A Predictive Model of Pandemic Disaster Fear Caused by Coronavirus (COVID-19): Implications for Decision-Makers
Abstract
:1. Introduction
Literature Review
- (a)
- disaster fear caused by the coronavirus disease has not been studied at an appropriate level; there is still a lack of reliable epidemiological data (COVID-19) on the psychological consequences of illness,
- (b)
- insufficient examination of the influences of various factors on people’s disaster fear caused by the coronavirus disease, which is needed to improve disaster risk communication strategies, the quality of psycho-social support, etc.
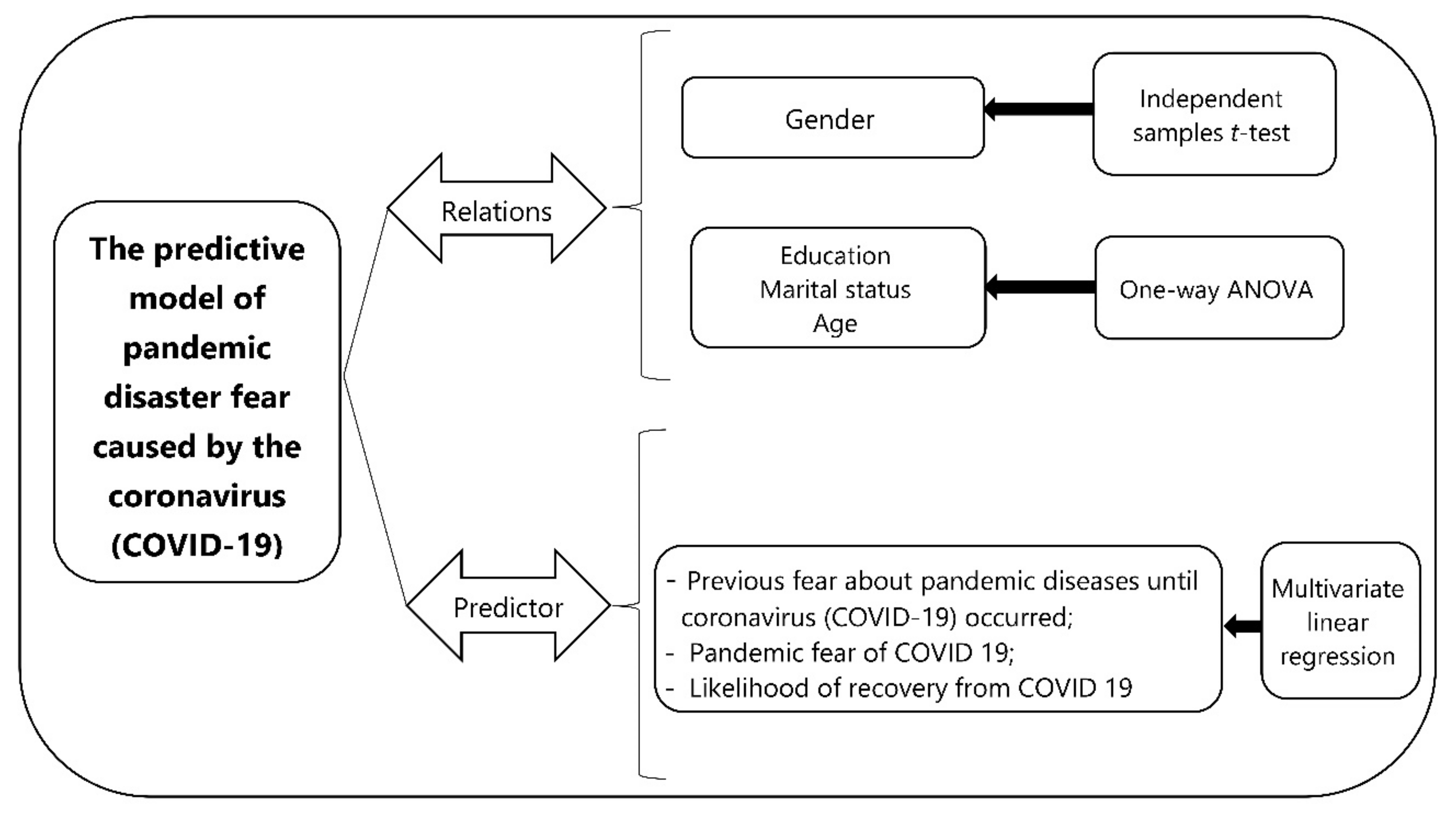
2. Materials and Methods
2.1. Study Area
2.2. Socioeconomic and Demographic Characteristics
2.3. Questionnaire Design
2.4. Analyses
3. Results
- The predictors of fear scores related to fear caused by coronavirus disease (COVID-19);
- Descriptive statistics and the relations between the variables and fear caused by coronavirus disease (COVID-19);
- Gender perspectives about fear caused by coronavirus disease (COVID-19).
3.1. The Predictors of Fear Scores Related to Fear Caused by the Coronavirus Disease (COVID-19)
3.2. Descriptive Statistics: The Relations between the Variables and Fear Caused by COVID-19
3.3. Gender Perspective about Fear Caused by COVID-19
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A
- 1.
- Country: ……………………….
- 2.
- Gender: (a) Male (b) Female (c) …………….
- 3.
- Age: ……………………….
- 4.
- Marital status:(a) single (b) married (c) divorced (d) widow
- 5.
- Education level:(a) Primary school (b) Secondary school (c) High school (d) Undergraduate (e) Master/doctorate
- 6.
- The number of children:(a) any (b) 1 (c) 2–3 (d) 4+
- 7.
- What do you think about your coronavirus knowledge (please mark with X):(a) very poor (b) poor (c) moderate (d) good (e) excellent
- 8.
- Please mark from 1 to 5 for the level of your fear.
Never Rarely Sometimes Often Always 1 2 3 4 5 - Have you ever fear about pandemic diseases until coronavirus disease (COVID-19) occurred?
- Do you have any fear about having coronavirus disease (COVID-19) disease?
- If you have coronavirus disease illness, what do you think about a recovery yourself?
- 9.
- What is the reason of fear caused by coronavirus disease (COVID-19)? Please mark from 1 to 5 for the level of your fear itemized (mark with X).
Strongly
DisagreeDisagree Neither Agree nor Disagree Agree Strongly Agree 1 2 3 4 5 I fear for my own life and health. I fear for the life and health of my wife/husband. I fear for the life and health of my children. I fear for the life and health of my grandmother/father. I fear for the life and health of my pets. I fear for losing goods in the house. I fear for losing my wealth (money, house, etc). I fear for losing my job. I fear the lack of food supplies. I fear the lack of medicine and pills. I fear from a post-pandemic period trauma. I fear that I have not got enough money for recovery. I fear losing my friends. I fear for not attend to (continue) my school. I fear for I cannot receive treatment in hospital. Other ………………………… (please write) - 10.
- Which sources are more reliable to get information about coronavirus disease (COVID-19)? (mark with x).
