Phagocytosis Checkpoints in Glioblastoma: CD47 and Beyond
Abstract
1. Introduction
1.1. Glioblastoma and Immunotherapy
1.2. Tumor-Associated Macrophages
1.3. Macrophage Phagocytosis of Glioma Cells
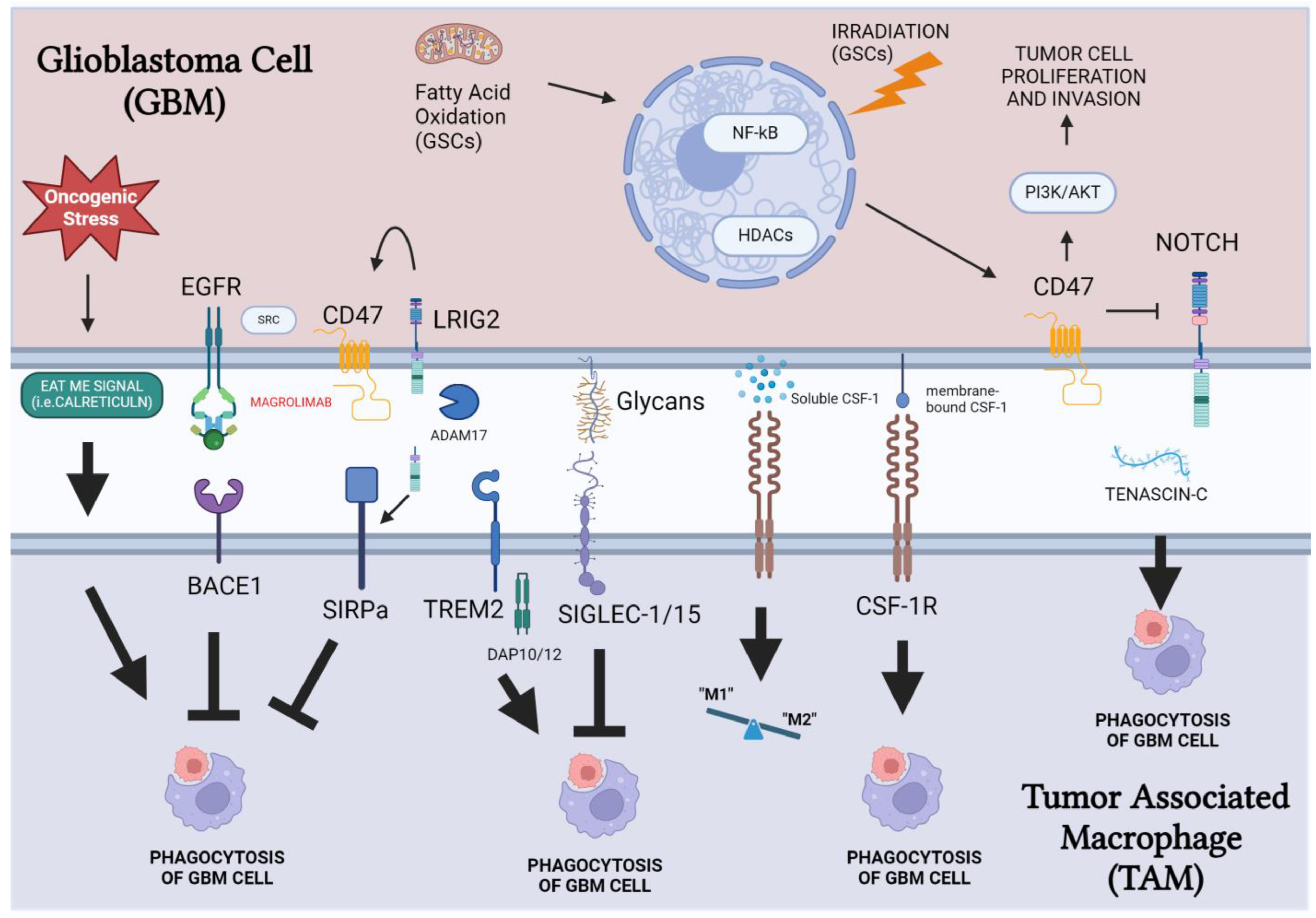
2. Pathways Regulating TAM Phagocytosis of GBM Cells
2.1. CD47/SIRP Pathway
2.2. CSF-1/CSF-1R Pathway
2.3. BACE-1
2.4. TREM2
2.5. Siglecs
2.6. Phagocytosis Checkpoint Cooperation with Anti-CTLA4/PD-1/PD-L1 ICIs
2.7. Chimeric Antigen Receptor-M
3. Conclusions and Perspectives
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ostrom, Q.T.; Price, M.; Neff, C.; Cioffi, G.; Waite, K.A.; Kruchko, C.; Barnholtz-Sloan, J.S. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2016–2020. Neuro Oncol. 2023, 25, IV1–IV99. [Google Scholar] [CrossRef] [PubMed]
- Du, R.; Tripathi, S.; Najem, H.; Brat, D.J.; Lukas, R.V.; Zhang, P.; Heimberger, A.B. Glioblastoma Phagocytic Cell Death: Balancing the Opportunities for Therapeutic Manipulation. Cells 2024, 13, 823. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Zhang, Y.; Xu, Y.; Huang, Z.; Cheng, G.; Xie, M.; Zhou, Z.; Yu, Y.; Xi, W.; Fan, Y. Tumor Immune Microenvironment and Immunotherapy Efficacy in BRAF Mutation Non-Small-Cell Lung Cancer. Cell Death Dis. 2022, 13, 1064. [Google Scholar] [CrossRef]
- Miyazaki, T.; Ishikawa, E.; Sugii, N.; Matsuda, M. Therapeutic Strategies for Overcoming Immunotherapy Resistance Mediated by Immunosuppressive Factors of the Glioblastoma Microenvironment. Cancers 2020, 12, 1960. [Google Scholar] [CrossRef] [PubMed]
- Sanders, S.; Debinski, W. Challenges to Successful Implementation of the Immune Checkpoint Inhibitors for Treatment of Glioblastoma. Int. J. Mol. Sci. 2020, 21, 2759. [Google Scholar] [CrossRef]
- Wang, X.; Guo, G.; Guan, H.; Yu, Y.; Lu, J.; Yu, J. Challenges and Potential of PD-1/PD-L1 Checkpoint Blockade Immunotherapy for Glioblastoma. J. Exp. Clin. Cancer Res. 2019, 38, 87. [Google Scholar] [CrossRef]
- Reardon, D.A.; Brandes, A.A.; Omuro, A.; Mulholland, P.; Lim, M.; Wick, A.; Baehring, J.; Ahluwalia, M.S.; Roth, P.; Bähr, O.; et al. Effect of Nivolumab vs Bevacizumab in Patients with Recurrent Glioblastoma: The CheckMate 143 Phase 3 Randomized Clinical Trial. JAMA Oncol. 2020, 6, 1003–1010. [Google Scholar] [CrossRef]
- Pacheco, J.M.; Camidge, D.R.; Doebele, R.C.; Schenk, E. A Changing of the Guard: Immune Checkpoint Inhibitors With and Without Chemotherapy as First Line Treatment for Metastatic Non-Small Cell Lung Cancer. Front. Oncol. 2019, 9, 195. [Google Scholar] [CrossRef] [PubMed]
- Lim, M.; Weller, M.; Idbaih, A.; Steinbach, J.; Finocchiaro, G.; Raval, R.R.; Ansstas, G.; Baehring, J.; Taylor, J.W.; Honnorat, J.; et al. Phase III Trial of Chemoradiotherapy with Temozolomide plus Nivolumab or Placebo for Newly Diagnosed Glioblastoma with Methylated MGMT Promoter. Neuro Oncol. 2022, 24, 1935–1949. [Google Scholar] [CrossRef]
- Omuro, A.; Brandes, A.A.; Carpentier, A.F.; Idbaih, A.; Reardon, D.A.; Cloughesy, T.; Sumrall, A.; Baehring, J.; van den Bent, M.; Bähr, O.; et al. Radiotherapy Combined with Nivolumab or Temozolomide for Newly Diagnosed Glioblastoma with Unmethylated MGMT Promoter: An International Randomized Phase III Trial. Neuro Oncol. 2023, 25, 123–134. [Google Scholar] [CrossRef]
- Cloughesy, T.F.; Mochizuki, A.Y.; Orpilla, J.R.; Hugo, W.; Lee, H.; Davidson, T.B.; Wang, A.C.; Ellingson, B.M.; Julie, A.; Sanders, C.M.; et al. Neoadjuvant anti-PD-1 immunotherapy promotes a survival benefit with intratumoral and systemic immune responses in recurrent glioblastoma. Nat. Med. 2019, 25, 477–486. [Google Scholar] [CrossRef] [PubMed]
- Schalper, K.A.; Rodriguez-Ruiz, M.E.; Diez-Valle, R.; López-Janeiro, A.; Porciuncula, A.; Idoate, M.A.; Inogés, S.; de Andrea, C.; López-Diaz de Cerio, A.; Tejada, S.; et al. Neoadjuvant Nivolumab Modifies the Tumor Immune Microenvironment in Resectable Glioblastoma. Nat. Med. 2019, 25, 470–476. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Tian, Y.; Li, Q.; Jiang, R.; Zhang, J. Uncovering the Immune Cell Infiltration Landscape in Low-Grade Glioma for Aiding Immunotherapy. J. Oncol. 2022, 2022, 3370727. [Google Scholar] [CrossRef] [PubMed]
- Joyce, J.; Pollard, J.W. Microenvironmental Regulation of Metastasis. Nat. Rev. Cancer 2009, 9, 239–252. [Google Scholar] [CrossRef]
- Kitamura, T.; Qian, B.-Z.; Soong, D.; Cassetta, L.; Noy, R.; Sugano, G.; Kato, Y.; Li, J.; Pollard, J.W. CCL2-Induced Chemokine Cascade Promotes Breast Cancer Metastasis by Enhancing Retention of Metastasis-Associated Macrophages. J. Exp. Med. 2015, 212, 1043–1059. [Google Scholar] [CrossRef] [PubMed]
- Quail, D.F.; Joyce, J.A. The Microenvironmental Landscape of Brain Tumors. Cancer Cell 2017, 31, 326–341. [Google Scholar] [CrossRef]
- Gieryng, A.; Kaminska, B. Myeloid-Derived Suppressor Cells in Gliomas. Wspolczesna Onkol. 2016, 20, 345–351. [Google Scholar] [CrossRef]
- Graeber, M.B.; Scheithauer, B.W.; Kreutzberg, G.W. Microglia in Brain Tumors. Glia 2002, 40, 252–259. [Google Scholar] [CrossRef]
- Locarno, C.V.; Simonelli, M.; Carenza, C.; Capucetti, A.; Stanzani, E.; Lorenzi, E.; Persico, P.; Della Bella, S.; Passoni, L.; Mavilio, D.; et al. Role of Myeloid Cells in the Immunosuppressive Microenvironment in Gliomas. Immunobiology 2020, 225, 151853. [Google Scholar] [CrossRef]
- Richard, Q.; Laurenge, A.; Mallat, M.; Sanson, M.; Castro-Vega, L.J. New Insights into the Immune TME of Adult-Type Diffuse Gliomas. Curr. Opin. Neurol. 2022, 35, 794–802. [Google Scholar] [CrossRef]
- Hambardzumyan, D.; Gutmann, D.H.; Kettenmann, H. The Role of Microglia and Macrophages in Glioma Maintenance and Progression. Nat. Neurosci. 2016, 19, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Galarneau, H.; Villeneuve, J.; Gowing, G.; Julien, J.P.; Vallières, L. Increased Glioma Growth in Mice Depleted of Macrophages. Cancer Res. 2007, 67, 8874–8881. [Google Scholar] [CrossRef] [PubMed]
