3 | Ubiquitin C-terminal hydrolase L3 |
| WSB1 | WD repeat and SOCS box containing 1 |
References
- Kamitani, T.; Kito, K.; Nguyen, H.P.; Yeh, E.T. Characterization of NEDD8, a developmentally down-regulated ubiquitin-like protein. J. Biol. Chem. 1997, 272, 28557–28562. [Google Scholar] [CrossRef]
- Xirodimas, D.P. Novel substrates and functions for the ubiquitin-like molecule NEDD8. Biochem. Soc. Trans. 2008, 36 Pt 5, 802–806. [Google Scholar] [CrossRef]
- Mergner, J.; Schwechheimer, C. The NEDD8 modification pathway in plants. Front. Plant Sci. 2014, 5, 103. [Google Scholar] [CrossRef]
- Kumar, S.; Yoshida, Y.; Noda, M. Cloning of a cDNA which encodes a novel ubiquitin-like protein. Biochem. Biophys. Res. Commun. 1993, 195, 393–399. [Google Scholar] [CrossRef]
- Enchev, R.I.; Schulman, B.A.; Peter, M. Protein neddylation: Beyond cullin-RING ligases. Nat. Rev. Mol. Cell Biol. 2015, 16, 30–44. [Google Scholar] [CrossRef]
- Zheng, Y.C.; Guo, Y.J.; Wang, B.; Wang, C.; Mamun, M.A.A.; Gao, Y.; Liu, H.M. Targeting neddylation E2s: A novel therapeutic strategy in cancer. J. Hematol. Oncol. 2021, 14, 57. [Google Scholar] [CrossRef]
- Zhao, Y.; Sun, Y. Cullin-RING Ligases as attractive anti-cancer targets. Curr. Pharm. Des. 2013, 19, 3215–3225. [Google Scholar] [CrossRef]
- Chen, Y.; Neve, R.L.; Liu, H. Neddylation dysfunction in Alzheimer’s disease. J. Cell Mol. Med. 2012, 16, 2583–2591. [Google Scholar] [CrossRef]
- Liu, Y.; Tan, X. Viral Manipulations of the Cullin-RING Ubiquitin Ligases. Adv. Exp. Med. Biol. 2020, 1217, 99–110. [Google Scholar]
- Petroski, M.D.; Deshaies, R.J. Function and regulation of cullin-RING ubiquitin ligases. Nat. Rev. Mol. Cell Biol. 2005, 6, 9–20. [Google Scholar] [CrossRef]
- Deshaies, R.J.; Joazeiro, C.A. RING domain E3 ubiquitin ligases. Annu. Rev. Biochem. 2009, 78, 399–434. [Google Scholar] [CrossRef]
- Nakayama, K.I.; Nakayama, K. Ubiquitin ligases: Cell-cycle control and cancer. Nat. Rev. Cancer 2006, 6, 369–381. [Google Scholar] [CrossRef]
- Zhou, L.; Jia, L. Targeting Protein Neddylation for Cancer Therapy. Adv. Exp. Med. Biol. 2020, 1217, 297–315. [Google Scholar]
- Du, M.; Sansores-Garcia, L.; Zu, Z.; Wu, K.K. Cloning and expression analysis of a novel salicylate suppressible gene, Hs-CUL-3, a member of cullin/Cdc53 family. J. Biol. Chem. 1998, 273, 24289–24292. [Google Scholar] [CrossRef]
- Hori, T.; Osaka, F.; Chiba, T.; Miyamoto, C.; Okabayashi, K.; Shimbara, N.; Kato, S.; Tanaka, K. Covalent modification of all members of human cullin family proteins by NEDD8. Oncogene 1999, 18, 6829–6834. [Google Scholar] [CrossRef]
- Shen, L.N.; Liu, H.; Dong, C.; Xirodimas, D.; Naismith, J.H.; Hay, R.T. Structural basis of NEDD8 ubiquitin discrimination by the deNEDDylating enzyme NEDP1. Embo J. 2005, 24, 1341–1351. [Google Scholar] [CrossRef]
- Frickel, E.M.; Quesada, V.; Muething, L.; Gubbels, M.J.; Spooner, E.; Ploegh, H.; Artavanis-Tsakonas, K. Apicomplexan UCHL3 retains dual specificity for ubiquitin and Nedd8 throughout evolution. Cell Microbiol. 2007, 9, 1601–1610. [Google Scholar] [CrossRef]
