Morphometric parameters of the optic disc in normal and glaucomatous eyes based on time-domain optical coherence tomography image analysis
Abstract
:1. Introduction
2. Materials and methods
2.1. Selection and characteristics of patients
2.2. Ophthalmologic examination
2.3. Imaging using TD-OCT and data acquisition
2.4. Data grouping
2.5. Statistical data analysis
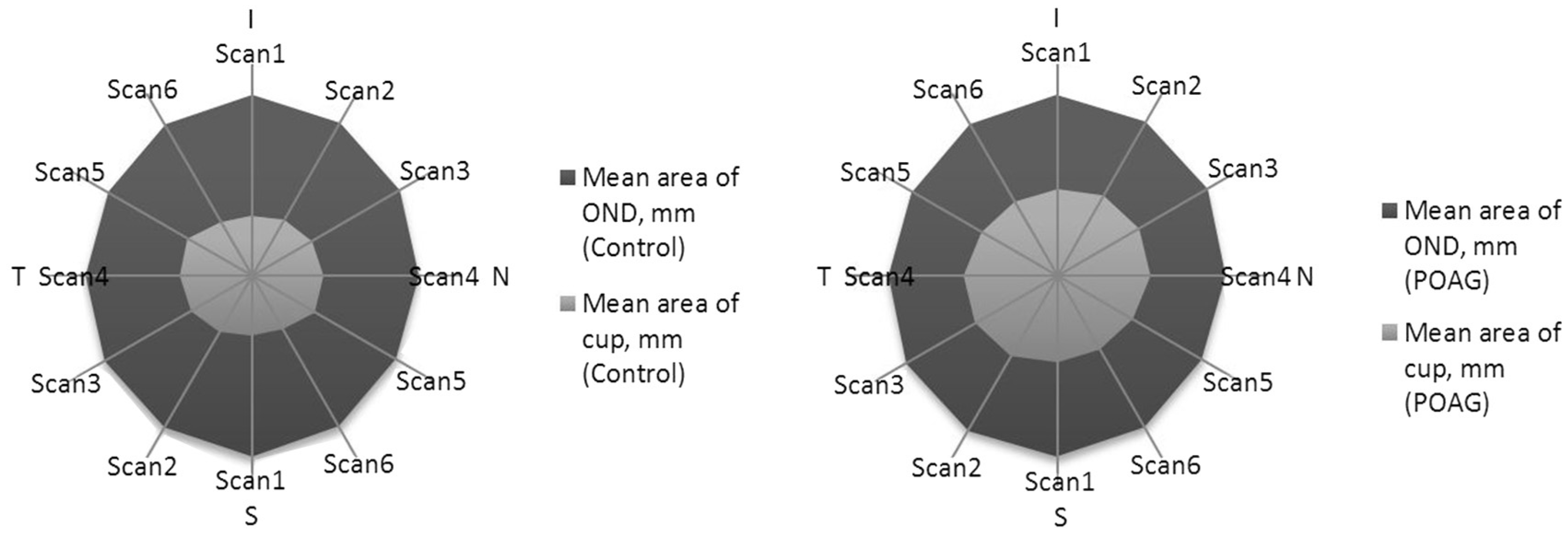
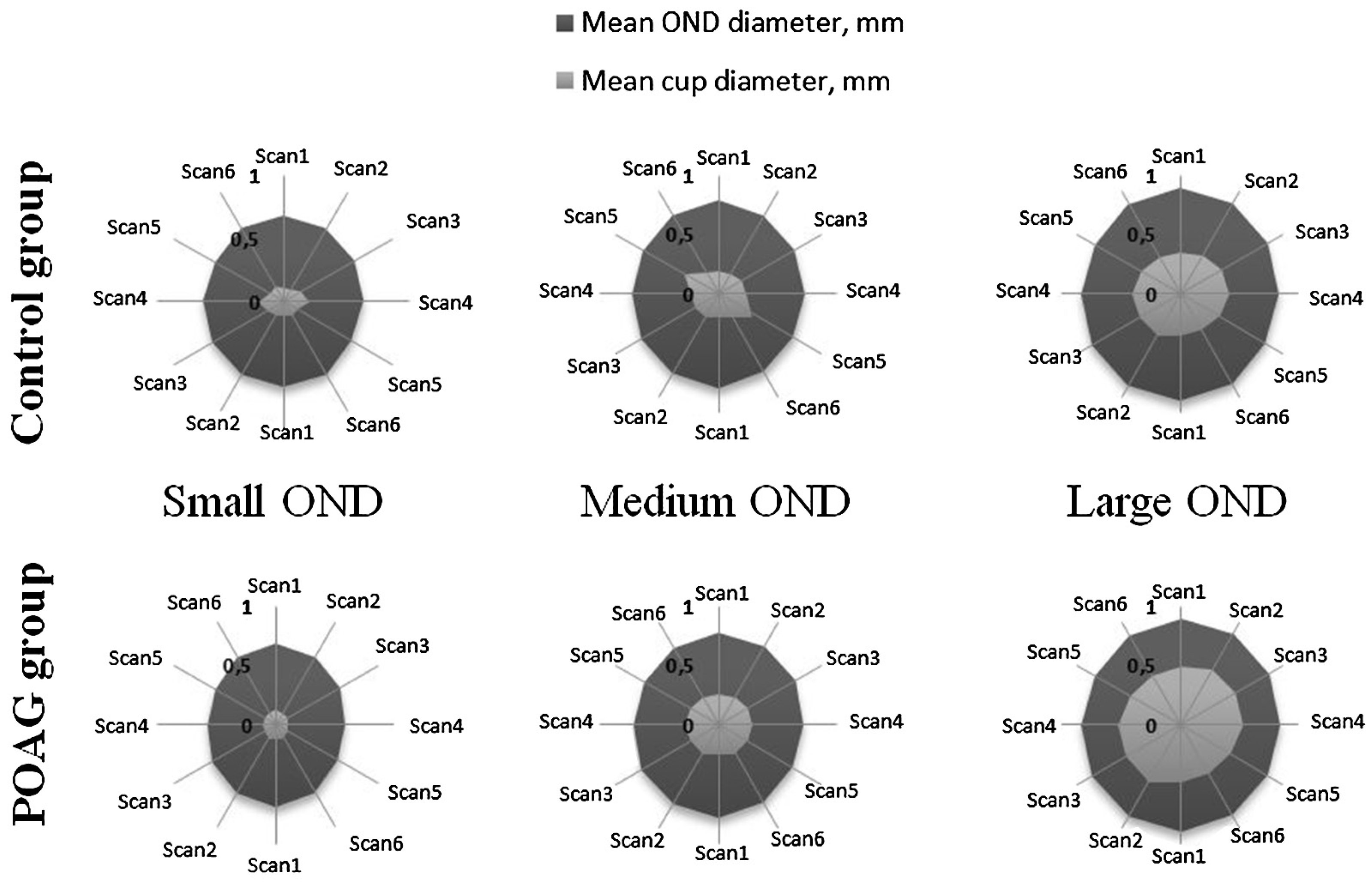
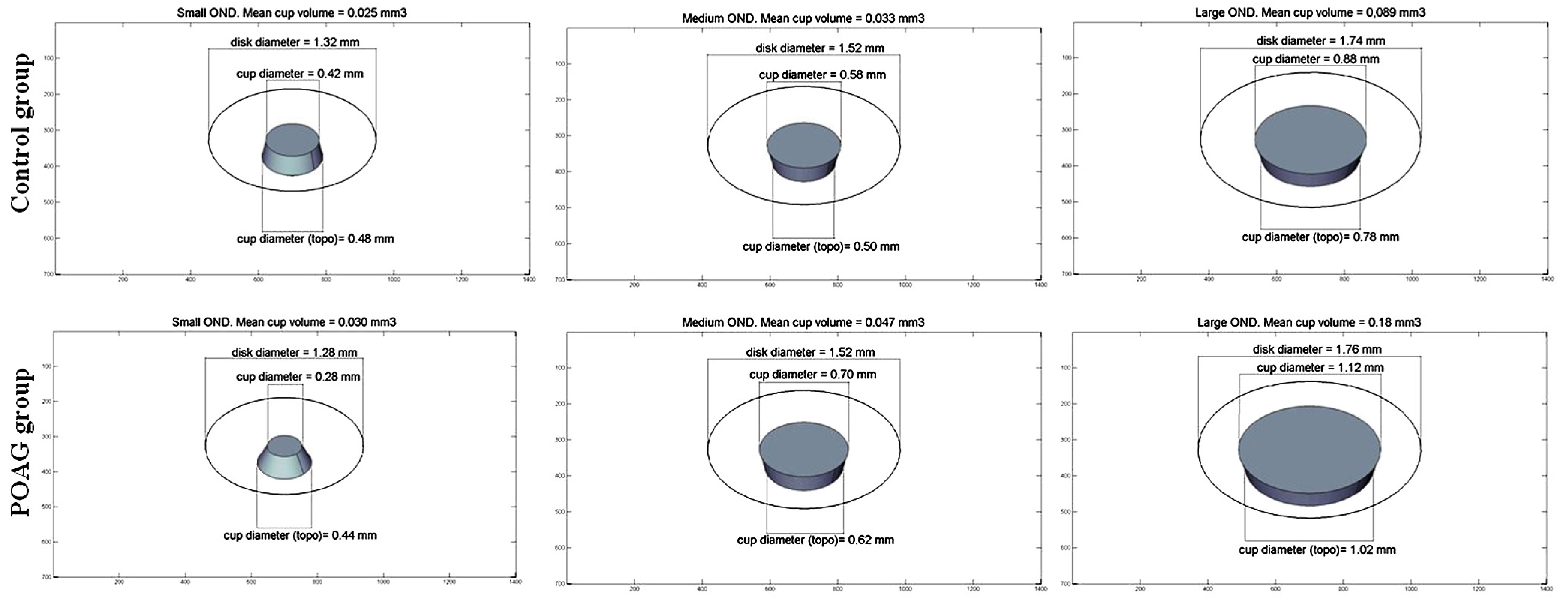
3. Results
4. Discussion
5. Conclusions
Author’ Contributions
Conflicts of Interest
R E F E R E N C E S
- Sanfilippo, PG; Cardini, A; Hewitt, AW; Crowston, JG; Mackey, DA. Optic disc morphology – rethinking shape. Prog Retin Eye Res 2009, 28, 227–48. [Google Scholar] [CrossRef] [PubMed]
- Leung, CK; Chan, W-M; Hui, Y-L; Yung, W-H; Woo, J; Tsang, M-K; et al. Analysis of retinal nerve fiber layer and optic nerve head in glaucoma with different reference plane offsets, using optical coherence tomography. Invest Ophthalmol Vis Sci 2005, 46, 891–9. [Google Scholar] [CrossRef] [PubMed]
- Arvind, H; George, R; Raju, P; Ve, RS; Mani, B; Kannan, P; et al. Neural rim characteristics of healthy south Indians: the Chennai glaucoma study. Invest Ophthalmol Vis Sci 2004, 49, 3457–46. [Google Scholar] [CrossRef] [PubMed]
- Bourne, RR. The optic nerve head in glaucoma. Community Eye Health 2006, 19, 44–5. [Google Scholar] [PubMed]
- Weinreb, RN; Khaw, PT. Primary open-angle glaucoma. Lancet 2004, 363, 1711–20. [Google Scholar] [CrossRef]
- Kwon, YH; Fingert, JH; Kuehn, MH; Alward, WLM. Primary open-angle glaucoma. New Engl J Med 2009, 360, 1113–24. [Google Scholar] [CrossRef] [PubMed]
- Bourne, RR; Foster, PJ; Bunce, C; Peto, T; Hitchings, RA; Khaw, PT; et al. The morphology of the optic nerve head in the Singaporean Chinese population (the TanjongPagar study): part 1 – optic nerve head morphology. Br J Ophthalmol 2009, 92, 303–9. [Google Scholar] [CrossRef] [PubMed]
