Promising Effects of Casearins in Tumor-Bearing Mice and Antinociceptive Action against Oncologic Pain: Molecular Docking and In Vivo Findings
Abstract
1. Introduction
2. Results
2.1. Fraction with Casearins Has Antitumor Activity in a Xenographic Model of Human Colon Carcinoma without Systemic Side Effects
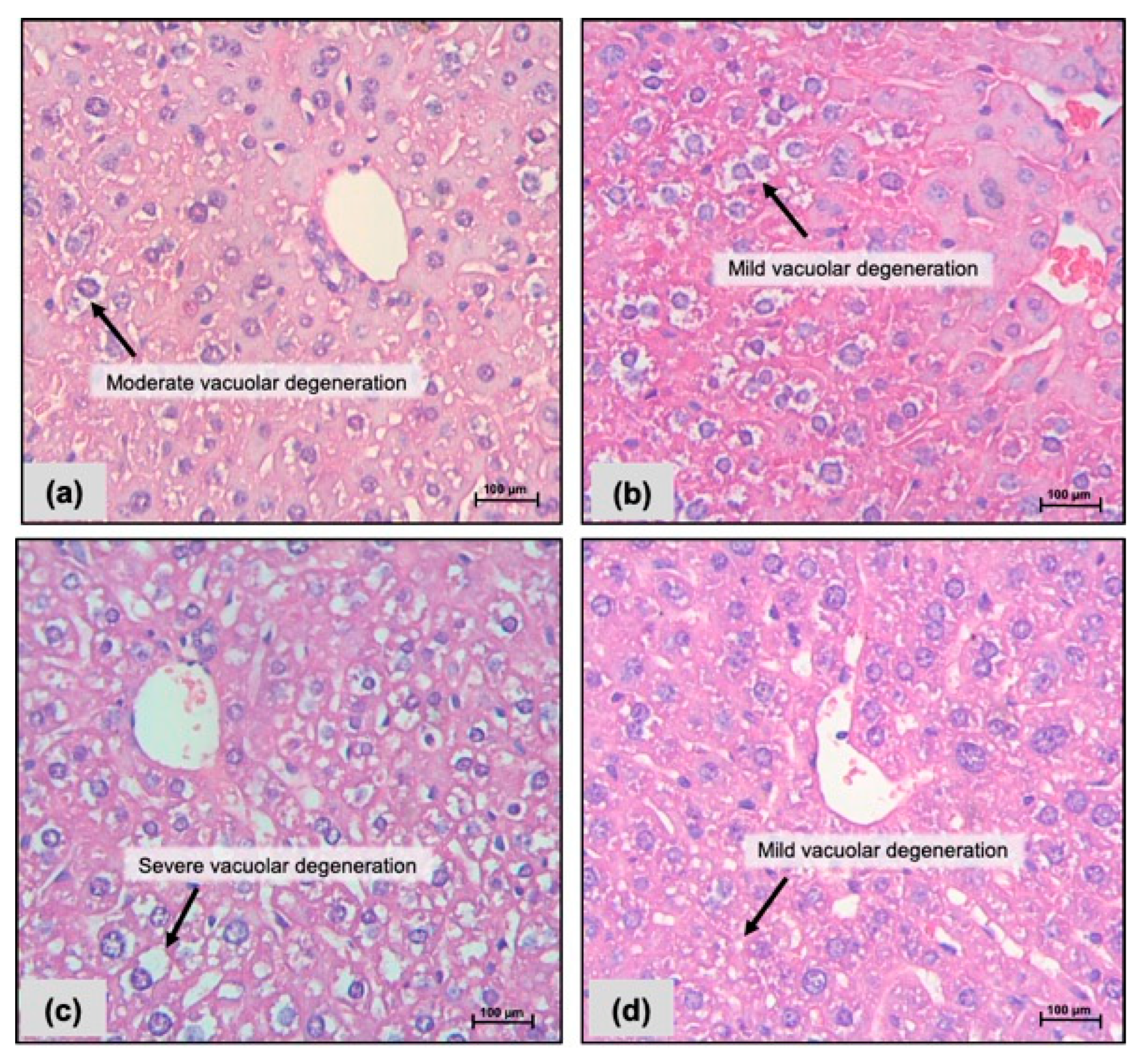
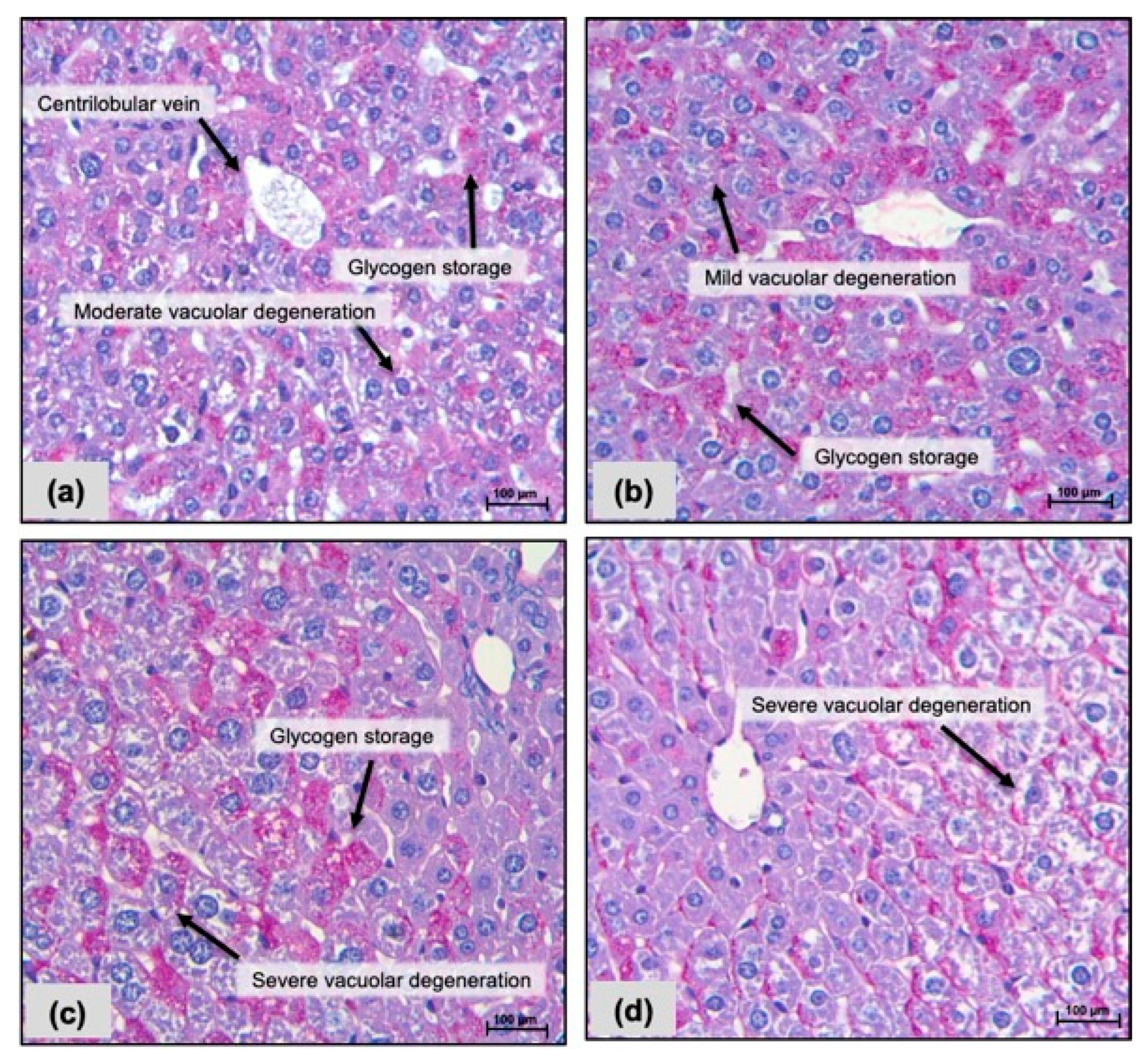
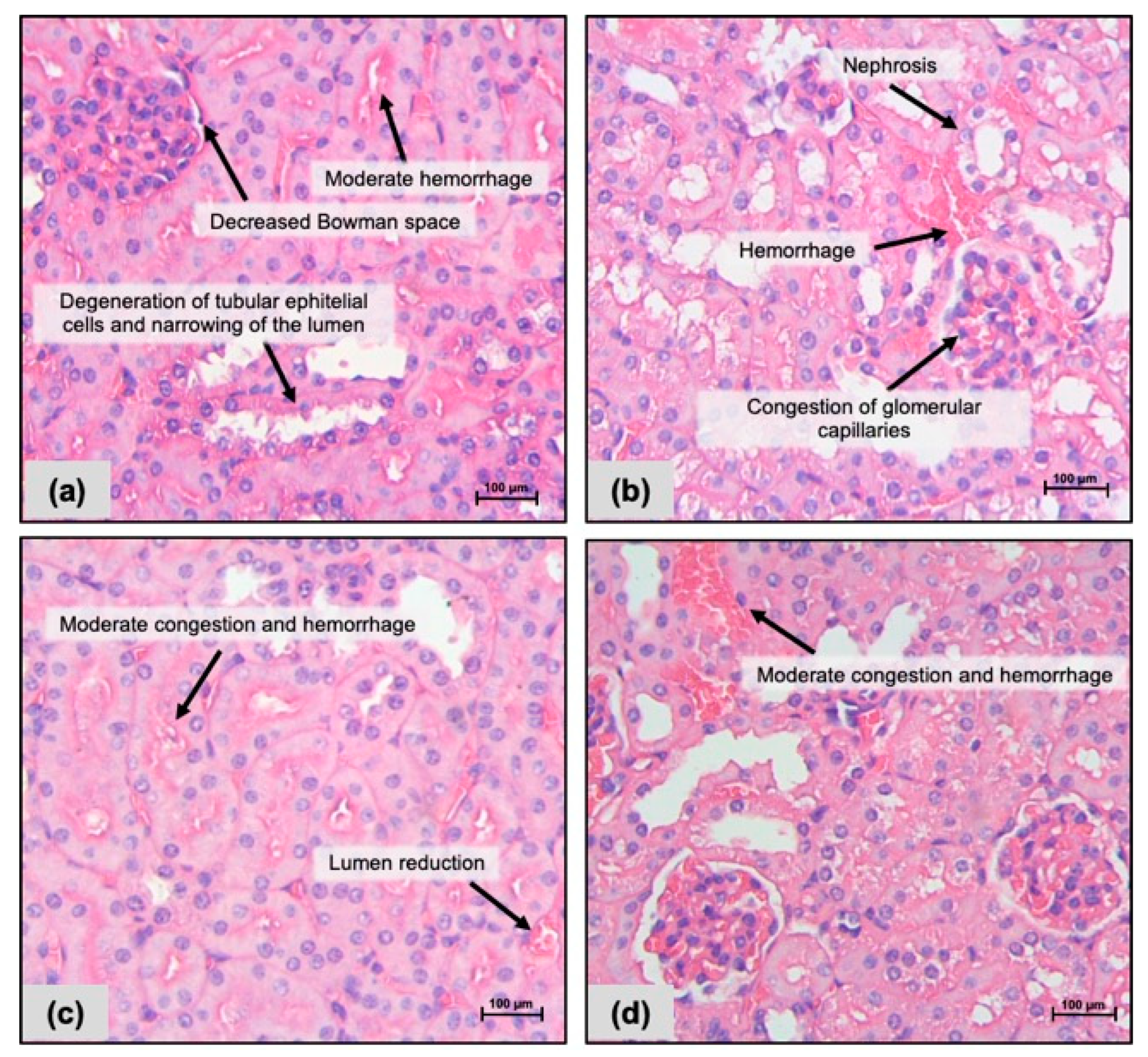
2.2. Histopathological Analysis
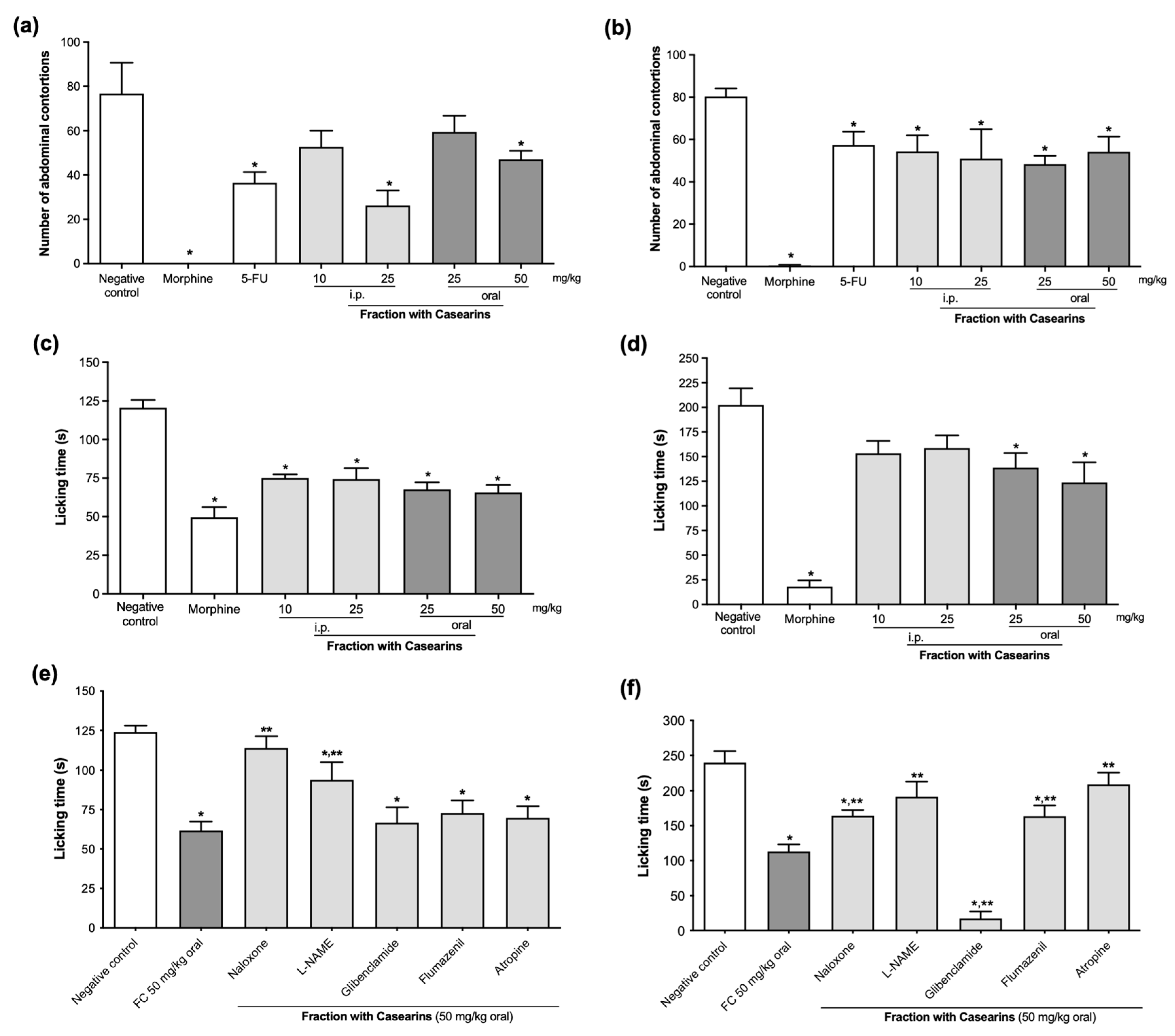
2.3. Antinociceptive Action against Chemically Induced Pain
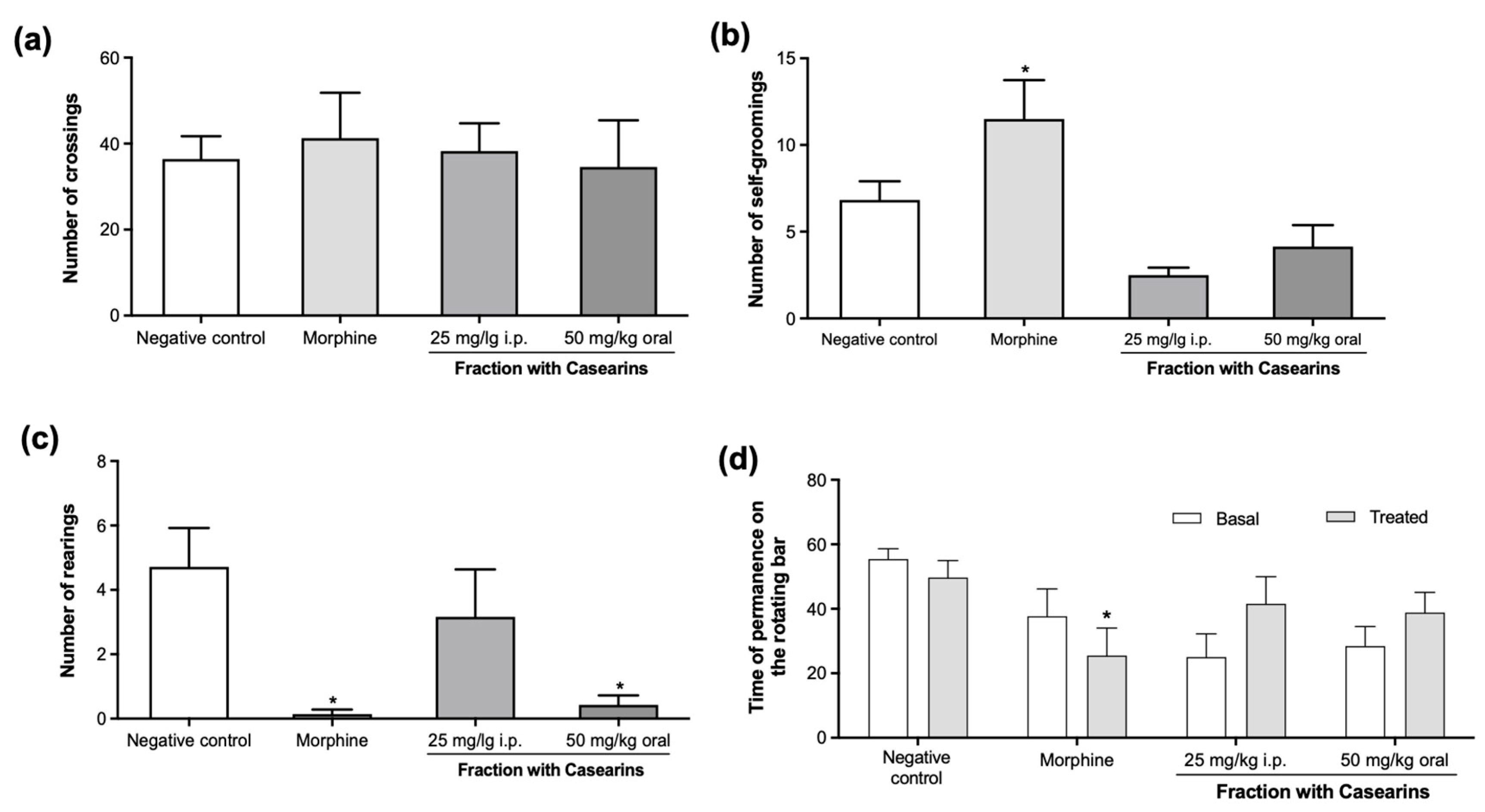
2.4. Fraction with Casearins Reduces Oncologic Pain in S180-Transplanted Mice
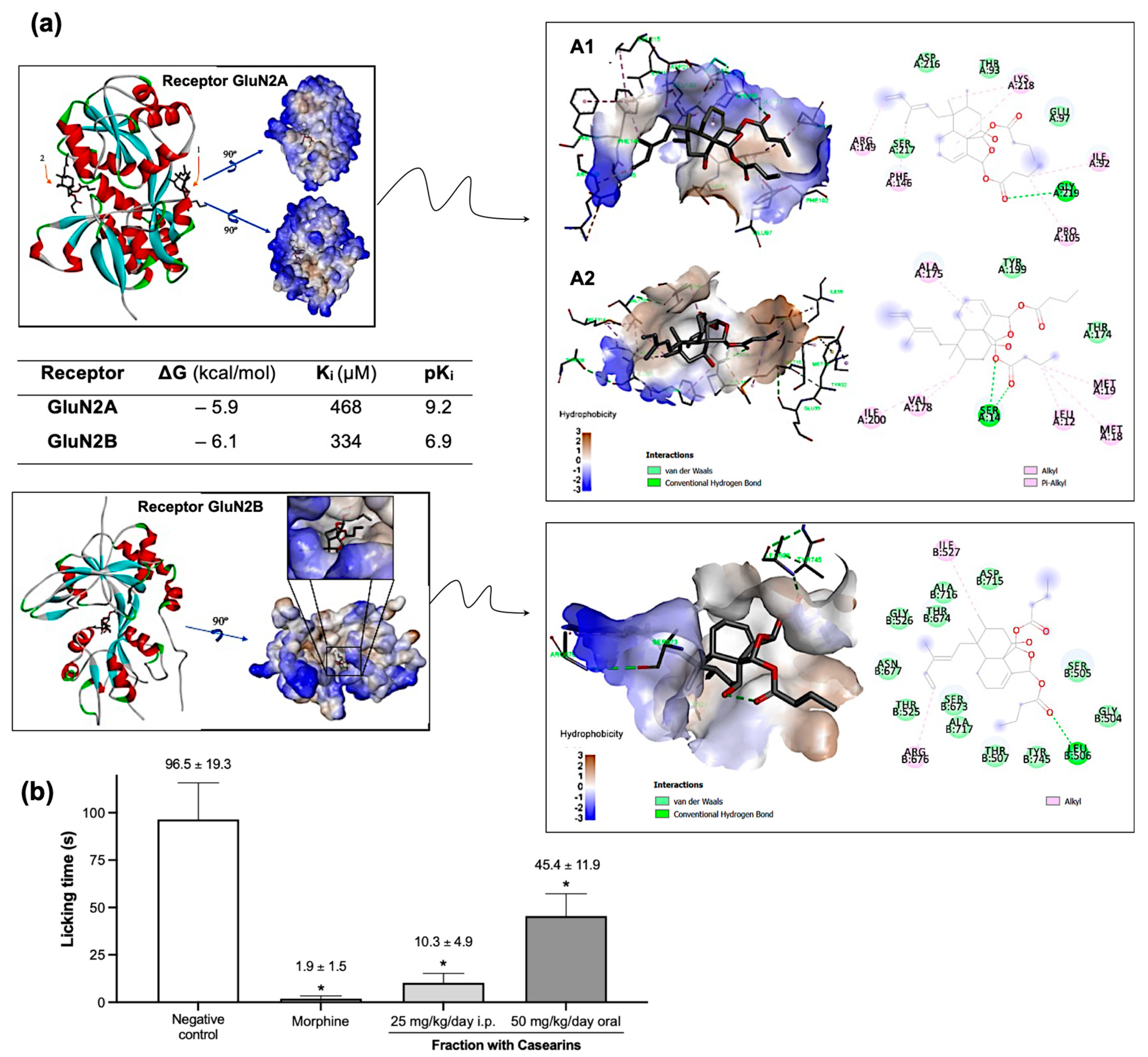
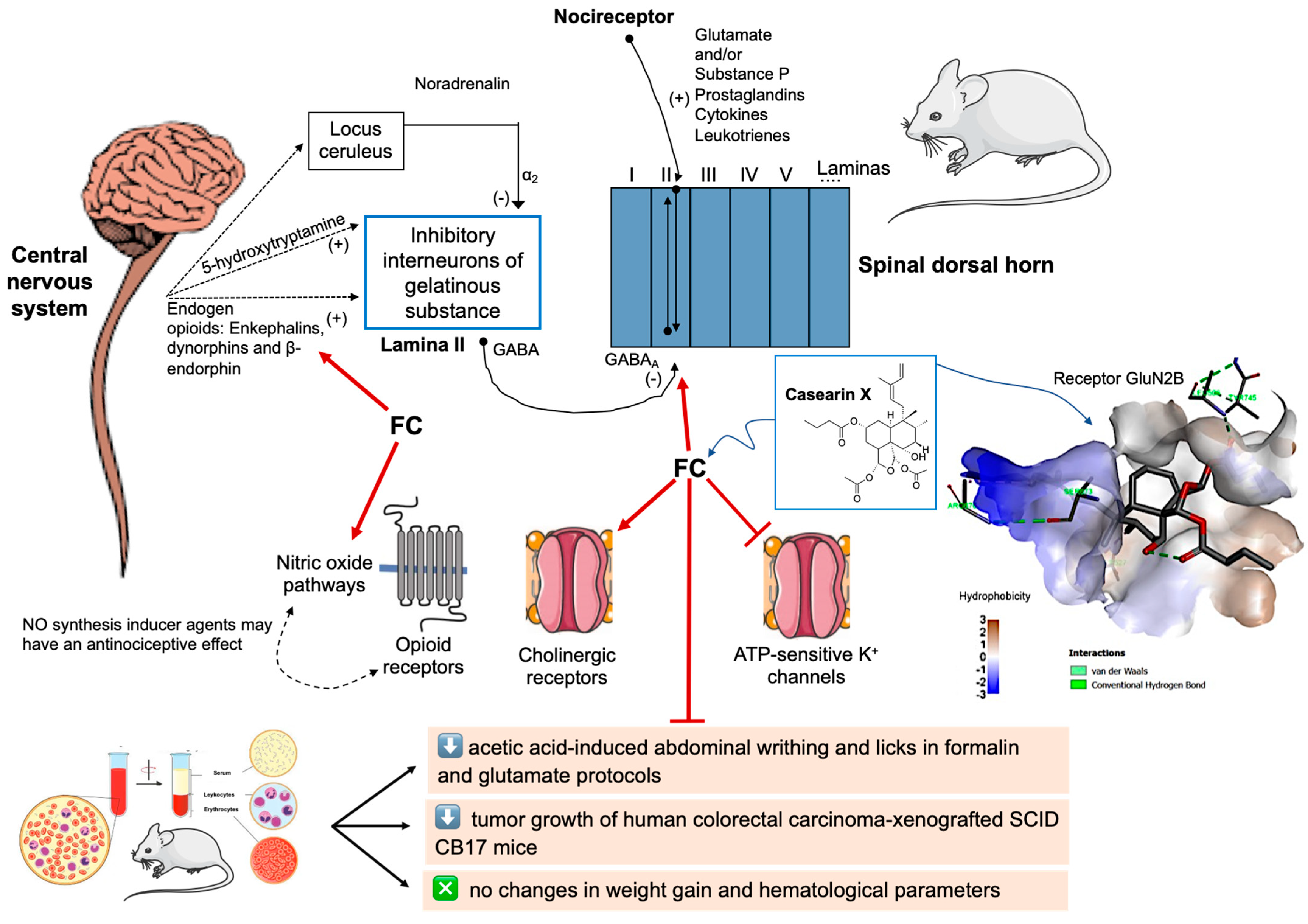
2.5. Casearin X Binds to NMDA-Type Glutamate Receptors
3. Discussion
3.1. Anticancer Action and Toxicological Issues
3.2. Analgesic In Vivo Effects
4. Materials and Methods
