Emerging Roles of Natural Compounds in Osteoporosis: Regulation, Molecular Mechanisms and Bone Regeneration
Abstract
:1. Introduction
2. Osteogenesis and Osteoclastogenesis Modulation
2.1. Promoting Osteoblast Differentiation
2.2. Stimulation of Bone Matrix Synthesis
2.3. Anti-Apoptotic Effects on Osteoblasts
2.4. Inhibition of Osteoclast Formation
2.5. Attenuation of Osteoclast Activity
2.6. Regulation of Osteoclast Survival
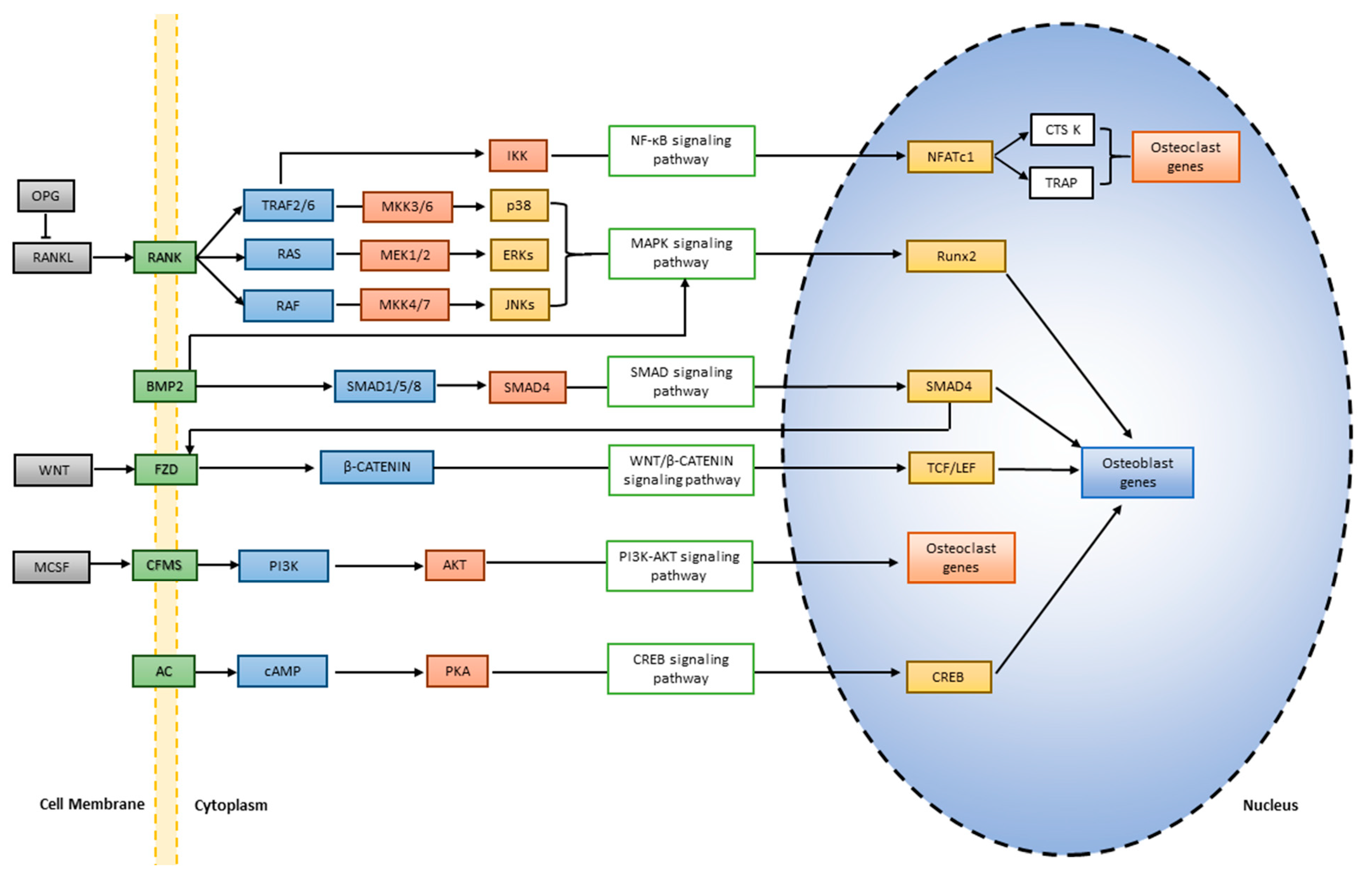
3. Signaling Pathways in Bone Remodeling
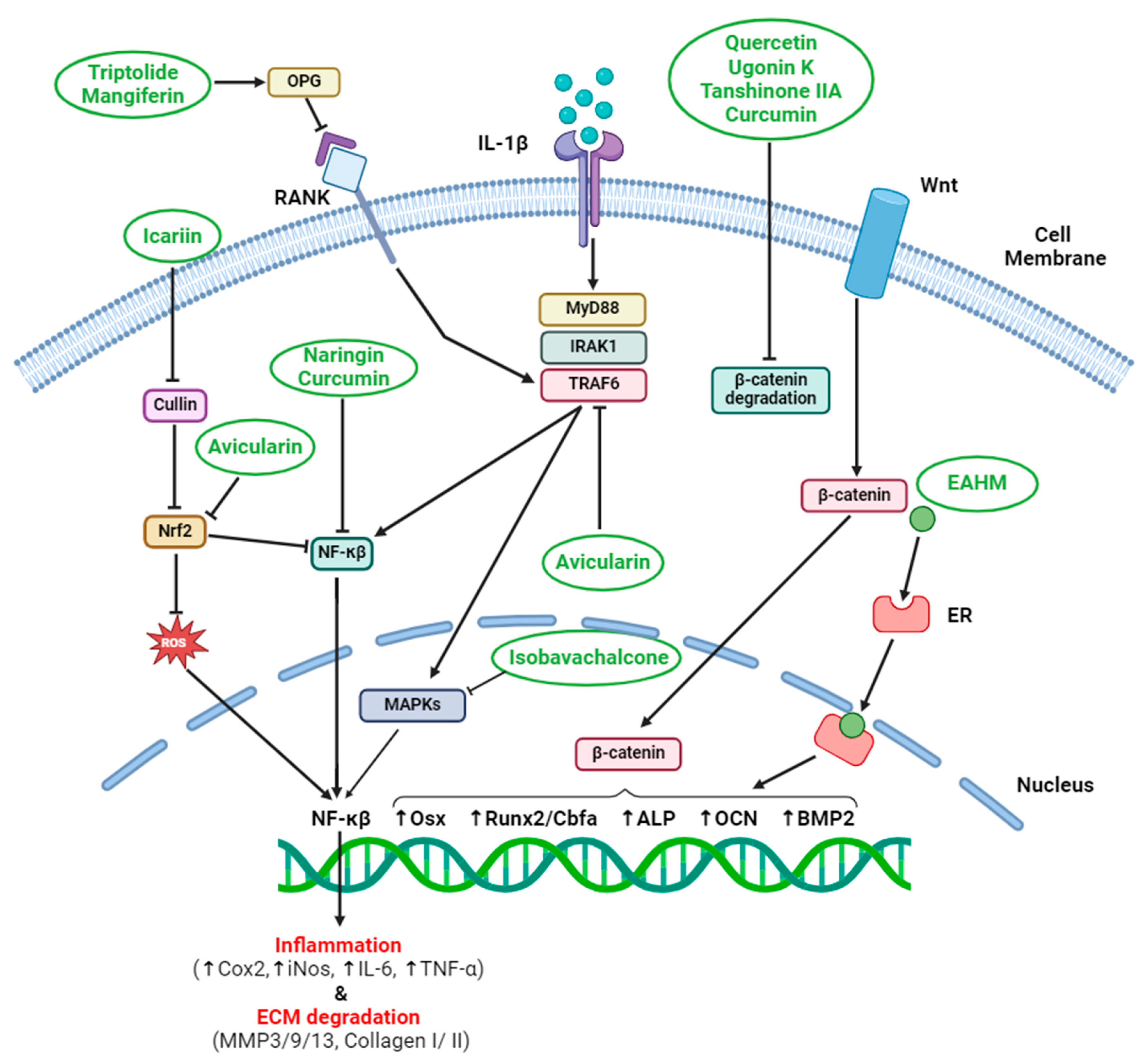
3.1. Wnt/β-Catenin Pathway (Bone Formation)
3.2. Bone Morphogenetic Proteins (BMP) Signaling Pathway (Bone Growth Factors)
3.3. MAPK Pathways (Diverse Ensemble for Balanced Remodeling)
3.4. RANKL/OPG System (Osteoclast Control)
3.5. cAMP Pathway (Bone Formation)
4. Anti-inflammatory Effects on Bone Microenvironment
4.1. Suppression of NF-κB Activation
4.2. Downregulation of Cox2 and Prostaglandins
4.3. Modulation of Macrophage Polarization
4.4. Reduction of Reactive Oxygen Species (ROS)
4.5. Interplay with Immune Cells
4.6. Herbal Formulas with Anti-inflammatory Properties
4.7. Regulation of Bone Turnover Markers
5. Epigenetic Modifications and EAHM-Induced Bone Regeneration
5.1. Epigenetic Memory and Cell Fate
5.2. Trans-Differentiation via Epigenetic Modification
5.3. Epigenomic Regulation for Bone Regeneration
5.4. Clinical Implications and Challenges
6. Pharmacokinetics and EAHM Compound Delivery to Bone Tissue
6.1. Pharmacokinetics
6.2. Challenges in Bone Tissue Delivery
6.3. Absorption and Bioavailability
6.4. Local vs. Systemic Administration
6.5. Combining EAHM with Biomaterials
7. Clinical Translation and Challenges
7.1. Proving Efficacy and Safety in Humans
7.2. Personalizing EAHM
7.3. Standardization of EAHM Formulation
7.4. Assessing Potential Risks and Side Effects
7.5. Gaining Regulatory Approval
7.6. Placebo Effects and Bias
7.7. Ethical Concerns
7.8. Making EAHM a Viable Option
7.9. Monitoring Long-Term Effects
8. Future Perspective and Concluding Remarks
8.1. Personalized Pathways
8.2. Combinatorial Approaches
8.3. Advanced Biomaterials and Tissue Engineering
8.4. Gene Therapy and Epigenetic Modulation
8.5. Clinical Trials and Evidence-Based Practice
8.6. Education and Integration
Funding
Conflicts of Interest
Correction Statement
References
- Kim, J.H.; Kim, N. Bone Cell Communication Factors Provide a New Therapeutic Strategy for Osteoporosis. Chonnam Med. J. 2020, 56, 94–98. [Google Scholar] [CrossRef] [PubMed]
- Manolagas, S.C. Birth and Death of Bone Cells: Basic Regulatory Mechanisms and Implications for the Pathogenesis and Treatment of Osteoporosis. Endocr. Rev. 2000, 21, 115–137. [Google Scholar] [PubMed]
- Hadjidakis, D.J.; Androulakis, I.I. Bone Remodeling. Ann. N. Y. Acad. Sci. 2006, 1092, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Hannah, S.S.; McFadden, S.; McNeilly, A.; McClean, C. “Take My Bone Away?” Hypoxia and Bone: A Narrative Review. J. Cell. Physiol. 2021, 236, 721–740. [Google Scholar] [CrossRef] [PubMed]
- Owen, M. Lineage of Osteogenic Cells and Their Relationship to the Stromal System. In Bone and Mineral Research; ScienceOpen, Inc.: Lexington, MA, USA, 1985; Volume 3. [Google Scholar]
- Suda, T.; Takahashi, N.; Martin, T.J. Modulation of Osteoclast Differentiation. Endocr. Rev. 1992, 13, 66–80. [Google Scholar] [CrossRef] [PubMed]
- Zou, M.L.; Chen, Z.H.; Teng, Y.Y.; Liu, S.Y.; Jia, Y.; Zhang, K.W.; Sun, Z.L.; Wu, J.J.; Yuan, Z.D.; Feng, Y.; et al. The Smad Dependent TGF-β and BMP Signaling Pathway in Bone Remodeling and Therapies. Front. Mol. Biosci. 2021, 8, 593310. [Google Scholar] [CrossRef] [PubMed]
- Arya, P.N.; Saranya, I.; Selvamurugan, N. Crosstalk between Wnt and Bone Morphogenetic Protein Signaling during Osteogenic Differentiation. World J. Stem Cells 2024, 16, 102–113. [Google Scholar] [CrossRef]
- Greenblatt, M.B.; Shim, J.H.; Bok, S.; Kim, J.M. The Extracellular Signal-Regulated Kinase Mitogen-Activated Protein Kinase Pathway in Osteoblasts. J. Bone Metab. 2022, 29, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Miron, R.J.; Zhang, Y.F. Osteoinduction: A Review of Old Concepts with New Standards. J. Dent. Res. 2012, 91, 736–744. [Google Scholar] [CrossRef]
- Zhu, S.; Ehnert, S.; Rouß, M.; Häussling, V.; Aspera-Werz, R.H.; Chen, T.; Nussler, A.K. From the Clinical Problem to the Basic Research—Co-Culture Models of Osteoblasts and Osteoclasts. Int. J. Mol. Sci. 2018, 19, 2284. [Google Scholar] [CrossRef]
- Hinoi, E.; Fujimori, S.; Wang, L.; Hojo, H.; Uno, K.; Yoneda, Y. Nrf2 Negatively Regulates Osteoblast Differentiation via Interfering with Runx2-Dependent Transcriptional Activation. J. Biol. Chem. 2006, 281, 18015–18024. [Google Scholar] [CrossRef] [PubMed]
- Ducy, P.; Zhang, R.; Geoffroy, V.; Ridall, A.L.; Karsenty, G. Osf2/Cbfa1: A Transcriptional Activator of Osteoblast Differentiation. Cell 1997, 89, 747–754. [Google Scholar] [CrossRef] [PubMed]
- Ren, B.X.; Ji, Y.; Tang, J.C.; Sun, D.P.; Hui, X.; Yang, D.Q.; Zhu, X.L. Effect of Tanshinone IIA Intrathecal Injections on Pain and Spinal Inflammation in Mice with Bone Tumors. Genet. Mol. Res. 2015, 14, 2133–2138. [Google Scholar] [CrossRef] [PubMed]