- Coniglio, S.J.; Eugenin, E.; Dobrenis, K.; Stanley, E.R.; West, B.L.; Symons, M.H.; Segall, J.E. Microglial Stimulation of Glioblastoma Invasion Involves Epidermal Growth Factor Receptor (EGFR) and Colony Stimulating Factor 1 Receptor (CSF-1R) Signaling. Mol. Med. 2012, 18, 519–527. [Google Scholar] [CrossRef] [PubMed]
- Zhu, C.; Mustafa, D.; Zheng, P.P.; Van Der Weiden, M.; Sacchetti, A.; Brandt, M.; Chrifi, I.; Tempel, D.; Leenen, P.J.M.; Duncker, D.J.; et al. Activation of CECR1 in M2-like TAMs Promotes Paracrine Stimulation-Mediated Glial Tumor Progression. Neuro Oncol. 2017, 19, 648–659. [Google Scholar] [CrossRef] [PubMed]
- Sielska, M.; Przanowski, P.; Pasierbińska, M.; Wojnicki, K.; Poleszak, K.; Wojtas, B.; Grzeganek, D.; Ellert-Miklaszewska, A.; Ku, M.; Kettenmann, H.; et al. Tumour-Derived CSF2/Granulocyte Macrophage Colony Stimulating Factor Controls Myeloid Cell Accumulation and Progression of Gliomas. Br. J. Cancer 2020, 123, 438–448. [Google Scholar] [CrossRef] [PubMed]
- Platten, M.; Kretz, A.; Naumann, U.; Aulwurm, S.; Egashira, K.; Isenmann, S.; Weller, M. Monocyte Chemoattractant Protein-1 Increases Microglial Infiltration and Aggressiveness of Gliomas. Ann. Neurol. 2003, 54, 388–392. [Google Scholar] [CrossRef] [PubMed]
- Maas, S.L.N.; Abels, E.R.; Van De Haar, L.L.; Zhang, X.; Morsett, L.; Sil, S.; Guedes, J.; Sen, P.; Prabhakar, S.; Hickman, S.E.; et al. Glioblastoma Hijacks Microglial Gene Expression to Support Tumor Growth. J. Neuroinflamm. 2020, 17, 120. [Google Scholar] [CrossRef] [PubMed]
- Yuan, D.; Tao, Y.; Chen, G.; Shi, T. Systematic Expression Analysis of Ligand-Receptor Pairs Reveals Important Cell-to-Cell Interactions inside Glioma. Cell Commun. Signal. 2019, 17, 48. [Google Scholar] [CrossRef] [PubMed]
- Schultze, J.L.; Freeman, T.; Hume, D.A.; Latz, E. A Transcriptional Perspective on Human Macrophage Biology. Semin. Immunol. 2015, 27, 44–50. [Google Scholar] [CrossRef]
- Xue, J.; Schmidt, S.V.; Sander, J.; Draffehn, A.; Krebs, W.; Quester, I.; De Nardo, D.; Gohel, T.D.; Emde, M.; Schmidleithner, L.; et al. Transcriptome-Based Network Analysis Reveals a Spectrum Model of Human Macrophage Activation. Immunity 2014, 40, 274–288. [Google Scholar] [CrossRef]
- Brooks, L.J.; Parrinello, S. Vascular Regulation of Glioma Stem-like Cells: A Balancing Act. Curr. Opin. Neurobiol. 2017, 47, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Kim, J.K.; Jeon, H.Y.; Ham, S.W.; Kim, H. CD133 Regulates IL-1β Signaling and Neutrophil Recruitment in Glioblastoma. Mol. Cells 2017, 40, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Dzaye, O.D.A.; Hu, F.; Derkow, K.; Haage, V.; Euskirchen, P.; Harms, C.; Lehnardt, S.; Synowitz, M.; Wolf, S.A.; Kettenmann, H. Glioma Stem Cells but Not Bulk Glioma Cells Upregulate IL-6 Secretion in Microglia/Brain Macrophages via Toll-like Receptor 4 Signaling. J. Neuropathol. Exp. Neurol. 2016, 75, 429–440. [Google Scholar] [CrossRef] [PubMed]
- Codrici, E.; Enciu, A.-M.; Popescu, I.-D.; Mihai, S.; Tanase, C. Glioma Stem Cells and Their Microenvironments: Providers of Challenging Therapeutic Targets. Stem Cells Int. 2016, 2016, 5728438. [Google Scholar] [CrossRef]
- Yao, Y.; Ye, H.; Qi, Z.; Mo, L.; Yue, Q.; Baral, A.; Hoon, D.S.B.; Vera, J.C.; Heiss, J.D.; Chen, C.C.; et al. B7-H4(B7x)-Mediated Cross-Talk between Glioma-Initiating Cells and Macrophages via the IL6/JAK/STAT3 Pathway Lead to Poor Prognosis in Glioma Patients. Clin. Cancer Res. 2016, 22, 2778–2790. [Google Scholar] [CrossRef]
- Wu, A.; Wei, J.; Kong, L.-Y.; Wang, Y.; Priebe, W.; Qiao, W.; Sawaya, R.; Heimberger, A.B. Glioma Cancer Stem Cells Induce Immunosuppressive Macrophages/Microglia. Neuro Oncol. 2010, 12, 1113–1125. [Google Scholar] [CrossRef]
- Coniglio, S.J.; Segall, J.E. Review: Molecular Mechanism of Microglia Stimulated Glioblastoma Invasion. Matrix Biol. 2013, 32, 372–380. [Google Scholar] [CrossRef]
- Gao, H.; Zhang, I.Y.; Zhang, L.; Song, Y.; Liu, S.; Ren, H.; Liu, H.; Zhou, H.; Su, Y.; Yang, Y.; et al. S100B Suppression Alters Polarization of Infiltrating Myeloid-Derived Cells in Gliomas and Inhibits Tumor Growth. Cancer Lett. 2018, 439, 91–100. [Google Scholar] [CrossRef]
- Wei, J.; Gabrusiewicz, K.; Heimberger, A. The Controversial Role of Microglia in Malignant Gliomas. Clin. Dev. Immunol. 2013, 2013, 285246. [Google Scholar] [CrossRef] [PubMed]
- AlShakweer, W.; Alwelaie, Y.; Mankung, A.M.; Graeber, M.B. Bone Marrow-Derived Microglia in Pilocytic Astrocytoma. Front. Biosci. 2011, 3, 371–379. [Google Scholar] [CrossRef][Green Version]
- Zhang, J.; Guan, M.; Wang, Q.; Zhang, J.; Zhou, T.; Sun, X. Single-Cell Transcriptome-Based Multilayer Network Biomarker for Predicting Prognosis and Therapeutic Response of Gliomas. Brief. Bioinform. 2020, 21, 1080–1097. [Google Scholar] [CrossRef] [PubMed]
- Gieryng, A.; Pszczolkowska, D.; Walentynowicz, K.A.; Rajan, W.D.; Kaminska, B. Immune Microenvironment of Gliomas. Lab. Investig. 2017, 97, 498–518. [Google Scholar] [CrossRef] [PubMed]
- Bronte, V.; Brandau, S.; Chen, S.H.; Colombo, M.P.; Frey, A.B.; Greten, T.F.; Mandruzzato, S.; Murray, P.J.; Ochoa, A.; Ostrand-Rosenberg, S.; et al. Recommendations for Myeloid-Derived Suppressor Cell Nomenclature and Characterization Standards. Nat. Commun. 2016, 7, 12150. [Google Scholar] [CrossRef] [PubMed]