- Walden, H.; Podgorski, M.S.; Huang, D.T.; Miller, D.W.; Howard, R.J.; Minor, D.L.; Holton, J.M.; Schulman, B.A. The structure of the APPBP1-UBA3-NEDD8-ATP complex reveals the basis for selective ubiquitin-like protein activation by an E1. Mol. Cell. 2003, 12, 1427–1437. [Google Scholar] [CrossRef]
- Soucy, T.A.; Smith, P.G.; Milhollen, M.A.; Berger, A.J.; Gavin, J.M.; Adhikari, S.; Brownell, J.E.; Burke, K.E.; Cardin, D.P.; Critchley, S.; et al. An inhibitor of NEDD8-activating enzyme as a new approach to treat cancer. Nature 2009, 458, 732–736. [Google Scholar] [CrossRef]
- Baek, K.; Krist, D.T.; Prabu, J.R.; Hill, S.; Klügel, M.; Neumaier, L.M.; von Gronau, S.; Kleiger, G.; Schulman, B.A. NEDD8 nucleates a multivalent cullin-RING-UBE2D ubiquitin ligation assembly. Nature 2020, 578, 461–466. [Google Scholar] [CrossRef]
- Mao, H.; Sun, Y. Neddylation-Independent Activities of MLN4924. Adv. Exp. Med. Biol. 2020, 1217, 363–372. [Google Scholar]
- Oladghaffari, M.; Islamian, J.P.; Baradaran, B.; Monfared, A.S. MLN4924 therapy as a novel approach in cancer treatment modalities. J. Chemother. 2016, 28, 74–82. [Google Scholar] [CrossRef]
- Zhou, L.; Lin, X.; Zhu, J.; Zhang, L.; Chen, S.; Yang, H.; Jia, L.; Chen, B. NEDD8-conjugating enzyme E2s: Critical targets for cancer therapy. Cell Death Discov. 2023, 9, 23. [Google Scholar] [CrossRef]
- Gong, L.; Yeh, E.T. Identification of the activating and conjugating enzymes of the NEDD8 conjugation pathway. J. Biol. Chem. 1999, 274, 12036–12042. [Google Scholar] [CrossRef]
- Huang, D.T.; Paydar, A.; Zhuang, M.; Waddell, M.B.; Holton, J.M.; Schulman, B.A. Structural basis for recruitment of Ubc12 by an E2 binding domain in NEDD8’s E1. Mol. Cell. 2005, 17, 341–350. [Google Scholar] [CrossRef]
- Zhao, Y.; Morgan, M.A.; Sun, Y. Targeting Neddylation pathways to inactivate cullin-RING ligases for anticancer therapy. Antioxid. Redox Signal. 2014, 21, 2383–2400. [Google Scholar] [CrossRef]
- Kandala, S.; Kim, I.M.; Su, H. Neddylation and deneddylation in cardiac biology. Am. J. Cardiovasc. Dis. 2014, 4, 140–158. [Google Scholar]
- Enchev, R.I.; Scott, D.C.; da Fonseca, P.C.; Schreiber, A.; Monda, J.K.; Schulman, B.A.; Peter, M.; Morris, E.P. Structural basis for a reciprocal regulation between SCF and CSN. Cell Rep. 2012, 2, 616–627. [Google Scholar] [CrossRef]
- Wei, N.; Deng, X.W. The COP9 signalosome. Annu. Rev. Cell Dev. Biol. 2003, 19, 261–286. [Google Scholar] [CrossRef]
- Xie, P.; Peng, Z.; Chen, Y.; Li, H.; Du, M.; Tan, Y.; Zhang, X.; Lu, Z.; Cui, C.P.; Liu, C.H.; et al. Neddylation of PTEN regulates its nuclear import and promotes tumor development. Cell Res. 2021, 31, 291–311. [Google Scholar] [CrossRef]
- Xie, P.; Zhang, M.; He, S.; Lu, K.; Chen, Y.; Xing, G.; Lu, Y.; Liu, P.; Li, Y.; Wang, S.; et al. The covalent modifier Nedd8 is critical for the activation of Smurf1 ubiquitin ligase in tumorigenesis. Nat. Commun. 2014, 5, 3733. [Google Scholar] [CrossRef]
- Gao, Q.; Yu, G.Y.; Shi, J.Y.; Li, L.H.; Zhang, W.J.; Wang, Z.C.; Yang, L.X.; Duan, M.; Zhao, H.; Wang, X.Y.; et al. Neddylation pathway is up-regulated in human intrahepatic cholangiocarcinoma and serves as a potential therapeutic target. Oncotarget 2014, 5, 7820–7832. [Google Scholar] [CrossRef]