- Tong, Y.; Xu, W.; Han, H.; Chen, Y.; Yang, J.; Qiao, H.; Hong, D.; Wu, Y.; Zhou, C. Tanshinone IIA Increases Recruitment of Bone Marrow Mesenchymal Stem Cells to Infarct Region via Up-Regulating Stromal Cell-Derived Factor-1/CXC Chemokine Receptor 4 Axis in a Myocardial Ischemia Model. Phytomedicine 2011, 18, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Cheon, Y.H.; Kwak, S.C.; Baek, J.M.; Yoon, K.H.; Lee, M.S.; Oh, J. Emodin Regulates Bone Remodeling by Inhibiting Osteoclastogenesis and Stimulating Osteoblast Formation. J. Bone Miner. Res. 2014, 29, 1541–1553. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.H.; Huang, Y.L.; Liao, J.F.; Chiou, W.F. Ugonin K Promotes Osteoblastic Differentiation and Mineralization by Activation of P38 MAPK- and ERK-Mediated Expression of Runx2 and Osterix. Eur. J. Pharmacol. 2011, 668, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Wang, Y.; Jia, Y.; Xu, J.; Chai, Y. Catalpol Promotes the Osteogenic Differentiation of Bone Marrow Mesenchymal Stem Cells via the Wnt/β-Catenin Pathway. Stem Cell Res. Ther. 2019, 10, 37. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Jin, X.; Shen, H.; Chen, X.; Chen, J.; Xu, B.; Xu, J. Icariin Attenuates Thioacetamide-Induced Bone Loss via the RANKL-P38/ERK-NFAT Signaling Pathway. Mol. Med. Rep. 2022, 25, 126. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Huang, Y.; Zhao, J.; Yang, H.; Kuai, F. Oridonin Promotes Osteogenesis through Wnt/β-Catenin Pathway and Inhibits RANKL-Induced Osteoclastogenesis in Vitro. Life Sci. 2020, 262, 118563. [Google Scholar] [CrossRef]
- Huong, L.T.; Gal, M.; Kim, O.; Tran, P.T.; Nhiem, N.X.; Van Kiem, P.; Van Minh, C.; Dang, N.H.; Lee, J.H. 23-Hydroxyursolic Acid from Viburnum Lutescens Inhibits Osteoclast Differentiation in Vitro and Lipopolysaccharide-Induced Bone Loss in Vivo by Suppressing c-Fos and NF-ΚB Signalling. Int. Immunopharmacol. 2022, 111, 109038. [Google Scholar] [CrossRef]
- Luo, D.; Ren, H.; Zhang, H.; Zhang, P.; Huang, Z.; Xian, H.; Lian, K.; Lin, D. The Protective Effects of Triptolide on Age-Related Bone Loss in Old Male Rats. Biomed. Pharmacother. 2018, 98, 280–285. [Google Scholar] [CrossRef]
- Tian, H.; Jiang, T.; Yang, K.; Ning, R.; Wang, T.; Zhou, Q.; Qian, N.; Huang, P.; Guo, L.; Jiang, M.; et al. α-Asarone Attenuates Osteoclastogenesis and Prevents Against Oestrogen-Deficiency Induced Osteoporosis. Front. Pharmacol. 2022, 13, 780590. [Google Scholar] [CrossRef]
- Jin, H.; Jiang, N.; Xu, W.; Zhang, Z.; Yang, Y.; Zhang, J.; Xu, H. Effect of Flavonoids from Rhizoma Drynariae on Osteoporosis Rats and Osteocytes. Biomed. Pharmacother. 2022, 153, 113379. [Google Scholar] [CrossRef]
- Jiang, Y.; Luo, W.; Wang, B.; Wang, X.; Gong, P.; Xiong, Y. Resveratrol Promotes Osteogenesis via Activating SIRT1/FoxO1 Pathway in Osteoporosis Mice. Life Sci. 2020, 246, 117422. [Google Scholar] [CrossRef] [PubMed]
- Saravanan, S.; Hairul Islam, V.I.; Thirugnanasambantham, K.; Pazhanivel, N.; Raghuraman, N.; Gabriel Paulraj, M.; Ignacimuthu, S. Swertiamarin Ameliorates Inflammation and Osteoclastogenesis Intermediates in IL-1β Induced Rat Fibroblast-like Synoviocytes. Inflamm. Res. 2014, 63, 451–462. [Google Scholar] [CrossRef] [PubMed]
- Yin, W.; Liu, S.; Dong, M.; Liu, Q.; Shi, C.; Bai, H.; Wang, Q.; Yang, X.; Niu, W.; Wang, L. A New NLRP3 Inflammasome Inhibitor, Dioscin, Promotes Osteogenesis. Small 2020, 16, e1905977. [Google Scholar] [CrossRef]
- Lu, L.; Wang, Z.; Zhang, H.; Liu, T.; Fang, H. Drynaria Fortunei Improves Lipid Profiles of Elderly Patients with Postmenopausal Osteoporosis via Regulation of Notch1-NLRP3 Inflammasome-Mediated Inflammation. Gynecol. Endocrinol. 2022, 38, 176–180. [Google Scholar] [CrossRef] [PubMed]
- Xi, Y.; Jiang, T.; Yu, J.; Xue, M.; Xu, N.; Wen, J.; Wang, W.; He, H.; Ye, X. Preliminary Studies on the Anti-Osteoporosis Activity of Baohuoside I. Biomed. Pharmacother. 2019, 115, 108850. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Feng, P.; Mo, G.; Li, D.; Li, Y.; Mo, L.; Yang, Z.; Liang, D. Icariin Influences Adipogenic Differentiation of Stem Cells Affected by Osteoblast-Osteoclast Co-Culture and Clinical Research Adipogenic. Biomed. Pharmacother. 2017, 88, 436–442. [Google Scholar] [CrossRef]
- Li, L.; Qu, Y.; Jin, X.; Guo, X.Q.; Wang, Y.; Qi, L.; Yang, J.; Zhang, P.; Li, L.Z. Protective Effect of Salidroside against Bone Loss via Hypoxia-Inducible Factor-1α Pathway-Induced Angiogenesis. Sci. Rep. 2016, 6, 32131. [Google Scholar] [CrossRef]
- Ding, L.Z.; Teng, X.; Zhang, Z.B.; Zheng, C.J.; Chen, S.H. Mangiferin Inhibits Apoptosis and Oxidative Stress via BMP2/Smad-1 Signaling in Dexamethasone-Induced MC3T3-E1 Cells. Int. J. Mol. Med. 2018, 41, 2517–2526. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.J.; Zhang, N.F.; Mao, G.X.; He, X.B.; Zhan, Y.C.; Deng, H.B.; Song, D.Q.; Li, D.D.; Li, Z.R.; Si, S.Y.; et al. Salidroside Stimulates Osteoblast Differentiation through BMP Signaling Pathway. Food Chem. Toxicol. 2013, 62, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Xi, H.R.; Ma, H.P.; Yang, F.F.; Gao, Y.H.; Zhou, J.; Wang, Y.Y.; Li, W.Y.; Xian, C.J.; Chen, K.M. Total Flavonoid Extract of Epimedium Herb Increases the Peak Bone Mass of Young Rats Involving Enhanced Activation of the AC10/CAMP/PKA/CREB Pathway. J. Ethnopharmacol. 2018, 223, 76–87. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zeng, G.F.; Zong, S.H.; Wu, P.P.; He, J.C.; Wu, Y.L.; Yan, F.N.; Qin, Z.X.; Huang, J.H. Molecular Mechanism of Polygonatum Sibiricum Polysaccharide in the Prevention and Treatment of Postmenopausal Osteoporosis. Chin. J. Tissue Eng. Res. 2018, 22, 493–498. [Google Scholar] [CrossRef]