4.1. Acquisition of Plant Samples and Phytochemical Analysis
4.2. Animals and Ethical Aspects
4.3. In Vivo Xenograft Antitumor Model Assay and Systemic-Related Assessments
4.4. Antinociceptive Assessments
4.4.1. Acetic Acid-Induced Abdominal Writhing
4.4.2. Formalin Nociception Tests
4.4.3. Glutamate-Induced Nociception
4.5. Oncological Pain Model Induced by Sarcoma 180 Tumor
4.5.1. Open Field Test
4.5.2. Rotarod Test
4.5.3. Mechanical Nociception by Von Frey Assay
4.6. Molecular Docking
4.7. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Anand, P.; Kunnumakkara, A.B.; Sundaram, C.; Harikumar, K.B.; Tharakan, S.T.; Lai, O.S.; Sung, B.; Aggarwal, B.B. Cancer is a preventable disease that requires major lifestyle changes. Pharm. Res. 2008, 25, 2097–2116. [Google Scholar] [CrossRef]
- Jan, R.; Chaudhry, G.E. Understanding apoptosis and apoptotic pathways targeted cancer therapeutics. Adv. Pharm. Bull. 2019, 9, 205–218. [Google Scholar] [CrossRef]
- Steinbichler, T.B.; Dudas, J.; Riechelmann, H.; Skvortsova, I. The role of exosomes in cancer metastasis. Semin. Cancer Biol. 2017, 44, 170–181. [Google Scholar] [CrossRef]
- Koo, M.M.; Swann, R.; McPhail, S.; Abel, G.A.; Elliss-Brookes, L.; Rubin, G.P.; Lyratzopoulos, G. Presenting symptoms of cancer and stage at diagnosis: Evidence from a cross-sectional, population-based study. Lancet Oncol. 2020, 21, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Schug, S.A.; Chandrasena, C. Pain management of the cancer patient. Expert Opin. Pharmacother. 2015, 16, 5–15. [Google Scholar] [CrossRef]
- Scarborough, B.M.; Smith, C.B. Optimal pain management for patients with cancer in the modern era: Pain Management for Patients with Cancer. CA Cancer J. Clin. 2018, 68, 182–196. [Google Scholar] [CrossRef] [PubMed]