Strongly
DisagreeDisagree Neither Agree nor Disagree Agree Strongly Agree 1 2 3 4 5 - (a)
- TV programs
- (b)
- Government (official)
- (c)
- Military or emergency services
- (d)
- Social media (Facebook, twitter, etc)
- (e)
- My friends or colleagues
- (f)
- Radio
- (g)
- Newspaper
- (h)
- Academic journals or magazine
- (i)
- Scientists
Other ……………………………………………. (please write)
References
- Orrù, G.; Bertelloni, D.; Diolaiuti, F.; Conversano, C.; Ciacchini, R.; Gemignani, A. A psychometric examination of the Coronavirus Anxiety Scale and the Fear of Coronavirus Disease 2019 Scale in the Italian population. Front. Psychol. 2021, 12, 2358. [Google Scholar] [CrossRef]
- Wibowo, Y.S.; Utami, R.K.; Nadia, Y.; Nizeyumukiza, E.; Setiawati, F.A. The fear of coronavirus disease scale: Exploratory and confirmatory factor analysis. Konselor 2020, 9, 75–80. [Google Scholar] [CrossRef]
- Şimşir, Z.; Koç, H.; Seki, T.; Griffiths, M.D. The relationship between fear of COVID-19 and mental health problems: A meta-analysis. Death Stud. 2021, 45, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Cvetković, V.M. Risk Perception of Building Fires in Belgrade. Int. J. Disaster Risk Manag. 2019, 1, 81–91. [Google Scholar] [CrossRef] [Green Version]
- Yıldırım, M.; Arslan, G.; Alkahtani, A.M. Do fear of COVID-19 and religious coping predict depression, anxiety, and stress among the Arab population during health crisis? Death Stud. 2021, 45, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Aknin, L.; De Neve, J.E.; Dunn, E.; Fancourt, D.; Goldberg, E.; Helliwell, J.F.; Lyubomirsky, S. Mental health during the first year of the COVID-19 pandemic: A review and recommendations for moving forward. Perspect. Psychol. Sci. 2021, in press. [Google Scholar]
- World Health Organization (WHO). Mental Health and Psychosocial Considerations during the COVID-19 Outbreak. 2020. Available online: https://www.who.int/docs/default-source/coronavirusdiseasee/mental-health-considerations.pdf (accessed on 28 September 2021).
- Khan, M.I.; Saleem, H.A.R.; Anwar, M.F.; Chang, Y.C. Novel Coronavirus and Emerging Mental Health Issues—A Timely Analysis of Potential Consequences and Legal Policies Perspective. Fudan J. Humanit. Soc. Sci. 2021, 14, 87–105. [Google Scholar] [CrossRef]
- Zepinic, V. COVID-19: An Urgency to Address Mental Health Consequences. Psychology 2021, 12, 735–748. [Google Scholar] [CrossRef]
- Valenzano, A.; Scarinci, A.; Monda, V.; Sessa, F.; Messina, A.; Monda, M.; Messina, G. The social brain and emotional contagion: COVID-19 effects. Medicina 2020, 56, 640. [Google Scholar] [CrossRef]
- Nami, M.; Gadad, B.S.; Chong, L.; Ghumman, U.; Misra, A.; Gadad, S.S.; Rao, K.S. The interrelation of neurological and psychological symptoms of COVID-19: Risks and remedies. J. Clin. Med. 2020, 9, 2624. [Google Scholar] [CrossRef]
- Feng, P.; Chen, Z.; Becker, B.; Liu, X.; Zhou, F.; He, Q.; Feng, T. Predisposing Variations in Fear-Related Brain Networks Prospectively Predict Fearful Feelings during the 2019 Coronavirus (COVID-19) Pandemic. Cereb. Cortex 2021, 00, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Parchani, A.; Vidhya, K.; Panda, P.; Rawat, V.S.; Bahurupi, Y.A.; Kalita, D.; Kumar, H. Fear, Anxiety, Stress, and Depression of Novel Coronavirus Disease (COVID-19) Pandemic among Patients and Their Healthcare Workers. 2021. Available online: https://ssrn.com/abstract=3855659 (accessed on 25 September 2021). [CrossRef]
- Pasquel-Lopez, C.; Valerio-Urena, G. Emotional contagion in social networks: The case of COVID-19 on Facebook. Texto Livre-Ling. E Tecnol. 2021, 14, 1–14. [Google Scholar]
- Wheaton, M.G.; Prikhidko, A.; Messner, G.R. Is fear of COVID-19 contagious? The effects of emotion contagion and social media use on anxiety in response to the coronavirus disease pandemic. Front. Psychol. 2021, 11, 3594. [Google Scholar] [CrossRef]
- Crocamo, C.; Viviani, M.; Famiglini, L.; Bartoli, F.; Pasi, G.; Carrà, G. Surveilling COVID-19 emotional contagion on twitter by sentiment analysis. Eur. Psychiatry 2021, 64, e17. [Google Scholar] [CrossRef]
- Liu, J.C.J.; Tong, E.M.W. The relation between official WhatsApp-distributed COVID-19 news exposure and psychological symptoms: Cross-sectional survey study. J. Med. Internet Res. 2020, 22, e22142. [Google Scholar] [CrossRef]
- Steinert, S. Corona and value change. The role of social media and emotional contagion. Ethics Inf. Technol. 2021, 23, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Su, Z.; McDonnell, D.; Wen, J.; Kozak, M.; Abbas, J.; Šegalo, S.; Cai, Y. Mental health consequences of COVID-19 media coverage: The need for effective crisis communication practices. Glob. Health 2021, 17, 1–8. [Google Scholar] [CrossRef]
- Li, N.; Li, S.; Fan, L. Risk factors of psychological disorders after the COVID-19 outbreak: The mediating role of social support and emotional intelligence. J. Adolesc. Health 2021, in press. [Google Scholar] [CrossRef]
- Fitzpatrick, K.M.; Harris, C.; Drawve, G. Fear of COVID-19 and the mental health consequences in America. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, S17. [Google Scholar] [CrossRef] [PubMed]
- Ekimova, V.I.; Rozenova, M.I.; Litvinova, A.V.; Koteneva, A.V. The Fear Traumatization: Psychological Consequences of COVID-19 Pandemic. J. Mod. Foreign Psychol. 2021, 10, 27–38. [Google Scholar] [CrossRef]
- Chow, K.M.; Law, B.M.H.; Ng, M.S.N.; Chan, D.N.S.; So, W.K.W.; Wong, C.L.; Chan, C.W.H. A review of psychological issues among patients and healthcare staff during two major coronavirus disease outbreaks in China: Contributory factors and management strategies. Int. J. Environ. Res. Public Health 2020, 17, 6673. [Google Scholar] [CrossRef]
- González-Sanguino, C.; Ausín, B.; Castellanos, M.A.; Saiz, J.; Muñoz, M. Mental health consequences of the COVID-19 outbreak in Spain. A longitudinal study of the alarm situation and return to the new normality. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 107, 110219. [Google Scholar] [CrossRef]
- Eugênia, J.; Vilar, R. Fear of COVID and trait anxiety: Mediation of resilience in university students. Psicol. Teor. E Prática 2021, 23, 1–16. [Google Scholar]
- Cagnin, A.; Di Lorenzo, R.; Marra, C.; Bonanni, L.; Cupidi, C.; Laganà, V.; Isella, V. Behavioral and psychological effects of coronavirus disease-19 quarantine in patients with dementia. Front. Psychiatry 2020, 11, 916. [Google Scholar] [CrossRef] [PubMed]
- Dai, L.L.; Wang, X.; Jiang, T.C.; Li, P.F.; Wang, Y.; Wu, S.J.; Cheng, Z. Anxiety and depressive symptoms among COVID-19 patients in Jianghan Fangcang Shelter Hospital in Wuhan, China. PLoS ONE 2020, 15, e0238416. [Google Scholar]
- Du, J.; Dong, L.; Wang, T.; Yuan, C.; Fu, R.; Zhang, L.; Qin, J. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen. Hosp. Psychiatry 2020, 67, 144. [Google Scholar] [CrossRef]