- Wallace, P.K.; Romet-Lemonne, J.L.; Chokri, M.; Kasper, L.H.; Fanger, M.W.; Fadul, C.E. Production of Macrophage-Activated Killer Cells for Targeting of Glioblastoma Cells with Bispecific Antibody to FcγRI and the Epidermal Growth Factor Receptor. Cancer Immunol. Immunother. 2000, 49, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharjee, M.; Bose, I.; Sarkar, P.; Banerjee, C.; Dutta, S.; Ghosh, A.; Mukherjee, J.; Acharya, S.; Goswami, S.; Mazumdar, A.; et al. A Sequential Scanning of the Immune Efficiency in Astrocytoma (Grade I to Grade III), Meningioma and Secondary Glioma Patients with and without Therapeutic Scheduling. Cancer Investig. 2006, 24, 502–513. [Google Scholar] [CrossRef] [PubMed]
- Schiltz, P.M.; Lee, G.J.; Zhang, J.G.; Hoa, N.; Wepsic, H.T.; Dillman, R.O.; Jadus, M.R. Human Allogeneic and Murine Xenogeneic Dendritic Cells Are Cytotoxic to Human Tumor Cells via Two Distinct Pathways. Cancer Biother Radiopharm 2007, 22, 672–683. [Google Scholar] [CrossRef]
- Sasaki, A.; Yokoo, H.; Tanaka, Y.; Homma, T.; Nakazato, Y.; Ohgaki, H. Characterization of Microglia/Macrophages in Gliomas Developed in S-100β-v-ErbB Transgenic Rats. Neuropathology 2013, 33, 505–514. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, L.; Astell, K.R.; Velikova, G.; Sieger, D. A Zebrafish Live Imaging Model Reveals Differential Responses of Microglia Toward Glioblastoma Cells In Vivo. Zebrafish 2016, 13, 523–534. [Google Scholar] [CrossRef] [PubMed]
- Gu, R.; Zhang, X.; Zhang, G.; Tao, T.; Yu, H.; Liu, L.; Dou, Y.; Li, A.; Qin, J. Probing the Bi-Directional Interaction Between Microglia and Gliomas in a Tumor Microenvironment on a Microdevice. Neurochem. Res. 2017, 42, 1478–1487. [Google Scholar] [CrossRef]
- Persano, S.; Vicini, F.; Poggi, A.; Fernandez, J.L.C.; Rizzo, G.M.R.; Gavilán, H.; Silvestri, N.; Pellegrino, T. Elucidating the Innate Immunological Effects of Mild Magnetic Hyperthermia on U87 Human Glioblastoma Cells: An In Vitro Study. Pharmaceutics 2021, 13, 1668. [Google Scholar] [CrossRef]
- Chang, J.C.Y.; Wang, C.Y.; Lin, S. Interrogation of Human Microglial Phagocytosis by CRISPR Genome Editing. Front. Immunol. 2023, 14, 1169725. [Google Scholar] [CrossRef] [PubMed]
- Lecoultre, M.; Chliate, S.; Espinoza, F.I.; Tankov, S.; Dutoit, V.; Walker, P.R. Radio-Chemotherapy of Glioblastoma Cells Promotes Phagocytosis by Macrophages in Vitro. Radiother. Oncol. 2024, 190, 110049. [Google Scholar] [CrossRef] [PubMed]
- Logtenberg, M.E.W.; Scheeren, F.A.; Schumacher, T.N. The CD47-SIRPα Immune Checkpoint. Immunity 2020, 52, 742–752. [Google Scholar] [CrossRef] [PubMed]
- Khalaji, A.; Yancheshmeh, F.B.; Farham, F.; Khorram, A.; Sheshbolouki, S.; Zokaei, M.; Vatankhah, F.; Soleymani-Goloujeh, M. Don’t Eat Me/Eat Me Signals as a Novel Strategy in Cancer Immunotherapy. Heliyon 2023, 9, e20507. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Wang, Y.; Yang, Y.; Weng, L.; Wu, Q.; Zhang, J.; Zhao, P.; Fang, L.; Shi, Y.; Wang, P. Emerging Phagocytosis Checkpoints in Cancer Immunotherapy. Signal Transduct. Target. Ther. 2023, 8, 104. [Google Scholar] [CrossRef] [PubMed]
- Barclay, A.N.; Brown, M.H. The SIRP Family of Receptors and Immune Regulation. Nat. Rev. Immunol. 2006, 6, 457–464. [Google Scholar] [CrossRef] [PubMed]
- Brooke, G.P.; Parsons, K.R.; Howard, C.J. Cloning of Two Members of the SIRPα Family of Protein Tyrosine Phosphatase Binding Proteins in Cattle That Are Expressed on Monocytes and a Subpopulation of Dendritic Cells and Which Mediate Binding to CD4 T Cells. Eur. J. Immunol. 1998, 28, 1–11. [Google Scholar] [CrossRef]
- Willingham, S.B.; Volkmer, J.-P.; Gentles, J.; Sahoo, D.; Dalerba, P.; Mitra, S.S.; Wang, J.; Contreras-Trujillo, H.; Martin, R.; Cohen, J.D.; et al. The CD47-Signal Regulatory Protein Alpha (SIRPa) Interaction Is a Therapeutic Target for Human Solid Tumors. Proc. Natl. Acad. Sci. USA 2012, 109, 6662–6667. [Google Scholar] [CrossRef]
- Tseng, D.; Volkmer, J.P.; Willingham, S.B.; Contreras-Trujillo, H.; Fathman, J.W.; Fernhoff, N.B.; Seita, J.; Inlay, M.A.; Weiskopf, K.; Miyanishi, M.; et al. Anti-CD47 Antibody-Mediated Phagocytosis of Cancer by Macrophages Primes an Effective Antitumor T-Cell Response. Proc. Natl. Acad. Sci. USA 2013, 110, 11103–11108. [Google Scholar] [CrossRef]
- Feng, M.; Chen, J.Y.; Weissman-Tsukamoto, R.; Volkmer, J.-P.; Ho, P.Y.; McKenna, K.M.; Cheshier, S.; Zhang, M.; Guo, N.; Gip, P.; et al. Macrophages Eat Cancer Cells Using Their Own Calreticulin as a Guide: Roles of TLR and Btk. Proc. Natl. Acad. Sci. USA 2015, 112, 2145–2150. [Google Scholar] [CrossRef]
- Maute, R.; Xu, J.; Weissman, I.L. CD47–SIRPα-Targeted Therapeutics: Status and Prospects. Immuno-Oncol. Technol. 2022, 13, 100070. [Google Scholar] [CrossRef] [PubMed]
- Gholamin, S.; Mitra, S.S.; Feroze, A.H.; Liu, J.; Kahn, S.A.; Zhang, M.; Esparza, R.; Richard, C.; Ramaswamy, V.; Remke, M.; et al. Disrupting the CD47-SIRPα Anti-Phagocytic Axis by a Humanized Anti-CD47 Antibody Is an Efficacious Treatment for Malignant Pediatric Brain Tumors. Sci. Transl. Med. 2017, 9, eaaf2968. [Google Scholar] [CrossRef] [PubMed]
- Sikic, B.I.; Lakhani, N.; Patnaik, A.; Shah, S.A.; Chandana, S.R.; Rasco, D.; Colevas, A.D.; O’Rourke, T.; Narayanan, S.; Papadopoulos, K.; et al. First-in-Human, First-in-Class Phase i Trial of the Anti-CD47 Antibody Hu5F9-G4 in Patients with Advanced Cancers. J. Clin. Oncol. 2019, 37, 946–953. [Google Scholar] [CrossRef] [PubMed]
- Ring, N.G.; Herndler-Brandstetter, D.; Weiskopf, K.; Shan, L.; Volkmer, J.P.; George, B.M.; Lietzenmayer, M.; McKenna, K.M.; Naik, T.J.; McCarty, A.; et al. Anti-SIRPα Antibody Immunotherapy Enhances Neutrophil and Macrophage Antitumor Activity. Proc. Natl. Acad. Sci. USA 2017, 114, E10578–E10585. [Google Scholar] [CrossRef]