- Bourne, RR; Foster, PJ; Bunce, C; Peto, T; Hitchings, RA; Khaw, PT; et al. The morphology of the optic nerve head in the Singaporean Chinese population (the Tanjong Pagar study): part 2 – biometric and systemic associations. Br J Ophthalmol 2008, 92, 310–4. [Google Scholar] [CrossRef] [PubMed]
- Garway-Heath, D; Wollstein, G; Hitchings, R. Aging changes of the optic nerve head in relation to open angle glaucoma. Br J Ophthalmol 1997, 81, 840–5. [Google Scholar] [CrossRef] [PubMed]
- Hellström, A; Svensson, E. Optic disc size and retinal vessel characteristics in healthy children. Acta Ophthalmol Scand 1998, 76, 260–7. [Google Scholar]
- Wang, Y; Xu, L; Zhang, L; Yang, H; Ma, Y; Jonas, JB. Optic disc size in a population based study in northern China: the Beijing eye study. Br J Ophthalmol 2006, 90, 353–6. [Google Scholar] [CrossRef] [PubMed]
- Garway-Heath, DF; Hitchings, RA. Quantitative evaluation of the optic nerve head in early glaucoma. Br J Ophthalmol 1998, 82, 352–61. [Google Scholar] [CrossRef] [PubMed]
- Moya, F; Brigatti, L; Caprioli, J. Effect of aging on optic nerve appearance: a longitudinal study. Br J Ophthalmol 1999, 83, 567–72. [Google Scholar] [CrossRef] [PubMed]
- Garway-Heath, D; Ruben, S; Viswanathan, A. Vertical cup/disc ratio in relation to optic disc size: its value in the assessment of the glaucoma suspect. Br J Ophthalmol 1998, 82, 1118–24. [Google Scholar] [CrossRef] [PubMed]
- Samarawickrama, C; Pai, A; Tariq, Y; Healey, PR; Wong, TY; Mitchell, P. Characteristics and appearance of the normal optic nerve head in 6-year-old children. Br J Ophthalmol 2012, 96, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Galloway, RL. The process and development of image-guided procedures. Annu Rev Biomed Eng 2001, 13, 83–108. [Google Scholar] [CrossRef] [PubMed]