- Khanal, P.; Devkota, N.; Dahal, M.; Paudel, K.; Joshi, D. Mental health impacts among health workers during COVID-19 in a low resource setting: A cross-sectional survey from Nepal. Glob. Health 2020, 16, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Miao, J.; Wang, H.; Xu, S.; Sun, W.; Fan, Y.; Wang, W. Psychological impact on women health workers involved in COVID-19 outbreak in Wuhan: A cross-sectional study. J. Neurol. Neurosurg. Psychiatry 2020, 91, 895–897. [Google Scholar] [CrossRef] [PubMed]
- Massicotte, V.; Ivers, H.; Savard, J. COVID-19 pandemic stressors and psychological symptoms in breast cancer patients. Curr. Oncol. 2021, 28, 294–300. [Google Scholar] [CrossRef]
- Oladunjoye, A.; Oladunjoye, O. An evolving problem—Mental health symptoms among health care workers during COVID-19 pandemic. Asian J. Psychiatry 2020, 54, 102257. [Google Scholar] [CrossRef]
- Shi, L.; Lu, Z.A.; Que, J.-Y.; Huang, X.L.; Liu, L.; Ran, M.S.; Sun, Y.K. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw. Open 2020, 3, e2014053. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.R.; Wang, K.; Yin, L.; Zhao, W.F.; Xue, Q.; Peng, M.; Wang, H. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother. Psychosom. 2020, 89, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Schimmenti, A.; Billieux, J.; Starcevic, V. The four horsemen of fear: An integrated model of understanding fear experiences during the COVID-19 pandemic. Clin. Neuropsychiatry 2020, 17, 41–45. [Google Scholar]
- Vos, L.M.W.; Habibović, M.; Nyklíček, I.; Smeets, T.; Mertens, G. Optimism, mindfulness, and resilience as potential protective factors for the mental health consequences of fear of the coronavirus disease. Psychiatry Res. 2021, 300, 113927. [Google Scholar] [CrossRef] [PubMed]
- French, M.T.; Mortensen, K.; Timming, A.R. Psychological Distress and Coronavirus Fears during the Initial Phase of the COVID-19 Pandemic in the United States. J. Ment. Health Policy Econ. 2020, 23, 93–100. [Google Scholar] [PubMed]
- Dahmen, A.; Keller, F.; Kötting, L.; Derksen, C.; Lippke, S. Fear of Coronavirus, Intention to Follow the AHA Rules and Risk Perception Regarding Visits to the Doctor: Cross-sectional Study with Patients suffering from Pre-existing Mental Illness. Gesundheitswesen 2021, 83, 274–281. [Google Scholar]
- Bösselmann, V.; Amatriain-Fernández, S.; Gronwald, T.; Murillo-Rodríguez, E.; Machado, S.; Budde, H. Physical Activity, Boredom and Fear of COVID-19 among Adolescents in Germany. Front. Psychol. 2021, 12, 624206. [Google Scholar] [CrossRef]
- Wright, L.J.; Williams, S.E.; Veldhuijzen van Zanten, J.J. Physical Activity Protects Against the Negative Impact of Coronavirus Fear on Adolescent Mental Health and Well-Being During the COVID-19 Pandemic. Front. Psychol. 2021, 12, 737. [Google Scholar] [CrossRef]
- Satici, B.; Saricali, M.; Satici, S.A.; Griffiths, M.D. Intolerance of uncertainty and mental wellbeing: Serial mediation by rumination and fear of COVID-19. Int. J. Ment. Health Addict. 2020, 1, 1–12. [Google Scholar] [CrossRef]
- Lee, S.A.; Crunk, E.A. Fear and psychopathology during the COVID-19 crisis: Neuroticism, hypochondriasis, reassurance-seeking, and coronaphobia as fear factors. OMEGA J. Death Dying 2020, 1–14. [Google Scholar] [CrossRef]
- Caci, B.; Miceli, S.; Scrima, F.; Cardaci, M. Neuroticism and fear of COVID-19. The interplay between boredom, fantasy engagement, and perceived control over time. Front. Psychol. 2020, 11, 2578. [Google Scholar] [CrossRef] [PubMed]
- Enea, V.; Eisenbeck, N.; Petrescu, T.C.; Carreno, D.F. Perceived impact of quarantine on loneliness, death obsession, and preoccupation with God: Predictors of increased fear of COVID-19. Front. Psychol. 2021, 12, 643977. [Google Scholar] [CrossRef] [PubMed]
- Barua, L.; Zaman, M.S.; Omi, F.R.; Faruque, M. Psychological burden of the COVID-19 pandemic and its associated factors among frontline doctors of Bangladesh: A cross-sectional study. F1000Research 2020, 9, 1304. [Google Scholar] [CrossRef]
- Harper, C.A.; Satchell, L.P.; Fido, D.; Latzman, R.D. Functional fear predicts public health compliance in the COVID-19 pandemic. Int. J. Ment. Health Addict. 2020, 1–14. [Google Scholar] [CrossRef]
- Gold, A.K.; Hoyt, D.L.; Milligan, M.; Hiserodt, M.L.; Samora, J.; Leyro, T.M.; Otto, M.W. The role of fear of COVID-19 in motivation to quit smoking and reductions in cigarette smoking: A preliminary investigation of at-risk cigarette smokers. Cogn. Behav. Ther. 2021, 50, 295–304. [Google Scholar] [CrossRef]
- Yıldırım, M.; Geçer, E.; Akgül, Ö. The impacts of vulnerability, perceived risk, and fear on preventive behaviours against COVID-19. Psychol. Health Med. 2021, 26, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Lippold, J.V.; Laske, J.I.; Hogeterp, S.A.; Duke, É.; Grünhage, T.; Reuter, M. The role of personality, political attitudes and socio-demographic characteristics in explaining individual differences in fear of coronavirus disease: A comparison over time and across countries. Front. Psychol. 2020, 11, 2356. [Google Scholar] [CrossRef]
- Mertens, G.; Duijndam, S.; Lodder, P.; Smeets, T. Pandemic panic? Results of a 6-month longitudinal study on fear of COVID-19. PsyArXiv 2020, 1, 1–40. [Google Scholar] [CrossRef]
- Sadiković, S.; Branovački, B.; Oljača, M.; Mitrović, D.; Pajić, D.; Smederevac, S. Daily monitoring of emotional responses to the coronavirus disease pandemic in Serbia: A citizen science approach. Front. Psychol. 2020, 11, 2133. [Google Scholar] [CrossRef]
- Mertens, G.; Gerritsen, L.; Duijndam, S.; Salemink, E.; Engelhard, I.M. Fear of the coronavirus disease (COVID-19): Predictors in an online study conducted in March 2020. J. Anxiety Disord. 2020, 74, 102258. [Google Scholar] [CrossRef]
- Lin, C.-Y.; Broström, A.; Griffiths, M.D.; Pakpour, A.H. Investigating mediated effects of fear of COVID-19 and COVID-19 misunderstanding in the association between problematic social media use, psychological distress, and insomnia. Internet Interv. 2020, 21, 100345. [Google Scholar] [CrossRef]
- Choompunuch, B.; Suksatan, W.; Sonsroem, J.; Kutawan, S.; In-udom, A. Stress, adversity quotient, and health behaviors of undergraduate students in a Thai university during COVID-19 outbreak. Belitung Nurs. J. 2021, 7, 1–7. [Google Scholar] [CrossRef]
- De Oliveira Araújo, F.J.; de Lima, L.S.A.; Cidade, P.I.M.; Nobre, C.B.; Neto, M.L.R. Impact of SARS-CoV-2 and its reverberation in global higher education and mental health. Psychiatry Res. 2020, 288, 112977. [Google Scholar] [CrossRef]
- Hakami, Z.; Vishwanathaiah, S.; Abuzinadah, S.H.; Alhaddad, A.J.; Bokhari, A.M.; Marghalani, H.Y.A.; Shahin, S.Y. Effects of COVID-19 lockdown on the mental health of dental students: A longitudinal study. J. Dent. Educ. 2021, 1–14. [Google Scholar] [CrossRef]
- Hossain, M.J.; Ahmmed, F.; Rahman, S.M.A.; Sanam, S.; Emran, T.B.; Mitra, S. Impact of online education on fear of academic delay and psychological distress among university students following one year of COVID-19 outbreak in Bangladesh. Heliyon 2021, 7, e07388. [Google Scholar] [CrossRef]