- Xie, P.; Yang, J.P.; Cao, Y.; Peng, L.X.; Zheng, L.S.; Sun, R.; Meng, D.F.; Wang, M.Y.; Mei, Y.; Qiang, Y.Y.; et al. Promoting tumorigenesis in nasopharyngeal carcinoma, NEDD8 serves as a potential theranostic target. Cell Death Dis. 2017, 8, e2834. [Google Scholar] [CrossRef]
- Jia, L.; Soengas, M.S.; Sun, Y. ROC1/RBX1 E3 ubiquitin ligase silencing suppresses tumor cell growth via sequential induction of G2-M arrest, apoptosis, and senescence. Cancer Res. 2009, 69, 4974–4982. [Google Scholar] [CrossRef]
- Abidi, N.; Xirodimas, D.P. Regulation of cancer-related pathways by protein NEDDylation and strategies for the use of NEDD8 inhibitors in the clinic. Endocr. Relat. Cancer 2015, 22, T55–T70. [Google Scholar] [CrossRef]
- Nawrocki, S.T.; Griffin, P.; Kelly, K.R.; Carew, J.S. MLN4924: A novel first-in-class inhibitor of NEDD8-activating enzyme for cancer therapy. Expert. Opin. Investig. Drugs. 2012, 21, 1563–1573. [Google Scholar] [CrossRef]
- Xu, Q.; Lin, G.; Xu, H.; Hu, L.; Wang, Y.; Du, S.; Deng, W.; Hu, W.; Cheng, W.; Jiang, K. MLN4924 neddylation inhibitor promotes cell death in paclitaxel-resistant human lung adenocarcinoma cells. Oncol. Lett. 2018, 15, 515–521. [Google Scholar] [CrossRef]
- Olaverria Salavaggione, G.N.; Duggan, M.C.; Carson, W.E. Analysis of MLN4924 (pevonedistat) as a potential therapeutic agent in malignant melanoma. Melanoma Res. 2018, 28, 390–397. [Google Scholar] [CrossRef]
- Gu, S.; Lin, C.; Li, Y.; Wei, Z.; Cao, B.; Shen, Z.; Deng, H. Neddylation inhibitor MLN4924 sensitizes head and neck squamous carcinoma cells to (S)-10-hydroxycamptothecin. Eur. J. Med. Res. 2023, 28, 326. [Google Scholar] [CrossRef]
- Capitanio, U.; Bensalah, K.; Bex, A.; Boorjian, S.A.; Bray, F.; Coleman, J.; Gore, J.L.; Sun, M.; Wood, C.; Russo, P. Epidemiology of Renal Cell Carcinoma. World J. Oncol. 2020, 11, 79–87. [Google Scholar] [CrossRef]
- Cohen, H.T.; McGovern, F.J. Renal-cell carcinoma. N. Engl. J. Med. 2005, 353, 2477–2490. [Google Scholar] [CrossRef]
- Hsieh, J.J.; Purdue, M.P.; Signoretti, S.; Swanton, C.; Albiges, L.; Schmidinger, M.; Heng, D.Y.; Larkin, J.; Ficarra, V. Renal cell carcinoma. Nat. Rev. Dis. Primers. 2017, 3, 17009. [Google Scholar] [CrossRef]
- Barata, P.C.; Rini, B.I. Treatment of renal cell carcinoma: Current status and future directions. CA Cancer J. Clin. 2017, 67, 507–524. [Google Scholar] [CrossRef]
- Ljungberg, B.; Albiges, L.; Abu-Ghanem, Y.; Bensalah, K.; Dabestani, S.; Fernández-Pello, S.; Giles, R.H.; Hofmann, F.; Hora, M.; Kuczyk, M.A.; et al. European Association of Urology Guidelines on Renal Cell Carcinoma: The 2019 Update. Eur. Urol. 2019, 75, 799–810. [Google Scholar] [CrossRef]
- Frew, I.J.; Moch, H. A clearer view of the molecular complexity of clear cell renal cell carcinoma. Annu. Rev. Pathol. 2015, 10, 263–289. [Google Scholar] [CrossRef]
- Choueiri, T.K.; Halabi, S.; Sanford, B.L.; Hahn, O.; Michaelson, M.D.; Walsh, M.K.; Feldman, D.R.; Olencki, T.; Picus, J.; Small, E.J.; et al. Cabozantinib Versus Sunitinib As Initial Targeted Therapy for Patients With Metastatic Renal Cell Carcinoma of Poor or Intermediate Risk: The Alliance A031203 CABOSUN Trial. J. Clin. Oncol. 2017, 35, 591–597. [Google Scholar] [CrossRef]