- Nickles, D.; Abschuetz, A.; Zimmer, H.; Kees, T.; Geibig, R.; Spiess, E.; Régnier-Vigouroux, A. End-Stage Dying Glioma Cells Are Engulfed by Mouse Microglia with a Strain-Dependent Efficacy. J. Neuroimmunol. 2008, 197, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Kees, T.; Lohr, J.; Noack, J.; Mora, R.; Gdynia, G.; Tödt, G.; Ernst, A.; Radlwimmer, B.; Falk, C.S.; Herold-Mende, C.; et al. Microglia Isolated from Patients with Glioma Gain Antitumor Activities on Poly (I:C) Stimulation. Neuro Oncol. 2012, 14, 64–78. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-J.; Park, J.H.; Kim, H.C.; Kim, C.W.; Kang, I.; Lee, H.K. Blood Monocyte-Derived CD169+ Macrophages Contribute to Antitumor Immunity against Glioblastoma. Nat. Commun. 2022, 13, 6211. [Google Scholar] [CrossRef] [PubMed]
- Reiter, I.; Krammer, B.; Schwamberger, G. Cutting Edge: Differential Effect of Apoptotic versus Necrotic Tumor Cells on Macrophage Antitumor Activities. J. Immunol. 1999, 163, 1730–1732. [Google Scholar] [CrossRef]
- Wu, M.; Wu, L.; Wu, W.; Zhu, M.; Li, J.; Wang, Z.; Li, J.; Ding, R.; Liang, Y.; Li, L.; et al. Phagocytosis of Glioma Cells Enhances the Immunosuppressive Phenotype of Bone Marrow-Derived Macrophages. Cancer Res. 2023, 83, 771–785. [Google Scholar] [CrossRef]
- Nylandsted, J.; Wick, W.; Hirt, U.A.; Brand, K.; Rohde, M.; Leist, M.; Weller, M.; Jäättelä, M. Eradication of Glioblastoma, and Breast and Colon Carcinoma Xenografts by Hsp70 Depletion. Cancer Res. 2002, 62, 7139–7142. [Google Scholar]
- Zhang, X.; Chen, W.; Fan, J.; Wang, S.; Xian, Z.; Luan, J.; Li, Y.; Wang, Y.; Nan, Y.; Luo, M.; et al. Disrupting CD47-SIRPα Axis Alone or Combined with Autophagy Depletion for the Therapy of Glioblastoma. Carcinogenesis 2018, 39, 689–699. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.T.; Brown, E.J.; Huang, E.J.; Seaman, W.E. Expression and Activation of Signal Regulatory Protein α on Astrocytomas. Cancer Res. 2004, 64, 117–127. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, R.P.; Chandra Sekhar, Y.B.V.K.; Panigrahi, M.; Babu, P.P. SIRP Alpha Protein Downregulates in Human Astrocytoma: Presumptive Involvement of Hsa-MiR-520d-5p and Hsa-MiR-520d-3p. Mol. Neurobiol. 2017, 54, 8162–8169. [Google Scholar] [CrossRef]
- Price, G.; Bouras, A.; Hambardzumyan, D.; Hadjipanayis, C.G. Current Knowledge on the Immune Microenvironment and Emerging Immunotherapies in Diffuse Midline Glioma. EBioMedicine 2021, 69, 103453. [Google Scholar] [CrossRef] [PubMed]
- Turco, V.; Pfleiderer, K.; Hunger, J.; Horvat, N.K.; Karimian-Jazi, K.; Schregel, K.; Fischer, M.; Brugnara, G.; Jähne, K.; Sturm, V.; et al. T Cell-Independent Eradication of Experimental Glioma by Intravenous TLR7/8-Agonist-Loaded Nanoparticles. Nat. Commun. 2023, 14, 771. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Zhang, Q.; Lubas, M.; Yuan, Y.; Yalcin, F.; Efe, I.E.; Xia, P.; Motta, E.; Buonfiglioli, A.; Lehnardt, S.; et al. Synergistic Toll-like Receptor 3/9 Signaling Affects Properties and Impairs Glioma-Promoting Activity of Microglia. J. Neurosci. 2020, 40, 6428–6443. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Guo, Y.; Chen, L.; Zhang, X.; Wu, W.; Yang, Z.; Li, X.; Wang, Y.; Hu, Z.; Wang, Z. Co-Delivery of Phagocytosis Checkpoint and STING Agonist by a Trojan Horse Nanocapsule for Orthotopic Glioma Immunotherapy. Theranostics 2022, 12, 5488–5503. [Google Scholar] [CrossRef]
- Jadus, M.R.; Irwin, M.C.; Irwin, M.R.; Horansky, R.D.; Sekhon, S.; Pepper, K.; Kohn, D.B.; Wepsic, H.T. Macrophages Can Recognize and Kill Tumor Cells Bearing the Membrane Isoform of Macrophage Colony-Stimulating Factor. Blood 1996, 87, 5232–5241. [Google Scholar] [CrossRef]
- Jadus, M.R.; Williams, C.C.; Avina, M.D.; Ly, M.; Kim, S.; Liu, Y.; Narasaki, R.; Lowell, C.A.; Wepsic, H.T. Macrophages Kill T9 Glioma Tumor Cells Bearing the Membrane Isoform of Macrophage Colony Stimulating Factor through a Phagocytosis-Dependent Pathway. J. Immunol. 1998, 160, 361–368. [Google Scholar] [CrossRef]
- Jadus, M.R.; Chen, Y.; Boldaji, M.T.; Delgado, C.; Sanchez, R.; Douglass, T.; Al-Atar, U.; Schulz, W.; Lloyd, C.; Wepsic, H.T. Human U251MG Glioma Cells Expressing the Membrane Form of Macrophage Colony-Stimulating Factor (MM-CSF) Are Killed by Human Monocytes in Vitro and Are Rejected within Immunodeficient Mice via Paraptosis That Is Associated with Increased Expression of Thre. Cancer Gene Ther. 2003, 10, 411–420. [Google Scholar] [CrossRef]
- Zhai, K.; Huang, Z.; Huang, Q.; Tao, W.; Fang, X.; Zhang, A.; Li, X.; Stark, G.R.; Hamilton, T.A.; Bao, S. Pharmacological Inhibition of BACE1 Suppresses Glioblastoma Growth by Stimulating Macrophage Phagocytosis of Tumor Cells. Nat. Cancer 2021, 2, 1136–1151. [Google Scholar] [CrossRef]
- Lu, J.; Wang, Z.; He, Z.; Hu, Y.; Duan, H.; Liu, Z.; Li, D.; Zhong, S.; Ren, J.; Zhao, G.; et al. Oligomer-Aβ42 Suppress Glioma Progression via Potentiating Phagocytosis of Microglia. CNS Neurosci. Ther. 2024, 30, e14495. [Google Scholar] [CrossRef]
- Sun, R.; Han, R.; McCornack, C.; Khan, S.; Tabor, G.T.; Chen, Y.; Hou, J.; Jiang, H.; Schoch, K.M.; Mao, D.D.; et al. TREM2 Inhibition Triggers Antitumor Cell Activity of Myeloid Cells in Glioblastoma. Sci. Adv. 2023, 9, eade3559. [Google Scholar] [CrossRef] [PubMed]
- Kopatz, J.; Beutner, C.; Welle, K.; Bodea, L.G.; Reinhardt, J.; Claude, J.; Linnartz-Gerlach, B.; Neumann, H. Siglec-h on Activated Microglia for Recognition and Engulfment of Glioma Cells. Glia 2013, 61, 1122–1133. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, A.S.G.; Van Den Berg, T.K.; Mullen, G.E.D. Sialoadhesin—A Macrophage-Restricted Marker of Immunoregulation and Inflammation. Immunology 2013, 138, 198–207. [Google Scholar] [CrossRef]
- Angata, T.; Varki, A. Discovery, Classification, Evolution and Diversity of Siglecs. Mol. Aspects Med. 2023, 90, 101117. [Google Scholar] [CrossRef]
- Chen, Q.; Chen, B.; Wang, C.; Hu, L.; Wu, Q.; Zhu, Y.; Zhang, Q. Dynamic Change in Siglec-15 Expression in Peritumoral Macrophages Confers an Immunosuppressive Microenvironment and Poor Outcome in Glioma. Front. Immunol. 2023, 14, 1159085. [Google Scholar] [CrossRef]