- Jeong, J.C.; Lee, J.W.; Yoon, C.H.; Kim, H.M.; Kim, C.H. Drynariae Rhizoma Promotes Osteoblast Differentiation and Mineralization in MC3T3-E1 Cells through Regulation of Bone Morphogenetic Protein-2, Alkaline Phosphatase, Type I Collagen and Collagenase-1. Toxicol. In Vitro 2004, 18, 829–834. [Google Scholar] [CrossRef] [PubMed]
- Gong, W.; Liu, M.; Zhang, Q.; Zhang, Q.; Wang, Y.; Zhao, Q.; Xiang, L.; Zheng, C.; Zhang, Q.; Qin, L. Orcinol Glucoside Improves Senile Osteoporosis through Attenuating Oxidative Stress and Autophagy of Osteoclast via Activating Nrf2/Keap1 and MTOR Signaling Pathway. Oxid. Med. Cell. Longev. 2022, 2022, 5410377. [Google Scholar] [CrossRef]
- Liu, M.; Ding, H.; Wang, H.; Wang, M.; Wu, X.; Gan, L.; Cheng, L.; Li, X. Moringa Oleifera Leaf Extracts Protect BMSC Osteogenic Induction Following Peroxidative Damage by Activating the PI3K/Akt/Foxo1 Pathway. J. Orthop. Surg. Res. 2021, 16, 150. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Song, D.; Lin, X.; Peng, H.; Su, Y.; Liang, J.; Hai, N.; Zhao, J.; Liu, Q. Corylifol A Protects against Ovariectomized-Induced Bone Loss and Attenuates RANKL-Induced Osteoclastogenesis via ROS Reduction, ERK Inhibition, and NFATc1 Activation. Free Radic. Biol. Med. 2023, 196, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.M. Protective Effect of Quercitrin against Hydrogen Peroxide-Induced Dysfunction in Osteoblastic MC3T3-E1 Cells. Exp. Toxicol. Pathol. 2012, 64, 211–216. [Google Scholar] [CrossRef]
- Nie, Z.; Deng, S.; Zhang, L.; Chen, S.; Lu, Q.; Peng, H. Crocin Protects against Dexamethasone-Induced Osteoblast Apoptosis by Inhibiting the ROS/Ca2+-Mediated Mitochondrial Pathway. Mol. Med. Rep. 2019, 20, 401–408. [Google Scholar] [CrossRef]
- Huang, Q.; Gao, B.; Wang, L.; Zhang, H.Y.; Li, X.J.; Shi, J.; Wang, Z.; Zhang, J.K.; Yang, L.; Luo, Z.J.; et al. Ophiopogonin D: A New Herbal Agent against Osteoporosis. Bone 2015, 74, 18–28. [Google Scholar] [CrossRef]
- He, X.; Andersson, G.; Lindgren, U.; Li, Y. Resveratrol Prevents RANKL-Induced Osteoclast Differentiation of Murine Osteoclast Progenitor RAW 264.7 Cells through Inhibition of ROS Production. Biochem. Biophys. Res. Commun. 2010, 401, 356–362. [Google Scholar] [CrossRef]
- Zhang, J.K.; Yang, L.; Meng, G.L.; Fan, J.; Chen, J.Z.; He, Q.Z.; Chen, S.; Fan, J.Z.; Luo, Z.J.; Liu, J. Protective Effect of Tetrahydroxystilbene Glucoside against Hydrogen Peroxide-Induced Dysfunction and Oxidative Stress in Osteoblastic MC3T3-E1 Cells. Eur. J. Pharmacol. 2012, 689, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Dong, B.; Yao, J.; Ou, G.; Li, M.; Fang, Q. To Explore the Molecular Mechanism of Kidney-Tonifying and Blood-Activating Method in the Prevention and Treatment of Postmenopausal Osteoporosis Based on CAMP-PKA-CREB Signaling Pathway. Osteoarthr. Cartil. 2019, 27, S236–S237. [Google Scholar] [CrossRef]
- Chen, M.; Cui, Y.; Li, H.; Luan, J.; Zhou, X.; Han, J. Icariin Promotes the Osteogenic Action of BMP2 by Activating the CAMP Signaling Pathway. Molecules 2019, 24, 3875. [Google Scholar] [CrossRef]
- Lee, H.W.; Suh, J.H.; Kim, H.-N.; Kim, A.Y.; Park, S.Y.; Shin, C.S.; Choi, J.-Y.; Kim, J.B. Berberine Promotes Osteoblast Differentiation by Runx2 Activation with P38 MAPK. J. Bone Miner. Res. 2008, 23, 1227–1237. [Google Scholar] [CrossRef] [PubMed]
- Boschetto, F.; Honma, T.; Adachi, T.; Kanamura, N.; Zhu, W.; Yamamoto, T.; Marin, E.; Pezzotti, G. Development and Evaluation of Osteogenic PMMA Bone Cement Composite Incorporating Curcumin for Bone Repairing. Mater. Today Chem. 2023, 27, 101307. [Google Scholar] [CrossRef]
- Lee, D.W.; Kim, K.M.; Park, S.; An, S.H.; Lim, Y.J.; Jang, W.G. Eucalyptol Induces Osteoblast Differentiation through ERK Phosphorylation in Vitro and in Vivo. J. Mol. Med. 2023, 101, 1083–1095. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Ye, C.; Sun, S.; Li, R.; Shi, X.; Wang, S.; Zeng, X.; Kuang, N.; Liu, Y.; Shi, Q.; et al. Curcumin Attenuates Collagen-Induced Rat Arthritis via Anti-Inflammatory and Apoptotic Effects. Int. Immunopharmacol. 2019, 72, 292–300. [Google Scholar] [CrossRef]
- Wu, J.B.; Fong, Y.C.; Tsai, H.Y.; Chen, Y.F.; Tsuzuki, M.; Tang, C.H. Naringin-Induced Bone Morphogenetic Protein-2 Expression via PI3K, Akt, c-Fos/c-Jun and AP-1 Pathway in Osteoblasts. Eur. J. Pharmacol. 2008, 588, 333–341. [Google Scholar] [CrossRef]
- Yu, K.E.; Alder, K.D.; Morris, M.T.; Munger, A.M.; Lee, I.; Cahill, S.V.; Kwon, H.K.; Back, J.H.; Lee, F.Y. Re-Appraising the Potential of Naringin for Natural, Novel Orthopedic Biotherapies. Ther. Adv. Musculoskelet. Dis. 2020, 12, 1759720X20966135. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Ji, Q.; Hu, W.; Zhang, Z.; Hu, F.; Cao, S.; Wang, Q.; Hao, Y.; Gao, M.; Zhang, X. Isobavachalcone Prevents Osteoporosis by Suppressing Activation of ERK and NF-ΚB Pathways and M1 Polarization of Macrophages. Int. Immunopharmacol. 2021, 94, 107370. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Sheng, D.; Shi, J.; Xiao, L.; Wang, Z.; Yin, Z.; Zhuang, Q.; Chen, S.; Li, Y.; Gu, Y.; et al. Avicularin Alleviates Osteoporosis-Induced Implant Loosening by Attenuating Macrophage M1 Polarization via Its Inhibitory Effect on the Activation of NF-ΚB. Biomed. Pharmacother. 2023, 158, 114113. [Google Scholar] [CrossRef] [PubMed]