- Gray, R.E.; Harris, G.T. Renal Cell Carcinoma: Diagnosis and Management. Am. Fam. Physician 2019, 99, 179–184. [Google Scholar]
- Zhao, J.; Eyzaguirre, E. Clear Cell Papillary Renal Cell Carcinoma. Arch. Pathol. Lab. Med. 2019, 143, 1154–1158. [Google Scholar] [CrossRef]
- Chen, N.X.; Liu, K.; Liu, X.; Zhang, X.X.; Han, D.Y. Induction and Regulation of the Immunoproteasome Subunit β5i (PSMB8) in Laryngeal and Hypopharyngeal Carcinoma Cells. Med. Sci. Monit. 2020, 26, e923621. [Google Scholar] [CrossRef]
- Kim, M.; Serwa, R.A.; Samluk, L.; Suppanz, I.; Kodroń, A.; Stępkowski, T.M.; Elancheliyan, P.; Tsegaye, B.; Oeljeklaus, S.; Wasilewski, M.; et al. Immunoproteasome-specific subunit PSMB9 induction is required to regulate cellular proteostasis upon mitochondrial dysfunction. Nat. Commun. 2023, 14, 4092. [Google Scholar] [CrossRef]
- Reis, J.; Hassan, F.; Guan, X.Q.; Shen, J.; Monaco, J.J.; Papasian, C.J.; Qureshi, A.A.; Van Way, C.W.; Vogel, S.N.; Morrison, D.C.; et al. The immunoproteasomes regulate LPS-induced TRIF/TRAM signaling pathway in murine macrophages. Cell Biochem. Biophys. 2011, 60, 119–126. [Google Scholar] [CrossRef]
- Agrawal, Y.; Sharma, T.; Islam, S.; Nadkarni, K.S.; Santra, M.K. F-box protein FBXO41 suppresses breast cancer growth by inducing autophagic cell death through facilitating proteasomal degradation of oncogene SKP2. Int. J. Biochem. Cell Biol. 2022, 147, 106228. [Google Scholar] [CrossRef]
- Suber, T.L.; Nikolli, I.; O’Brien, M.E.; Londino, J.; Zhao, J.; Chen, K.; Mallampalli, R.K.; Zhao, Y. FBXO17 promotes cell proliferation through activation of Akt in lung adenocarcinoma cells. Respir. Res. 2018, 19, 206. [Google Scholar] [CrossRef]
- Yao, J.; Wang, X.P.; Yang, J.; Yang, Z.; Zhang, Z.Y. SCF-FBXL8 contributes to liver metastasis and stem-cell-like features in colorectal cancer cells by mediating ubiquitination and degradation of TP53. Clin. Transl. Med. 2023, 13, e1208. [Google Scholar] [CrossRef]
- Kim, Y.J.; Zhao, Y.; Myung, J.K.; Yi, J.M.; Kim, M.J.; Lee, S.J. Suppression of breast cancer progression by FBXL16 via oxygen-independent regulation of HIF1α stability. Cell Rep. 2021, 37, 109996. [Google Scholar] [CrossRef]
- Xu, L.; Yu, W.; Xiao, H.; Lin, K. BIRC5 is a prognostic biomarker associated with tumor immune cell infiltration. Sci. Rep. 2021, 11, 390. [Google Scholar] [CrossRef]
- Sansam, C.L.; Shepard, J.L.; Lai, K.; Ianari, A.; Danielian, P.S.; Amsterdam, A.; Hopkins, N.; Lees, J.A. DTL/CDT2 is essential for both CDT1 regulation and the early G2/M checkpoint. Genes. Dev. 2006, 20, 3117–3129. [Google Scholar] [CrossRef]
- Nguyen, H.D.; Kim, Y.E.; Nguyen, L.T.N.; Kwak, I.H.; Lee, Y.K.; Kim, Y.J.; Nguyen, T.T.H.; Pham, H.N.; Ma, H.I. Upregulation of immunoproteasome PSMB8 is associated with Parkinson′s disease. Park. Relat. Disord. 2023, 114, 105797. [Google Scholar] [CrossRef]
