Does Colchicine Substitute Corticosteroids in Treatment of Idiopathic and Viral Pediatric Pericarditis?
Abstract
1. Background
2. Methods
3. Results
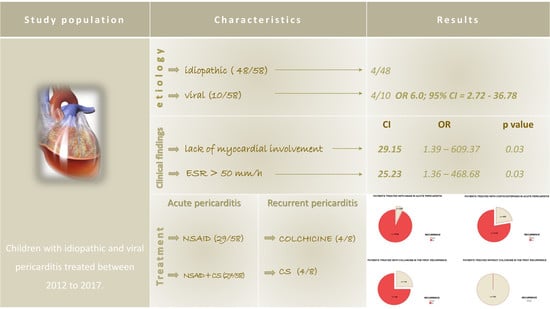
3.1. Aetiology
3.2. Clinical Findings
3.3. Treatment
4. Discussion
4.1. Aetiology
4.2. Treatment
5. Conclusions
Limitations
Author Contributions
Funding
Conflicts of Interest
References
- Geggel, R.L. Conditions Leading to Pediatric Cardiology Consultation in a Tertiary Academic Hospital. Pediatrics 2004, 114, e409–e417. [Google Scholar] [CrossRef] [PubMed]
- Dudzinski, D.M.; Mak, G.S.; Hung, J.W. Pericardial diseases. Curr. Probl. Cardiol. 2012, 37, 75–118. [Google Scholar] [CrossRef] [PubMed]
- Brucato, A.; Valenti, A.; Maisch, B. Acute and Recurrent Pericarditis: Still Idiopathic? J. Am. Coll. Cardiol. 2017, 69, 2775. [Google Scholar] [CrossRef] [PubMed]
- Imazio, M. Idiopathic recurrent pericarditis as an immune-mediated disease: Current insights into pathogenesis and emerging treatment options. Expert Rev. Clin. Immunol. 2014, 10, 1487–1492. [Google Scholar] [CrossRef] [PubMed]
- Imazio, M. Pericarditis: Pathophysiology, Diagnosis, and Management. Curr. Infect. Dis. Rep. 2011, 13, 308–316. [Google Scholar] [CrossRef] [PubMed]
- Ratnapalan, S.; Brown, K.; Benson, L. Children Presenting with Acute Pericarditis to the Emergency Department. Pediatr. Emerg. Care 2011, 27, 581–585. [Google Scholar] [CrossRef]
- Adler, Y.; Charron, P.; Imazio, M.; Badano, L.; Barón-Esquivias, G.; Bogaert, J.; Brucato, A.; Gueret, P.; Klingel, K.; Lionis, C.; et al. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC) Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2015, 36, 2921–2964. [Google Scholar]
- Alabed, S.; Pérez-Gaxiola, G.; Burls, A. Colchicine for children with pericarditis: Systematic review of clinical studies. Arch. Dis. Child. 2016, 101, 953–956. [Google Scholar] [CrossRef]
- Imazio, M.; Brucato, A.; Pluymaekers, N.; Breda, L.; Calabri, G.; Cantarini, L.; Cimaz, R.; Colimodio, F.; Corona, F.; Cumetti, D.; et al. Recurrent pericarditis in children and adolescents: Etiology, presentation, therapies, and out-comes: A multicenter cohort study. J. Cardiovasc. Med. 2016, 17, 707–712. [Google Scholar] [CrossRef]
- Drossner, D.M.; Hirsh, D.A.; Sturm, J.J.; Mahle, W.T.; Goo, D.J.; Massey, R.; Simon, H.K. Cardiac disease in pediatric patients presenting to a pediatric ED with chest pain. Am. J. Emerg. Med. 2011, 29, 632–638. [Google Scholar] [CrossRef]
- Imazio, M.; Brucato, A.; Barbieri, A.; Ferroni, F.; Maestroni, S.; Ligabue, G.; Chinaglia, A.; Cumetti, D.; Casa, G.D.; Bonomi, F.; et al. Good prognosis for pericarditis with and without myocardial involvement: Results from multicentre prospective cohort study. Circulation 2013, 128, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Caforio, A.L.P.; Pankuweit, S.; Arbustini, E.; Basso, C.; Gimeno-Blanes, J.; Felix, S.B.; Fu, M.; Heliö, T.; Heymans, S.; Jahns, R.; et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: A position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur. Hear J. 2013, 34, 2636–2648. [Google Scholar] [CrossRef] [PubMed]
