Design of Experiment (DoE) Approach for Developing Inhalable PLGA Microparticles Loaded with Clofazimine for Tuberculosis Treatment
Abstract
1. Introduction
2. Results and Discussion
2.1. Characterization of CFZ MP
2.2. Spray Drying
2.2.1. Experimental Design
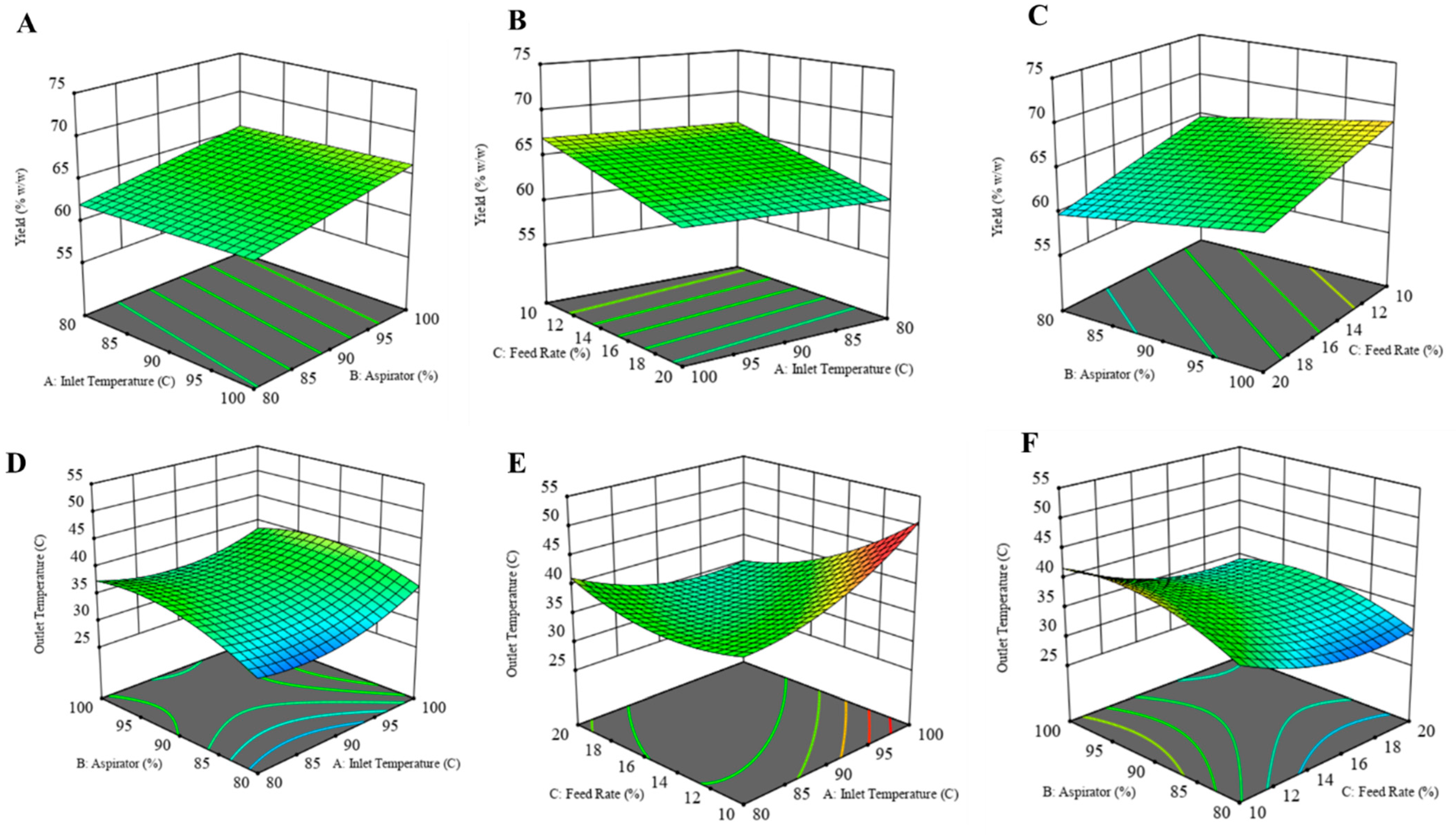
2.2.2. Response Surface Mapping
Product Yield
Outlet Temperature
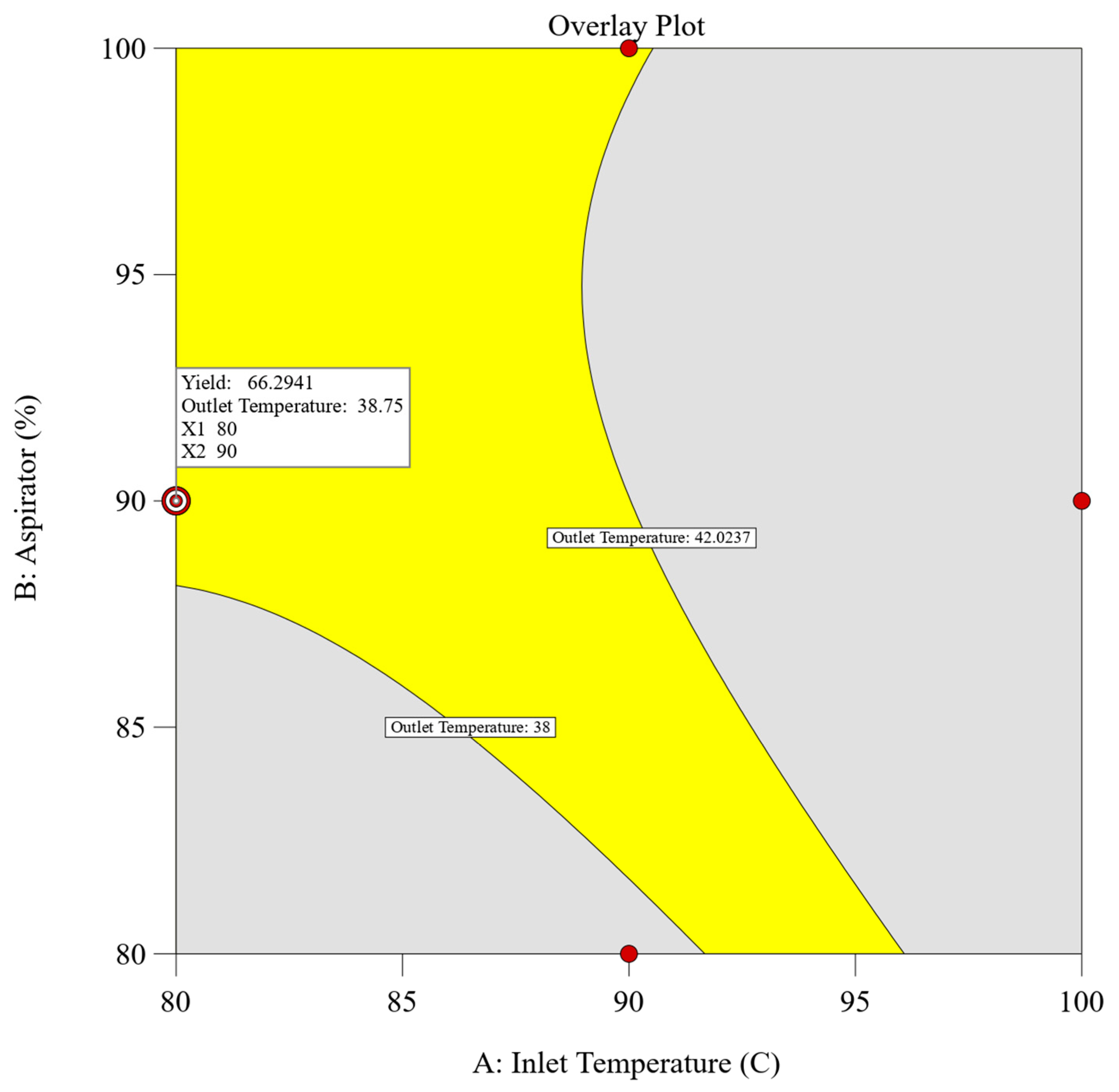
2.2.3. Determination of Design Space
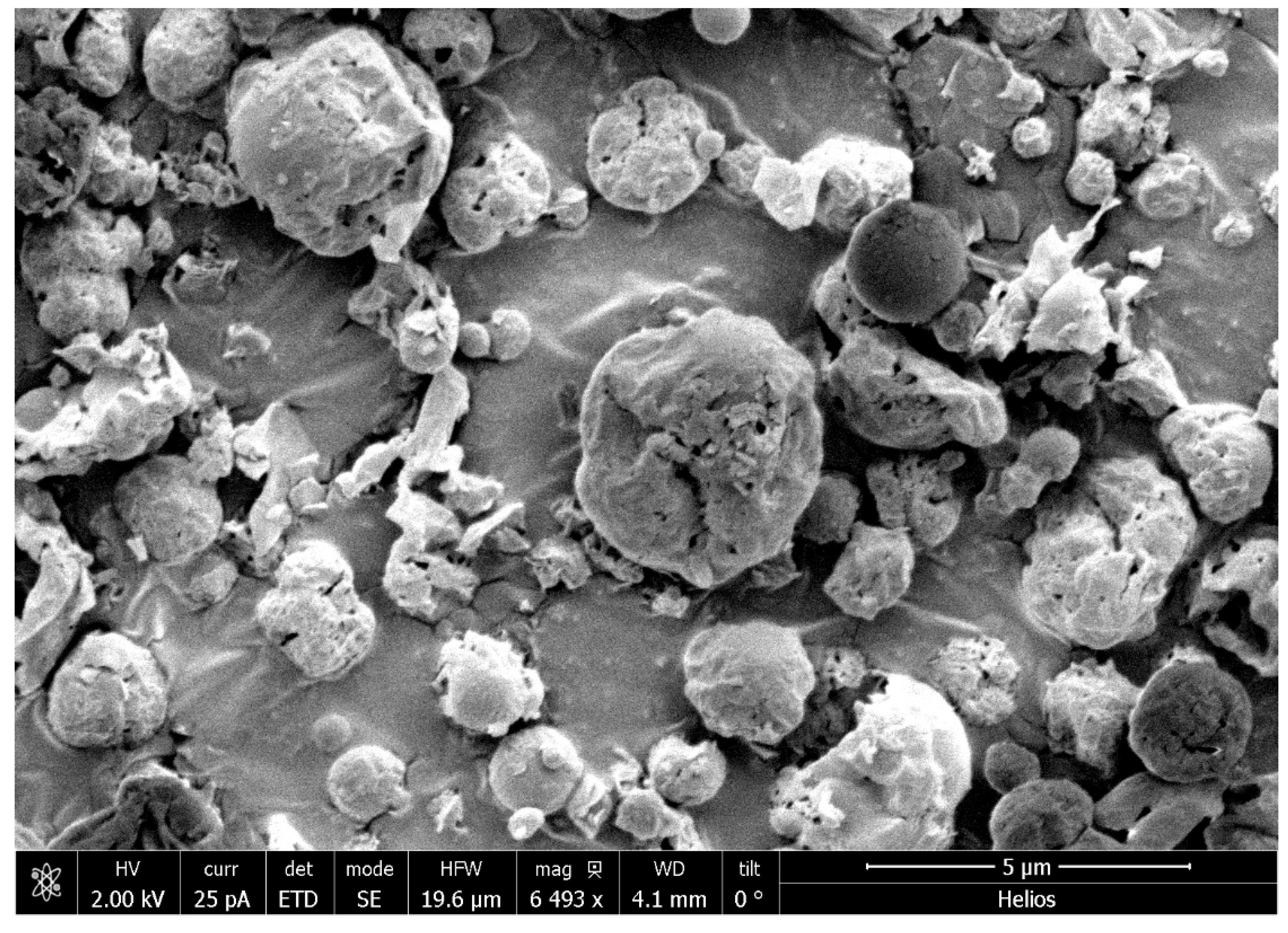
2.3. Optimized Dry Powder Formulation
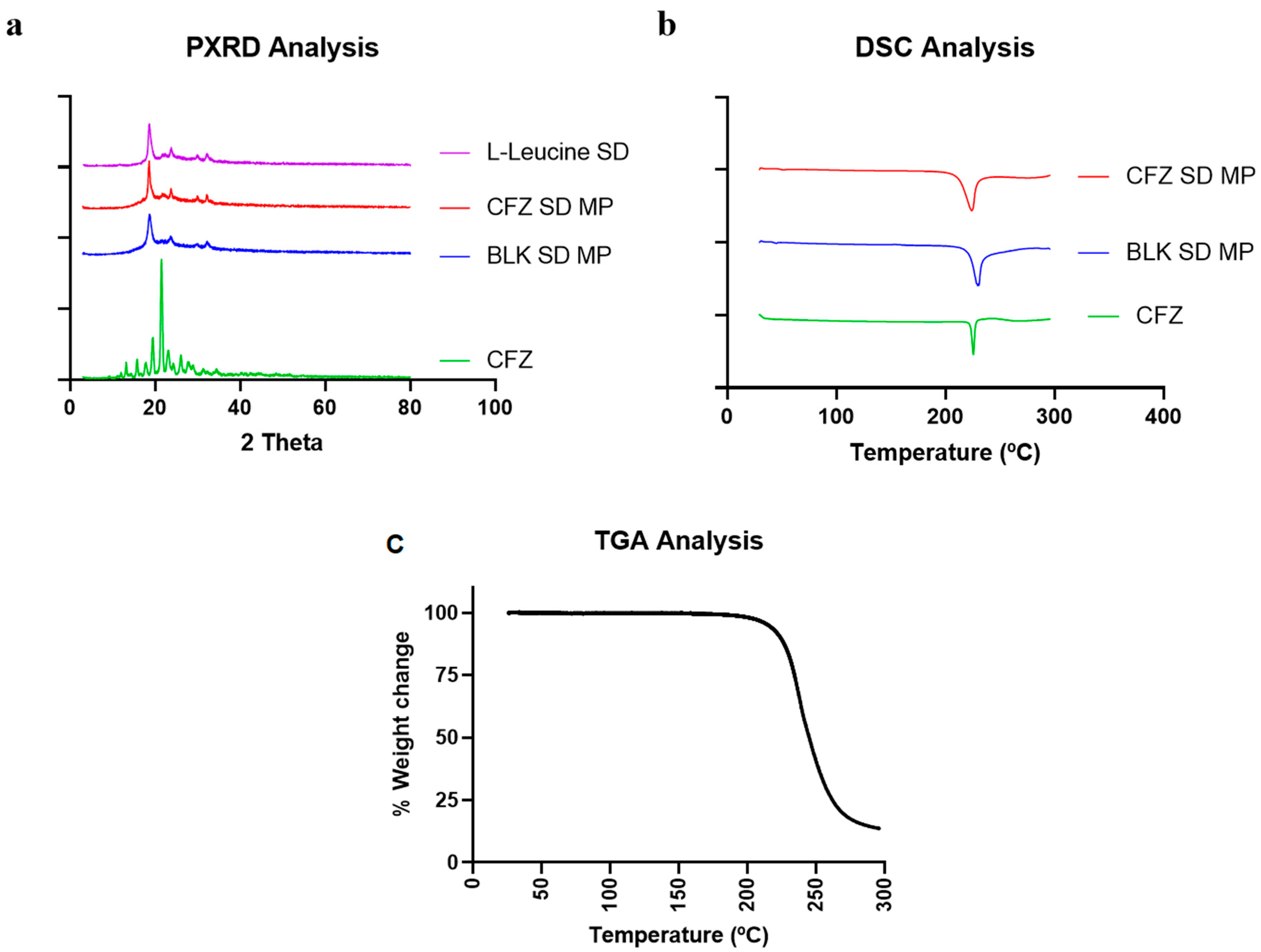
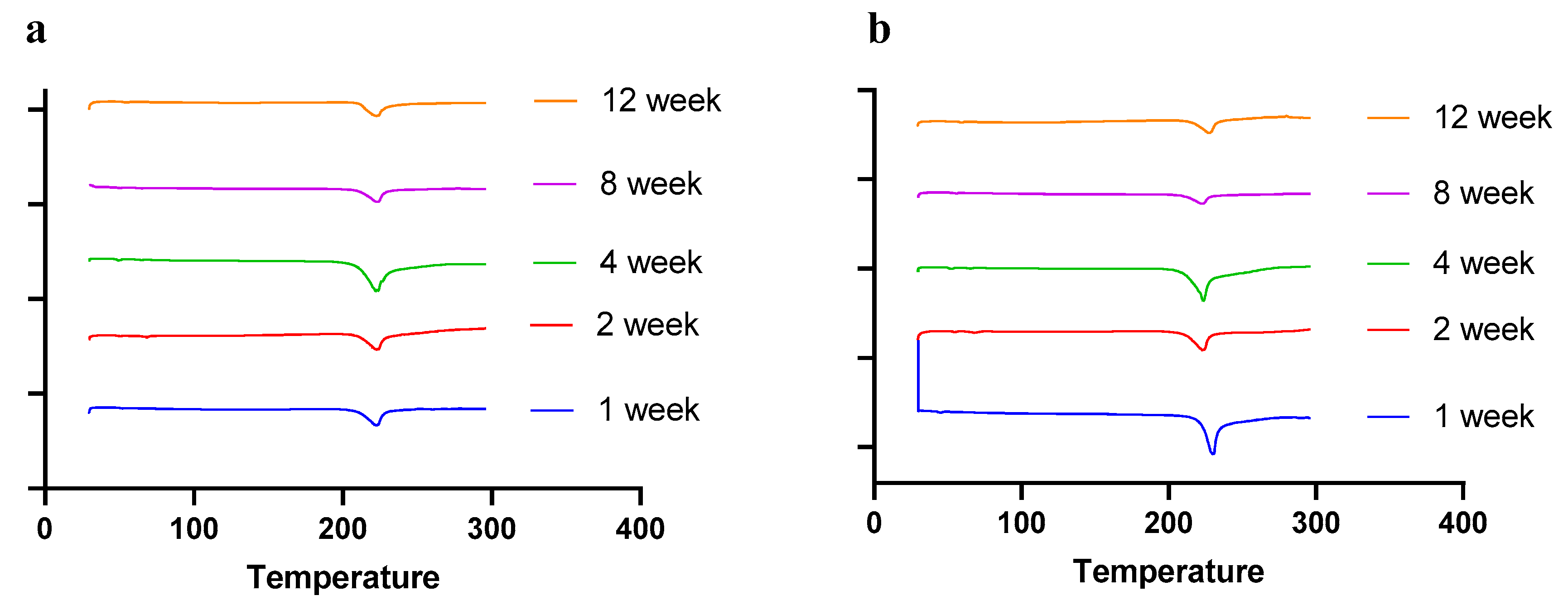