- Fujimoto, JG; Pitris, C; Boppart, SA; Brezinski, ME. Optical coherence tomography: an emerging technology for biomedical imaging and optical biopsy. Neoplasia 2000, 2, 9–25. [Google Scholar] [CrossRef] [PubMed]
- Buteikiene, D; Paunksnis, A; Barzdziukas, V; Zaliuniene, D; Balciunienė, JV; Jegelevicius, D. Correlations between digital planimetry and optical coherence tomography, confocal scanning laser ophthalmoscopy in assessment of optic disc parameters. Medicina (Kaunas) 2012, 48, 150–8. [Google Scholar] [CrossRef] [PubMed]
- Mills, RP; Budenz, DL; Lee, PP; Noecker, JR; Siegartel, LR; et al. Categorizing the stage of glaucoma from pre-diagnosis to end-stage disease. Am J Ophthalmol 2006, 1, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Oduntan, OA; Mashige, KP; Raliavhegwa-Makhado, MA. Comparison of two methods of log MAR visual acuity data scoring for statistical analysis. S Afr Optom 2009, 68, 155–63. [Google Scholar]
- Oliveira, C; Harizman, N; Girkin, CA; Xie, A; Tello, C; Liebmann, JM; et al. Axial length and optic disc size in normal eyes. Br J Ophthalmol 2007, 91(1), 37–9. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, EM; Zangwill, LM; Crowston, JG; Weinreb, RN. Optic disk size and glaucoma. Surv Ophthalmol 2007, 52, 32–49. [Google Scholar] [PubMed]
- Manassakorn, A; Ishikawa, H; Kim, JS; Wollstein, G; Bilonick, RA; Kagemann, L; et al. Comparison of optic disc margin identified by color disc photography and high-speed ultrahigh-resolution optical coherence tomography. Arch Ophthalmol 2008, 126, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Kim, JS; Manassakorn, A; Wollstein, G; Bilonick, RA; Kagemann, L; Sung, KR; et al. Comparison of optic disc margin identified by planimetry and high speed ultrahigh-resolution optical coherence tomography (Spectral OCT, SOCT). ARVO’06. Association for Research in Vision and Ophthalmology, 2006; poster 3642-B243. [Google Scholar]