- Gambeta, E.; Kopruszinski, C.M.; Reis, R.C.; Zanoveli, J.M.; Chichorro, J.G. Evaluation of heat hyperalgesia and anxiety like-behaviors in a rat model of orofacial cancer. Neurosci. Lett. 2016, 619, 100–105. [Google Scholar] [CrossRef]
- Elad, S.; Yarom, N.; Zadik, Y.; Kuten-Shorrer, M.; Sonis, S.T. The broadening scope of oral mucositis and oral ulcerative mucosal toxicities of anticancer therapies. CA Cancer J. Clin. 2022, 72, 57–77. [Google Scholar] [CrossRef]
- Wood, H.; Dickman, A.; Star, A.; Boland, J.W. Updates in palliative care—Overview and recent advancements in the pharmacological management of cancer pain. Clin. Med. 2018, 18, 17–22. [Google Scholar] [CrossRef]
- Højsted, J.; Sjøgren, P. Addiction to opioids in chronic pain patients: A literature review. Eur. J. Pain 2007, 11, 490–518. [Google Scholar] [CrossRef]
- National Cancer Institute (NCI). Cancer Pain (PDQ®)—Health Professional Version. Available online: https://www.cancer.gov/about-cancer/treatment/side-effects/pain/pain-hp-pdq#_59_toc (accessed on 6 May 2023).