- Cheng, X.; Alborzinia, H.; Merz, K.H.; Steinbeisser, H.; Mrowka, R.; Scholl, C.; Kitanovic, I.; Eisenbrand, G.; Wölfl, S. Indirubin Derivatives Modulate TGFβ/BMP Signaling at Different Levels and Trigger Ubiquitin-Mediated Depletion of Nonactivated R-Smads. Chem. Biol. 2012, 19, 1423–1436. [Google Scholar] [CrossRef]
- Thaler, R.; Maurizi, A.; Roschger, P.; Sturmlechner, I.; Khani, F.; Spitzer, S.; Rumpler, M.; Zwerina, J.; Karlic, H.; Dudakovic, A.; et al. Anabolic and Antiresorptive Modulation of Bone Homeostasis by the Epigenetic Modulator Sulforaphane, a Naturally Occurring Isothiocyanate. J. Biol. Chem. 2016, 291, 6754–6771. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Wang, M.; Zhuo, T.; Li, Y.; Lin, W.; Ding, L.; Zhang, M.; Zhou, C.; Zhang, J.; Li, G.; et al. Hydroxysafflor Yellow A Promotes Osteogenesis and Bone Development via Epigenetically Regulating β-Catenin and Prevents Ovariectomy-Induced Bone Loss. Int. J. Biochem. Cell Biol. 2021, 137, 106033. [Google Scholar] [CrossRef]
- Zhang, Q.; Liu, L.; Lin, W.; Yin, S.; Duan, A.; Liu, Z.; Cao, W. Rhein Reverses Klotho Repression via Promoter Demethylation and Protects against Kidney and Bone Injuries in Mice with Chronic Kidney Disease. Kidney Int. 2017, 91, 144–156. [Google Scholar] [CrossRef] [PubMed]
- Mahady, G.B.; Raut, N.; Lawal, T.O.; Patel, S. Epigenetic Regulation of Osteoblastogenesis by Blackcurrant Fruit Extracts in Vitro and in Vivo. FASEB J. 2019, 33, 471.14. [Google Scholar] [CrossRef]
- Shakibaei, M.; Buhrmann, C.; Mobasheri, A. Resveratrol-Mediated SIRT-1 Interactions with P300 Modulate Receptor Activator of NF-ΚB Ligand (RANKL) Activation of NF-ΚB Signaling and Inhibit Osteoclastogenesis in Bone-Derived Cells. J. Biol. Chem. 2011, 286, 11492–11505. [Google Scholar] [CrossRef]
- Jing, Z.; Wang, C.; Yang, Q.; Wei, X.; Jin, Y.; Meng, Q.; Liu, Q.; Liu, Z.; Ma, X.; Liu, K.; et al. Luteolin Attenuates Glucocorticoid-Induced Osteoporosis by Regulating ERK/Lrp-5/GSK-3β Signaling Pathway in Vivo and in Vitro. J. Cell. Physiol. 2019, 234, 4472–4490. [Google Scholar] [CrossRef]
- Weber, G.F.; Zawaideh, S.; Hikita, S.; Kumar, V.A.; Cantor, H.; Ashkar, S. Phosphorylation-Dependent Interaction of Osteopontin with Its Receptors Regulates Macrophage Migration and Activation. J. Leukoc. Biol. 2002, 72, 752–761. [Google Scholar] [CrossRef] [PubMed]
- Zou, Z.-L.; Sun, M.-H.; Yin, W.-F.; Yang, L.; Kong, L. Avicularin Suppresses Cartilage Extracellular Matrix Degradation and Inflammation via TRAF6/MAPK Activation. Phytomedicine 2021, 91, 153657. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Li, J.; Xie, R.; Zeng, L.; Chen, W.; Li, H. Osteoporosis Guidelines on TCM Drug Therapies: A Systematic Quality Evaluation and Content Analysis. Front. Endocrinol. 2023, 14, 1276631. [Google Scholar] [CrossRef] [PubMed]
- Carracedo, A.; Ma, L.; Teruya-Feldstein, J.; Rojo, F.; Salmena, L.; Alimonti, A.; Egia, A.; Sasaki, A.T.; Thomas, G.; Kozma, S.C.; et al. Inhibition of MTORC1 Leads to MAPK Pathway Activation through a PI3K-Dependent Feedback Loop in Human Cancer. J. Clin. Investig. 2008, 118, 3065–3074. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.; Zhao, S.; Chen, Q.; Wu, Y.; Zhang, J.; Li, N. Crocin Inhibits RANKL-Induced Osteoclastogenesis by Regulating JNK and NF-ΚB Signaling Pathways. Mol. Med. Rep. 2018, 17, 7947–7951. [Google Scholar] [CrossRef] [PubMed]
- Algandaby, M.M. Crocin Attenuates Metabolic Syndrome-Induced Osteoporosis in Rats. J. Food Biochem. 2019, 43, e12895. [Google Scholar] [CrossRef] [PubMed]
- Jeong, J.C.; Lee, J.W.; Yoon, C.H.; Lee, Y.C.; Chung, K.H.; Kim, M.G.; Kim, C.H. Stimulative Effects of Drynariae Rhizoma Extracts on the Proliferation and Differentiation of Osteoblastic MC3T3-E1 Cells. J. Ethnopharmacol. 2005, 96, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Izawa, A.; Ishihara, Y.; Mizutani, H.; Kobayashi, S.; Goto, H.; Okabe, E.; Takeda, H.; Ozawa, Y.; Kamiya, Y.; Sugita, Y.; et al. Inflammatory Bone Loss in Experimental Periodontitis Induced by Aggregatibacter Actinomycetemcomitans in Interleukin-1 Receptor Antagonist Knockout Mice. Infect. Immun. 2014, 82, 1904–1913. [Google Scholar] [CrossRef] [PubMed]
- Damani, J.J.; De Souza, M.J.; VanEvery, H.L.; Strock, N.C.A.; Rogers, C.J. The Role of Prunes in Modulating Inflammatory Pathways to Improve Bone Health in Postmenopausal Women. Adv. Nutr. 2022, 13, 1476–1492. [Google Scholar] [CrossRef]
- Tabatabaei-Malazy, O.; Salari, P.; Khashayar, P.; Larijani, B. New Horizons in Treatment of Osteoporosis. DARU J. Pharm. Sci. 2017, 25, 2. [Google Scholar] [CrossRef]
- Heo, D.N.; Ko, W.K.; Moon, H.J.; Kim, H.J.; Lee, S.J.; Lee, J.B.; Bae, M.S.; Yi, J.K.; Hwang, Y.S.; Bang, J.B.; et al. Inhibition of Osteoclast Differentiation by Gold Nanoparticles Functionalized with Cyclodextrin Curcumin Complexes. ACS Nano 2014, 8, 12049–12062. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Zhu, B.; Li, S.; Zhai, Y.; Yang, Y.; Bai, Z.; Zeng, Y.; Li, D. Curcumin Protects Bone Biomechanical Properties and Microarchitecture in Type 2 Diabetic Rats with Osteoporosis via the TGFβ/Smad2/3 Pathway. Exp. Ther. Med. 2020, 20, 2200–2208. [Google Scholar] [CrossRef] [PubMed]