- Zhu, H.; Leiss, L.; Yang, N.; Rygh, C.B.; Mitra, S.S.; Cheshier, S.H.; Weissman, I.L.; Huang, B.; Miletic, H.; Bjerkvig, R.; et al. Surgical Debulking Promotes Recruitment of Macrophages and Triggers Glioblastoma Phagocytosis in Combination with CD47 Blocking Immunotherapy. Oncotarget 2017, 8, 12145–12157. [Google Scholar] [CrossRef]
- Zhang, M.; Hutter, G.; Kahn, S.A.; Azad, T.D.; Gholamin, S.; Xu, C.Y.; Liu, J.; Achrol, A.S.; Richard, C.; Sommerkamp, P.; et al. Anti-CD47 Treatment Stimulates Phagocytosis of Glioblastoma by M1 and M2 Polarized Macrophages and Promotes M1 Polarized Macrophages In Vivo. PLoS ONE 2016, 11, e0153550. [Google Scholar] [CrossRef]
- Gholamin, S.; Youssef, O.A.; Rafat, M.; Esparza, R.; Kahn, S.; Shahin, M.; Giaccia, A.J.; Graves, E.E.; Weissman, I.; Mitra, S.; et al. Irradiation or Temozolomide Chemotherapy Enhances Anti-CD47 Treatment of Glioblastoma. Innate Immun. 2020, 26, 130–137. [Google Scholar] [CrossRef]
- von Roemeling, C.A.; Wang, Y.; Qie, Y.; Yuan, H.; Zhao, H.; Liu, X.; Yang, Z.; Yang, M.; Deng, W.; Bruno, K.A.; et al. Therapeutic Modulation of Phagocytosis in Glioblastoma Can Activate Both Innate and Adaptive Antitumour Immunity. Nat. Commun. 2020, 11, 1508. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wang, S.; Nan, Y.; Fan, J.; Chen, W.; Luan, J.; Wang, Y.; Liang, Y.; Li, S.; Tian, W.; et al. Inhibition of Autophagy Potentiated the Anti-Tumor Effects of VEGF and CD47 Bispecific Therapy in Glioblastoma. Appl. Microbiol. Biotechnol. 2018, 102, 6503–6513. [Google Scholar] [CrossRef] [PubMed]
- Xu, B.; Tian, L.; Chen, J.; Wang, J.; Ma, R.; Dong, W.; Li, A.; Zhang, J.; Antonio Chiocca, E.; Kaur, B.; et al. An Oncolytic Virus Expressing a Full-Length Antibody Enhances Antitumor Innate Immune Response to Glioblastoma. Nat. Commun. 2021, 12, 5908. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Zhang, H.; Wang, D.; Wang, J.; Zhou, J.; Zhang, Z.; Wang, J.; Hu, Y.; Xu, Q.; Xie, C.; et al. Hydrogel Loading Functionalized PAMAM/ShRNA Complex for Postsurgical Glioblastoma Treatment. J. Control. Release 2021, 338, 583–592. [Google Scholar] [CrossRef] [PubMed]
- Ye, L.; Lv, W.; He, W.; Li, S.; Min, Z.; Gong, L.; Zhang, Q.; Teng, C.; Sun, S.; Lv, L.; et al. Reduced Malignant Glioblastoma Recurrence Post-Resection through the Anti-CD47 Antibody and Temozolomide Co-Embedded in-Situ Hydrogel System. J. Control Release 2023, 359, 224–233. [Google Scholar] [CrossRef]
- Tsai, R.K.; Discher, D.E. Inhibition of “Self” Engulfment through Deactivation of Myosin-II at the Phagocytic Synapse between Human Cells. J. Cell Biol. 2008, 180, 989–1003. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Jiang, P.; Xu, Z.; Ye, H. Opportunities and Challenges for Anti-CD47 Antibodies in Hematological Malignancies. Front. Immunol. 2024, 15, 1348852. [Google Scholar] [CrossRef] [PubMed]
- Piccione, E.C.; Juarez, S.; Tseng, S.; Liu, J.; Stafford, M.; Narayanan, C.; Wang, L.; Weiskopf, K.; Majeti, R. SIRPα-Antibody Fusion Proteins Selectively Bind and Eliminate Dual Antigen-Expressing Tumor Cells. Clin. Cancer Res. 2016, 22, 5109–5119. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Li, S.; Chen, D.; Liu, D.; Guo, H.; Yang, C.; Zhang, W.; Zhang, L.; Zhao, G.; Tu, X.; et al. SIRPα-Fc Fusion Protein IMM01 Exhibits Dual Anti-Tumor Activities by Targeting CD47/SIRPα Signal Pathway via Blocking the “Don’t Eat Me” Signal and Activating the “Eat Me” Signal. J. Hematol. Oncol. 2022, 15, 2–5. [Google Scholar] [CrossRef]
- Shimu, A.S.; Wei, H.; Li, Q.; Zheng, X.; Li, B. The New Progress in Cancer Immunotherapy. Clin. Exp. Med. 2022, 23, 553–567. [Google Scholar] [CrossRef]
- Marquardt, V.; Theruvath, J.; Pauck, D.; Picard, D.; Qin, N.; Blümel, L.; Maue, M.; Bartl, J.; Ahmadov, U.; Langini, M.; et al. Tacedinaline (CI-994), a Class I HDAC Inhibitor, Targets Intrinsic Tumor Growth and Leptomeningeal Dissemination in MYC-Driven Medulloblastoma While Making Them Susceptible to Anti-CD47-Induced Macrophage Phagocytosis via NF-ΚB-TGM2 Driven Tumor Inflammat. J. Immunother. Cancer 2023, 11, e005871. [Google Scholar] [CrossRef]
- Tu, J.; Fang, Y.; Han, D.; Tan, X.; Xu, Z.; Jiang, H.; Wang, X.; Hong, W.; Wei, W. MicroRNA-22 Represses Glioma Development via Activation of Macrophage-Mediated Innate and Adaptive Immune Responses. Oncogene 2022, 41, 2444–2457. [Google Scholar] [CrossRef]
- Wu, R.; Sun, C.; Chen, X.; Yang, R.; Luan, Y.; Zhao, X.; Yu, P.; Luo, R.; Hou, Y.; Tian, R.; et al. NSUN5/TET2-Directed Chromatin-Associated RNA Modification of 5-Methylcytosine to 5-Hydroxymethylcytosine Governs Glioma Immune Evasion. Proc. Natl. Acad. Sci. USA 2024, 121, e2321611121. [Google Scholar] [CrossRef] [PubMed]
- Sick, E.; Boukhari, A.; Deramaudt, T.; Rondé, P.; Bucher, B.; André, P.; Gies, J.P.; Takeda, K. Activation of CD47 Receptors Causes Proliferation of Human Astrocytoma but Not Normal Astrocytes via an Akt-Dependent Pathway. Glia 2011, 59, 308–319. [Google Scholar] [CrossRef]
- Liu, X.; Wu, X.; Wang, Y.; Li, Y.; Chen, X.; Yang, W.; Jiang, L. CD47 Promotes Human Glioblastoma Invasion through Activation of the PI3K/Akt Pathway. Oncol. Res. 2019, 27, 415–422. [Google Scholar] [CrossRef]
- Daubon, T.; Léon, C.; Clarke, K.; Andrique, L.; Salabert, L.; Darbo, E.; Pineau, R.; Guérit, S.; Maitre, M.; Dedieu, S.; et al. Deciphering the Complex Role of Thrombospondin-1 in Glioblastoma Development. Nat. Commun. 2019, 10, 1146. [Google Scholar] [CrossRef] [PubMed]
- Ma, D.; Liu, S.; Lal, B.; Wei, S.; Wang, S.; Zhan, D.; Zhang, H.; Lee, R.S.; Gao, P.; Lopez-Bertoni, H.; et al. Extracellular Matrix Protein Tenascin C Increases Phagocytosis Mediated by CD47 Loss of Function in Glioblastoma. Cancer Res. 2019, 79, 2697–2708. [Google Scholar] [CrossRef]