- Gaspari, S.; Marsili, M.; Imazio, M.; Brucato, A.; Cuccio, C.D.B.L.; Chiarelli, F.; Breda, L. New insights in the pathogenesis and therapy of idiopathic recurrent pericarditis in children. Clin. Exp. Rheumatol. 2013, 31, 788–794. [Google Scholar] [PubMed]
- Imazio, M.; Brucato, A.; Trinchero, R.; Spodick, D.; Adler, Y. Individualized therapy for pericarditis. Expert Rev. Cardiovasc. Ther. 2009, 7, 965–975. [Google Scholar] [CrossRef] [PubMed]
- Bolin, E.H.; Tang, X.; Lang, S.M.; Daily, J.A.; Collins, R.T. Characteristics of Non-Postoperative Pediatric Pericardial Effusion: A Multicenter Retrospective Cohort Study from the Pediatric Health Information System. (PHIS). Pediatr. Cardiol. 2018, 39, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Imazio, M.; Brucato, A.; Maestroni, S.; Cumetti, D.; Dominelli, A.; Natale, G.; Trinchero, R. Prevalence of C-reactive protein elevation and time course of normalization in acute pericarditis: Implications for the diagnosis, therapy, and prognosis of pericarditis. Circulation 2011, 123, 1092–1097. [Google Scholar] [CrossRef]
- Finetti, M.; Insalaco, A.; Cantarini, L.; Meini, A.; Breda, L.; Alessio, M.; D’Alessandro, M.; Picco, P.; Martini, A.; Gattorno, M. Long-Term Efficacy of Interleukin-1 Receptor Antagonist (Anakinra) in Corticosteroid-Dependent and Colchicine-Resistant Recurrent Pericarditis. J. Pediatr. 2014, 164, 1425–1431. [Google Scholar] [CrossRef]
- Levy, P.-Y.; Fournier, P.-E.; Charrel, R.; Metras, D.; Habib, G.; Raoult, D. Molecular analysis of pericardial fluid: A 7-year experience. Eur. Hear J. 2006, 27, 1942–1946. [Google Scholar] [CrossRef]
- Gaaloul, I.; Riabi, S.; Harrath, R.; Hunter, T.; Hamda, K.B.; Ghzala, A.B.; Huber, S.; Aouni, M. Coxsackievirus B detection in cases of myocarditis, myopericarditis, pericarditis and dilated cardiomyopathy in hospitalized patients. Mol. Med. Rep. 2014, 10, 2811–2818. [Google Scholar] [CrossRef]
- Horneffer, P.J.; Miller, R.H.; A Pearson, T.; Rykiel, M.F.; A Reitz, B.; Gardner, T.J. The effective treatment of postpericardiotomy syndrome after cardiac operations. A randomized placebo-controlled trial. J. Thorac. Cardiovasc. Surg. 1990, 100, 292–296. [Google Scholar]
- Maisch, B. Task Force on the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology. Guidelines on the diagnosis and management of pericardial diseases executive summary. Eur. Heart J. 2004, 25, 587–610. [Google Scholar] [PubMed]