- Woo, J.T.; Nakagawa, H.; Notoya, M.; Yonezawa, T.; Udagawa, N.; Lee, I.S.; Ohnishi, M.; Hagiwara, H.; Nagai, K. Quercetin Suppresses Bone Resorption by Inhibiting the Differentiation and Activation of Osteoclasts. Biol. Pharm. Bull. 2004, 27, 504–509. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Lv, J.; Sun, X.; Ma, J.; Xing, G.; Wang, Y.; Sun, L.; Wang, J.; Li, F.; Li, Y.; et al. Naringin Ameliorates Bone Loss Induced by Sciatic Neurectomy and Increases Semaphorin 3A Expression in Denervated Bone. Sci. Rep. 2016, 6, 24562. [Google Scholar] [CrossRef] [PubMed]
- Shi, W.; Gao, Y.; Wang, Y.; Zhou, J.; Wei, Z.; Ma, X.; Ma, H.; Xian, C.J.; Wang, J.; Chen, K. The Flavonol Glycoside Icariin Promotes Bone Formation in Growing Rats by Activating the CAMP Signaling Pathway in Primary Cilia of Osteoblasts. J. Biol. Chem. 2017, 292, 20883–20896. [Google Scholar] [CrossRef] [PubMed]
- Moriishi, T.; Maruyama, Z.; Fukuyama, R.; Ito, M.; Miyazaki, T.; Kitaura, H.; Ohnishi, H.; Furuichi, T.; Kawai, Y.; Masuyama, R.; et al. Overexpression of Bcl2 in Osteoblasts Inhibits Osteoblast Differentiation and Induces Osteocyte Apoptosis. PLoS ONE 2011, 6, e27487. [Google Scholar] [CrossRef] [PubMed]
- Córdoba, A.; Manzanaro-Moreno, N.; Colom, C.; Rønold, H.J.; Lyngstadaas, S.P.; Monjo, M.; Ramis, J.M. Quercitrin Nanocoated Implant Surfaces Reduce Osteoclast Activity in Vitro and in Vivo. Int. J. Mol. Sci. 2018, 19, 3319. [Google Scholar] [CrossRef] [PubMed]
- Nusse, R.; Clevers, H. Wnt/β-Catenin Signaling, Disease, and Emerging Therapeutic Modalities. Cell 2017, 169, 985–999. [Google Scholar] [CrossRef]
- Niwano, Y.; Kohzaki, H.; Shirato, M.; Shishido, S.; Nakamura, K. Anti-Osteoporotic Mechanisms of Polyphenols Elucidated Based on In Vivo Studies Using Ovariectomized Animals. Antioxidants 2022, 11, 217. [Google Scholar] [CrossRef]
- Elseweidy, M.M.; El-Swefy, S.E.; Shaheen, M.A.; Baraka, N.M.; Hammad, S.K. Effect of Resveratrol and Mesenchymal Stem Cell Monotherapy and Combined Treatment in Management of Osteoporosis in Ovariectomized Rats: Role of SIRT1/FOXO3a and Wnt/β-Catenin Pathways. Arch. Biochem. Biophys. 2021, 703, 108856. [Google Scholar] [CrossRef]
- Awasthi, H.; Mani, D.; Singh, D.; Gupta, A. The Underlying Pathophysiology and Therapeutic Approaches for Osteoporosis. Med. Res. Rev. 2018, 38, 2024–2057. [Google Scholar] [CrossRef]
- Yamaguchi, M.; Vikulina, T.; Arbiser, J.L.; Weitzmann, M.N. Suppression of NF-κB Activation By Gentian Violet Promotes Osteoblastogenesis and Suppresses Osteoclastogenesis. Curr. Mol. Med. 2014, 14, 783–792. [Google Scholar] [CrossRef]
- Feng, J.; Liu, S.; Ma, S.; Zhao, J.; Zhang, W.; Qi, W.; Cao, P.; Wang, Z.; Lei, W. Protective Effects of Resveratrol on Postmenopausal Osteoporosis: Regulation of SIRT1-NF-ΚB Signaling Pathway. Acta Biochim. Biophys. Sin. 2014, 46, 1024–1033. [Google Scholar] [CrossRef]
- Tzavlaki, K.; Moustakas, A. TGF-β Signaling. Biomolecules 2020, 10, 487. [Google Scholar] [CrossRef]
- Yousefzadeh, G.; Larijani, B.; Mohammadirad, A.; Heshmat, R.; Dehghan, G.; Rahimi, R.; Abdollahi, M. Determination of Oxidative Stress Status and Concentration of TGF-β1 in the Blood and Saliva of Osteoporotic Subjects. Ann. N. Y. Acad. Sci. 2006, 1091, 142–150. [Google Scholar] [CrossRef]
- Poudel, S.; Martins, G.; Cancela, L.M.; Gavaia, P. Resveratrol-Mediated Reversal of Doxorubicin-Induced Osteoclast Differentiation Alleviates Oxidative Stress via FoxM1 Expression. Bone Rep. 2022, 16, 101396. [Google Scholar] [CrossRef]
- Si, Y.; Li, Y.; Gu, K.; Yin, H.; Ma, Y. Icariin Ameliorates Osteoporosis in Ovariectomized Rats by Targeting Cullin 3/Nrf2/OH Pathway for Osteoclast Inhibition. Biomed. Pharmacother. 2024, 173, 116422. [Google Scholar] [CrossRef]
- Zhao, H.; Zhao, N.; Zheng, P.; Xu, X.; Liu, M.; Luo, D.; Xu, H.; Ju, D. Prevention and Treatment of Osteoporosis Using Chinese Medicinal Plants: Special Emphasis on Mechanisms of Immune Modulation. J. Immunol. Res. 2018, 2018, 6345857. [Google Scholar] [CrossRef]
- Zhou, C.; Shen, S.; Zhang, M.; Luo, H.; Zhang, Y.; Wu, C.; Zeng, L.; Ruan, H. Mechanisms of Action and Synergetic Formulas of Plant-Based Natural Compounds from Traditional Chinese Medicine for Managing Osteoporosis: A Literature Review. Front. Med. 2023, 10, 1235081. [Google Scholar] [CrossRef]
- Lee, J.H.; Wei, Y.J.; Zhou, Z.Y.; Hou, Y.M.; Wang, C.L.; Wang, L.B.; Wu, H.J.; Zhang, Y.; Dai, W.W. Efficacy of the Herbal Pair, Radix Achyranthis Bidentatae and Eucommiae Cortex, in Preventing Glucocorticoid-Induced Osteoporosis in the Zebrafish Model. J. Integr. Med. 2022, 20, 83–90. [Google Scholar] [CrossRef]
- Cheng, B.R.; Wu, R.Y.; Gao, Q.Y.; Jiang, K.X.; Li, S.S.; Qi, S.H.; Yuan, M.Y.; Liu, J.P. Chinese Proprietary Medicine Xianling Gubao Capsule for Osteoporosis: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Front. Endocrinol. 2022, 13, 870277. [Google Scholar] [CrossRef]
- Liu, T.; Yao, M.; Zhao, Y.; Zhao, S.; Rui, C.; Yang, F. Chinese Medicine Gushukang Capsule for Treating Primary Osteoporosis: A Systematic Review and Meta-Analysis. J. Orthop. Surg. Res. 2023, 18, 845. [Google Scholar] [CrossRef]