- Gao, X.; McDonald, J.T.; Hlatky, L.; Enderling, H. Acute and Fractionated Irradiation Differentially Modulate Glioma Stem Cell Division Kinetics. Cancer Res. 2013, 73, 1481–1490. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Lv, B.; Liu, Y.; Hua, T.; Han, J.; Sun, C.; Xu, L.; Zhang, Z.; Feng, Z.; Cai, Y.; et al. Blocking the CD47-SIRPα Axis by Delivery of Anti-CD47 Antibody Induces Antitumor Effects in Glioma and Glioma Stem Cells. Oncoimmunology 2018, 7, e1391973. [Google Scholar] [CrossRef]
- Sun, T.; Liu, B.; Cao, Y.; Li, Y.; Cai, L.; Yang, W. AMPK-Mediated CD47 H3K4 Methylation Promotes Phagocytosis Evasion of Glioma Stem Cells Post-Radiotherapy. Cancer Lett. 2024, 583, 216605. [Google Scholar] [CrossRef]
- Affronti, H.C.; Wellen, K.E. Epigenetic Control of Fatty-Acid Metabolism Sustains Glioma Stem Cells. Cancer Discov. 2019, 9, 1161–1163. [Google Scholar] [CrossRef] [PubMed]
- Jiang, N.; Xie, B.; Xiao, W.; Fan, M.; Xu, S.; Duan, Y.; Hamsafar, Y.; Evans, A.C.; Huang, J.; Zhou, W.; et al. Fatty Acid Oxidation Fuels Glioblastoma Radioresistance with CD47-Mediated Immune Evasion. Nat. Commun. 2022, 13, 1511. [Google Scholar] [CrossRef]
- Simion, C.; Cedano-Prieto, M.E.; Sweeney, C. The LRIG Family: Enigmatic Regulators of Growth Factor Receptor Signaling. Endocr. Relat. Cancer 2014, 21, R431–R443. [Google Scholar] [CrossRef]
- Mao, F.; Wang, B.; Xiao, Q.; Cheng, F.; Lei, T.; Guo, D. LRIG Proteins in Glioma: Functional Roles, Molecular Mechanisms, and Potential Clinical Implications. J. Neurol. Sci. 2017, 383, 56–60. [Google Scholar] [CrossRef] [PubMed]
- Xie, R.; Yang, H.; Xiao, Q.; Mao, F.; Zhang, S.; Ye, F.; Wan, F.; Wang, B.; Lei, T.; Guo, D. Downregulation of LRIG1 Expression by RNA Interference Promotes the Aggressive Properties of Glioma Cells via EGFR/Akt/c-Myc Activation. Oncol. Rep. 2013, 29, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Rondahl, V.; Holmlund, C.; Karlsson, T.; Wang, B.; Faraz, M.; Henriksson, R.; Hedman, H. Lrig2-Deficient Mice Are Protected against PDGFB-Induced Glioma. PLoS ONE 2013, 8, e73635. [Google Scholar] [CrossRef]
- Hu, J.; Dong, F.; He, Y.; Xia, X.; Cheng, F.; Chen, S.; Hou, X.; Zhang, P.; Liu, G.; Li, Y.; et al. LRIG2 Promotes Glioblastoma Progression by Modulating Innate Antitumor Immunity through Macrophage Infiltration and Polarization. J. Immunother. Cancer 2022, 10, e004452. [Google Scholar] [CrossRef] [PubMed]
- Gowda, P.; Patrick, S.; Singh, A.; Sheikh, T.; Sen, E. Mutant Isocitrate Dehydrogenase 1 Disrupts PKM2-β-Catenin-BRG1 Transcriptional Network-Driven CD47 Expression. Mol. Cell. Biol. 2018, 38, e00001-18. [Google Scholar] [CrossRef]
- de Groot, J.F.; Gilbert, M.R.; Aldape, K.; Hess, K.R.; Hanna, T.; Ictech, S.; Groves, M.D.; Conrad, C.; Colman, H.; Puduvalli, V.K.; et al. Phase II Study of Carboplatin and Erlotinib (Tarceva, OSI-774) in Patients with Recurrent Glioblastoma. J. Neurooncol. 2008, 90, 89–97. [Google Scholar] [CrossRef]
- Du, L.; Su, Z.; Wang, S.; Meng, Y.; Xiao, F.; Xu, D.; Li, X.; Qian, X.; Lee, S.B.; Lee, J.-H.; et al. EGFR-Induced and c-Src-Mediated CD47 Phosphorylation Inhibits TRIM21-Dependent Polyubiquitylation and Degradation of CD47 to Promote Tumor Immune Evasion. Adv. Sci. 2023, 10, e2206380. [Google Scholar] [CrossRef]
- Stanley, E.R.; Chitu, V. CSF-1 Receptor Signaling in Myeloid Cells. Cold Spring Harb. Perspect. Biol. 2014, 6, a021857. [Google Scholar] [CrossRef]
- Guerriero, J.L. Macrophages: The Road Less Traveled, Changing Anticancer Therapy. Trends Mol. Med. 2018, 24, 472–489. [Google Scholar] [CrossRef]
- Ulland, T.K.; Wang, Y.; Colonna, M. Regulation of Microglial Survival and Proliferation in Health and Diseases. Semin. Immunol. 2015, 27, 410–415. [Google Scholar] [CrossRef]
- Di Nunno, V.; Aprile, M.; Gatto, L.; Tosoni, A.; Ranieri, L.; Bartolini, S.; Franceschi, E. Tumor Microenvironment in Gliomas: A Treatment Hurdle or an Opportunity to Grab? Cancers 2023, 15, 1042. [Google Scholar] [CrossRef]
- Condeelis, J.; Pollard, J.W. Macrophages: Obligate Partners for Tumor Cell Migration, Invasion, and Metastasis. Cell 2006, 124, 263–266. [Google Scholar] [CrossRef]
- Cannarile, M.A.; Weisser, M.; Jacob, W.; Jegg, A.-M.; Ries, C.H.; Rüttinger, D. Colony-Stimulating Factor 1 Receptor (CSF1R) Inhibitors in Cancer Therapy. J. Immunother. Cancer 2017, 5, 53. [Google Scholar] [CrossRef]
- Coniglio, S.J.; Segall, J.E. Microglial-Stimulation of Glioma Invasion Involves the EGFR Ligand Amphiregulin. PLoS ONE 2021, 16, e0260252. [Google Scholar] [CrossRef]
- Zeren, N.; Afzal, Z.; Morgan, S.; Marshall, G.; Uppiliappan, M.; Merritt, J.; Coniglio, S.J. The Chemokine Receptor CCR1 Mediates Microglia Stimulated Glioma Invasion. Int. J. Mol. Sci. 2023, 24, 5136. [Google Scholar] [CrossRef]
- Pyonteck, S.M.; Akkari, L.; Schuhmacher, A.J.; Bowman, R.L.; Sevenich, L.; Quail, D.F.; Olson, O.C.; Quick, M.L.; Huse, J.T.; Teijeiro, V.; et al. CSF-1R Inhibition Alters Macrophage Polarization and Blocks Glioma Progression. Nat. Med. 2013, 19, 1264–1272. [Google Scholar] [CrossRef]
- Rougerie, P.; Miskolci, V.; Cox, D. Generation of Membrane Structures during Phagocytosis and Chemotaxis of Macrophages: Role and Regulation of the Actin Cytoskeleton. Immunol. Rev. 2013, 256, 222–239. [Google Scholar] [CrossRef]
- Fermi, V.; Warta, R.; Wöllner, A.; Lotsch, C.; Jassowicz, L.; Rapp, C.; Knoll, M.; Jungwirth, G.; Jungk, C.; Dao Trong, P.; et al. Effective Reprogramming of Patient-Derived M2-Polarized Glioblastoma-Associated Microglia/Macrophages by Treatment with GW2580. Clin. Cancer Res. 2023, 29, 4685–4697. [Google Scholar] [CrossRef]