- Hwang, S.; Kwon, A.Y.; Jeong, J.Y.; Kim, S.; Kang, H.; Park, J.; Kim, J.H.; Han, O.J.; Lim, S.M.; An, H.J. Immune gene signatures for predicting durable clinical benefit of anti-PD-1 immunotherapy in patients with non-small cell lung cancer. Sci. Rep. 2020, 10, 643. [Google Scholar] [CrossRef]
- Yan, M.; Cao, H.; Tao, K.; Xiao, B.; Chu, Y.; Ma, D.; Huang, X.; Han, Y.; Ji, T. HDACs alters negatively to the tumor immune microenvironment in gynecologic cancers. Gene 2023, 885, 147704. [Google Scholar] [CrossRef]
- Oliva, J.; Bardag-Gorce, F.; Lin, A.; French, B.A.; French, S.W. The role of cytokines in UbD promoter regulation and Mallory-Denk body-like aggresomes. Exp. Mol. Pathol. 2010, 89, 1–8. [Google Scholar] [CrossRef]
- Stoyanova, T.; Roy, N.; Kopanja, D.; Raychaudhuri, P.; Bagchi, S. DDB2 (damaged-DNA binding protein 2) in nucleotide excision repair and DNA damage response. Cell Cycle 2009, 8, 4067–4071. [Google Scholar] [CrossRef]
- Haque, M.; Kendal, J.K.; MacIsaac, R.M.; Demetrick, D.J. WSB1: From homeostasis to hypoxia. J. Biomed. Sci. 2016, 23, 61. [Google Scholar] [CrossRef]
- Liu, P.; Verhaar, A.P.; Peppelenbosch, M.P. Signaling Size: Ankyrin and SOCS Box-Containing ASB E3 Ligases in Action. Trends Biochem. Sci. 2019, 44, 64–74. [Google Scholar] [CrossRef]
- Narayanan, S.; Cai, C.Y.; Assaraf, Y.G.; Guo, H.Q.; Cui, Q.; Wei, L.; Huang, J.J.; Ashby, C.R., Jr.; Chen, Z.S. Targeting the ubiquitin-proteasome pathway to overcome anti-cancer drug resistance. Drug Resist. Updat. 2020, 48, 100663. [Google Scholar]
- Zhou, L.; Zhang, W.; Sun, Y.; Jia, L. Protein neddylation and its alterations in human cancers for targeted therapy. Cell Signal. 2018, 44, 92–102. [Google Scholar] [CrossRef]
- Zhu, J.; Chu, F.; Zhang, M.; Sun, W.; Zhou, F. Association Between Neddylation and Immune Response. Front. Cell Dev. Biol. 2022, 10, 890121. [Google Scholar] [CrossRef]
- Lu, Y.; Yang, X. The pivotal roles of neddylation pathway in immunoregulation. Immun. Inflamm. Dis. 2020, 8, 782–792. [Google Scholar] [CrossRef]
- Zhou, L.; Jiang, Y.; Luo, Q.; Li, L.; Jia, L. Neddylation: A novel modulator of the tumor microenvironment. Mol. Cancer. 2019, 18, 77. [Google Scholar] [CrossRef]
- Hinshaw, D.C.; Shevde, L.A. The Tumor Microenvironment Innately Modulates Cancer Progression. Cancer Res. 2019, 79, 4557–4566. [Google Scholar] [CrossRef]
- Joyce, J.A. Therapeutic targeting of the tumor microenvironment. Cancer Cell. 2005, 7, 513–520. [Google Scholar] [CrossRef]
- Sounni, N.E.; Noel, A. Targeting the tumor microenvironment for cancer therapy. Clin. Chem. 2013, 59, 85–93. [Google Scholar] [CrossRef]
- Whiteside, T.L. The tumor microenvironment and its role in promoting tumor growth. Oncogene 2008, 27, 5904–5912. [Google Scholar] [CrossRef]
- Liu, D.; Che, X.; Wu, G. Deciphering the role of neddylation in tumor microenvironment modulation: Common outcome of multiple signaling pathways. Biomark. Res. 2024, 12, 5. [Google Scholar] [CrossRef]
- Zhang, S.; Zhang, E.; Long, J.; Hu, Z.; Peng, J.; Liu, L.; Tang, F.; Li, L.; Ouyang, Y.; Zeng, Z. Immune infiltration in renal cell carcinoma. Cancer Sci. 2019, 110, 1564–1572. [Google Scholar] [CrossRef]