- Michalak, I.; Püsküllüoğlu, M. Look into my onco-forest—Review of plant natural products with anticancer activity. Curr. Top. Med. Chem. 2022, 22, 922–938. [Google Scholar] [CrossRef]
- Ferreira, P.M.P.; Sousa, L.Q.; Sousa, R.W.R.; Rodrigues, D.J.; Moncao-Filho, E.S.; Chaves, M.H.; Vieira Júnior, G.M.; Rizzo, M.S.; Filgueiras, L.A.; Mendes, A.N.; et al. Toxic profile of marinobufagin from poisonous Amazon toads and antitumoral effects on human colorectal carcinomas. J. Ethonopharmacol. 2023, 310, 116406. [Google Scholar] [CrossRef]
- Ferreira, P.M.P.; Arcanjo, D.D.R.; Peron, A.P. Drug development, Brazilian biodiversity and political choices: Where are we heading? J. Toxicol. Environ. Health B Crit. Rev. 2023, 26, 257–274. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro-Neto, F.R.; Lopes, E.M.; Acha, B.T.; Gomes, L.S.; Dias, W.A.; Reis Filho, A.C.; Leal, B.S.; Rodrigues, D.C.N.; Silva, J.N.; Dittz, D.; et al. α-Phellandrene exhibits antinociceptive and tumor-reducing effects in a mouse model of oncologic pain. Toxicol. Appl. Pharmacol. 2021, 418, 115497. [Google Scholar] [CrossRef]
- Sleumer, H.O. Flacourtiaceae. Flora Neotrop. 1980, 22, 1–499. [Google Scholar]
- Balunas, M.J.; Jones, W.P.; Chin, Y.W.; Mi, Q.; Farnsworth, N.R.; Soejarto, D.D.; Cordell, G.A.; Swanson, S.M.; Pezzuto, J.M.; Chai, H.B.; et al. Relationships between Inhibitory activity against a cancer cell line panel, profiles of plants collected, and compound classes isolated in an anticancer drug discovery project. Chem. Biodivers. 2006, 3, 897–915. [Google Scholar] [CrossRef]
- Santos, A.G.; Ferreira, P.M.P.; Júnior, G.M.V.; Perez, C.C.; Tininis, A.G.; Silva, G.H.; Bolzani, V.S.; Costa-Lotufo, L.V.; Pessoa, C.O.; Cavalheiro, A.J. Casearin X, its degradation product and other clerodane diterpenes from leaves of Casearia sylvestris: Evaluation of cytotoxicity against normal and tumor human cells. Chem. Biodivers. 2010, 7, 205–215. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, P.M.P.; Bezerra, D.P.; Silva, J.N.; da Costa, M.P.; Ferreira, J.R.; Alencar, N.M.; Figueiredo, I.S.; Cavalheiro, A.J.; Machado, C.M.; Chammas, R.; et al. Preclinical anticancer effectiveness of a fraction from Casearia sylvestris and its component casearin X: In vivo and ex vivo methods and microscopy examinations. J. Ethnopharmacol. 2016, 186, 270–279. [Google Scholar] [CrossRef]
- Pereira, F.G.; Marquete, R.; Domingos, L.T.; Rocha, M.E.N.; Ferreira-Pereira, A.; Mansur, E.; Moreira, D.L. Antifungal activities of the essential oil and its fractions rich in sesquiterpenes from leaves of Casearia sylvestris Sw. An. Acad. Bras. Cienc. 2017, 89, 2817–2824. [Google Scholar] [CrossRef][Green Version]
- Araújo, E.J.F.; Almeida, A.A.C.; Silva, O.A.; Costa, I.H.F.; Rezende-Júnior, L.M.; Lima, F.C.A.; Cavalheiro, A.J.; Pessoa, C.; Moraes, M.O.; Ferreira, P.M.P. Behavioral effects induced by antitumor cleronade diterpenes from Casearia sylvestris and in silico interactions with neuron receptors. J. Ethnopharmacol. 2017, 198, 460–467. [Google Scholar] [CrossRef]
- Campos, E.P.; Trombini, L.N.; Rodrigues, R.; Portella, D.L.; Werner, A.C.; Ferraz, M.C.; Oliveira, R.V.M.; Cogo, J.C.; Oshima-Franco, Y.; Aranha, N.; et al. Healing activity of Casearia sylvestris Sw. in second-degree scald burns in rodents. BMC Res. Notes 2015, 8, 269. [Google Scholar] [CrossRef]
- Araújo, E.J.F.; Oliveira, G.A.L.; Sousa, L.Q.; Bolzani, V.S.; Cavalheiro, A.J.; Tomé, A.R.; Peron, A.P.; Santos, A.G.; Citó, A.M.G.L.; Pessoa, C.; et al. Counteracting effects on free radicals and histological alterations induced by a fraction with casearins. An. Acad. Bras. Cienc. 2015, 87, 1791–1807. [Google Scholar] [CrossRef]
- Espinosa, J.; Medeiros, L.F.; Souza, A.; Guntzel, A.R.C.; Rucker, B.; Casali, E.A.; Ethur, E.M.; Wink, M.R.; Torres, I.L.S. Ethanolic extract of Casearia sylvestris Sw. exhibits in vitro antioxidant and antimicrobial activities and in vivo hypolipidemic effect in rats. Rev. Bras. Pl. Med. 2015, 17, 305–315. [Google Scholar] [CrossRef]
- Antinarelli, L.M.R.; Pinto, N.C.; Scio, E.; Coimbra, E.S. Antileishmanial activity of some Brazilian plants, with particular reference to Casearia sylvestris. An. Acad. Bras. Cienc. 2015, 87, 733–742. [Google Scholar] [CrossRef]
- Pierri, E.G.; Castro, R.C.; Vizioli, E.O.; Ferreira, C.M.R.; Cavalheiro, A.J.; Tininis, A.G.; Man Chin, C.; Santos, A.G. Anti-inflammatory action of ethanolic extract and clerodane diterpenes from Casearia sylvestris. Rev. Bras. Farmacogn. 2017, 27, 495–501. [Google Scholar] [CrossRef]
- Heymanns, A.C.; Albano, M.N.; Silveira, M.R.; Muller, S.D.; Petronilho, F.C.; Gainski, L.D.; Cargnin-Ferreira, E.; Piovezan, A.P. Macroscopic, biochemical and hystological evaluation of topical anti-inflammatory activity of Casearia sylvestris (Flacourtiaceae) in mice. J. Ethnopharmacol. 2021, 10, 113139. [Google Scholar] [CrossRef]
- Spósito, L.; Oda, F.B.; Vieira, J.H.; Carvalho, F.A.; Ramos, M.A.S.; Castro, R.C.; Crevelin, E.J.; Crotti, A.E.M.; Santos, A.G.; Silva, P.B.; et al. In vitro and in vivo anti-Helicobacter pylori activity of Casearia sylvestris leaf derivatives. J. Ethnopharmacol. 2019, 233, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Oberlies, N.H.; Burgess, J.P.; Navarro, H.A.; Pinos, R.E.; Fairchild, C.R.; Peterson, R.W.; Soejarto, D.D.; Farnsworth, N.R.; Kinghorn, A.D.; Wani, M.C.; et al. Novel bioactive clerodane diterpenoids from the leaves and twigs of Casearia sylvestris. J. Nat. Prod. 2002, 65, 95–99. [Google Scholar] [PubMed]
- Santos, A.G.; Perez, C.C.; Tininis, A.G.; Bolzani, V.S.; Cavalheiro, A.J. Clerodane diterpenes from the leaves of Caseria sylvestris Swartz. Quím. Nova 2007, 30, 1100–1103. [Google Scholar] [CrossRef]
- Ferreira, P.M.P.; Costa-Lotufo, L.V.; Moraes, M.O.; Barros, F.W.A.; Martins, A.M.A.; Cavalheiro, A.J.; Bolzani, V.S.; Santos, A.G.; Pessoa, C. Folk uses and pharmacological properties of Casearia sylvestris: A medicinal review. Acad. Bras. Cienc. 2011, 83, 1373–1384. [Google Scholar] [CrossRef]