2.4. Solid State Characterization (DSC, PXRD, TGA)
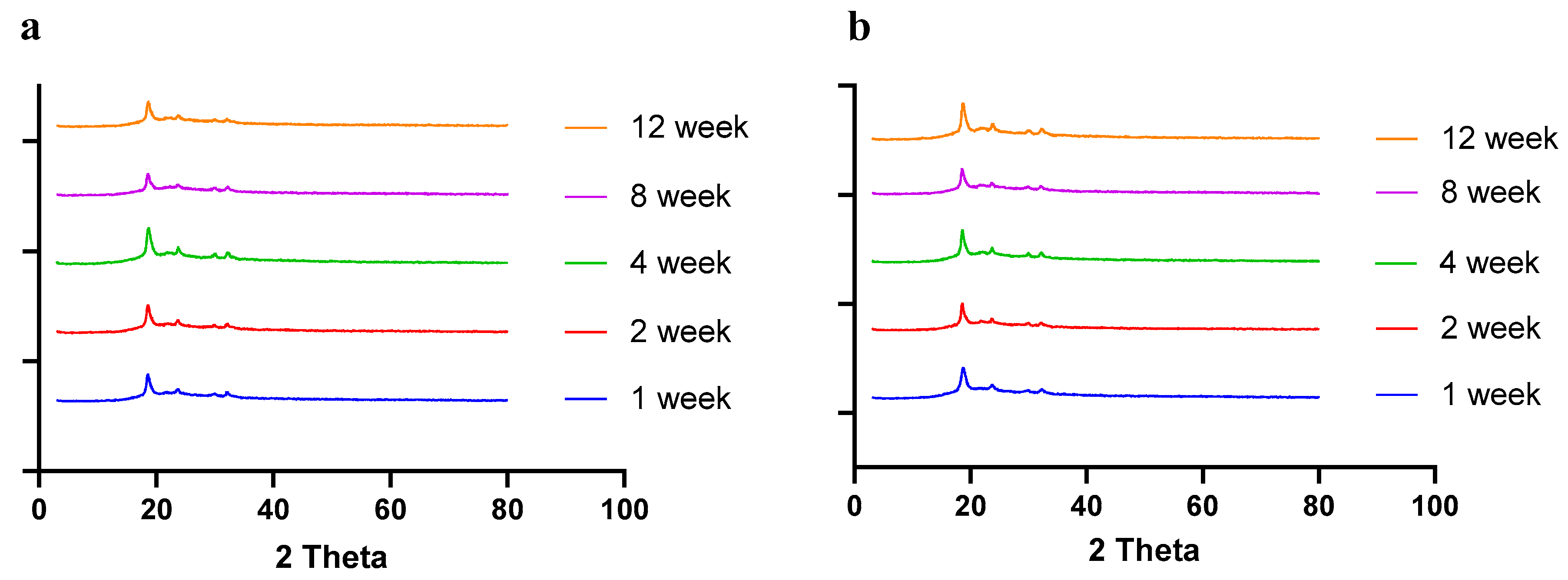
2.4.1. Powder X-ray Diffraction (PXRD)
2.4.2. Differential Scanning Calorimetry and Thermogravimetric Analysis (DSC and TGA)
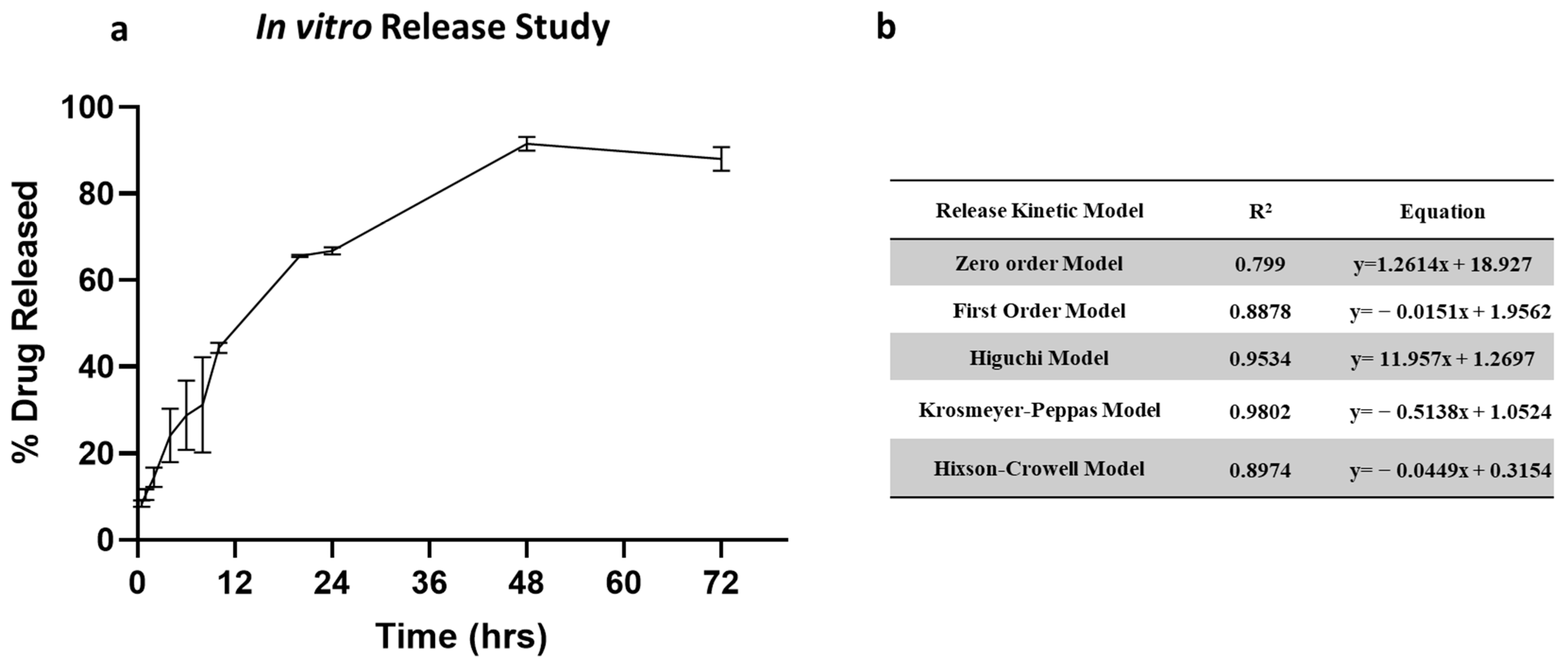
2.5. In Vitro Release Study
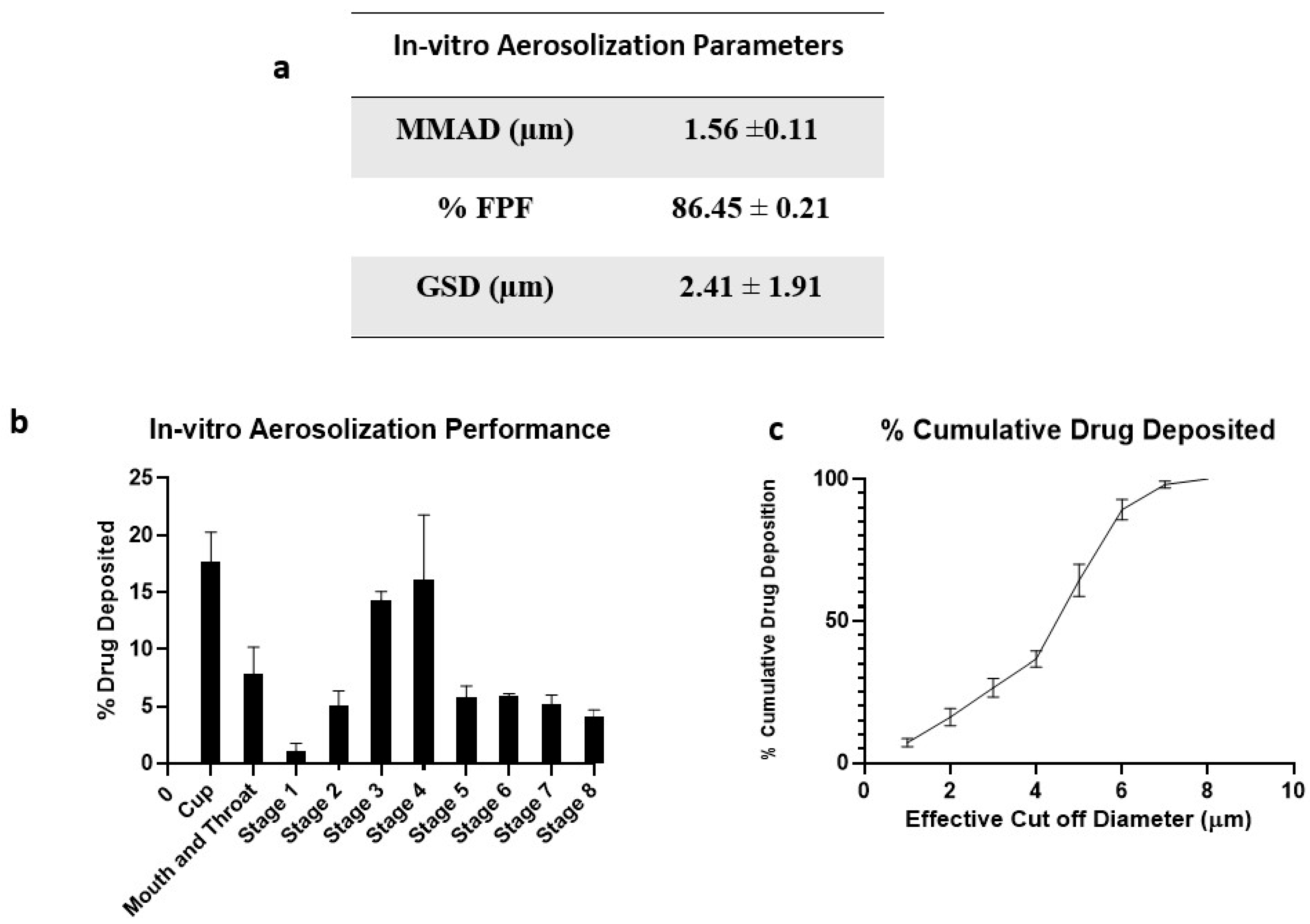
2.6. In Vitro Aerosolization Studies
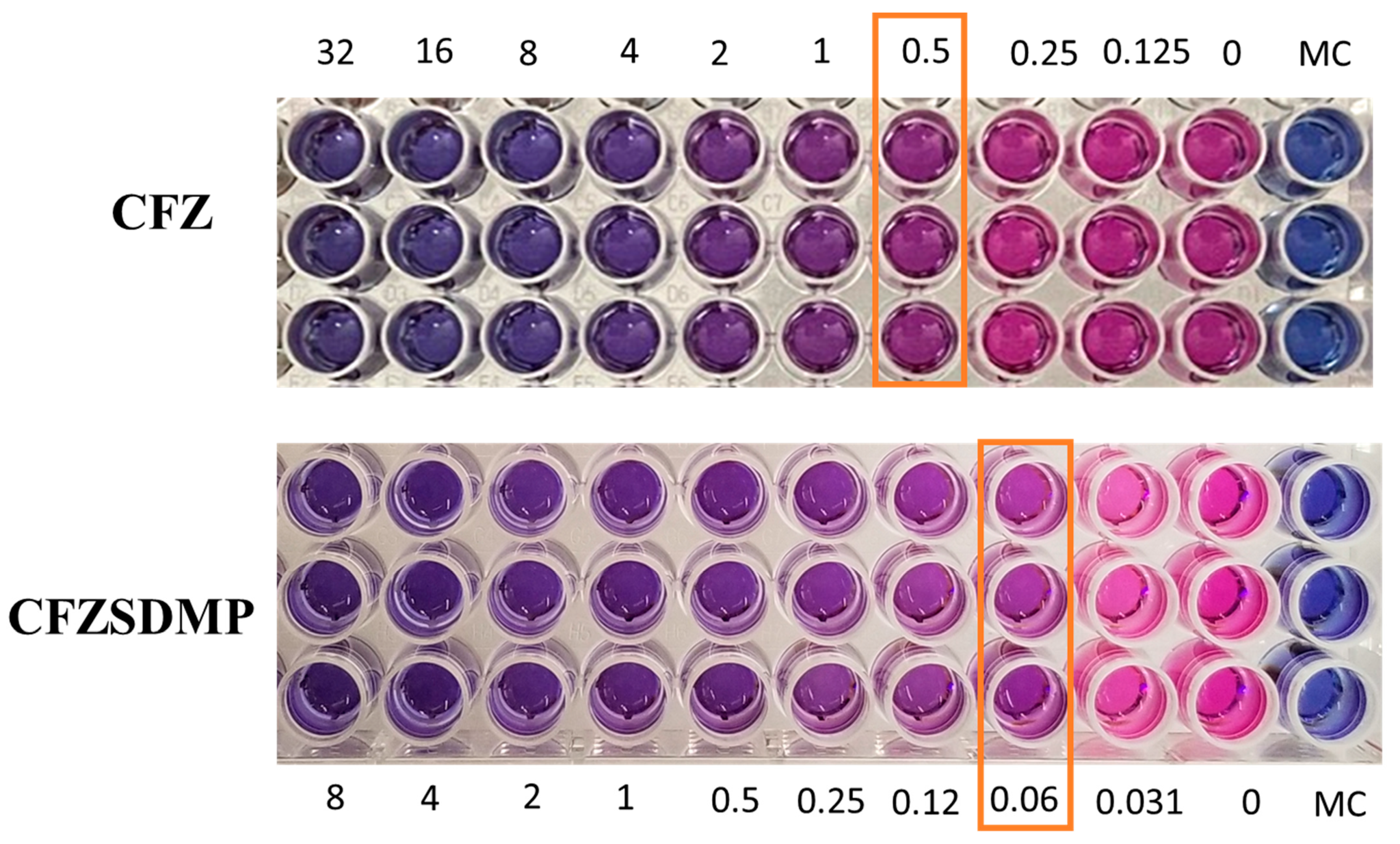
2.7. In Vitro Anti-Microbial Activity (MIC) Studies
2.8. Stability Studies
3. Materials and Methods
3.1. Materials
3.2. Preparation of CFZ-Loaded PLGA MPs
3.2.1. Characterization of CFZ PLGA MPs
Particle Size and Zeta-potential