- Lathabhavan, R.; Griffiths, M. First case of student suicide in India due to the COVID-19 education crisis: A brief report and preventive measures. Asian J. Psychiatry 2020, 53, 102202. [Google Scholar] [CrossRef]
- Nola, M.; Guiot, C.; Damiani, S.; Brondino, N.; Milani, R.; Politi, P. Not a matter of quantity: Quality of relationships and personal interests predict university students’ resilience to anxiety during COVID-19. Curr. Psychol. 2021, 1–8. [Google Scholar] [CrossRef]
- Pourghaznein, T.; Salati, S.; Jamali, J.; Rangani, F.; Khazaei, E. Study of behaviors and psychological indicators in Iranian medical students during the COVID-19 pandemic self-quarantine. J. Health Lit. 2021, 6, 61–71. [Google Scholar]
- Sahu, P. Closure of universities due to coronavirus disease 2019 (COVID-19): Impact on education and mental health of students and academic staff. Cureus 2020, 12, e7541. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sánchez-Ballester, C. Mental Health and Educational Trajectories in Students during the Coronavirus Pandemic. Eur. J. Environ. Public Health 2021, 5, em0087. [Google Scholar] [CrossRef]
- Al-Maroof, R.S.; Salloum, S.A.; Hassanien, A.E.; Shaalan, K. Fear from COVID-19 and technology adoption: The impact of Google Meet during Coronavirus pandemic. Interact. Learn. Environ. 2020, 1–16. [Google Scholar] [CrossRef]
- Mahmud, M.S.; Talukder, M.U.; Rahman, S.M. Does ‘Fear of COVID-19′ trigger future career anxiety? An empirical investigation considering depression from COVID-19 as a mediator. Int. J. Soc. Psychiatry 2021, 67, 35. [Google Scholar] [CrossRef]
- Bechard, L.E.; Bergelt, M.; Neudorf, B.; DeSouza, T.C.; Middleton, L.E. Using the Health Belief Model to Understand Age Differences in Perceptions and Responses to the COVID-19 Pandemic. Front. Psychol. 2021, 12, 1216. [Google Scholar] [CrossRef] [PubMed]
- De Vries, M.; Claassen, L.; Te Wierik, M.J.M.; van den Hof, S.; Brabers, A.E.M.; de Jong, J.D.; Timen, A. Dynamic public perceptions of the coronavirus disease crisis, the Netherlands, 2020. Emerg. Infect. Dis. 2021, 27, 1098. [Google Scholar] [CrossRef]
- Muto, H.; Gondo, Y.; Kasuga, A.; Nakagawa, T.; Ishioka, Y.L.; Onoguchi, W.; Hori, N. Associations among anxiety, risk perception, preventive behaviors, and personality in Japanese older adults aged 78 to 99 years during the COVID-19 pandemic. PsyArXiv 2021, 1–20. [Google Scholar] [CrossRef]
- Nino, M.; Harris, C.; Drawve, G.; Fitzpatrick, K.M. Race and ethnicity, gender, and age on perceived threats and fear of COVID-19: Evidence from two national data sources. SSM Popul. Health 2021, 13, 100717. [Google Scholar] [CrossRef]
- Mistry, S.K.; Ali, A.M.; Akther, F.; Yadav, U.N.; Harris, M.F. Exploring fear of COVID-19 and its correlates among older adults in Bangladesh. Glob. Health 2021, 17, 1–9. [Google Scholar] [CrossRef]
- Giordani, R.C.F.; Zanoni da Silva, M.; Muhl, C.; Giolo, S.R. Fear of COVID-19 scale: Assessing fear of the coronavirus disease pandemic in Brazil. J. Health Psychol. 2020, 1–12. [Google Scholar] [CrossRef]
- Bitan, D.T.; Grossman-Giron, A.; Bloch, Y.; Mayer, Y.; Shiffman, N.; Mendlovic, S. Fear of COVID-19 scale: Psychometric characteristics, reliability and validity in the Israeli population. Psychiatry Res. 2020, 289, 113100. [Google Scholar] [CrossRef] [PubMed]
- Mete, B.; Tanir, F.; Kanat, C. The effect of fear of COVID-19 and social isolation on the fragility in the elderly. Türk Geriatr. Derg. 2021, 24, 23–31. [Google Scholar] [CrossRef]
- Majeed, M.M.; Sarwar, H.; Ramzan, Z. The psychology of coronavirus disease fear: Are dentists of pakistan suffering from corona-phobia. J. Pak. Dent. Assoc. 2021, 30, 1–6. [Google Scholar] [CrossRef]
- Dymecka, J.; Gerymski, R.; Machnik-Czerwik, A. Fear of COVID-19 as a buffer in the relationship between perceived stress and life satisfaction in the Polish population at the beginning of the global pandemic. Health Psychol. Rep. 2021, 9, 149–159. [Google Scholar] [CrossRef]
- Satici, B.; Gocet-Tekin, E.; Deniz, M.E.; Satici, S.A. Adaptation of the Fear of COVID-19 Scale: Its association with psychological distress and life satisfaction in Turkey. Int. J. Ment. Health Addict. 2020, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Dymecka, J.; Gerymski, R.; Machnik-Czerwik, A. How does stress affect life satisfaction during the COVID-19 pandemic? Moderated mediation analysis of sense of coherence and fear of coronavirus disease. Psychol. Health Med. 2021, 1–9. [Google Scholar] [CrossRef]
- Labrague, L.J.; de Los Santos, J.A.A. Fear of COVID-19, psychological distress, work satisfaction and turnover intention among frontline nurses. J. Nurs. Manag. 2021, 29, 395–403. [Google Scholar] [CrossRef]
- Cvetković, V.M.; Tanasić, J.; Ocal, A.; Kešetović, Ž.; Nikolić, N.; Dragašević, A. Capacity Development of Local Self-Governments for Disaster Risk Management. Int. J. Environ. Res. Public Health. 2021, 18, 10406. [Google Scholar] [CrossRef] [PubMed]
- Cvetković, V.; Roder, G.O.A.; Tarolli, P.; Dragićević, S. The Role of Gender in Preparedness and Response Behaviors towards Flood Risk in Serbia. Int. J. Environ. Res. Public Health. 2018, 15, 2761. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hunter, W. The Serbian Epidemics of Typhus and Relapsing Fever in 1915: Their Origin, Course, and Preventive Measures Employed for their Arrest (An Etiological and Preventive Study Based on Records of British Military Sanitary Mission to Serbia 1915). Available online: https://journals.sagepub.com/doi/pdf/10.1177/003591572001301502 (accessed on 28 September 2021).
- Ristanović, E. Infectious agents as a security challenge: Experience of typhus, variola and tularemia outbreaks in Serbia. Bezbednost 2015, 57, 5–20. [Google Scholar] [CrossRef]
- Čukić, G.J. Batut, 1915: Enlightened sons, start the meaningful fight against the typhus! Acta Med. Median. 2018, 57, 145–154. [Google Scholar]
- World Health Organization. The Global Eradication of Smallpox: Final Report of the Global Commission for the Certification of Smallpox Eradication; World Health Organization: Geneva, Switzerland, 1979; Available online: https://apps.who.int/iris/handle/10665/39253 (accessed on 28 September 2021).
- Janković, B.; Cvetković, V.M. Public perception of police behaviors in the disaster COVID-19–The case of Serbia. Polic. Int. J. 2020, 43, 979–992. [Google Scholar] [CrossRef]
- Institute of Public Health of Serbia “Dr Milan Jovanovic Batut”. WHO. Available online: https://covid19.rs/ (accessed on 9 December 2021).
- Cvetković, V.; Ristanović, E.; Gačić, J. Citizens attitudes about the emergency situations caused by epidemics in serbia. Iran. J. Public Health 2018, 47, 1213–1214. [Google Scholar]
- Statistical Office of the Republic of Serbia. Municipalities and Regions in the Republic of Serbia. 2017. Available online: http://pod2.stat.gov.rs/ObjavljenePublikacije/G2016/pdf/G20162020.pdf (accessed on 4 November 2021).