- Oda, F.B.; Crevelin, E.J.; Crotti, A.E.M.; Orlando, A.B.; Medeiros, A.I.; Nogueira, F.A.R.; Santos, A.G. Acidic and hepatic derivatives of bioactive clerodane diterpenes casearins J and O. Fitoterapia 2019, 137, 104197. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Sun, X.R.; He, X.T.; Zhou, X.M.; Wu, X.W.; Zhang, R.H.; Zhang, X.J.; Li, X.L.; Xiao, W.L. 16,17-dinor-abietane diterpenoids from Casearia kurzii. Fitoterapia 2023, 28, 105519. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, P.M.P.; Militão, G.C.G.; Lima, D.J.B.; Costa, N.D.J.; Machado, K.C.; Santos, A.G.; Cavalheiro, A.J.; Bolzani, V.S.; Silva, D.H.S.; Pessoa, C. Morphological and biochemical alterations activated by antitumor clerodane diterpenes. Chem. Biol. Interact. 2014, 222, 112–125. [Google Scholar] [CrossRef] [PubMed]
- Andrade, F.C.P.; Mendes, N.A. Computational analysis of eugenol inhibitory activity in lipoxygenase and cyclooxygenase pathways. Sci. Rep. 2020, 10, 16204. [Google Scholar] [CrossRef] [PubMed]
- Atanasov, A.G.; Waltenberger, B.; Pferschy-Wenzig, E.M.; Linder, T.; Wawrosch, C.; Uhrin, P.; Temml, V.; Wang, L.; Schwaiger, S.; Heiss, E.H.; et al. Discovery and resupply of pharmacologically active plant-derived natural products: A review. Biotechnol. Adv. 2015, 33, 1582–1614. [Google Scholar] [CrossRef] [PubMed]
- Itokawa, H.; Totsuka, N.; Morita, H.; Takeya, K.; Iitaka, Y.; Schenkel, E.P.; Motidome, M. New antitumor principles, Casearins A-F, from Casearia sylvestris Sw. (Flacourtiaceae). Chem. Pharm. Bull. 1990, 38, 3384–3388. [Google Scholar] [CrossRef] [PubMed]
- Morita, H.; Nakayama, M.; Kojima, H.; Takeya, K.; Itokawa, H.; Schenkel, E.P.; Motidome, M. Structure and cytotoxic activity relationship of casearins, new clerodane diterpenes from Casearia sylvestris Sw. Chem. Pharm. Bull. 1991, 39, 693–697. [Google Scholar] [CrossRef] [PubMed]
- Silva, S.L.; Chaar, J.S.; Figueiredo, P.M.S.; Yano, T. Cytotoxic evaluation of essential oil from Casearia sylvestris Sw. on human cancer cells and erythrocytes. Acta Amaz. 2008, 38, 107–112. [Google Scholar] [CrossRef]
- Silva, S.L.; Calgarotto, A.K.; Chaar, J.S.; Ma-Rangoni, S. Isolation and characterization of ellagic acid derivatives isolated from Casearia sylvestris Sw. aqueous extract with anti-PLA2 activity. Toxicon 2008, 52, 655–666. [Google Scholar] [CrossRef]
- Silva, S.L.; Chaar, J.S.; Yano, T. Chemotherapeutic potential of two gallic acid derivative compounds from leaves of Casearia sylvestris Sw (Flacourtiaceae). Eur. J. Pharmacol. 2009, 608, 76–83. [Google Scholar] [CrossRef]
- Ferreira, P.M.P.; Santos, A.G.; Tininis, A.G.; Costa, P.M.; Cavalheiro, A.J.; Bolzani, V.S.; Moraes, M.O.; Costa-Lotufo, L.V.; Montenegro, R.C.; Pessoa, C. Casearin X exhibits cytotoxic effects in leukemia cells triggered by apoptosis. Chem. Biol. Interact. 2010, 188, 497–504. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Zhao, J.; Wang, Y.H.; Smillie, T.A.; Li, X.C.; Khan, I.A. Diterpenoids from Casearia sylvestris. Planta Med. 2009, 75, 1436–1441. [Google Scholar] [CrossRef] [PubMed]
- Almeida, A. Atividades Anti-Inflamatoria e Antitumoral do Extrato Hidroalcoólico de Casearia sylvestris: Estudo Comparativo Com os Anti-Inflamatorios Piroxicam e Meloxicam. Ph.D. Thesis, University of Sao Paulo, São Paulo, Brazil, 2000. [Google Scholar]
- Felipe, K.B.; Kviecinski, M.R.; da Silva, F.O.; Bücker, N.F.; Farias, M.S.; Castro, L.S.E.P.W. Inhibition of tumor proliferation associated with cell cycle arrest caused by extract and fraction from Casearia Sylvestris (Salicaceae). J. Ethnopharmacol. 2014, 155, 1492–1499. [Google Scholar] [CrossRef] [PubMed]
- Suggitt, M.; Cooper, P.A.; Shnyder, S.D.; Bibby, M. The hollow fibre model-facilitating anti-cancer pre-clinical pharmacodynamics and improving animal welfare. Int. J. Oncol. 2006, 29, 1493–1499. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, P.M.P.; Santos, D.B.; Silva, J.N.; Goudinho, A.F.; Ramos, C.L.S.; Souza, P.C.; Almeida, R.S.C.; Moura, D.S.; Oliveira, R.; Grisolia, C.K.; et al. Toxicological findings about an anticancer fraction with casearins described by traditional and alternative techniques as support to the Brazilian Unified Health System (SUS). J. Ethnopharmacol. 2019, 241, 112004. [Google Scholar] [CrossRef] [PubMed]
- Fyfe, J.J.; Bishop, D.J.; Bartlett, J.D.; Hanson, E.; Anderson, M.; Garnham, A.; Stepto, N. Enhanced skeletal muscle ribosome biogenesis, yet attenuated mTORC1 and ribosome biogenesis-related signalling, following short-term concurrent versus single-mode resistance training. Sci. Rep. 2018, 8, 560. [Google Scholar] [CrossRef] [PubMed]
- Jongen, J.L.; Huijsman, M.L.; Jessurun, J.; Ogenio, K.; Schipper, D.; Verkouteren, D.R.; Moorman, P.W.; Van Der Rijt, C.C.; Vissers, K.C. The evidence for pharmacologic treatment of neuropathic cancer pain: Beneficial and adverse effects. J. Pain Symptom Manag. 2012, 46, 581–590. [Google Scholar] [CrossRef] [PubMed]
- Manchikanti, L.; Manchikanti, K.N.; Kaye, A.D.; Kaye, A.M.; Hirsch, J.A. Challenges and concerns of persistent opioid use in cancer patients. Expert. Rev. Anticancer Ther. 2018, 18, 705–718. [Google Scholar] [CrossRef]
- Sowemimo, A.; Onakoya, M.; Fageyinbo, M.S.; Fadoju, T. Studies on the anti-inflammatory and anti-nociceptive properties of Blepharis maderaspatensis leaves. Brazilian J. Pharmacogn. 2013, 23, 830–835. [Google Scholar] [CrossRef]
- Hegen, M.; Keith, J.C.; Collins, M.; Nickerson-Nutter, C.L. Utility of animal models for identification of potential therapeutics for rheumatoid arthritis. Ann. Rheum. Dis. 2008, 67, 1505–1515. [Google Scholar] [CrossRef]
- Hirschmann, G.S.; Arias, A.R. A survey of medicinal plants in Minas Gerais, Brazil. J. Ethnopharmacol. 1990, 29, 159–172. [Google Scholar] [CrossRef] [PubMed]
- Ruppelt, B.M.; Pereira, E.F.; Gonçalves, L.C.; Pereira, N.A. Pharmacological screening of plants recommended by folk medicine as anti-snake venom—I. Analgesic and anti-inflammatory activities. Mem. Inst. Oswaldo Cruz 1991, 86, 203–205. [Google Scholar] [CrossRef]
- Esteves, I.; Souza, I.R.; Rodrigues, M.; Cardoso, L.G.; Santos, L.; Sertie, J.; Perazzo, F.; Lima, L.; Schneedorf, J.M.; Bastos, J.; et al. Gastric anti-ulcer and anti-inflammatory activities of the essential oil from Casearia sylvestris Sw. J. Ethnorpharmacol. 2005, 101, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Mattos, E.S.; Frederico, M.J.S.; Colle, T.D.; Pieri, D.V.; Peters, R.R.; Piovezan, A.P. Evaluation of antinociceptive activity of Casearia sylvestris and possible mechanism of action. J. Ethnopharmacol. 2007, 112, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.T.; Mata, A.M.O.; Aguiar, R.P.S. Therapeutic potential of essential oils focusing on diterpenes. Phyt. Res. 2016, 30, 1420–1444. [Google Scholar] [CrossRef]