Entrapment Efficiency and Drug Loading
3.3. Experimental Design
3.4. Preparation of Spray-Dried CFZ MPs
3.4.1. Spray Drying Product Yield
3.4.2. Resuspendibility
3.5. Morphology
3.6. Solid-State Characterization of Clofazimine Spray-Dried MPs
3.6.1. Differential Scanning Calorimetry (DSC)
3.6.2. Powder X-ray Diffraction (PXRD)
3.6.3. Thermogravimetric Analysis (TGA)
3.7. In Vitro Release Study
3.8. In Vitro Aerosolization Study
3.9. Stability Studies
3.10. Resazurin-Based Microtiter Plate Assay
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO Guidelines on Tuberculosis Documentation for World Health Assembly 67. World Health Organization. Available online: https://www.who.int/publications/digital/global-tuberculosis-report-2021/featured-topics/tb-guidelines (accessed on 28 May 2024).
- Center for Disease Control and Prevention Basic Tuberculosis (TB) Facts. Available online: https://www.cdc.gov/tb/topic/basics/default.h (accessed on 28 May 2024).
- Natarajan, A.; Beena, P.M.; Devnikar, A.V.; Mali, S. A Systemic Review on Tuberculosis. Indian J. Tuberc. 2020, 67, 295–311. [Google Scholar] [CrossRef]
- Sun, J.; Champion, P.A.; Bigi, F. Editorial: Cellular and Molecular Mechanisms of Mycobacterium Tuberculosis Virulence. Front. Cell. Infect. Microbiol. 2019, 9, 331. [Google Scholar] [CrossRef]
- Bussi, C.; Gutierrez, M.G. Mycobacterium Tuberculosis Infection of Host Cells in Space and Time. FEMS Microbiol. Rev. 2019, 43, 341–361. [Google Scholar] [CrossRef]
- Pai, M.; Behr, M.A.; Dowdy, D.; Dheda, K.; Divangahi, M.; Boehme, C.C.; Ginsberg, A.; Swaminathan, S.; Spigelman, M.; Getahun, H.; et al. Tuberculosis. Nat. Rev. Dis. Primer 2016, 2, 16076. [Google Scholar] [CrossRef]
- TB Guidelines. Available online: https://www.cdc.gov/tb/publications/guidelines/treatment.htm (accessed on 28 May 2024).