- Shen, Y.; Wang, N.; Zhang, Q.; Liu, Y.; Wu, Q.; He, Y.; Wang, Y.; Wang, X.; Zhao, Q.; Zhang, Q.; et al. Jin-Tian-Ge Ameliorates Ovariectomy-Induced Bone Loss in Rats and Modulates Osteoblastogenesis and Osteoclastogenesis in Vitro. Chin. Med. 2022, 17, 78. [Google Scholar] [CrossRef]
- Jia, Y.; Sun, J.; Zhao, Y.; Tang, K.; Zhu, R.; Zhao, W.; Wang, R.; Zhang, Y.; Lin, N.; Chen, W. Chinese Patent Medicine for Osteoporosis: A Systematic Review and Meta-Analysis. Bioengineered 2022, 13, 5581–5597. [Google Scholar] [CrossRef]
- Balcerzak, M.; Hamade, E.; Zhang, L.; Pikula, S.; Azzar, G.; Radisson, J.; Bandorowicz-Pikula, J.; Buchet, R. The Roles of Annexins and Alkaline Phosphatase in Mineralization Process Circled White Star. Acta Biochim. Pol. 2003, 50, 1019–1038. [Google Scholar] [CrossRef]
- Wennberg, C.; Hessle, L.; Lundberg, P.; Mauro, S.; Narisawa, S.; Lerner, U.H.; Millán, J.L. Functional Characterization of Osteoblasts and Osteoclasts from Alkaline Phosphatase Knockout Mice. J. Bone Miner. Res. 2000, 15, 1879–1888. [Google Scholar] [CrossRef]
- Saito, M.; Marumo, K. Collagen Cross-Links as a Determinant of Bone Quality: A Possible Explanation for Bone Fragility in Aging, Osteoporosis, and Diabetes Mellitus. Osteoporos. Int. 2010, 21, 195–214. [Google Scholar] [CrossRef]
- Boskey, A. Bone Mineral Crystal Size. Osteoporos. Int. 2003, 14, 16–21. [Google Scholar] [CrossRef]
- Behera, J.; Ison, J.; Rai, H.; Tyagi, N. Allyl Sulfide Promotes Osteoblast Differentiation and Bone Density via Reducing Mitochondrial DNA Release Mediated Kdm6b/H3K27me3 Epigenetic Mechanism. Biochem. Biophys. Res. Commun. 2021, 543, 87–94. [Google Scholar] [CrossRef]
- Raimondi, L.; De Luca, A.; Giavaresi, G.; Barone, A.; Tagliaferri, P.; Tassone, P.; Amodio, N. Impact of Natural Dietary Agents on Multiple Myeloma Prevention and Treatment: Molecular Insights and Potential for Clinical Translation. Curr. Med. Chem. 2018, 27, 187–215. [Google Scholar] [CrossRef]
- Fernandes, G.F.S.; Silva, G.D.B.; Pavan, A.R.; Chiba, D.E.; Chin, C.M.; Dos Santos, J.L. Epigenetic Regulatory Mechanisms Induced by Resveratrol. Nutrients 2017, 9, 1201. [Google Scholar] [CrossRef]
- Shakibaei, M.; Shayan, P.; Busch, F.; Aldinger, C.; Buhrmann, C.; Lueders, C.; Mobasheri, A. Resveratrol Mediated Modulation of Sirt-1/Runx2 Promotes Osteogenic Differentiation of Mesenchymal Stem Cells: Potential Role of Runx2 Deacetylation. PLoS ONE 2012, 7, e35712. [Google Scholar] [CrossRef]
- Jiang, M.; Wang, T.; Yan, X.; Liu, Z.; Yan, Y.; Yang, K.; Qi, J.; Zhou, H.; Qian, N.; Zhou, Q.; et al. A Novel Rhein Derivative Modulates Bone Formation and Resorption and Ameliorates Estrogen-Dependent Bone Loss. J. Bone Miner. Res. 2019, 34, 361–374. [Google Scholar] [CrossRef]
- Deng, Z.; Chen, J.; Lin, B.; Li, J.; Wang, H.; Wang, D.; Pang, L.; Zeng, X.; Wang, H.; Zhang, Y. A Novel 3D Printed Bioactive Scaffolds with Enhanced Osteogenic Inspired by Ancient Chinese Medicine HYSA for Bone Repair. Exp. Cell Res. 2020, 394, 112139. [Google Scholar] [CrossRef]
- Lai, Y.; Cao, H.; Wang, X.; Chen, S.; Zhang, M.; Wang, N.; Yao, Z.; Dai, Y.; Xie, X.; Zhang, P.; et al. Porous Composite Scaffold Incorporating Osteogenic Phytomolecule Icariin for Promoting Skeletal Regeneration in Challenging Osteonecrotic Bone in Rabbits. Biomaterials 2018, 153, 1–13. [Google Scholar] [CrossRef]
- Fan, H.; Hui, J.; Duan, Z.; Fan, D.; Mi, Y.; Deng, J.; Li, H. Novel Scaffolds Fabricated Using Oleuropein for Bone Tissue Engineering. Biomed. Res. Int. 2014, 2014, 652432. [Google Scholar] [CrossRef]
- Xin, Y.; Dai, Y.Y.; Zhang, X.W.; Yang, H.X.; Hou, A.L.; Yang, K.; Li, Z.Y.; Li, B.; Liu, H. A Brief Discussion on Evidence-Based Clinical Research of Traditional Chinese Medicine. Ann. Palliat. Med. 2021, 10, 12937–12944. [Google Scholar] [CrossRef]
- Huang, C.Y.; Cheng, C.J.; Chiou, W.F.; Chang, W.C.; Kang, Y.N.; Lee, M.H. Efficacy and Safety of Duhuo Jisheng Decoction Add-on Bisphosphonate Medications in Patients with Osteoporosis: A Meta-Analysis of Randomized Controlled Trials. J. Ethnopharmacol. 2022, 283, 114732. [Google Scholar] [CrossRef]
- Fung, F.Y.; Linn, Y.C. Developing Traditional Chinese Medicine in the Era of Evidence-Based Medicine: Current Evidences and Challenges. Evid.-Based Complement. Altern. Med. 2015, 2015, 425037. [Google Scholar] [CrossRef]
- Zuo, T.T.; Jin, H.Y.; Zhang, L.; Liu, Y.L.; Nie, J.; Chen, B.L.; Fang, C.F.; Xue, J.; Bi, X.Y.; Zhou, L.; et al. Innovative Health Risk Assessment of Heavy Metals in Chinese Herbal Medicines Based on Extensive Data. Pharmacol. Res. 2020, 159, 104987. [Google Scholar] [CrossRef]
- Li, W.; Ye, B.; Huang, Z.; Zhou, H.; Feng, J.; Chen, Q.; Huang, H.; Meng, S.; Qie, F.; Shi, X. Effects of Kidney Tonic Herbs for Primary Osteoporosis: A Systematic Review and Meta-Analysis. Medicine 2023, 102, e35061. [Google Scholar] [CrossRef] [PubMed]
- You, L.; Liang, K.; An, R.; Wang, X. The Path towards FDA Approval: A Challenging Journey for Traditional Chinese Medicine. Pharmacol. Res. 2022, 182, 106314. [Google Scholar] [CrossRef] [PubMed]
| Target | EAHM | Ingredient | Mechanism | Pathways | Study | Outcome | Ref. |
|---|---|---|---|---|---|---|---|