- Del Río-Casanova, L.; Sánchez-Martín, M.; García-Dantas, A.; González-Vázquez, A.; Justo, A. Psychological Responses According to Gender during the Early Stage of COVID-19 in Spain. Int. J. Environ. Res. Public Health 2021, 18, 3731. [Google Scholar] [CrossRef]
- Hammarberg, K.; Tran, T.; Kirkman, M.; Fisher, J. Sex and age differences in clinically significant symptoms of depression and anxiety among people in Australia in the first month of COVID-19 restrictions: A national survey. BMJ Open 2020, 10, e042696. [Google Scholar] [CrossRef]
- Horesh, D.; Kapel Lev-Ari, R.; Hasson-Ohayon, I. Risk factors for psychological distress during the COVID-19 pandemic in Israel: Loneliness, age, gender, and health status play an important role. Br. J. Health Psychol. 2020, 25, 925–933. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Miao, Y.; Zeng, X.; Tarimo, C.S.; Wu, C.; Wu, J. Prevalence and factors for anxiety during the coronavirus disease 2019 (COVID-19) epidemic among the teachers in China. J. Affect. Disord. 2020, 277, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Yang, L.; Zhang, C.; Xu, Y.; Cai, L.; Ma, S.; Li, R. Gender differences in mental health problems of healthcare workers during the coronavirus disease 2019 outbreak. J. Psychiatr. Res. 2021, 137, 393–400. [Google Scholar] [CrossRef]
- Tyebkhan, G. Declaration of Helsinki: The Ethical Cornerstone of Human Clinical Research. Indian J. Dermatol. Venereol. Leprol. 2003, 69, 245–247. Available online: https://www.ijdvl.com/text.asp?2003/69/3/245/1013 (accessed on 25 September 2021). [PubMed]
- Kim, T.K. T test as a parametric statistic. Korean J. Anesthesiol. 2015, 68, 540–546. [Google Scholar] [CrossRef] [Green Version]
- Heiberger, R.M.; Neuwirth, E. (Eds.) One-Way ANOVA. In R through Excel; Springer: New York, NY, USA, 2009; pp. 165–191. [Google Scholar]
- Yuan, M.; Ekici, A.; Lu, Z.; Monteiro, R. Dimension reduction and coefficient estimation in multivariate linear regression. J. R. Stat. Soc. Ser. B Stat. Methodol. 2007, 69, 329–346. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S.; Ullman, J.B. Using Multivariate Statistics, 5th ed.; Pearson: Boston, MA, USA, 2007. [Google Scholar]
- Cvetković, V.M.; Öcal, A.; Ivanov, A. Young adults’ fear of disasters: A case study of residents from Turkey, Serbia and Macedonia. Int. J. Disaster Risk Reduct. 2019, 35, 101095. [Google Scholar] [CrossRef]
- Paradise, T.R. Perception of earthquake risk in Agadir, Morocco: A case study from a Muslim community. Glob. Environ. Chang. Part B Environ. Hazards 2005, 6, 167–180. [Google Scholar] [CrossRef]
- Norris, F.H.; Friedman, M.J.; Watson, P.J.; Byrne, C.M.; Diaz, E.; Kaniasty, K. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981–2001. Psychiatry 2002, 65, 207–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baytiyeh, H.; Öcal, A. High school students’ perceptions of earthquake disaster: A comparative study of Lebanon and Turkey. Int. J. Disaster Risk Reduct. 2016, 18, 56–63. [Google Scholar] [CrossRef]
- Ramzan, M.; Ansar, A.; Nadeem, S. Dengue epidemics: Knowledge perhaps is the only key to success. J. Ayub Med. Coll. Abbottabad 2015, 27, 402–406. [Google Scholar]
- Abebe, G.; Deribew, A.; Apers, L.; Woldemichael, K.; Shiffa, J.; Tesfaye, M.; Bezabih, M. Knowledge, health seeking behavior and perceived stigma towards tuberculosis among tuberculosis suspects in a rural community in southwest Ethiopia. PLoS ONE 2010, 5, e13339. [Google Scholar] [CrossRef]
- Barberi, F.; Davis, M.S.; Isaia, R.; Nave, R.; Ricci, T. Volcanic risk perception in the Vesuvius population. J. Volcanol. Geotherm. Res. 2008, 172, 244–258. [Google Scholar] [CrossRef]
- Armas, I. Social vulnerability and seismic risk perception. Case study: The historic center of the Bucharest Municipality/Romania. Nat. Hazards 2008, 47, 397–410. [Google Scholar] [CrossRef]
- Kwok, K.O.; Li, K.K.; Chan, H.H.; Yi, Y.Y.; Tang, A.; Wei, W.I.; Wong, Y.S.J. Community responses during the early phase of the COVID-19 epidemic in Hong Kong: Risk perception, information exposure and preventive measures. Emerg. Infect. Dis. 2020, 26, 1575. [Google Scholar] [CrossRef]
- Collantoni, E.; Saieva, A.M.; Meregalli, V.; Girotto, C.; Carretta, G.; Boemo, D.G.; Nesoti, M.V. Psychological distress, fear of COVID-19, and resilient coping abilities among healthcare workers in a tertiary first-line hospital during the coronavirus disease pandemic. J. Clin. Med. 2021, 10, 1465. [Google Scholar] [CrossRef]
- Doshi, D.; Karunakar, P.; Sukhabogi, J.R.; Prasanna, J.S.; Mahajan, S.V. Assessing coronavirus disease fear in Indian population using the fear of COVID-19 scale. Int. J. Ment. Health Addict. 2020, 19, 1–9. [Google Scholar] [CrossRef]
- Haktanir, A.; Seki, T.; Dilmaç, B. Adaptation and evaluation of Turkish version of the fear of COVID-19 scale. Death Stud. 2020, 1–9. [Google Scholar] [CrossRef]
- Asai, K.; Wakashima, K.; Toda, S.; Koiwa, K. Fear of novel coronavirus disease (COVID-19) among pregnant and infertile women in Japan. J. Affect. Disord. Rep. 2021, 4, 100104. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.A.; Jahid, M.I.K.; Hossain, K.M.A.; Walton, L.M.; Uddin, Z.; Haque, M.O.; Faruqui, R. Knowledge, attitudes, and fear of COVID-19 during the Rapid Rise Period in Bangladesh. PLoS ONE 2020, 15, e0239646. [Google Scholar] [CrossRef]
- Broche-Pérez, Y.; Fernández-Fleites, Z.; Jiménez-Puig, E.; Fernández-Castillo, E.; Rodríguez-Martin, B.C. Gender and fear of COVID-19 in a Cuban population sample. Int. J. Ment. Health Addict. 2020, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Broche-Pérez, Y.; Fernández-Fleites, Z.; Fernández-Castillo, E.; Jiménez-Puig, E.; Vizcaíno-Escobar, A.E.; Ferrer-Lozano, D.M.; Martín-González, R. Anxiety, health self-perception, and worry about the resurgence of COVID-19 predict fear reactions among genders in the Cuban population. Front. Glob. Women’s Health 2021, 2, 14. [Google Scholar] [CrossRef] [PubMed]