- Brunaugh, A.D.; Jan, S.U.; Ferrati, S.; Smyth, H.D.C. Excipient-Free Pulmonary Delivery and Macrophage Targeting of Clofazimine via Air Jet Micronization. Mol. Pharm. 2017, 14, 4019–4031. [Google Scholar] [CrossRef]
- Lange, C.; Chesov, D.; Heyckendorf, J. Clofazimine for the Treatment of Multidrug-Resistant Tuberculosis. Clin. Microbiol. Infect. 2019, 25, 128–130. [Google Scholar] [CrossRef]
- Espinosa-Pereiro, J.; Sánchez-Montalvá, A.; Aznar, M.L.; Espiau, M. MDR Tuberculosis Treatment. Med. Kaunas Lith. 2022, 58, 188. [Google Scholar] [CrossRef]
- Holdiness, M.R. Clinical Pharmacokinetics of Clofazimine. Clin. Pharmacokinet. 1989, 16, 74–85. [Google Scholar] [CrossRef]
- Cholo, M.C.; Steel, H.C.; Fourie, P.B.; Germishuizen, W.A.; Anderson, R. Clofazimine: Current Status and Future Prospects. J. Antimicrob. Chemother. 2011, 67, 290–298. [Google Scholar] [CrossRef]
- Mehta, P.; Bothiraja, C.; Kadam, S.; Pawar, A. Potential of Dry Powder Inhalers for Tuberculosis Therapy: Facts, Fidelity and Future. Artif. Cells Nanomed. Biotechnol. 2018, 46, S791–S806. [Google Scholar] [CrossRef] [PubMed]
- Parumasivam, T.; Chang, R.Y.K.; Abdelghany, S.; Ye, T.T.; Britton, W.J.; Chan, H.-K. Dry Powder Inhalable Formulations for Anti-Tubercular Therapy. Adv. Drug Deliv. Rev. 2016, 102, 83–101. [Google Scholar] [CrossRef]
- Choi, J.-C.; Kang, J.-H.; Kim, D.-W.; Park, C.-W. Preparation and Evaluation of Inhalable Amifostine Microparticles Using Wet Ball Milling. Pharmaceutics 2023, 15, 1696. [Google Scholar] [CrossRef]
- Oh, Y.J.; Lee, J.; Seo, J.Y. Preparation of Budesonide-Loaded Porous PLGA Microparticles and Their Therapeutic Efficacy in a Murine Asthma Model. J Control. Release 2011, 150, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Wischke, C.; Schwendeman, S.P. Principles of Encapsulating Hydrophobic Drugs in PLA/PLGA Microparticles. Int. J. Pharm. 2008, 364, 298–327. [Google Scholar] [CrossRef]
- Lagreca, E.; Onesto, V.; Di Natale, C.; La Manna, S.; Netti, P.A.; Vecchione, R. Recent Advances in the Formulation of PLGA Microparticles for Controlled Drug Delivery. Prog. Biomater. 2020, 9, 153–174. [Google Scholar] [CrossRef]
- Bao, T.Q.; Hiep, N.T.; Kim, Y.H.; Yang, H.M.; Lee, B.T. Fabrication and Characterization of Porous Poly(Lactic-Co-Glycolic Acid) (PLGA) Microspheres for Use as a Drug Delivery System. J. Mater. Sci. 2011, 46, 2510–2517. [Google Scholar] [CrossRef]
- Biswal, A.K.; Hariprasad, P.; Saha, S. Efficient and Prolonged Antibacterial Activity from Porous PLGA Microparticles and Their Application in Food Preservation. Mater. Sci. Eng. C 2020, 108, 110496. [Google Scholar] [CrossRef]
- Kunda, N.; Alfagih, I.; Saleem, I.; Hutcheon, G. Polymer-Based Delivery Systems for the Pulmonary Delivery of Biopharmaceuticals. In Pulmonary Drug Delivery: Advances and Challenges; Wiley: Hoboken, NJ, USA, 2015; pp. 301–320. ISBN 978-1-118-79954-3. [Google Scholar]
- Zendehdel Baher, S.; Yaqoubi, S.; Asare-Addo, K.; Hamishehkar, H.; Nokhodchi, A. Dry Powder Formulation of Simvastatin Nanoparticles for Potential Application in Pulmonary Arterial Hypertension. Pharmaceutics 2022, 14, 895. [Google Scholar] [CrossRef]
- Han, F.Y.; Thurecht, K.J.; Whittaker, A.K.; Smith, M.T. Bioerodable PLGA-Based Microparticles for Producing Sustained-Release Drug Formulations and Strategies for Improving Drug Loading. Front. Pharmacol. 2016, 7, 185. [Google Scholar] [CrossRef]
- Lee, W.-H.; Loo, C.-Y.; Traini, D.; Young, P.M. Nano- and Micro-Based Inhaled Drug Delivery Systems for Targeting Alveolar Macrophages. Expert Opin. Drug Deliv. 2015, 12, 1009–1026. [Google Scholar] [CrossRef]
- Makino, K.; Yamamoto, N.; Higuchi, K.; Harada, N.; Ohshima, H.; Terada, H. Phagocytic Uptake of Polystyrene Microspheres by Alveolar Macrophages: Effects of the Size and Surface Properties of the Microspheres. Colloids Surf. B Biointerfaces 2003, 27, 33–39. [Google Scholar] [CrossRef]
- Parikh, R.; Dalwadi, S.; Aboti, P.; Patel, L. Inhaled Microparticles of Antitubercular Antibiotic for in Vitro and in Vivo Alveolar Macrophage Targeting and Activation of Phagocytosis. J. Antibiot. 2014, 67, 387–394. [Google Scholar] [CrossRef]
- Lim, P.N.; Cervantes, M.M.; Pham, L.K.; Rothchild, A.C. Alveolar Macrophages: Novel Therapeutic Targets for Respiratory Diseases. Expert Rev. Mol. Med. 2021, 23, e18. [Google Scholar] [CrossRef]
- Kemala, T.; Budianto, E.; Soegiyono, B. Preparation and Characterization of Microspheres Based on Blend of Poly(Lactic Acid) and Poly(ɛ-Caprolactone) with Poly(Vinyl Alcohol) as Emulsifier. Arab. J. Chem. 2012, 5, 103–108. [Google Scholar] [CrossRef]
- Quintanar-Guerrero, D.; Fessi, H.; Allémann, E.; Doelker, E. Influence of Stabilizing Agents and Preparative Variables on the Formation of Poly(d,l-Lactic Acid) Nanoparticles by an Emulsification-Diffusion Technique. Int. J. Pharm. 1996, 143, 133–141. [Google Scholar] [CrossRef]
- Kunda, N.K.; Alfagih, I.M.; Miyaji, E.N.; Figueiredo, D.B.; Gonçalves, V.M.; Ferreira, D.M.; Dennison, S.R.; Somavarapu, S.; Hutcheon, G.A.; Saleem, I.Y. Pulmonary Dry Powder Vaccine of Pneumococcal Antigen Loaded Nanoparticles. Int. J. Pharm. 2015, 495, 903–912. [Google Scholar] [CrossRef]