| RANKL | Rehmanniae glutinosa | Catalpol | Increases ALP, Ca and MSC differentiation to osteoblast | Activated Wnt/β-catenin signaling | Pre-clinical | Promote osteogenesis | [18] |
| Rheum palmatum | Emodin | Increase in Runx2, OCN and ALP for osteoblast differentiation | Activated MAPK (ERK, JNK, p38) signaling pathway, suppress NFATC1/c-Fos signaling | Pre-clinical | Promote osteogensis, inhibit osteoclastogenesis | [16] | |
| Epimedium brevicornu | Icariin (ICA) | Thioacetamide induced bone loss | Suppress RANKL-p38/ERK-NFAT signaling | Pre-clinical | Inhibit osteoclast differentiation | [19] | |
| Rabdosia rubens | Oridonin (ORI) | Increase ALP, Ca2+ nodules, inhibit TRAP, NFATc1/c-Fos | Activated Wnt/β-catenin signaling | Pre-clinical | Promote osteogenesis, inhibit osteoclastogenesis | [20] | |
| Viburnum lutescens | Hydroxyurosolic acid (HUA) | Inhibits osteoclast differentiation | Suppress c-Fos and NF-κB signaling | Pre-clinical | Inhibit osteoclast differentiation | [21] | |
| Tripterygium wilfordii | Triptolide | Increased OPG, decreased RANKL | Activated OPG/RANKL signaling | Pre-clinical | Inhibit osteoclastogenesis | [22] | |
| Acorus tatarinowii | α-asarone (ASA) | Inhibit osteoclastogenesis | AKT, p38 and NF-κB, followed by NFATc1/c-fos signaling pathway | Pre-clinical | Attenuate osteoclastogenesis | [23] | |
| TRAP | Drynariae fortunei | Naringenin (NAR) | Increased ALP, OCN, Runx2, parathyroid receptor1 (PTH1R), MSC proliferation | Activated Wnt/β-catenin signaling | Pre-clinical | Influence osteocyte/osteoblast/osteoclast activity | [24] |
| Fruits | Resveratrol (RSV) | Increased ALP, Runx2, SOD, PINP SIRT1, Osx decreased TRAP | Activated SIRT1/FOXO1 signaling | Pre-clinical | Promote osteogenesis | [25] | |
| MMP9 | Enicosttema axillare | Swertiamarin | Inhibit cytokines, Cox2, MMPs and RANKL | Activated MAPK (ERK, JNK, p38) signaling | Pre-clinical | Amoliate inflammation, attenuate osteoclastogenesis | [26] |
| NLRP3 | Drynaria fortunei | Dioscin | Increased ALP, Runx2, OCN | Suppress NLRP3 | Pre-clinical | Promote osteogenesis | [27] |
| Extract | Suppress NLRP3 cytokines and Notch1 by increasing SIRT1 | Suppress Notch1 independent of SIRT1 | Pre-clinical | Amoliate inflammation, improve lipid profile in OP | [28] | ||
| Immune cells and Cytokines | Epimedium brevicornu | Baohuoside 1 | Increased ALP, MSC differentiation | Inhibit cytokines and adipogenesis | Pre-clinical | Promote BMSC differentiation | [29] |
| PPAR-γ | Epimedium brevicornu | Icariin (ICA) | Increased ALP, TGF-β1 and OPG, decreased RANK expression and NF-kβ | PPAR-γ inhibition | Pre-clinical | Promote and/or inhibit differentiation of stem cells based on osteoblast-osteoclast co-cultering | [30] |
| VEGF | Rhodiola rosea | Salidroside (SAL) | Increased VEGF | Activated HIF-1α/VEGF signaling | Pre-clinical | Promotes osteogenesis and angiogenesis | [31] |
| BMP2 | Mangifera indica | Mangiferin | Increased OPG | Activated BMP (Smad1/5/8, Smad4) signaling | Pre-clinical | Inhibit MC3T3 cells apoptosis | [32] |
| Rhodiola rosea | Salidroside | Increased phosphorylation of BMP2, BMP7, Smad 1/5/8 and ERK1/2 | Activated BMP signaling | Pre-clinical | Stimulate osteoblast differentiation | [33] | |
| Epimedium brevicornu | Extract | Enhanced expression of Runx2, Osx and BMP2 | Activated AC10/cAMP/PKA/CREB | Pre-clinical | Increases maximum bone density during growth | [34] | |
| Osx | Helminthostachys zeylanica | Ugonin K | Increased Osx and runx2 | Activated MAPK (ERK, JNK, p38) signaling | Pre-clinical | Stimulate osteoblast differentiation | [17] |
| Cathepsin K | Polygonatum sibiricum | Polysaccharide (PSP) | Increased ALP, runx2, Col1A1, OCN, supresss ACP5 and cathepsin K | Suppress cathepsin K | Pre-clinical | Promotes osteogenesis, inhibit osteoclastogenesis | [35] |
| Drynariae fortunei | Extract | Increased ALP, BMP2 | Suppress resorption induced by Catk | Pre-clinical | Promote osteoblast differentiation | [36] | |
| Oxidative stress (OS) | Curculigo orchioides Gaertn | Orcinol glucoside (OG) | Decrease oxidative stress and autophagy of osteoclast | Activated Nrf2/Keap1 and mTOR signaling | Pre-clinical | Promote bone health by reducing oxidative stress | [37] |
| Moringa oleifer | Extract | Osteoblast survival | PI3K, AKT, Fox1 signaling | Pre-clinical | Promote osteoblast differentiation | [38] | |
| Cullen corylifolium | Corylifol A | Increased antioxidant enzymes; CAT, HMOX1, NQO1 | Suppress ROS and osteoclast differentiation | Pre-clinical | Inhibit osteoclastogenesis | [39] | |
| Eurya cilliata | Quercetin (QUE) | Increased ALP, Ca2+ and collagen | Activated MAPK (ERK, JNK, p38) signaling | Pre-clinical | Enhance osteoblast activity | [40] | |
| ROS | Crocus sativus | Crocin (CRO) | Increased Bcl2, bax and cytochrome C | Suppress ROS/Ca2 mitochrondrial signaling | Pre-clinical | Protect osteoblast from ROS | [41] |
| Radix ophiopogon japonicus | Ophiopogonin D (OP-D) | Decreased ROS, CTX1 and TRAP | FOXO3a-β-catenin signaling | Pre-clinical | Promotes osteogenesis/inhibit osteoclastogenesis | [42] | |
| Grapes | Resveratrol (RSV) | Decreased ROS and RANKL | Activated Wnt/β-catenin signaling | Pre-clinical | Inhibit RANKL-induced osteoclastogenesis | [43] | |