- Graham, J.E.; Robles, T.F.; Kiecolt-Glaser, J.K.; Malarkey, W.B.; Bissell, M.G.; Glaser, R. Hostility and pain are related to inflammation in older adults. Brain Behav. Immun. 2006, 20, 389–400. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K.; et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef]
- Birditt, K.S.; Turkelson, A.; Fingerman, K.L.; Polenick, C.A.; Oya, A. Age differences in stress, life changes, and social ties during the COVID-19 pandemic: Implications for psychological wellbeing. Gerontologist 2021, 61, 205–216. [Google Scholar] [CrossRef]
- Jiang, D. Perceived stress and daily wellbeing during the COVID-19 outbreak: The moderating role of age. Front. Psychol. 2020, 11, 571873. [Google Scholar] [CrossRef]
- Ceccato, I.; Palumbo, R.; Di Crosta, A.; La Malva, P.; Marchetti, D.; Maiella, R.; Palumbo, R. Age-related differences in the perception of COVID-19 emergency during the Italian outbreak. Aging Ment. Health 2021, 25, 1305–1313. [Google Scholar] [CrossRef]
- Mangolian Shahrbabaki, P.; Dehghan, M.; Maazallahi, M.; Asadi, N. Fear and anxiety in girls aged 7 to 11 years old and related factors during the coronavirus disease pandemic. Clin. Child. Psychol. Psychiatry 2021, 1–10. [Google Scholar] [CrossRef]
- Elsharkawy, N.B.; Abdelaziz, E.M. Levels of fear and uncertainty regarding the spread of coronavirus disease (COVID-19) among university students. Perspect. Psychiatr. Care 2020, 57, 1356–1364. [Google Scholar] [CrossRef]
- Cvetković, V.M.; Nikolić, N.; Nenadić, R.U.; Ocal, A.; Zečević, M. Preparedness and preventive behaviors for a pandemic disaster caused by COVID-19 in Serbia. Int. J. Environ. Res. Public Health 2020, 17, 4124. [Google Scholar] [CrossRef]
- Kumiko, F.; Shaw, R. Preparing International Joint Project: Use of Japanese Flood Hazard Map in Bangladesh. Int. J. Disaster Risk Manag. 2019, 1, 62–80. [Google Scholar]
- Olawuni, P.; Olowoporoku, O.; Daramola, O. Determinants of Residents’ Participation in Disaster Risk Management in Lagos Metropolis Nigeria. Int. J. Disaster Risk Manag. 2020, 2, 1–19. [Google Scholar] [CrossRef]
- Öcal, A.; Cvetković, V.M.; Baytiyeh, H.; Tedim, F.M.S.; Zečević, M. Public reactions to the disaster COVID-19: A comparative study in Italy, Lebanon, Portugal, and Serbia. Geomat. Nat. Hazards Risk 2020, 11, 1864–1885. [Google Scholar] [CrossRef]
- Ornell, F.; Schuch, J.B.; Sordi, A.O.; Kessler, F.H.P. “Pandemic fear” and COVID-19: Mental health burden and strategies. Braz. J. Psychiatry 2020, 42, 232–235. [Google Scholar] [CrossRef] [Green Version]
- Kennedy, P.J.; Ressler, E. Handbook of Disaster Research; Springer Science & Business Media: New York, NY, USA, 2009; pp. 1–605. [Google Scholar]
- Zaccagni, L.; Toselli, S.; Barbieri, D. Physical Activity during COVID-19 Lockdown in Italy: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 6416. [Google Scholar] [CrossRef] [PubMed]





| Variable | Category | (f) | % |
|---|---|---|---|
| Male | Male | 580 | 47.3 |
| Female | 646 | 52.6 | |
| Age | 18–30 | 650 | 53.02 |
| 31–45 | 380 | 31 | |
| 46–64 | 196 | 15.9 | |
| Marital status | Single | 491 | 40 |
| Married | 512 | 41.8 | |
| Divorced | 212 | 17.3 | |
| Widower/Widow | 11 | 0.9 | |
| Education | Primary Sch. (grade 4–5) | 89 | 7.26 |
| Secondary Sch. (grade 8–9) | 690 | 56.2 | |
| High school (grade 11–12) | 85 | 6.9 | |
| Undergraduate | 272 | 22.19 | |
| Master/doctorate | 90 | 7.34 | |
| Number of children | 1 | 570 | 46.49 |
| 2–3 | 111 | 9.05 | |
| 4+ | 65 | 5.30 | |
| None (0) | 480 | 39.15 | |
| COVİD-19 knowledge | Very poor | 34 | 2.8 |
| Poor | 91 | 7.4 | |
| Moderate | 529 | 43.1 | |
| Good | 470 | 38.3 | |
| Excellent | 102 | 8.3 | |
| TOTAL | 1226 | 100 | |
| Predictor Variable | Previous Fear | Fear About COVID-19 | Recover of Yourself | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE | β | B | SE | β | B | SE | β | |
| Gender | −0.234 | 0.056 | −0.119 ** | −0.218 | 0.063 | −0.099 ** | 0.261 | 0.101 | 0.074 * |
| Age | 0.036 | 0.073 | 0.018 | −0.223 | 0.082 | −0.098 * | −0.215 | 0.132 | −0.059 |
| Marital status | −0.155 | 0.056 | −0.085 * | −0.098 | 0.063 | −0.048 | 0.017 | 0.101 | 0.005 |
| Education level | −0.105 | 0.370 | −0.008 | −1.02 | 0.414 | −0.071 * | 1.704 | 0.668 | 0.073 * |
| Children | −0.007 | 0.087 | −0.003 | −0.164 | 0.098 | −0.061 | −0.049 | 0.158 | −0.011 |
| Knowledge of coronavirus | −0.009 | 0.085 | −0.003 | 0.054 | 0.095 | 0.016 | 0.246 | 0.153 | 0.046 |
| Adjusted R2 | 0.16 | 0.18 | 0.12 | ||||||
| Variable | F | p | Sum of Squares | Mean Square | Single | Married | Divorced | Widow |
|---|---|---|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | M (SD) | |||||
| Previous fear | 5.43 | 0.001 ** | 13.02 | 4.34 | 1.62 (0.92) | 3.77 (1.12) | 2.68 (1.05) | 2.45 (1.03) |
| Fear about COVID-19 | 1.54 | 0.200 | 4.70 | 1.57 | 1.88 (0.99) | 2.01 (1.00) | 1.96 (1.05) | 2.18 (0.87) |
| Recovery of yourself | 1.12 | 0.339 | 8.82 | 2.94 | 2.52 (1.65) | 2.49 (1.60) | 2.68 (1.59) | 3.09 (1.04) |
| I fear for my own life and health | 5.48 | 0.001 ** | 26.87 | 8.95 | 2.38 (1.26) | 2.55 (1.24) | 2.75 (1.39) | 2.18 (1.07) |
| I fear for the life and health of my wife/husband | 52.49 | 0.000 ** | 363.08 | 121.02 | 2.18 (1.61) | 3.16 (1.44) | 3.52 (1.46) | 2.91 (1.30) |
| I fear for the life and health of my children | 66.33 | 0.000 ** | 535.30 | 178.43 | 2.11 (1.63) | 2.24 (1.66) | 3.87 (1.58) | 3.09 (1.57) |
| I fear for the life and health of my parents | 2.16 | 0.090 | 10.04 | 3.34 | 4.13 (1.26) | 4.25 (1.18) | 4.01 (1.34) | 4.45 (0.68) |