- Butowski, N.; Colman, H.; De Groot, J.F.; Omuro, A.M.; Nayak, L.; Wen, P.Y.; Cloughesy, T.F.; Marimuthu, A.; Haidar, S.; Perry, A.; et al. Orally Administered Colony Stimulating Factor 1 Receptor Inhibitor PLX3397 in Recurrent Glioblastoma: An Ivy Foundation Early Phase Clinical Trials Consortium Phase II Study. Neuro Oncol. 2016, 18, 557–564. [Google Scholar] [CrossRef]
- Eda, H.; Zhang, J.; Keith, R.H.; Michener, M.; Beidler, D.R.; Monahan, J.B. Macrophage-Colony Stimulating Factor and Interleukin-34 Induce Chemokines in Human Whole Blood. Cytokine 2010, 52, 215–220. [Google Scholar] [CrossRef]
- Pixley, F.J.; Stanley, E.R. CSF-1 Regulation of the Wandering Macrophage: Complexity in Action. Trends Cell Biol. 2004, 14, 628–638. [Google Scholar] [CrossRef]
- Miners, J.S.; Baig, S.; Palmer, J.; Palmer, L.E.; Kehoe, P.G.; Love, S. Aβ-Degrading Enzymes in Alzheimer’s Disease. Brain Pathol. 2008, 18, 240–252. [Google Scholar] [CrossRef]
- Cappellano, G.; Vecchio, D.; Magistrelli, L.; Clemente, N.; Raineri, D.; Barbero Mazzucca, C.; Virgilio, E.; Dianzani, U.; Chiocchetti, A.; Comi, C. The Yin-Yang of Osteopontin in Nervous System Diseases: Damage versus Repair. Neural Regen. Res. 2021, 16, 1131–1137. [Google Scholar] [CrossRef]
- Peshoff, M.M.; Gupta, P.; Trivedi, R.; Oberai, S.; Chakrapani, P.; Dang, M.; Milam, N.; Maynard, M.E.; Vaillant, B.D.; Huse, J.T.; et al. Triggering Receptor Expressed on Myeloid Cells 2 (TREM2) Regulates Phagocytosis in Glioblastoma. bioRxiv Prepr. Serv. Biol. 2023, 26, 826–839. [Google Scholar] [CrossRef]
- Zheng, J.; Wang, L.; Zhao, S.; Zhang, W.; Chang, Y.; Dheer, A.; Gao, S.; Xu, S.; Ayasoufi, K.; Al-Kharboosh, R.; et al. TREM2 Mediates MHCII-Associated CD4 + T Cell Response against Gliomas. bioRxiv Prepr. Serv. Biol. 2023, 31–41. [Google Scholar] [CrossRef]
- Wolf, E.M.; Fingleton, B.; Hasty, A.H. The Therapeutic Potential of TREM2 in Cancer. Front. Oncol. 2022, 12, 984193. [Google Scholar] [CrossRef]
- Luo, Y.; Pollard, J.W.; Casadevall, A. Fcgamma Receptor Cross-Linking Stimulates Cell Proliferation of Macrophages via the ERK Pathway. J. Biol. Chem. 2010, 285, 4232–4242. [Google Scholar] [CrossRef]
- Gordon, S. Phagocytosis: An Immunobiologic Process. Immunity 2016, 44, 463–475. [Google Scholar] [CrossRef]
- Maverakis, E.; Kim, K.; Shimoda, M.; Gershwin, M.E.; Patel, F.; Wilken, R.; Raychaudhuri, S.; Ruhaak, L.R.; Lebrilla, C.B. Glycans in the Immune System and The Altered Glycan Theory of Autoimmunity: A Critical Review. J. Autoimmun. 2015, 57, 1–13. [Google Scholar] [CrossRef]
- Qin, R.; Mahal, L.K. The Host Glycomic Response to Pathogens. Curr. Opin. Struct. Biol. 2021, 68, 149–156. [Google Scholar] [CrossRef]
- Duan, S.; Paulson, J.C. Siglecs as Immune Cell Checkpoints in Disease. Annu. Rev. Immunol. 2020, 38, 365–395. [Google Scholar] [CrossRef]
- Grabenstein, S.; Barnard, K.N.; Anim, M.; Armoo, A.; Weichert, W.S.; Bertozzi, C.R.; Parrish, C.R.; Willand-Charnley, R. Deacetylated Sialic Acids Modulates Immune Mediated Cytotoxicity via the Sialic Acid-Siglec Pathway. Glycobiology 2021, 31, 1279–1294. [Google Scholar] [CrossRef]
- Imbert, P.R.C.; Saric, A.; Pedram, K.; Bertozzi, C.R.; Grinstein, S.; Freeman, S.A. An Acquired and Endogenous Glycocalyx Forms a Bidirectional “Don’t Eat” and “Don’t Eat Me” Barrier to Phagocytosis. Curr. Biol. 2021, 31, 77–89.e5. [Google Scholar] [CrossRef]
- Boelaars, K.; van Kooyk, Y. Targeting Myeloid Cells for Cancer Immunotherapy: Siglec-7/9/10/15 and Their Ligands. Trends Cancer 2024, 10, 230–241. [Google Scholar] [CrossRef]
- Stanczak, M.A.; Mantuano, N.R.; Kirchhammer, N.; Sanin, D.E.; Jacob, F.; Coelho, R.; Everest-Dass, A.V.; Wang, J.; Trefny, M.P.; Monaco, G.; et al. Targeting Cancer Glycosylation Repolarizes Tumor-Associated Macrophages Allowing Effective Immune Checkpoint Blockade. Sci. Transl. Med. 2022, 14, eabj1270. [Google Scholar] [CrossRef]
- Barkal, A.A.; Brewer, R.E.; Markovic, M.; Kowarsky, M.; Barkal, S.A.; Zaro, B.W.; Krishnan, V.; Hatakeyama, J.; Dorigo, O.; Barkal, L.J.; et al. CD24 Signalling through Macrophage Siglec-10 Is a Target for Cancer Immunotherapy. Nature 2019, 572, 392–396. [Google Scholar] [CrossRef]
- Läubli, H.; Nalle, S.C.; Maslyar, D. Targeting the Siglec-Sialic Acid Immune Axis in Cancer: Current and Future Approaches. Cancer Immunol. Res. 2022, 10, 1423–1432. [Google Scholar] [CrossRef]
- Cordoba, S.; Onuoha, S.; Thomas, S.; Pignataro, D.S.; Hough, R.; Ghorashian, S.; Vora, A.; Bonney, D.; Veys, P.; Rao, K.; et al. CAR T Cells with Dual Targeting of CD19 and CD22 in Pediatric and Young Adult Patients with Relapsed or Refractory B Cell Acute Lymphoblastic Leukemia: A Phase 1 Trial. Nat. Med. 2021, 27, 1797–1805. [Google Scholar] [CrossRef] [PubMed]
- Narayan, R.; Piérola, A.A.; Donnellan, W.B.; Yordi, A.M.; Abdul-Hay, M.; Platzbecker, U.; Subklewe, M.; Kadia, T.M.; Alonso-Domínguez, J.M.; McCloskey, J.; et al. First-in-Human Study of JNJ-67571244, a CD33 × CD3 Bispecific Antibody, in Relapsed/Refractory Acute Myeloid Leukemia and Myelodysplastic Syndrome. Clin. Transl. Sci. 2024, 17, e13742. [Google Scholar] [CrossRef] [PubMed]
- Guijarro-Albaladejo, B.; Marrero-Cepeda, C.; Rodríguez-Arbolí, E.; Sierro-Martínez, B.; Pérez-Simón, J.A.; García-Guerrero, E. Chimeric Antigen Receptor (CAR) Modified T Cells in Acute Myeloid Leukemia: Limitations and Expectations. Front. Cell Dev. Biol. 2024, 12, 1376554. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Peng, W. Recent Progress in Targeting the Sialylated Glycan-SIGLEC Axis in Cancer Immunotherapy. Cancer Biol. Med. 2023, 20, 369–384. [Google Scholar] [CrossRef] [PubMed]