| Polygonum multiflorum | Tetrahydroxystilbene-2-O-β-D-glucoside (TSG) | Increased ALP, OCN while decreased RANKL, ROS, malondialdehyde (MDA) | Activated JNK, PI3K/AKT and ROS-NO signaling | Pre-clinical | Protect osteoblast | [44] | |
| Epimedium brevicornu | Icariin (ICA) | Increased BMP2 and cAMP | cAMP/PKA/CREB signaling | Pre-clinical | Promote osteogenesis | [45,46] | |
| adipocyte differentiation | Coptischinensis franch | Berberine (BBR) | Increased OCN, Runx2, Cox2 | Activated MAPK (ERK, JNK, p38) signaling, suppress adipocyte differentiation | Pre-clinical | Promote osteoblast differentiation | [47] |
| Inflammation | Curcuma longa | Curcumin (CUR) | Decreased cytokines, promote bone healing | Bone composite mixing PMMA | Pre-clinical | Promote bone healing | [48] |
| Eucalyptus globules | Eucalyptol (EU) | Increased ERK phosphorylation | Activated MAPK (ERK, JNK, p38) signaling | Pre-clinical | Promote osteoblast differentiation | [49] | |
| NF-κB | Curcuma longa | Curcumin (CUR) | Inhibit TNF-α and IL-17 | suppress NF-κB signaling | Pre-clinical | Anti-inflammatory and anti-apoptosis effect | [50] |
| Salvia miltiorrhiza | Tanshinone IIA | Inhibit expression of TRAF6 and NFTAc1 | suppress NF-κB signaling | Pre-clinical | Reduce inflammation and pain in bone tumor | [14] | |
| Citrus fruits | Naringin (NAG) | Increased BMP2 | Activated PI3K, AKT, c-Fos/c-Jun and AP1 signaling | Pre-clinical | Promote osteogenesis/inhibit osteoclastogenesis | [51,52] | |
| Macrophage M1 polarization | Psoralea corylifolia | Isobavachalcone (ISO) | Decreased inflammatory cytokines and macrophage M1 polarization | Suppress ERK, NF-κB signaling | Pre-clinical | Reduce osteoclast activity and bone resorption | [53] |
| Polygonum aviculare | Avicularin (AL) | Decreased inflammatory cytokines and macrophage M1 polarization | Suppress NF-κB signaling | Pre-clinical | Reduce inflammation and M1 macrophage activity | [54] | |
| Smad degradation | Drynariae fortunei | Indirubin | Inhibit Smad | BMP signaling | Pre-clinical | Regulate bone formation | [55] |
| Epigenetics and autophagy | Sprouts of cruciferous vegetables | Sulforaphane | Prevent osteoblast apoptosis and promote its differentiation | Activated gene expression by TET1/2 dependent DNA | Pre-clinical | Promote osteogenesis, inhibit osteoclastogenesis via epigenetic mechanism | [56] |
| Carthamus tinctorius | Hydroxysafflor yellow A (HSYA) | Regulate β-catenin and promote MSC differentiation to osteoblast | Histone demethylation by KDM7A | Pre-clinical | Promote osteogenesis by epigenetically regulating β-catenin | [57] | |
| Rheum palmatum | Rhein and its derivatives | Estrogen dependent bone loss and formation | Decreased Dnmt1/dnm3a activity and hydroxymethylation of Klotho promoter | Pre-clinical | Reverse DNA methylation that activate Klotho gene and promote bone health | [58] | |
| Ribes nigrum | Anthocyanins | Enhanced proliferation of osteoblasts | Altered expression of Bcl2, Bax, HDAC1/3 by upregulated SIRT1/3 and PGC-1α | Pre-clinical | Promote osteogenesis | [59] | |
| Grapes | Resveratrol (RSV) | Induce SIRT1 deacetylase | Inhibit NF-κB Signaling | Pre-clinical | Inhibit osteoclastogenesis by influencing P300 interating with RANKL | [60] | |
| Reseda odorata | Luteolin | Bcl2, Bax, caspase 3/9 | Regulate ERK/LRP-5/GSK-3β signaling | Pre-clinical | Enhance osteogenesis, inhibit osteoclastogenesis | [61] |
| EAHM | Patent | URLs |
|---|---|---|
| Extract of Epimedii and Salvia miltiorrhiza | CN101023982A | https://patents.google.com/patent/CN102218089B/en, accessed on 22 July 2024 |
| Extract of Drynariae | WO2002053164 | http://engpat.kipris.or.kr/engpat/biblioa.do?method=biblioFrame, accessed on 22 July 2024 |
| Extract of Epimedii alongwith other active components | CN117949573A | https://patents.google.com/patent/CN117949573A/en?oq=CN117949573A, accessed on 22 July 2024 |
| Extracts of Epimedii, Drynariae and Achyranthis Bidentatae | CN103251671B | https://patents.google.com/patent/CN103251671B/en?oq=CN103251671B, accessed on 22 July 2024 |
| Extracts of Epimedii, Polygonum multiflorum | CN105616630A | https://patents.google.com/patent/CN105616630A/en?oq=CN105616630A, accessed on 22 July 2024 |
| Extracts of Epimedii, Polygonum multiflorum and Drynariae | CN105456711A | https://patents.google.com/patent/CN105456711A/en?oq=CN105456711A, accessed on 22 July 2024 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ilyas, S.; Lee, J.; Lee, D. Emerging Roles of Natural Compounds in Osteoporosis: Regulation, Molecular Mechanisms and Bone Regeneration. Pharmaceuticals 2024, 17, 984. https://doi.org/10.3390/ph17080984
Ilyas S, Lee J, Lee D. Emerging Roles of Natural Compounds in Osteoporosis: Regulation, Molecular Mechanisms and Bone Regeneration. Pharmaceuticals. 2024; 17(8):984. https://doi.org/10.3390/ph17080984
Chicago/Turabian StyleIlyas, Sidra, Juni Lee, and Donghun Lee. 2024. "Emerging Roles of Natural Compounds in Osteoporosis: Regulation, Molecular Mechanisms and Bone Regeneration" Pharmaceuticals 17, no. 8: 984. https://doi.org/10.3390/ph17080984
APA StyleIlyas, S., Lee, J., & Lee, D. (2024). Emerging Roles of Natural Compounds in Osteoporosis: Regulation, Molecular Mechanisms and Bone Regeneration. Pharmaceuticals, 17(8), 984. https://doi.org/10.3390/ph17080984