- Choong, YF; Rakebrandt, F; North, RV; Morgan, JE. Acutance, an objective measure of retinal nerve fibre image clarity. Br J Ophthalmol 2003, 87, 322–6. [Google Scholar] [CrossRef] [PubMed]
- Laemmer, R; Schroeder, S; Martus, P; Viestenz, A; Mardin. Quantification of neuroretinal rim loss using digital planimetry in long-term follow-up of normals and patients with ocular hypertension. J Glaucoma 2007, 16, 430–6. [Google Scholar] [CrossRef] [PubMed]
- Mardin, CY; Horn, F; Viestenz, A; mmer R, Jü nemann, A. Healthy optic discs with large cups – a diagnostic challenge in glaucoma. Klin Monbl Augenheilkd 2006, 223, 3080–14. [Google Scholar]
- Jonas, JB; Thomas, R; George, R; Berenshtein, E; Muliyil, J. Optic disc morphology in south India: the Vellore eye study. Br J Ophthalmol 2003, 87, 189–96. [Google Scholar] [CrossRef] [PubMed]


| Characteristic | Group | P | |
|---|---|---|---|
| Control | POAG | ||
| N = 499 | N = 198 | ||
| (n* = 998) | (n* = 394) | ||
| Age, years | 65.3 ± 8.5 | 65.1 ± 9.0 | 0.8 |
| Male/female, % | 38.3/61.7 | 26.8/73.2 | |
| BCVA by Log MAR | 0.15 ± 0.21 | 0.19 ± 0.21 | 0.004 |
| Spherical equivalent of refraction, diopter | 1.03 ± 2.24 | 0.52 ± 2.29 | 0.001 |
| Eye axial length, mm | 23.14 ± 1.24 | 23.2 ± 1.11 | 0.4 |
| Values are mean ± standard deviation unless otherwise indicated. BCVA by Log MAR, best corrected visual acuity by logarithm of the minimum angle of resolution; N, number of subjects; n*, number of eyes. | |||
| Parameter | Control group | P1 | POAG group | P2 | P |
|---|---|---|---|---|---|
| Optic disc area size, mm2 | 2.14 ± 0.39 | 2.19 ± 0.43 | 0.02 | ||
| Age | 0.3 | ||||
| <60 years | 2.10 ± 0.4 | 0.2 | 2.15 ± 0.41 | 0.3*,** | |
| 60–65 years | 2.15 ± 0.35 | 2.21 ± 0.52 | 0.2*** | 0.3 | |
| 66–70 years | 2.12 ± 0.37 | 2.21 ± 0.43 | 0.9****,****** | 0.1 | |
| >70 years | 2.16 ± 0.42 | 2.21 ± 0.41 | 0.2 | ||
| Male | 2.17 ± 0.38 | 0.03 | 2.11 ± 0.40 | 0.02 | 0.2 |