- Leibovich, B.C.; Lohse, C.M.; Crispen, P.L.; Boorjian, S.A.; Thompson, R.H.; Blute, M.L.; Cheville, J.C. Histological subtype is an independent predictor of outcome for patients with renal cell carcinoma. J. Urol. 2010, 183, 1309–1315. [Google Scholar] [CrossRef]
- Gupta, K.; Miller, J.D.; Li, J.Z.; Russell, M.W.; Charbonneau, C. Epidemiologic and socioeconomic burden of metastatic renal cell carcinoma (mRCC): A literature review. Cancer Treat. Rev. 2008, 34, 193–205. [Google Scholar] [CrossRef]
- Porta, C.; Cosmai, L.; Leibovich, B.C.; Powles, T.; Gallieni, M.; Bex, A. The adjuvant treatment of kidney cancer: A multidisciplinary outlook. Nat. Rev. Nephrol. 2019, 15, 423–433. [Google Scholar] [CrossRef]
- Hu, J.; Chen, Z.; Bao, L.; Zhou, L.; Hou, Y.; Liu, L.; Xiong, M.; Zhang, Y.; Wang, B.; Tao, Z.; et al. Single-Cell Transcriptome Analysis Reveals Intratumoral Heterogeneity in ccRCC, which Results in Different Clinical Outcomes. Mol. Ther. 2020, 28, 1658–1672. [Google Scholar] [CrossRef]
- Li, Q.; Pan, Y.; Cao, Z.; Zhao, S. Comprehensive Analysis of Prognostic Value and Immune Infiltration of Chromobox Family Members in Colorectal Cancer. Front. Oncol. 2020, 10, 582667. [Google Scholar] [CrossRef]
- Requena, D.O.; Garcia-Buitrago, M. Molecular Insights Into Colorectal Carcinoma. Arch. Med. Res. 2020, 51, 839–844. [Google Scholar] [CrossRef]
- Hashimoto, H.; Vertino, P.M.; Cheng, X. Molecular coupling of DNA methylation and histone methylation. Epigenomics 2010, 2, 657–669. [Google Scholar] [CrossRef]
- Meng, H.; Cao, Y.; Qin, J.; Song, X.; Zhang, Q.; Shi, Y.; Cao, L. DNA methylation, its mediators and genome integrity. Int. J. Biol. Sci. 2015, 11, 604–617. [Google Scholar] [CrossRef]
- Moore, L.D.; Le, T.; Fan, G. DNA methylation and its basic function. Neuropsychopharmacology 2013, 38, 23–38. [Google Scholar] [CrossRef]
- Dai, X.; Ren, T.; Zhang, Y.; Nan, N. Methylation multiplicity and its clinical values in cancer. Expert. Rev. Mol. Med. 2021, 23, e2. [Google Scholar] [CrossRef]
- Bagcchi, S. Sunitinib still fi rst-line therapy for metastatic renal cancer. Lancet Oncol. 2014, 15, e420. [Google Scholar] [CrossRef]
- Ravaud, A.; Motzer, R.J.; Pandha, H.S.; George, D.J.; Pantuck, A.J.; Patel, A.; Chang, Y.H.; Escudier, B.; Donskov, F.; Magheli, A.; et al. Adjuvant Sunitinib in High-Risk Renal-Cell Carcinoma after Nephrectomy. N. Engl. J. Med. 2016, 375, 2246–2254. [Google Scholar] [CrossRef]
- Jayaprakash, N.G.; Surolia, A. Role of glycosylation in nucleating protein folding and stability. Biochem. J. 2017, 474, 2333–2347. [Google Scholar] [CrossRef]
- Choudhary, C.; Mann, M. Decoding signalling networks by mass spectrometry-based proteomics. Nat. Rev. Mol. Cell Biol. 2010, 11, 427–439. [Google Scholar] [CrossRef]
- Narita, T.; Weinert, B.T.; Choudhary, C. Functions and mechanisms of non-histone protein acetylation. Nat. Rev. Mol. Cell Biol. 2019, 20, 156–174. [Google Scholar] [CrossRef]
- King, C.M.; Glowinski, I.B. Acetylation, deacetylation and acyltransfer. Environ. Health Perspect. 1983, 49, 43–50. [Google Scholar] [CrossRef]