| I fear for the life and health of my pets | 4.31 | 0.005 * | 34.49 | 11.49 | 2.24 (1.58) | 2.29 (1.59) | 2.53 (1.69) | 2.45 (1.50) |
| I fear for losing goods in the house | 0.44 | 0.718 | 2.56 | 0.85 | 2.22 (1.34) | 2.31 (1.37) | 2.31 (1.48) | 2.27 (0.90) |
| I fear losing my wealth | 1.99 | 0.113 | 11.46 | 3.82 | 2.20 (1.32) | 2.32 (1.40) | 2.46 (1.49) | 2.00 (1.09) |
| I fear for losing my job | 2.71 | 0.044 * | 17.27 | 5.75 | 2.13 (1.46) | 2.08 (1.42) | 2.06 (1.51) | 2.11 (1.32) |
| I fear the lack of food supplies | 1.91 | 0.125 | 9.29 | 3.09 | 2.23 (1.19) | 2.27 (1.29) | 2.46 (1.38) | 2.64 (0.94) |
| I fear the lack of medicine and pills | 5.65 | 0.001 ** | 33.98 | 11.32 | 2.64 (1.39) | 2.61 (1.38) | 2.01 (1.37) | 2.55 (1.46) |
| I fear from a post-pandemic period trauma | 1.81 | 0.142 | 9.97 | 3.32 | 2.08 (1.29) | 2.15 (1.35) | 2.32 (1.46) | 2.55 (1.57) |
| I fear for I have not got enough money for recovery | 1.74 | 0.156 | 10.86 | 3.62 | 2.47 (1.44) | 2.57 (1.40) | 2.73 (1.53) | 2.73 (1.19) |
| I fear for losing my friends | 5.77 | 0.001 ** | 41.79 | 13.93 | 2.49 (1.59) | 2.42 (1.50) | 2.76 (1.58) | 2.66 (1.47) |
| I fear for not attend to (continue) my school | 0.89 | 0.444 | 5.35 | 1.78 | 2.26 (1.38) | 2.23 (1.45) | 2.08 (1.36) | 2.18 (1.40) |
| I fear for I cannot receive treatment in the hospital | 0.96 | 0.407 | 5.91 | 1.97 | 3.30 (1.45) | 3.41 (1.37) | 3.42 (1.50) | 3.82 (1.32) |
| Variable | F | p | Sum of Squares | Mean Square | Primary Sch. (Grade 4–5) | Secondary Sch. (Grade 8–9) | High School (Grade 11–12) | Undergraduate | Master/Doctorate |
|---|---|---|---|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | |||||
| Previous fear | 0.519 | 0.669 | 1.25 | 0.42 | 1.67 (1.63) | 1.65 (0.90) | 1.72 (0.90) | 1.75 (0.82) | 1.64 (0.89) |
| Fear about COVID-19 | 2.54 | 0.055 | 7.71 | 2.57 | 1.00 (0.00) | 1.88 (0.96) | 1.98 (1.02) | 1.99 (1.00) | 1.87 (0.99) |
| Recovery of yourself | 5.04 | 0.002 * | 39.30 | 13.10 | 2.13 (1.46) | 1.85 (1.35) | 2.01 (1.34) | 2.5 (1.31) | 1.89 (1.40) |
| I fear for my own life and health | 1.41 | 0.236 | 7.02 | 2.34 | 4. 33 (1.63) | 2.34 (1.58) | 2.56 (1.63) | 2.49 (1.61) | 2.76 (1.56) |
| I fear for the life and health of my wife/husband | 0.10 | 0.959 | 0.79 | 0.26 | 2.00 (1.67) | 2.51 (1.35) | 2.57 (1.28) | 2.53 (1.39) | 2.36 (1.08) |
| I fear for the life and health of my children | 2.27 | 0.079 | 21.20 | 7.06 | 3.00 (2.19) | 2.79 (1.66) | 2.84 (1.61) | 2.82 (1.41) | 2.85 (1.46) |
| I fear for the life and health of my parents | 6.65 | 0.000 ** | 30.51 | 10.17 | 3.85 (1.25) | 3.90 (1.28) | 4.05 (1.35) | 3.95 (1.18) | 4.09 (1.23) |
| I fear for the life and health of my pets | 4.12 | 0.006 * | 33.07 | 11.01 | 2.17 (1.58) | 2.30 (1.62) | 2.21 (1.68) | 2.44 (1.64) | 1.99 (1.47) |
| I fear for losing goods in the house | 5.88 | 0.001 ** | 33.21 | 11.07 | 2.21 (1.37) | 2.42 (1.45) | 2.34 (1.64) | 2.15 (1.58) | 1.98 (1.27) |
| I fear losing my wealth | 0.93 | 0.423 | 5.93 | 1.79 | 1.67 (1.63) | 2.42 (1.45) | 2.30 (1.35) | 1.65 (0.95) | 1.87 (1.26) |
| I fear for losing my job | 2.49 | 0.058 | 15.89 | 5.29 | 1.66 (1.63) | 2.37 (1.46) | 2.29 (1.37) | 2.40 (1.57) | 2.20 (1.30) |
| I fear the lack of food supplies | 3.05 | 0.028 | 14.73 | 4.91 | 1.67 (1.63) | 2.28 (1.55) | 2.16 (1.45) | 1.90 (1.26) | 2.00 (1.38) |
| I fear the lack of medicine and pills | 1.30 | 0.272 | 7.92 | 2.64 | 1.65 (1.63) | 2.41 (1.39) | 2.29 (1.22) | 2.06 (1.21) | 1.85 (1.95) |
| I fear from a post-pandemic period trauma | 3.49 | 0.015 | 19.13 | 6.37 | 3.33 (1.96) | 2.68 (1.49) | 2.73 (1.40) | 2.53 (1.32) | 2.15 (1.58) |
| I fear for I have not got enough money for recovery | 5.11 | 0.002 * | 31.57 | 10.52 | 2.18 (1.36) | 2.37 (1.46) | 2.10 (1.48) | 2.05 (1.39) | 1.98 (1.40) |
| I fear for losing my friends | 2.22 | 0.084 | 16.23 | 5.41 | 2.00 (1.67) | 2.13 (1.33) | 2.23 (1.38) | 1.84 (1.17) | 1.54 (1.58) |
| I fear for not attend to (continue) my school | 9.83 | 0.000 ** | 57.70 | 19.23 | 3.50 (1.97) | 2.24 (1.45) | 2.30 (1.42) | 1.69 (1.06) | 3.01 (1.01) |
| I fear for I cannot receive treatment in the hospital | 1.62 | 0.059 | 15.94 | 5.31 | 3.67 (2.06) | 3.27 (1.47) | 3.45 (1.39) | 3.15 (1.46) | 3.01 (1.95) |
| Variable | F | p | Sum of Squares | Mean Square | 18–30 | 31–45 | 46–64 |
|---|---|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | |||||
| Previous fear | 1.30 | 0.272 | 3.15 | 1.05 | 1.91 (0.98) | 2.17 (1.09) | 1.83 (0.96) |
| Fear about COVID-19 | 4.71 | 0.003 * | 14.23 | 4.76 | 1.73 (0.88) | 1.69 (0.87) | 1.71 (0.85) |
| Recovery of yourself | 1.75 | 0.155 | 13.70 | 4.57 | 2.48 (1.63) | 2.71 (1.61) | 2.58 (1.47) |
| I fear for my own life and health | 1.42 | 0.234 | 7.05 | 2.35 | 2.51 (1.29) | 2.52 (1.18) | 2.69 (1.32) |
| I fear for the life and health of my wife/husband | 9.36 | 0.000 ** | 71.44 | 23.81 | 2.70 (1.62) | 3.06 (1.55) | 3.42 (1.45) |
| I fear for the life and health of my children | 41.10 | 0.000 ** | 349.71 | 116.57 | 2.20 (1.66) | 2.90 (1.80) | 3.94 (1.58) |
| I fear for the life and health of my parents | 7.26 | 0.000 ** | 32.94 | 10.98 | 4.25 (1.16) | 3.95 (1.36) | 3.98 (1.41) |
| I fear for the life and health of my pets | 1.91 | 0.053 | 23.30 | 7.76 | 2.45 (1.67) | 2.11 (1.50) | 2.45 (1.56) |
| I fear for losing goods in the house | 1.85 | 0.056 | 16.20 | 5.40 | 2.96 (1.35) | 2.18 (1.40) | 2.48 (1.52) |
| I fear losing my wealth | 1.19 | 0.310 | 6.88 | 2.29 | 2.27 (1.36) | 2.34 (1.39) | 2.48 (1.55) |
| I fear for losing my job | 11.44 | 0.000 ** | 71.32 | 23.77 | 2.02 (1.41) | 2.37 (1.51) | 2.48 (1.53) |
| I fear the lack of food supplies | 1.72 | 0.160 | 8.35 | 2.78 | 2.26 (1.24) | 2.37 (1.27) | 2.48 (1.49) |