| Female | 2.11 ± 0.40 | 2.22 ± 0.44 | 0.02 | <0.001 | |
| Ocular AL | |||||
| Short | 2.20 ± 0.40 | 0.04* | 2.16 ± 0.36 | 0.06* | 0.4 |
| Medium | 2.14 ± 0.37 | <0.001** | 2.26 ± 0.44 | 0.008** | <0.001 |
| Long | 1.86 ± 0.43 | <0.001*** | 1.97 ± 0.49 | <0.001*** | 0.2 |
| NRR area size, mm2 | 1.60 ± 0.38 | 1.33 ± 0.41 | <0.001 | ||
| Age | |||||
| <60 years | 1.58 ± 0.31 | 0.4 | 1.43 ± 0.37 | 0.05* | <0.001 |
| 60–65 years | 1.64 ± 0.53 | 1.31 ± 0.44 | 0.04** 0.02*** 0.9****,****** | <0.001 | |
| 66–70 years | 1.59 ± 0.33 | 1.30 ± 0.48 | <0.001 | ||
| >70 years | 1.6 ± 0.36 | 1.3 ± 0.37 | <0.001 | ||
| Male | 1.60 ± 0.36 | 0.8 | 1.29 ± 0.43 | 0.2 | <0.001 |
| Female | 1.60 ± 0.40 | 1.35 ± 0.40 | 0.02 | <0.001 | |
| OD | |||||
| Small | 1.18 ± 0.24 | 1.14 ± 0.27 | 0.1–0.7 | 0.7 | |
| Medium | 1.48 ± 0.26 | <0.001*,**,*** | 1.33 ± 0.31 | <0.001 | |
| Large | 1.69 ± 0.36 | 1.35 ± 0.45 | <0.001 | ||
| Ocular AL | |||||
| Short | 1.71 ± 0.39 | 0.001*,**,*** | 1.44 ± 0.40 | 0.01* | <0.001 |
| Medium | 1.59 ± 0.36 | 1.32 ± 0.42 | <0.001** | <0.001 | |
| Long | 1.34 ± 0.4 | 1.16 ± 0.36 | 0.01*** | 0.01 | |
| Cup area size, mm2 | 0.55 ± 0.41 | 0.86 ± 0.58 | <0.001 | ||
| Age | |||||
| <60 years | 0.52 ± 0.37 | 0.3 | 0.72 ± 0.48 | 0.01*, 0.03** | <0.001 |
| 60–65 years | 0.54 ± 0.41 | 0.93 ± 0.65 | 0.01*** | <0.001 | |
| 66–70 years | 0.52 ± 0.38 | 0.91 ± 0.64 | 0.8***,**** | <0.001 | |
| >70 years | 0.58 ± 0.46 | 0.91 ± 0.55 | 0.9****** | <0.001 | |
| Male | 0.58 ± 0.41 | 0.1 | 0.82 ± 0.53 | 0.4 | <0.001 |
| Female | 0.53 ± 0.41 | 0.87 ± 0.60 | <0.001 | ||
| OD | |||||
| Small | 0.21 ± 0.18 | 0.05* | 0.16 ± 0.25 | 0.03* | 0.4 |
| Medium | 0.33 ± 0.26 | <0.001**,*** | 0.46 ± 0.30 | <0.001**,*** | <0.001 |
| Large | 0.69 ± 0.43 | 1.1 ± 0.55 | <0.001 | ||
| Ocular AL | |||||
| Short | 0.52 ± 0.43 | 0.1* 0.9** 0.5*** | 0.72 ± 0.51 | 0.001* 0.4** 0.1*** | <0.001 |
| Medium | 0.56 ± 0.40 | 0.94 ± 0.6 | <0.001 | ||