- van Schie, E.H.; van Amerongen, R. Aberrant WNT/CTNNB1 Signaling as a Therapeutic Target in Human Breast Cancer: Weighing the Evidence. Front. Cell Dev. Biol. 2020, 8, 25. [Google Scholar] [CrossRef]
- Moroney, M.R.; Woodruff, E.; Qamar, L.; Bradford, A.P.; Wolsky, R.; Bitler, B.G.; Corr, B.R. Inhibiting Wnt/beta-catenin in CTNNB1-mutated endometrial cancer. Mol. Carcinog. 2021, 60, 511–523. [Google Scholar] [CrossRef]
- Giménez, N.; Martínez-Trillos, A.; Montraveta, A.; Lopez-Guerra, M.; Rosich, L.; Nadeu, F.; Valero, J.G.; Aymerich, M.; Magnano, L.; Rozman, M.; et al. Mutations in the RAS-BRAF-MAPK-ERK pathway define a specific subgroup of patients with adverse clinical features and provide new therapeutic options in chronic lymphocytic leukemia. Haematologica 2019, 104, 576–586. [Google Scholar] [CrossRef]
- Ros, J.; Baraibar, I.; Sardo, E.; Mulet, N.; Salvà, F.; Argilés, G.; Martini, G.; Ciardiello, D.; Cuadra, J.L.; Tabernero, J.; et al. BRAF, MEK and EGFR inhibition as treatment strategies in BRAF V600E metastatic colorectal cancer. Ther. Adv. Med. Oncol. 2021, 13, 1758835921992974. [Google Scholar] [CrossRef]
- Lam, K.K.; Tang, C.L.; Tan, E.; Wong, S.H.; Cheah, P.Y. KRAS mutation-independent downregulation of MAPK/PI3K signaling in colorectal cancer. Mol. Oncol. 2022, 16, 1171–1183. [Google Scholar] [CrossRef]
- Mármol, I.; Sánchez-de-Diego, C.; Pradilla Dieste, A.; Cerrada, E.; Rodriguez Yoldi, M.J. Colorectal Carcinoma: A General Overview and Future Perspectives in Colorectal Cancer. Int. J. Mol. Sci. 2017, 18, 197. [Google Scholar] [CrossRef]
- Asati, V.; Bharti, S.K.; Mahapatra, D.K.; Asati, V.; Budhwani, A.K. Triggering PIK3CA Mutations in PI3K/Akt/mTOR Axis: Exploration of Newer Inhibitors and Rational Preventive Strategies. Curr. Pharm. Des. 2016, 22, 6039–6054. [Google Scholar] [CrossRef]
- Finkel, T.; Deng, C.X.; Mostoslavsky, R. Recent progress in the biology and physiology of sirtuins. Nature 2009, 460, 587–591. [Google Scholar] [CrossRef]
- Garcia-Peterson, L.M.; Li, X. Trending topics of SIRT1 in tumorigenicity. Biochim. Biophys. Acta Gen. Subj. 2021, 1865, 129952. [Google Scholar] [CrossRef]
- Alves-Fernandes, D.K.; Jasiulionis, M.G. The Role of SIRT1 on DNA Damage Response and Epigenetic Alterations in Cancer. Int. J. Mol. Sci. 2019, 20, 3153. [Google Scholar] [CrossRef]
- Wang, T.; Cao, Y.; Zheng, Q.; Tu, J.; Zhou, W.; He, J.; Zhong, J.; Chen, Y.; Wang, J.; Cai, R.; et al. SENP1-Sirt3 Signaling Controls Mitochondrial Protein Acetylation and Metabolism. Mol. Cell. 2019, 75, 823–834.e5. [Google Scholar] [CrossRef]
- Li, H.; Liu, J.W.; Sun, L.P.; Yuan, Y. A Meta-Analysis of the Association between DNMT1 Polymorphisms and Cancer Risk. Biomed. Res. Int. 2017, 2017, 3971259. [Google Scholar] [CrossRef]
- Parveen, R.; Harihar, D.; Chatterji, B.P. Recent histone deacetylase inhibitors in cancer therapy. Cancer 2023, 129, 3372–3380. [Google Scholar] [CrossRef]
- Willis-Martinez, D.; Richards, H.W.; Timchenko, N.A.; Medrano, E.E. Role of HDAC1 in senescence, aging, and cancer. Exp. Gerontol. 2010, 45, 279–285. [Google Scholar] [CrossRef]