| I fear the lack of medicine and pills | 7.14 | 0.000 ** | 42.70 | 14.23 | 2.63 (1.41) | 2.78 (1.31) | 3.19 (1.59) |
| I fear from a post-pandemic period trauma | 3.88 | 0.009 * | 21.24 | 7.08 | 2.50 (1.41) | 2.14 (1.44) | 2.13 (1.32) |
| I fear for I have not got enough money for recovery | 3.79 | 0.010 * | 23.54 | 7.84 | 2.50 (1.40) | 2.41 (1.50) | 2.38 (1.48) |
| I fear for losing my friends | 4.67 | 0.003 * | 33.85 | 11.28 | 2.44 (1.65) | 2.59 (1.53) | 2.99 (1.61) |
| I fear for not attend to (continue) my school | 8.48 | 0.000 ** | 49.71 | 16.57 | 2.31 (1.44) | 1.80 (1.19) | 2.27 (1.38) |
| I fear for I cannot receive treatment in the hospital | 0.55 | 0.645 | 3.38 | 1.13 | 3.35 (1.41) | 3.44 (1.40) | 3.40 (1.52) |
| Variable | Marital Status | Education Level | Age | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | p | Sum of Squares | Mean Square | F | p | Sum of Squares | Mean Square | F | p | Sum of Squares | Mean Square | |
| TV programs | 0.960 | 0.411 | 3.92 | 1.30 | 3.32 | 0.019 * | 13.50 | 4.50 | 1.98 | 0.114 | 8.05 | 2.68 |
| Government (official) | 2.64 | 0.048 * | 13.03 | 4.34 | 1.76 | 0.153 | 8.69 | 2.90 | 14.01 | 0.000 ** | 67.17 | 22.39 |
| Military or emergency services | 4.78 | 0.003 * | 22.63 | 7.54 | 2.68 | 0.045 * | 12.76 | 4.25 | 11.54 | 0.000 ** | 53.75 | 17.91 |
| Social media (Facebook, Twitter) | 0.219 | 0.883 | 0.81 | 0.27 | 0.455 | 0.714 | 1.68 | 0.56 | 0.227 | 0.878 | 0.84 | 0.28 |
| My friends or colleagues | 1.53 | 0.203 | 4.80 | 1.60 | 2.07 | 0.102 | 6.46 | 2.15 | 4.97 | 0.002 * | 15.25 | 5.08 |
| Radio | 2.29 | 0.077 | 8.69 | 2.89 | 1.52 | 0.207 | 5.78 | 1.92 | 1.88 | 0.131 | 7.09 | 2.36 |
| Newspaper | 2.82 | 0.037 | 9.63 | 3.21 | 1.84 | 0.057 | 9.68 | 3.22 | 1.67 | 0.171 | 5.66 | 1.88 |
| Academic journals or magazines | 4.29 | 0.005 | 22.60 | 7.53 | 5.50 | 0.001 ** | 28.90 | 9.63 | 0.963 | 0.409 | 5.10 | 1.70 |
| Scientists | 1.20 | 0.306 | 3.92 | 1.30 | 0.815 | 0.485 | 2.65 | 0.88 | 1.63 | 0.179 | 5.32 | 1.77 |
| Variable | Gender | |||||
|---|---|---|---|---|---|---|
| F | t | Sig. (2-Tailed) | df | Male X (SD) | Female X (SD) | |
| Previous fear | 14.98 | −4.58 | 0.000 ** | 804 | 1.54 (0.768) | 1.78 (0.933) |
| Fear about COVID-19 | 0.000 | −3.31 | 0.001 ** | 1224 | 1.80 (0.941) | 2.01 (1.02) |
| Recovery of yourself | 2.66 | 2.67 | 0.008 * | 1224 | 2.73 (1.67) | 2.46 (1.58) |
| I fear for my own life and health | 1.81 | −4.95 | 0.000 ** | 1224 | 2.25 (1.23) | 2.64 (1.28) |
| I fear for the life and health of my wife/husband | 0.440 | −1.10 | 0.270 | 1224 | 2.75 (1.58) | 2.86 (1.62) |
| I fear for the life and health of my children | 10.49 | −1.04 | 0.285 | 1224 | 2.41 (1.69) | 2.52 (1.79) |
| I fear for the life and health of my parents | 3.64 | −3.84 | 0.000 ** | 1224 | 3.95 (1.31) | 4.25 (1.20) |
| I fear for the life and health of my pets | 2.18 | −1.60 | 0.109 | 1224 | 2.27 (1.61) | 2.44 (1.64) |
| I fear for losing goods in the house | 0.350 | −2.65 | 0.008 * | 1224 | 2.12 (1.39) | 2.34 (1.36) |
| I fear for losing my wealth | 0.412 | −1.27 | 0.204 | 1224 | 2.22 (1.41) | 2.33 (1.33) |
| I fear losing my job | 5.19 | −1.56 | 0.118 | 728 | 2.05 (1.39) | 2.19 (1.48) |
| I fear the lack of food supplies | 3.23 | −1.44 | 0.159 | 1224 | 2.21 (1.22) | 2.32 (1.29) |
| I fear the lack of medicine and pills | 0.132 | −4.95 | 0.000 ** | 851 | 2.39 (1.39) | 2.83 (1.41) |
| I fear from a post-pandemic period trauma | 62.40 | −7.99 | 0.000 ** | 746 | 1.73 (1.11) | 2.34 (1.40) |
| I fear for have not got enough money to recover | 12.18 | −5.42 | 0.000 ** | 772 | 2.23 (1.33) | 2.70 (1.46) |
| I fear for losing my friends | 27.50 | −3.03 | 0.002 ** | 736 | 2.32 (1.41) | 2.60 (1.61) |
| I fear for not attending to (continue) my school | 12.47 | −4.18 | 0.000 ** | 634 | 1.97 (1.32) | 2.32 (1.43) |
| I fear for I cannot receive treatment in the hospital | 5.59 | −7.04 | 0.000 ** | 1224 | 2.92 (1.47) | 3.56 (1.36) |
| Variable | Gender | |||||
|---|---|---|---|---|---|---|
| F | Sig. (2-Tailed) | t | df | Male X (SD) | Female X (SD) | |
| TV programs | 17.36 | 0.000 ** | −4.15 | 1224 | 2.68 (1.24) | 2.98 (1.11) |
| Government (official) | 8.17 | 0.000 ** | −5.22 | 1224 | 3.30 (1.35) | 3.71 (1.23) |
| Military or emergency services | 10.42 | 0.000 ** | −4.81 | 625 | 3.32 (1.34) | 3.71 (1.20) |
| Social media | 22.72 | 0.017 * | 2.38 | 612 | 2.18 (1.20) | 2.00 (1.06) |
| My friends or colleagues | 4.08 | 0.053 | 1.71 | 1224 | 2.44 (1.06) | 2.33 (0.999) |
| Radio | 0.306 | 0.000 ** | −4.47 | 1224 | 2.22 (1.10) | 2.53 (1.12) |
| Newspaper | 0.315 | 0.005 * | −2.79 | 1224 | 2.05 (1.10) | 2.24 (1.04) |
| Academic journals or magazines | 5.02 | 0.000 ** | −4.72 | 1224 | 2.78 (1.37) | 3.17 (1.29) |
| Scientists | 3.19 | 0.000 ** | −3.50 | 1224 | 3.89 (1.10) | 4.12 (1.00) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cvetković, V.M.; Nikolić, N.; Ocal, A.; Martinović, J.; Dragašević, A. A Predictive Model of Pandemic Disaster Fear Caused by Coronavirus (COVID-19): Implications for Decision-Makers. Int. J. Environ. Res. Public Health 2022, 19, 652. https://doi.org/10.3390/ijerph19020652
Cvetković VM, Nikolić N, Ocal A, Martinović J, Dragašević A. A Predictive Model of Pandemic Disaster Fear Caused by Coronavirus (COVID-19): Implications for Decision-Makers. International Journal of Environmental Research and Public Health. 2022; 19(2):652. https://doi.org/10.3390/ijerph19020652
Chicago/Turabian StyleCvetković, Vladimir M., Neda Nikolić, Adem Ocal, Jovana Martinović, and Aleksandar Dragašević. 2022. "A Predictive Model of Pandemic Disaster Fear Caused by Coronavirus (COVID-19): Implications for Decision-Makers" International Journal of Environmental Research and Public Health 19, no. 2: 652. https://doi.org/10.3390/ijerph19020652