| Long | 0.53 ± 0.47 | 0.81 ± 0.56 | 0.003 | ||
| Values are mean ± standard deviation. P, between the control and the POAG groups; P1, within the control group; P2, within the POAG group. Multiple comparisons between different age groups: *between <60 and 60–65, **between <60 and 66–70, ***between <60 and >70, ****between 60–65 and 66–70, *****between 60–65 and >70, ******between 66–70 and >70; between different disc area size groups: *between small and medium, **between small and large, ***between medium and large; between different ocular ALs: *between <22.5 mm and 22.5–24.5 mm, **between <22.5 mm and >24.5 mm, ***between 22.5–24.5 mm and >24.5 mm. | |||||
| Scans | Control group | P1 | POAG group | P2 | P |
|---|---|---|---|---|---|
| Scan 1 | |||||
| Cup diameter by age | |||||
| <60 years | 0.58 ± 0.38 | 0.4 | 0.76 ± 0.46 | 0.6 | <0.001 |
| 60–65 years | 0.60 ± 0.43 | 0.86 ± 0.50 | <0.001 | ||
| 66–70 years | 0.52 ± 0.44 | 0.82 ± 0.56 | <0.001 | ||
| >70 years | 0.57 ± 0.46 | 0.84 ± 0.50 | <0.001 | ||
| OD diameter, mm | |||||
| Male | 1.71 ± 0.18 | 0.95 | 1.66 ± 0.17 | <0.001 | 0.024 |
| Female | 1.71 ± 0.20 | 1.74 ± 0.20 | 0.02 | ||
| Cup diameter, mm | |||||
| Male | 0.58 ± 0.44 | 0.72 | 0.77 ± 0.47 | 0.23 | <0.001 |
| Female | 0.57 ± 0.42 | 0.84 ± 0.51 | <0.001 | ||
| Scan 2 | |||||
| Cup diameter by age, mm | |||||
| <60 years | 0.60 ± 0.43 | 0.5 | 0.78 ± 0.48 | 0.1 | <0.001 |
| 60–65 years | 0.63 ± 0.45 | 0.89 ± 0.52 | <0.001 | ||
| 66–70 years | 0.56 ± 0.46 | 0.87 ± 0.57 | <0.001 | ||
| >70 years | 0.62 ± 0.49 | 0.96 ± 0.50 | <0.001 | ||
| OD diameter | |||||
| Male | 1.68 ± 0.18 | 0.50 | 1.65 ± 0.18 | 0.07 | 0.15 |
| Female | 1.67 ± 0.19 | 1.71 ± 0.20 | 0.005 | ||
| Cup diameter | |||||
| Male | 0.62 ± 0.48 | 0.72 | 0.84 ± 0.49 | 0.37 | <0.001 |
| Female | 0.61 ± 0.45 | 0.89 ± 0.53 | <0.001 | ||
| Scan 3 | |||||
| Cup diameter by age, mm | |||||