- Ene, C.I.; Ene, C.I.; Kreuser, S.A.; Jung, M.; Jung, M.; Zhang, H.; Arora, S.; White Moyes, K.; Szulzewsky, F.; Barber, J.; et al. Anti-PD-L1 Antibody Direct Activation of Macrophages Contributes to a Radiation-Induced Abscopal Response in Glioblastoma. Neuro Oncol. 2020, 22, 639–651. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Varanasi, S.K.; Hara, T.; Traina, K.; Sun, M.; McDonald, B.; Farsakoglu, Y.; Clanton, J.; Xu, S.; Garcia-Rivera, L.; et al. CTLA-4 Blockade Induces a Microglia-Th1 Cell Partnership That Stimulates Microglia Phagocytosis and Anti-Tumor Function in Glioblastoma. Immunity 2023, 56, 2086–2104.e8. [Google Scholar] [CrossRef] [PubMed]
- Lim, W.A.; June, C.H. The Principles of Engineering Immune Cells to Treat Cancer. Cell 2017, 168, 724–740. [Google Scholar] [CrossRef] [PubMed]
- Luo, C.; Wang, P.; He, S.; Zhu, J.; Shi, Y.; Wang, J. Progress and Prospect of Immunotherapy for Triple-Negative Breast Cancer. Front. Oncol. 2022, 12, 919072. [Google Scholar] [CrossRef]
- Brandt, L.J.B.; Barnkob, M.B.; Michaels, Y.S.; Heiselberg, J.; Barington, T. Emerging Approaches for Regulation and Control of CAR T Cells: A Mini Review. Front. Immunol. 2020, 11, 326. [Google Scholar] [CrossRef]
- Bonte, S.; De Munter, S.; Goetgeluk, G.; Ingels, J.; Pille, M.; Billiet, L.; Taghon, T.; Leclercq, G.; Vandekerckhove, B.; Kerre, T. T-Cells with a Single Tumor Antigen-Specific T-Cell Receptor Can Be Generated in Vitro from Clinically Relevant Stem Cell Sources. Oncoimmunology 2020, 9, 1727078. [Google Scholar] [CrossRef]
- Zhang, D.K.Y.; Adu-Berchie, K.; Iyer, S.; Liu, Y.; Cieri, N.; Brockman, J.M.; Neuberg, D.; Wu, C.J.; Mooney, D.J. Enhancing CAR-T Cell Functionality in a Patient-Specific Manner. Nat. Commun. 2023, 14, 506. [Google Scholar] [CrossRef]
- Sharma, P.; Debinski, W. Receptor-Targeted Glial Brain Tumor Therapies. Int. J. Mol. Sci. 2018, 19, 3326. [Google Scholar] [CrossRef] [PubMed]
- Sloas, C.; Gill, S.; Klichinsky, M. Engineered CAR-Macrophages as Adoptive Immunotherapies for Solid Tumors. Front. Immunol. 2021, 12, 783305. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Yu, Z.; Tan, X.; Jiang, H.; Xu, Z.; Fang, Y.; Han, D.; Hong, W.; Wei, W.; Tu, J. CAR-Macrophage: A New Immunotherapy Candidate against Solid Tumors. Biomed. Pharmacother. 2021, 139, 111605. [Google Scholar] [CrossRef]
- Qu, T.; Li, B.; Wang, Y. Targeting CD47/SIRPα as a Therapeutic Strategy, Where We Are and Where We Are Headed. Biomark. Res. 2022, 10, 20. [Google Scholar] [CrossRef]
- Huo, Y.; Zhang, H.; Sa, L.; Zheng, W.; He, Y.; Lyu, H.; Sun, M.; Zhang, L.; Shan, L.; Yang, A.; et al. M1 Polarization Enhances the Antitumor Activity of Chimeric Antigen Receptor Macrophages in Solid Tumors. J. Transl. Med. 2023, 21, 225. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Jing, W.; Chen, Y.; Wang, G.; Abdalla, M.; Gao, L.; Han, M.; Shi, C.; Li, A.; Sun, P.; et al. Intracavity Generation of Glioma Stem Cell–Specific CAR Macrophages Primes Locoregional Immunity for Postoperative Glioblastoma Therapy. Sci. Transl. Med. 2022, 14, eabn1128. [Google Scholar] [CrossRef]
- Wang, S.; Yang, Y.; Ma, P.; Zha, Y.; Zhang, J.; Lei, A.; Li, N. CAR-Macrophage: An Extensive Immune Enhancer to Fight Cancer. eBioMedicine 2022, 76, 103873. [Google Scholar] [CrossRef]
- Titov, A.; Zmievskaya, E.; Ganeeva, I.; Valiullina, A.; Petukhov, A.; Rakhmatullina, A.; Miftakhova, R.; Fainshtein, M.; Rizvanov, A.; Bulatov, E. Adoptive Immunotherapy beyond CAR T-Cells. Cancers 2021, 13, 743. [Google Scholar] [CrossRef]
- Li, S.Y.; Guo, Y.L.; Tian, J.W.; Zhang, H.J.; Li, R.F.; Gong, P.; Yu, Z.L. Anti-Tumor Strategies by Harnessing the Phagocytosis of Macrophages. Cancers 2023, 15, 2717. [Google Scholar] [CrossRef]
- Flynn, R.A.; Pedram, K.; Malaker, S.A.; Batista, P.J.; Smith, B.A.H.; Johnson, A.G.; George, B.M.; Majzoub, K.; Villalta, P.W.; Carette, J.E.; et al. Small RNAs Are Modified with N-Glycans and Displayed on the Surface of Living Cells. Cell 2021, 184, 3109–3124.e22. [Google Scholar] [CrossRef] [PubMed]
- Pedram, K.; Shon, D.J.; Tender, G.S.; Mantuano, N.R.; Northey, J.J.; Metcalf, K.J.; Wisnovsky, S.P.; Riley, N.M.; Forcina, G.C.; Malaker, S.A.; et al. Design of a Mucin-Selective Protease for Targeted Degradation of Cancer-Associated Mucins. bioRxiv 2022. [Google Scholar] [CrossRef]
| Phagocytic Checkpoint Receptor (on Tumor Associated Macrophage) | Ligand (on GBM Cell) | Summary | References |
|---|---|---|---|
| SIRPa | CD47 | CD47 “don’t eat me signal” engages SIRPa on TAM and prevents phagocytosis | [71,72,73,74,75,76,77] |
| CSF-1R | Membrane CSF-1 | Membrane-bound CSF-1 on GBM cells induces strong phagocytic response in TAMs | [78,79,80] |
| BACE-1 | Beta-amyloid/unknown | Inhibition of BACE-1 enhances TAM mediated phagocytosis of GBM | [81,82] |
| TREM2 | Unknown | TREM2 correlates with enhanced phagocytosis of GBM | [83] |
| Siglec-H/1/15 | Sialic acid modified cell surface proteins | Inhibition of siglec expression on TAMs enhances phagocytosis | [84,85,86,87] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Afzal, A.; Afzal, Z.; Bizink, S.; Davis, A.; Makahleh, S.; Mohamed, Y.; Coniglio, S.J. Phagocytosis Checkpoints in Glioblastoma: CD47 and Beyond. Curr. Issues Mol. Biol. 2024, 46, 7795-7811. https://doi.org/10.3390/cimb46080462
Afzal A, Afzal Z, Bizink S, Davis A, Makahleh S, Mohamed Y, Coniglio SJ. Phagocytosis Checkpoints in Glioblastoma: CD47 and Beyond. Current Issues in Molecular Biology. 2024; 46(8):7795-7811. https://doi.org/10.3390/cimb46080462
Chicago/Turabian StyleAfzal, Amber, Zobia Afzal, Sophia Bizink, Amanda Davis, Sara Makahleh, Yara Mohamed, and Salvatore J. Coniglio. 2024. "Phagocytosis Checkpoints in Glioblastoma: CD47 and Beyond" Current Issues in Molecular Biology 46, no. 8: 7795-7811. https://doi.org/10.3390/cimb46080462
APA StyleAfzal, A., Afzal, Z., Bizink, S., Davis, A., Makahleh, S., Mohamed, Y., & Coniglio, S. J. (2024). Phagocytosis Checkpoints in Glioblastoma: CD47 and Beyond. Current Issues in Molecular Biology, 46(8), 7795-7811. https://doi.org/10.3390/cimb46080462