- Wang, X.; Wan, W.; Lu, J.; Quan, G.; Pan, X.; Liu, P. Effects of L-Leucine on the Properties of Spray-Dried Swellable Microparticles with Wrinkled Surfaces for Inhalation Therapy of Pulmonary Fibrosis. Int. J. Pharm. 2021, 610, 121223. [Google Scholar] [CrossRef]
- Kunda, N.K.; Alfagih, I.M.; Dennison, S.R.; Tawfeek, H.M.; Somavarapu, S.; Hutcheon, G.A.; Saleem, I.Y. Bovine Serum Albumin Adsorbed PGA-Co-PDL Nanocarriers for Vaccine Delivery via Dry Powder Inhalation. Pharm. Res. 2015, 32, 1341–1353. [Google Scholar] [CrossRef]
- Takeuchi, I.; Taniguchi, Y.; Tamura, Y.; Ochiai, K.; Makino, K. Effects of L-Leucine on PLGA Microparticles for Pulmonary Administration Prepared Using Spray Drying: Fine Particle Fraction and Phagocytotic Ratio of Alveolar Macrophages. Colloids Surf. A 2018, 537, 411–417. [Google Scholar] [CrossRef]
- Li, L.; Sun, S.; Parumasivam, T.; Denman, J.A.; Gengenbach, T.; Tang, P.; Mao, S.; Chan, H.-K. L-Leucine as an Excipient against Moisture on in Vitro Aerosolization Performances of Highly Hygroscopic Spray-Dried Powders. Eur. J. Pharm. Biopharm. 2016, 102, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Dharmadhikari, A.S.; Kabadi, M.; Gerety, B.; Hickey, A.J.; Fourie, P.B.; Nardell, E. Phase I, Single-Dose, Dose-Escalating Study of Inhaled Dry Powder Capreomycin: A New Approach to Therapy of Drug-Resistant Tuberculosis. Antimicrob. Agents Chemother. 2013, 57, 2613–2619. [Google Scholar] [CrossRef] [PubMed]
- Maury, M.; Murphy, K.; Kumar, S.; Shi, L.; Lee, G. Effects of Process Variables on the Powder Yield of Spray-Dried Trehalose on a Laboratory Spray-Dryer. Eur. J. Pharm. Biopharm. 2005, 59, 565–573. [Google Scholar] [CrossRef] [PubMed]
- Focaroli, S.; Mah, P.T.; Hastedt, J.E.; Gitlin, I.; Oscarson, S.; Fahy, J.V.; Healy, A.M. A Design of Experiment (DoE) Approach to Optimise Spray Drying Process Conditions for the Production of Trehalose/Leucine Formulations with Application in Pulmonary Delivery. Int. J. Pharm. 2019, 562, 228–240. [Google Scholar] [CrossRef] [PubMed]
- Park, K.; Otte, A.; Sharifi, F.; Garner, J.; Skidmore, S.; Park, H.; Jhon, Y.K.; Qin, B.; Wang, Y. Potential Roles of the Glass Transition Temperature of PLGA Microparticles in Drug Release Kinetics. Mol. Pharm. 2021, 18, 18–32. [Google Scholar] [CrossRef] [PubMed]
- Saha, T.; Sinha, S.; Harfoot, R.; Quinones-Mateu, M.; Das, S. Manipulation of Spray-Drying Conditions to Develop an Inhalable Ivermectin Dry Powder. Pharmaceutics 2022, 14, 1432. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Yang, Z.; Ren, Y.; Mei, X. Effects of Formulation and Operating Variables on Zanamivir Dry Powder Inhalation Characteristics and Aerosolization Performance. Drug Deliv. 2014, 21, 480–486. [Google Scholar] [CrossRef]
- Chang, Y.-X.; Yang, J.-J.; Pan, R.-L.; Chang, Q.; Liao, Y.-H. Anti-Hygroscopic Effect of Leucine on Spray-Dried Herbal Extract Powders. Powder Technol. 2014, 266, 388–395. [Google Scholar] [CrossRef]
- Tavares, M.; Cabral, R.P.; Costa, C.; Martins, P.; Fernandes, A.R.; Casimiro, T.; Aguiar-Ricardo, A. Development of PLGA Dry Powder Microparticles by Supercritical CO2-Assisted Spray-Drying for Potential Vaccine Delivery to the Lungs. J. Supercrit. Fluids 2017, 128, 235–243. [Google Scholar] [CrossRef]
- Wang, Y.-B.; Watts, A.B.; Peters, J.I.; Liu, S.; Batra, A.; Williams, R.O. In Vitro and In Vivo Performance of Dry Powder Inhalation Formulations: Comparison of Particles Prepared by Thin Film Freezing and Micronization. AAPS PharmSciTech 2014, 15, 981–993. [Google Scholar] [CrossRef]
- Shetty, N.; Park, H.; Zemlyanov, D.; Mangal, S.; Bhujbal, S.; Zhou, Q.T. Influence of Excipients on Physical and Aerosolization Stability of Spray Dried High-Dose Powder Formulations for Inhalation. Int. J. Pharm. 2018, 544, 222–234. [Google Scholar] [CrossRef]
- Rosati, J.A.; Leith, D.; Kim, C.S. Monodisperse and Polydisperse Aerosol Deposition in a Packed Bed. Aerosol Sci. Technol. 2003, 37, 528–535. [Google Scholar] [CrossRef]
- Jadaun, G.P.S.; Agarwal, C.; Sharma, H.; Ahmed, Z.; Upadhyay, P.; Faujdar, J.; Gupta, A.K.; Das, R.; Gupta, P.; Chauhan, D.S.; et al. Determination of Ethambutol MICs for Mycobacterium Tuberculosis and Mycobacterium Avium Isolates by Resazurin Microtitre Assay. J. Antimicrob. Chemother. 2007, 60, 152–155. [Google Scholar] [CrossRef] [PubMed]
- Banfi, E.; Scialino, G.; Monti-Bragadin, C. Development of a Microdilution Method to Evaluate Mycobacterium Tuberculosis Drug Susceptibility. J. Antimicrob. Chemother. 2003, 52, 796–800. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Zheng, M.-Q.; Wang, B.; Zhao, W.-J.; Li, P.; Chu, N.-H.; Liang, B.-W. [Activities of clofazimine against Mycobacterium tuberculosis in vitro and in vivo]. Zhonghua Jie He He Hu Xi Za Zhi 2008, 31, 752–755. [Google Scholar] [PubMed]
- Wang, W.; Zhou, Q.T.; Sun, S.-P.; Denman, J.A.; Gengenbach, T.R.; Barraud, N.; Rice, S.A.; Li, J.; Yang, M.; Chan, H.-K. Effects of Surface Composition on the Aerosolisation and Dissolution of Inhaled Antibiotic Combination Powders Consisting of Colistin and Rifampicin. AAPS J. 2016, 18, 372–384. [Google Scholar] [CrossRef] [PubMed]
- Chiou, D.; Langrish, T.A.G. Crystallization of Amorphous Components in Spray-Dried Powders. Dry. Technol. 2007, 25, 1427–1435. [Google Scholar] [CrossRef]