- Hunskaar, S.; Fasmer, O.B.; Hole, K. Formalin test in mice, a useful technique for evaluating mild analgesics. J. Neurosci. Methods 1985, 14, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Tjølsen, A.; Berge, O.G.; Hunskaar, S.; Rosland, J.H.; Hole, K. The formalin test: An evaluation of the method. Pain 1992, 51, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Rosland, J.H.; Tjølsen, A.; Maehle, B.; Hole, K. The formalin test in mice: Effect of formalin concentration. Pain 1990, 42, 235–242. [Google Scholar] [CrossRef]
- Akca, O.; Doufas, A.G.; Sessler, D.I. Use of selective opiate receptor inhibitors to prevent postoperative ileus. Minerva Anestesiol. 2002, 68, 162–165. [Google Scholar]
- Passos, F.F.; Lopes, E.M.; de Araujo, J.M.; de Sousa, D.P.; Veras, L.M.; Leite, J.R.; Almeida, F.R. Involvement of cholinergic and opioid system in gamma-terpinene-mediated antinociception. Evid. Based Complement. Alternat. Med. 2015, 2015, 829414. [Google Scholar] [CrossRef]
- Calás, T.; Wilkin, M.; Oliphant, C.M. Naloxone: An opportunity for another chance. J. Nurse Pract. 2016, 12, 154–160. [Google Scholar] [CrossRef]
- Gouveia, D.N.; Costa, J.S.; Oliveira, M.A.; Rabelo, T.K.; de Silva, A.M.O.; Carvalho, A.A. α-Terpineol reduces cancer pain via modulation of oxidative stress and inhibition of iNOS. Biomed. Pharmacother. 2018, 105, 652–661. [Google Scholar] [CrossRef]
- Mehanna, M.M.; Domiati, S.; Chmaisse, H.N.; El Mallah, A. Antinociceptive effect of tadalafil in various pain models: Involvement of opioid receptors and nitric oxide cyclic GMP pathway. Toxicol. Appl. Pharmacol. 2018, 352, 170–175. [Google Scholar] [CrossRef]
- Moore, P.K.; Wallace, P.; Hart, S.L.; Babbedge, R.C. Characterization of the novel nitric oxide synthase inhibitor 7-nitro indazole and related indazoles: Antinociceptive and cardiovascular effects. Br. J. Pharmacol. 1993, 110, 219–224. [Google Scholar] [CrossRef]
- Li, M.; Shang, X.; Zhang, R.; Jia, Z. Antinociceptive and anti-inflammatory activities of iridoid glycosides extract of Lamiophlomis rotata (Benth.) Kudo. Fitoterapia 2010, 81, 167–172. [Google Scholar] [CrossRef]
- Ferrari, S.; Vanti, C.; Pellizzer, M.; Dozza, L.; Monticone, M.; Pillastrini, P. Is there a relationship between self-efficacy, disability, pain and sociodemographic characteristics in chronic low back pain? A multicenter retrospective analysis. Arch. Physiother. 2019, 9, 1–9. [Google Scholar] [CrossRef]
- Jones, D.H.; Kilgour, R.D.; Comtois, A.S. Test–retest reliability of pressure pain threshold measurements of the upper limb and torso in young healthy women. J. Pain 2007, 8, 650–656. [Google Scholar] [CrossRef]
- Abelson, J.L.; Curtis, G.C.; Sagher, O.; Albucher, R.C.; Harrigan, M.; Taylor, S.F.; Martis, B.; Giordani, B. Deep brain stimulation for refractory obsessive-compulsive disorder. Biol. Psychiatry 2005, 57, 510–516. [Google Scholar] [CrossRef]
- Taguchi, K.; Kato, M.; Kikuta, J.; Abe, K.; Chikuma, T.; Utsunomiya, I. The effects of morphine-induced increases in extracellular acetylcholine levels in the rostral ventrolateral medulla of rat. J. Pharmacol. Exp. Ther. 1999, 289, 1539–1544. [Google Scholar]
- Naser, P.V.; Kuner, R. Molecular, cellular and circuit basis of cholinergic modulation of pain. Neuroscience 2017, 387, 135–148. [Google Scholar] [CrossRef]
- Tamaddonfard, E.; Erfanparast, A. Role of μ-opioid receptor in parafascicular nucleus of thalamus on morphine-induced antinociception in a rat model of acute trigeminal pain. Vet. Res. Forum 2017, 8, 29–34. [Google Scholar]
- Ong, H.M.; Ahmad Azmi, A.F.; Leong, S.W.; Abas, F.; Perimal, E.K.; Farouk, A.A.O.; Israf, D.A.; Sulaiman, M.R. The involvement of l-arginine-nitric oxide-cGMP-ATP-sensitive K+ channel pathway in antinociception of BBHC, a novel diarylpentanoid analogue, in mice model. Molecules 2021, 26, 7431. [Google Scholar] [CrossRef]
- Reis, F.J.; Rocha, N.P. Efeito analgésico de longa duração da dipirona sobre a hiperalgesia persistente induzida pela constrição do nervo ciático em ratos: Participação do óxido nítrico. Rev. Bras. Cienc. Farm. São Paulo 2006, 42, 513–522. [Google Scholar] [CrossRef][Green Version]
- Chen, T.S.; Huang, T.H.; Lai, M.C.; Huang, C.W. The role of glutamate receptors in epilepsy. Biomedicines 2023, 11, 783. [Google Scholar] [CrossRef]
- Wiggers, H.J.; Rocha, J.R.; Cheleski, J.; Montanari, C.A. Integration of ligand- and target-based virtual screening for the discovery of cruzain inhibitors. Mol. Inform. 2011, 30, 565–578. [Google Scholar] [CrossRef]
- Zhu, S.; Stein, R.A.; Yoshioka, C.; Lee, C.H.; Goehring, A.; McHaourab, H.S.; Gouaux, E. Mechanism of NMDA receptor inhibition and activation. Cell 2016, 165, 704–714. [Google Scholar] [CrossRef]
- Ellison, D.L. Physiology of pain. Crit. Care Nurs. Clin. N. Am. 2017, 29, 397–406. [Google Scholar] [CrossRef]
- Sauerstein, K.; Liebelt, J.; Namer, B.; Schmidt, R.; Rukwied, R.; Schmelz, M. Low-frequency stimulation of silent nociceptors induces secondary mechanical hyperalgesia in human skin. Neuroscience 2018, 387, 4–12. [Google Scholar] [CrossRef]
- Borges, M.H.; Soares, A.M.; Rodrigues, V.M. Effects of aqueous extract of Casearia sylvestris (Flacourtiaceae) on actions of snake and bee venoms and on activity of phospholipases A2. Comp. Biochem. Physiol. B Biochem. Mol. Biol. 2000, 127, 21–30. [Google Scholar] [CrossRef]
- Lozano-Ondoua, A.N.; Symons-Liguori, A.M.; Vanderah, T.W. Cancer-induced bone pain: Mechanisms and models. Neurosci. Lett. 2013, 557, 52–59. [Google Scholar] [CrossRef]
- Zhu, Y.F.; Kwiecien, J.M.; Dabrowski, W.; Ungard, R.; Zhu, K.L.; Huizinga, J.; Henry, J.; Singh, G. Cancer pain and neuropathic pain are associated with A beta sensory neuronal plasticity in dorsal root ganglia and abnormal sprouting in lumbar spinal cord. Mol. Pain 2018, 14, 1744806918810099. [Google Scholar] [CrossRef]
- Brazil. Presidency of the Republic General Secretary. Sub-office for Legal Affairs. Law nº 13,123/2015. Available online: http://www.planalto.gov.br/ccivil_03/_ato2015-2018/2015/lei/l13123.htm (accessed on 15 August 2022).