| <60 years | 0.67 ± 0.42 | 0.8 | 0.82 ± 0.47 | 0.2 | 0.02 |
| 60–65 years | 0.68 ± 0.46 | 0.97 ± 0.48 | <0.001 | ||
| 66–70 years | 0.64 ± 0.43 | 0.86 ± 0.56 | 0.02 | ||
| >70 years | 0.66 ± 0.48 | 0.94 ± 0.48 | <0.001 | ||
| OD diameter, mm | |||||
| Male | 1.64 ± 0.19 | 0.03 | 1.61 ± 0.25 | 0.34 | 0.28 |
| Female | 1.61 ± 0.19 | 1.67 ± 0.20 | <0.001 | ||
| Cup diameter, mm | |||||
| Male | 0.67 ± 0.46 | 0.46 | 0.87 ± 0.48 | 0.49 | <0.001 |
| Female | 0.65 ± 0.44 | 0.91 ± 0.50 | <0.001 | ||
| Scan 4 | |||||
| Cup diameter by age, mm | |||||
| <60 years | 0.69 ± 0.39 | 0.9 | 0.80 ± 0.42 | 0.1 | 0.01 |
| 60–65 years | 0.67 ± 0.42 | 0.95 ± 0.48 | <0.001 | ||
| 66–70 years | 0.68 ± 0.42 | 0.87 ± 0.53 | 0.05 | ||
| >70 years | 0.68 ± 0.45 | 0.93 ± 0.46 | <0.001 | ||
| OD diameter, mm | |||||
| Male | 1.59 ± 0.19 | 0.05 | 1.58 ± 0.22 | 0.29 | 0.51 |
| Female | 1.57 ± 0.19 | 1.60 ± 0.22 | 0.013 | ||
| Cup diameter, mm | |||||
| Male | 0.70 ± 0.43 | 0.24 | 0.87 ± 0.45 | 0.64 | <0.001 |
| Female | 0.67 ± 0.42 | 0.90 ± 0.48 | <0.001 | ||
| Scan 5 | |||||
| Cup diameter by age, mm | |||||
| <60 years | 0.65 ± 0.37 | 0.6 | 0.76 ± 0.41 | 0.2 | 0.02 |
| 60–65 years | 0.65 ± 0.39 | 0.88 ± 0.48 | <0.001 | ||
| 66–70 years | 0.60 ± 0.40 | 0.86 ± 0.49 | <0.001 | ||
| >70 years | 0.82 ± 3.35 | 0.85 ± 0.42 | 0.91 | ||
| OD diameter, mm | |||||
| Male | 1.59 ± 0.18 | 0.04 | 1.57 ± 0.19 | 0.19 | 0.30 |
| Female | 1.57 ± 0.18 | 1.60 ± 0.20 | 0.013 | ||
| Cup diameter, mm | |||||
| Male | 0.83 ± 3.25 | 0.13 | 0.81 ± 0.40 | 0.59 | 0.96 |
| Female | 0.62 ± 0.39 | 0.84 ± 0.46 | <0.001 | ||
| Scan 6 | |||||
| Cup diameter by age, mm | |||||
| <60 years | 0.60 ± 0.37 | 0.4 | 0.73 ± 0.44 | 0.3 | 0.08 |
| 60–65 years | 0.61 ± 0.40 | 0.84 ± 0.52 | 0.001 | ||
| 66–70 years | 0.54 ± 0.40 | 0.81 ± 0.49 | <0.001 | ||
| >70 years | 0.59 ± 0.42 | 0.84 ± 0.45 | <0.001 | ||
| OD diameter, mm | |||||