- Shetty, N.; Zeng, L.; Mangal, S.; Nie, H.; Rowles, M.R.; Guo, R.; Han, Y.; Park, J.H.; Zhou, Q.T. Effects of Moisture-Induced Crystallization on the Aerosol Performance of Spray Dried Amorphous Ciprofloxacin Powder Formulations. Pharm. Res. 2018, 35, 7. [Google Scholar] [CrossRef] [PubMed]
- Patil, S.M.; Diorio, A.M.; Kommarajula, P.; Kunda, N.K. A Quality-by-Design Strategic Approach for the Development of Bedaquiline-Pretomanid Nanoparticles as Inhalable Dry Powders for TB Treatment. Int. J. Pharm. 2024, 653, 123920. [Google Scholar] [CrossRef] [PubMed]
- Patil, S.M.; Sawant, S.S.; Kunda, N.K. Inhalable Bedaquiline-Loaded Cubosomes for the Treatment of Non-Small Cell Lung Cancer (NSCLC). Int. J. Pharm. 2021, 607, 121046. [Google Scholar] [CrossRef]
- Sawant, S.; Patil, S.; Shukla, S.; Kulkarni, N.; Gupta, V.; Kunda, N. Pulmonary Delivery of Osimertinib Liposomes for Non-Small Cell Lung Cancer Treatment: Formulation Development and in Vitro Evaluation. Drug Deliv. Transl. Res. 2022, 12, 2474–2487. [Google Scholar] [CrossRef]
- Kim, Y.; Park, E.J.; Kim, T.W.; Na, D.H. Recent Progress in Drug Release Testing Methods of Biopolymeric Particulate System. Pharmaceutics 2021, 13, 1313. [Google Scholar] [CrossRef] [PubMed]
- Patil, S.M.; Barji, D.S.; Aziz, S.; McChesney, D.A.; Bagde, S.; Muttil, P.; Kunda, N.K. Pulmonary Delivery of Spray-Dried Nisin ZP Antimicrobial Peptide for Non-Small Cell Lung Cancer (NSCLC) Treatment. Int. J. Pharm. 2023, 634, 122641. [Google Scholar] [CrossRef] [PubMed]
- Khalifa, R.A.; Nasser, M.S.; Gomaa, A.A.; Osman, N.M.; Salem, H.M. Resazurin Microtiter Assay Plate Method for Detection of Susceptibility of Multidrug Resistant Mycobacterium Tuberculosis to Second-Line Anti-Tuberculous Drugs. Egypt. J. Chest Dis. Tuberc. 2013, 62, 241–247. [Google Scholar] [CrossRef]
- Sharma, S.; Gelman, E.; Narayan, C.; Bhattacharjee, D.; Achar, V.; Humnabadkar, V.; Balasubramanian, V.; Ramachandran, V.; Dhar, N.; Dinesh, N. Simple and Rapid Method to Determine Antimycobacterial Potency of Compounds by Using Autoluminescent Mycobacterium Tuberculosis. Antimicrob. Agents Chemother. 2014, 58, 5801–5808. [Google Scholar] [CrossRef]
| MP Sample | Particle Size (µm) | Zeta Potential (mV) | % Entrapment Efficiency (%w/w) | Drug Loading µg/mg) |
|---|---|---|---|---|
| CFZMP001 @8000 rpm 10 min | 2.16 ± 0.15 | −29.06 ± 0.51 | 66.03 ± 2.04 | 33.62 ± 1.05 |
| CFZMP002 @10,000 rpm 12 min | 1.04 ± 0.08 | −31.42 ± 5.35 | 66.40 ± 2.22 | 33.06 ± 1.45 |
| S. No. | Independent Process Parameters | Dependent Product Parameters | |||
|---|---|---|---|---|---|
| SD Sample ID | Inlet Temperature (°C) | Feed Rate (%) | Aspirator Setting (%) | Yield (% w/w) | Outlet Temperature (°C) |
| CFZ01 | 100 | 15 | 100 | 64.44 | 41 |
| CFZ02 | 100 | 10 | 90 | 66.75 | 46 |
| CFZ03 | 80 | 20 | 90 | 63.86 | 46 |
| CFZ04 | 80 | 15 | 100 | 61.95 | 36 |
| CFZ05 | 90 | 20 | 100 | 63.84 | 31 |
| CFZ06 | 90 | 20 | 80 | 56.71 | 29 |
| CFZ07 | 90 | 10 | 80 | 61.58 | 40 |
| CFZ08 | 80 | 10 | 90 | 71.01 | 38 |
| CFZ09 | 90 | 15 | 90 | 61.92 | 36 |
| CFZ10 | 80 | 15 | 80 | 60.38 | 29 |
| CFZ11 | 90 | 15 | 90 | 67.72 | 36 |
| CFZ12 | 100 | 20 | 90 | 63.20 | 36 |
| CFZ13 | 100 | 15 | 80 | 65.21 | 38 |
| CFZ14 | 90 | 10 | 100 | 68.04 | 44 |
| CFZ15 | 90 | 15 | 90 | 65.52 | 36 |
| Responses | Model | R2 | Adj R2 | SD | %CV |
|---|---|---|---|---|---|
| Yield | Linear | 0.4396 | 0.2868 | 2.97 | 4.62 |
| Outlet Temperature | Quadratic | 0.7659 | 0.3446 | 4.35 | 11.60 |
| SD Sample | Inlet Temperature. (°C) | Pump % | Aspirator % | % Yield (%w/w) | Outlet Temperature (°C) | Drug Content (µg/mg) | Resuspending Index (%) |
|---|---|---|---|---|---|---|---|
| CFZ08 | 80 | 10 | 90 | 71.01 ± 3.67 | 38 | 19.33 ± 3.24 | 99.7% |
| MP Sample | MIC | MIC 4-Week 4 °C | MIC 12-Week 4 °C | MIC 12-Week 25 °C |
|---|---|---|---|---|
| CFZ-Free Drug | 0.25 to 0.5 µg/mL | |||
| CFZ SD MPs | 0.0625 µg/mL | 0.0625 µg/mL | 0.0625 µg/mL | 0.125 µg/mL |
| Independent Process Variables | |||
|---|---|---|---|
| Levels | Low (−1) | Medium (0) | High (+1) |
| INLET TEMPERATURE (℃) | 80 | 90 | 100 |
| ASPIRATOR (%) | 80 | 90 | 100 |
| FEED RATE (%) | 10 | 15 | 20 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rongala, D.S.; Patil, S.M.; Kunda, N.K. Design of Experiment (DoE) Approach for Developing Inhalable PLGA Microparticles Loaded with Clofazimine for Tuberculosis Treatment. Pharmaceuticals 2024, 17, 754. https://doi.org/10.3390/ph17060754
Rongala DS, Patil SM, Kunda NK. Design of Experiment (DoE) Approach for Developing Inhalable PLGA Microparticles Loaded with Clofazimine for Tuberculosis Treatment. Pharmaceuticals. 2024; 17(6):754. https://doi.org/10.3390/ph17060754
Chicago/Turabian StyleRongala, Druva Sarika, Suyash M. Patil, and Nitesh K. Kunda. 2024. "Design of Experiment (DoE) Approach for Developing Inhalable PLGA Microparticles Loaded with Clofazimine for Tuberculosis Treatment" Pharmaceuticals 17, no. 6: 754. https://doi.org/10.3390/ph17060754
APA StyleRongala, D. S., Patil, S. M., & Kunda, N. K. (2024). Design of Experiment (DoE) Approach for Developing Inhalable PLGA Microparticles Loaded with Clofazimine for Tuberculosis Treatment. Pharmaceuticals, 17(6), 754. https://doi.org/10.3390/ph17060754