- Ferreira, P.M.P.; Machado, K.C.; Lavorato, S.N.; Oliveira, F.C.E.; Silva, J.N.; Almeida, A.A.C.; Santos, L.S.; Silva, V.R.; Bezerra, D.P.; Soares, M.B.P.; et al. Pharmacological and physicochemical profile of arylacetamides as tools against human cancers. Toxicol. Appl. Pharmacol. 2019, 380, 114692. [Google Scholar] [CrossRef]
- Waynforth, B.H.; Flecknell, P.A. Experimental and Surgical Techniques in the Rat, 2nd ed.; Academic Press: London, UK, 1995. [Google Scholar]
- Biermann, H.; Pietz, B.; Dreier, R.; Schmid, K.W.; Sorg, C.; Sunderkötter, C. Murine leukocytes with ring-shaped nuclei include granulocytes, monocytes, and their precursors. J. Leukoc. Biol. 1999, 65, 217–231. [Google Scholar] [CrossRef]
- Koster, R.; Anderson, M.; De Beer, E.J. Acetic Acid for Analgesic Screening. Fed. Proc. 1959, 18, 412–417. [Google Scholar]
- Beirith, A.; Santos, A.R.; Calixto, J.B. Mechanisms underlying the nociception and paw oedema caused by injection of glutamate into the mouse paw. Brain Res. 2002, 924, 219–228. [Google Scholar] [CrossRef]
- Guimarães, A.G.; Scotti, L.; Scotti, M.T.; Mendonça Júnior, F.J.B.; Melo, N.S.R.; Alves, R.S.; De Lucca Júnior, W.; Bezerra, D.P.; Gelain, D.P.; Quintans Júnior, L.J. Evidence for the involvement of descending pain-inhibitory mechanisms in the attenuation of cancer pain by carvacrol aided through a docking study. Life Sci. 2014, 116, 8–15. [Google Scholar] [CrossRef]
- Guimarães, A.G.; Oliveira, M.A.; Alves, R.S.; Menezes, P.P.; Serafini, M.R.; Souza Araújo, A.A.; Bezerra, D.P.; Quintans Júnior, L.J. Encapsulation of carvacrol, a monoterpene present in the essential oil of oregano, with β-cyclodextrin, improves the pharmacological response on cancer pain experimental protocols. Chem. Biol. Interact. 2015, 227, 69–76. [Google Scholar] [CrossRef]
- Ferreira, S.H. A new method for measuring variations of rat paw volume. J. Pharm. Pharmacol. 1979, 31, 648. [Google Scholar] [CrossRef]
- Broadhurst, P.L. Determinants of emotionality in the rat. Br. J. Psychol. 1957, 48, 1–12. [Google Scholar] [CrossRef]
- Archer, J. Tests for emotionality in rats and mice: A review. Anim. Behav. 1973, 21, 205–235. [Google Scholar] [CrossRef]
- Crawley, J.N. Behavioral phenotyping of transgenic and knockout mice: Experimental design and evaluation of general health, sensory functions, motor abilities, and specific behavioral tests. Brain Res. 1999, 835, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Chaplan, S.R.; Bach, W.F.; Pogrel, J.W.; Chung, J.M.; Yaksh, T.L. Quantitative assessment of tactile allodynia in the rat paw. J. Neurosci. Methods 1994, 53, 55–63. [Google Scholar] [CrossRef] [PubMed]


| Route | Sample | Dose (mg/kg) | Survival | g/100 g of Wet Body Mass | Tumor Mass (g) | % Tumor Inhibition | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Liver | Kidney | Lung | Heart | Stomach | ||||||
| Intraperitoneal | Vehicle | – | 12/12 | 4.91 ± 0.18 | 1.52 ± 0.04 | 0.86 ± 0.03 | 0.62 ± 0.02 | - | 1.08 ± 0.07 | - |
| 5-FU | 15 | 10/12 | 5.16 ± 0.51 | 1.66 ± 0.08 | 0.97 ± 0.07 | 0.68 ± 0.02 | - | 0.69 ± 0.03 * | 36.34 * | |
| FC | 5 | 12/12 | 4.71 ± 0.24 | 1.73 ± 0.04 | 0.97 ± 0.03 | 0.67 ± 0.04 | - | 0.74 ± 0.05 * | 31.12 * | |
| 10 | 12/12 | 5.41 ± 0.29 | 1.52 ± 0.07 | 0.81 ± 0.04 | 0.61 ± 0.03 | - | 0.66 ± 0.05 * | 39.27 * | ||
| Oral | Vehicle | – | 12/12 | 4.81 ± 0.22 | 1.51 ± 0.06 | 0.90 ± 0.04 | 0.60 ± 0.02 | 1.36 ± 0.13 | 1.06 ± 0.04 | - |
| FC | 10 | 12/12 | 4.80 ± 0.19 | 1.52 ± 0.05 | 0.86 ± 0.04 | 0.59 ± 0.02 | 1.13 ± 0.08 | 0.99 ± 0.04 | 6.05 | |
| 25 | 12/12 | 4.42 ± 0.16 | 1.60 ± 0.06 | 0.99 ± 0.05 | 0.66 ± 0.05 | 1.35 ± 0.08 | 0.70 ± 0.06 * | 34.12 * | ||
| Route | Sample | Dose (mg/kg) | Erythrocytes (106 Cell/µL) | Total Leukocytes (103 Cél/µL) | Differential Leukocyte Count (%) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Basophils | Eosinophils | Neutrophils | Lymphocytes | Monocytes | |||||
| Intraperitoneal | Vehicle | - | 8.23 ± 0.30 | 3.86 ± 0.34 | 0 | 1 | 73.75 | 24.25 | 1 |
| 5-FU | 15 | 7.06 ± 0.91 | 2.23 ± 0.20 * | 0 | 1 | 48.00 | 50.00 | 1 | |
| FC | 5 | 7.16 ± 0.90 | 3.71 ± 0.72 | 0 | 1 | 47.60 | 50.40 | 1 | |
| 10 | 7.23 ± 0.20 | 4.40 ± 0.99 | 0 | 1 | 61.00 | 37.00 | 1 | ||
| Oral | Vehicle | - | 9.58 ± 0.60 | 5.06 ± 0.80 | 0 | 1 | 78.89 | 19.11 | 1 |
| FC | 10 | 7.75 ± 0.55 | 5.05 ± 0.90 | 0 | 1 | 64.00 | 32.25 | 1 | |
| 25 | 7.66 ± 0.72 | 3.14 ± 0.49 | 0 | 1 | 33.80 | 64.20 | 1 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, J.d.N.; Beserra Filho, J.I.A.; Acha, B.T.; Almeida, F.R.d.C.; Batista, E.K.F.; Silva, V.R.; Bomfim, L.M.; Soares, M.B.P.; Bezerra, D.P.; dos Santos, A.G.; et al. Promising Effects of Casearins in Tumor-Bearing Mice and Antinociceptive Action against Oncologic Pain: Molecular Docking and In Vivo Findings. Pharmaceuticals 2024, 17, 633. https://doi.org/10.3390/ph17050633
Silva JdN, Beserra Filho JIA, Acha BT, Almeida FRdC, Batista EKF, Silva VR, Bomfim LM, Soares MBP, Bezerra DP, dos Santos AG, et al. Promising Effects of Casearins in Tumor-Bearing Mice and Antinociceptive Action against Oncologic Pain: Molecular Docking and In Vivo Findings. Pharmaceuticals. 2024; 17(5):633. https://doi.org/10.3390/ph17050633
Chicago/Turabian StyleSilva, Jurandy do Nascimento, José Ivo Araújo Beserra Filho, Boris Timah Acha, Fernanda Regina de Castro Almeida, Emanuelle Karine Frota Batista, Valdenizia Rodrigues Silva, Larissa Mendes Bomfim, Milena Botelho Pereira Soares, Daniel Pereira Bezerra, André Gonzaga dos Santos, and et al. 2024. "Promising Effects of Casearins in Tumor-Bearing Mice and Antinociceptive Action against Oncologic Pain: Molecular Docking and In Vivo Findings" Pharmaceuticals 17, no. 5: 633. https://doi.org/10.3390/ph17050633
APA StyleSilva, J. d. N., Beserra Filho, J. I. A., Acha, B. T., Almeida, F. R. d. C., Batista, E. K. F., Silva, V. R., Bomfim, L. M., Soares, M. B. P., Bezerra, D. P., dos Santos, A. G., de Andrade, F. d. C. P., Mendes, A. N., Arcanjo, D. D. R., & Ferreira, P. M. P. (2024). Promising Effects of Casearins in Tumor-Bearing Mice and Antinociceptive Action against Oncologic Pain: Molecular Docking and In Vivo Findings. Pharmaceuticals, 17(5), 633. https://doi.org/10.3390/ph17050633