| Male | 1.66 ± 0.18 | 0.36 | 1.61 ± 0.19 | 0.003 | 0.10 |
| Female | 1.65 ± 0.19 | 1.68 ± 0.21 | 0.045 | ||
| Cup diameter, mm | |||||
| Male | 0.60 ± 0.40 | 0.45 | 0.76 ± 0.44 | 0.22 | 0.001 |
| Female | 0.58 ± 0.40 | 0.82 ± 0.48 | <0.001 | ||
| Values are mean ± standard deviation. P, between the control and POAG groups; P1, within the control group; P2, within the POAG group (ANOVA). | |||||
© 2017 The Lithuanian University of Health Sciences. Production and hosting by Elsevier Sp. z o.o. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Share and Cite
Buteikienė, D.; Kybartaitė-Žilienė, A.; Kriaučiūnienė, L.; Barzdžiukas, V.; Janulevičienė, I.; Paunksnis, A. Morphometric parameters of the optic disc in normal and glaucomatous eyes based on time-domain optical coherence tomography image analysis. Medicina 2017, 53, 242-252. https://doi.org/10.1016/j.medici.2017.05.007
Buteikienė D, Kybartaitė-Žilienė A, Kriaučiūnienė L, Barzdžiukas V, Janulevičienė I, Paunksnis A. Morphometric parameters of the optic disc in normal and glaucomatous eyes based on time-domain optical coherence tomography image analysis. Medicina. 2017; 53(4):242-252. https://doi.org/10.1016/j.medici.2017.05.007
Chicago/Turabian StyleButeikienė, Dovilė, Asta Kybartaitė-Žilienė, Loresa Kriaučiūnienė, Valerijus Barzdžiukas, Ingrida Janulevičienė, and Alvydas Paunksnis. 2017. "Morphometric parameters of the optic disc in normal and glaucomatous eyes based on time-domain optical coherence tomography image analysis" Medicina 53, no. 4: 242-252. https://doi.org/10.1016/j.medici.2017.05.007
APA StyleButeikienė, D., Kybartaitė-Žilienė, A., Kriaučiūnienė, L., Barzdžiukas, V., Janulevičienė, I., & Paunksnis, A. (2017). Morphometric parameters of the optic disc in normal and glaucomatous eyes based on time-domain optical coherence tomography image analysis. Medicina, 53(4), 242-252. https://doi.org/10.1016/j.medici.2017.05.007