- Jo, H.; Shim, K.; Kim, H.U.; Jung, H.S.; Jeoung, D. HDAC2 as a target for developing anti-cancer drugs. Comput. Struct. Biotechnol. J. 2023, 21, 2048–2057. [Google Scholar] [CrossRef]
- Quail, D.F.; Joyce, J.A. Microenvironmental regulation of tumor progression and metastasis. Nat. Med. 2013, 19, 1423–1437. [Google Scholar] [CrossRef]
- Bader, J.E.; Voss, K.; Rathmell, J.C. Targeting Metabolism to Improve the Tumor Microenvironment for Cancer Immunotherapy. Mol. Cell. 2020, 78, 1019–1033. [Google Scholar] [CrossRef]
- Tomczak, K.; Czerwińska, P.; Wiznerowicz, M. The Cancer Genome Atlas (TCGA): An immeasurable source of knowledge. Contemp. Oncol. 2015, 19, A68–A77. [Google Scholar] [CrossRef]
- Chen, J.; Zaidi, S.; Rao, S.; Chen, J.S.; Phan, L.; Farci, P.; Su, X.; Shetty, K.; White, J.; Zamboni, F.; et al. Analysis of Genomes and Transcriptomes of Hepatocellular Carcinomas Identifies Mutations and Gene Expression Changes in the Transforming Growth Factor-β Pathway. Gastroenterology 2018, 154, 195–210. [Google Scholar] [CrossRef]
- Yang, W.; Soares, J.; Greninger, P.; Edelman, E.J.; Lightfoot, H.; Forbes, S.; Bindal, N.; Beare, D.; Smith, J.A.; Thompson, I.R.; et al. Genomics of Drug Sensitivity in Cancer (GDSC): A resource for therapeutic biomarker discovery in cancer cells. Nucleic Acids Res. 2013, 41, D955–D961. [Google Scholar] [CrossRef]





| Oligonucleotides | Nucleotide Sequence | |
|---|---|---|
| siRNA | PSMB10-Homo-334 | Sense: GCUGCGAGAAGAUCCACUUTT |
| Antisense: AAGUGGAUCUUCUCGCAGCTT | ||
| PSMB10-Homo-908 | Sense: GGAGCUAGUGGAGGAAACUTT | |
| Antisense: AGUUUCCUCCACUAGCUCCTT | ||
| Negative control FAM | Sense: UUCUCCGAACGUGUCACGUTT | |
| Antisense: ACGUGACACGUUCGGAGAATT | ||
| Primer | GAPDH | Forward 5′-TGAAGGGTGGAGCCAAAAG-3′ |
| Reverse 5′-AGTCTTCTGGGTGGCAGTGAT-3′ | ||
| PSMB10 | Forward 5′-GGCAATGTGGACGCATGTG-3′ | |
| Reverse 5′-CTCCACTAGCTCCAGGGTTAGT-3′ | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, D.; Wu, G.; Wang, S.; Zheng, X.; Che, X. Evaluating the Role of Neddylation Modifications in Kidney Renal Clear Cell Carcinoma: An Integrated Approach Using Bioinformatics, MLN4924 Dosing Experiments, and RNA Sequencing. Pharmaceuticals 2024, 17, 635. https://doi.org/10.3390/ph17050635
Liu D, Wu G, Wang S, Zheng X, Che X. Evaluating the Role of Neddylation Modifications in Kidney Renal Clear Cell Carcinoma: An Integrated Approach Using Bioinformatics, MLN4924 Dosing Experiments, and RNA Sequencing. Pharmaceuticals. 2024; 17(5):635. https://doi.org/10.3390/ph17050635
Chicago/Turabian StyleLiu, Dequan, Guangzhen Wu, Shijin Wang, Xu Zheng, and Xiangyu Che. 2024. "Evaluating the Role of Neddylation Modifications in Kidney Renal Clear Cell Carcinoma: An Integrated Approach Using Bioinformatics, MLN4924 Dosing Experiments, and RNA Sequencing" Pharmaceuticals 17, no. 5: 635. https://doi.org/10.3390/ph17050635
APA StyleLiu, D., Wu, G., Wang, S., Zheng, X., & Che, X. (2024). Evaluating the Role of Neddylation Modifications in Kidney Renal Clear Cell Carcinoma: An Integrated Approach Using Bioinformatics, MLN4924 Dosing Experiments, and RNA Sequencing. Pharmaceuticals, 17(5), 635. https://doi.org/10.3390/ph17050635