- Cremer, P.C.; Kumar, A.; Kontzias, A.; Tan, C.D.; Rodriguez, E.R.; Imazio, M.; Klein, A.L. Complicated Pericarditis: Understanding risk factors and pathophysiology to inform imaging and treatment. J. Am. Coll. Cardiol. 2016, 68, 2311–2328. [Google Scholar] [CrossRef] [PubMed]
- Shakti, D.; Hehn, R.; Gauvreau, K.; Sundel, R.P.; Newburger, J.W. Idiopathic Pericarditis and Pericardial Effusion in Children: Contemporary Epidemiology and Management. J. Am. Hear Assoc. 2014, 3, 001483. [Google Scholar] [CrossRef] [PubMed]
- Imazio, M.; Brucato, A.; Adler, Y. A Randomized Trial of Colchicine for Acute Pericarditis. N. Engl. J. Med. 2014, 370, 780–781. [Google Scholar] [CrossRef] [PubMed]
- Mager, A.; Talmor, Y.; Azzerad, C.C.; Iakobishvili, Z.; Porter, A.; Kornowski, R.; Hasdai, D. Does colchicine decrease the rate of recurrence of acute idiopathic pericarditis treated with glucocorticoids? J. Cardiol. 2018, 71, 409–413. [Google Scholar] [CrossRef] [PubMed]
- Raatikka, M.; Pelkonen, P.M.; Karjalainen, J.; Jokinen, E.V. Recurrent pericarditis in children and adolescents: Report of 15 cases. J. Am. Coll. Cardiol. 2003, 42, 759–764. [Google Scholar] [CrossRef]
- Pepi, M.; Muratori, M. Echocardiography in the diagnosis and management of pericardial disease. J. Cardiovasc. Med. 2006, 7, 533–544. [Google Scholar] [CrossRef]
- Imazio, M.; Brucato, A.; DeRosa, F.G.; Lestuzzi, C.; Bombana, E.; Scipione, F.; Leuzzi, S.; Cecchi, E.; Trinchero, R.; Adler, Y. Aetiological diagnosis in acute and recurrent pericarditis: When and how. J. Cardiovasc. Med. 2009, 10, 217–230. [Google Scholar] [CrossRef]
- Imazio, M.; Gaita, F.; LeWinter, M.; Imazio, M.M.; Gaita, M.F.; LeWinter, M.M. Evaluation and Treatment of Pericarditis. JAMA 2015, 314, 1498–1506. [Google Scholar] [CrossRef]
- Artom, G.; Koren-Morag, N.; Spodick, D.H.; Brucato, A.; Guindo, J.; Bayes-De-Luna, A.; Brambilla, G.; Finkelstein, Y.; Granel, B.; Bayes-Genis, A.; et al. Pretreatment with corticosteroids attenuates the efficacy of colchicine in preventing recurrent pericarditis: A multi-centre all-case analysis. Eur. Hear J. 2005, 26, 723–727. [Google Scholar] [CrossRef]
- Assolari, A.; Maestroni, S.; Cumetti, D.; Valenti, A.; Parisi, F.; Brucato, A. Clinical management and therapy of idiopathic recurrent pericarditis. Clin. Manag. Issues 2018, 12. [Google Scholar] [CrossRef]
- Imazio, M.; Belli, R.; Brucato, A.; Cemin, R.; Ferrua, S.; Beqaraj, F.; Demarie, D.; Ferro, S.; Forno, D.; Maestroni, S.; et al. Efficacy and safety of colchicine for treatment of multiple recurrences of pericarditis (CORP-2): A multicentre, double-blind, placebo-controlled, randomised trial. Lancet 2014, 383, 2232–2237. [Google Scholar] [CrossRef]

| Aetiology | Acute Pericarditis-No (%) | First Recurrence-No (%) |
|---|---|---|
| Idiopathic | 46 (82.14) | 4 (50.0) |
| Viral | 10 (17.24) | 4 (50.0) |
| Adeno | 3 | 2 |
| EBV | 3 | 2 |
| Coxsackie Parvo B 19 | 2 | 0 |
| 1 | 0 | |
| Influenza | 1 | 0 |
| Total | 56 (100) | 8 (100) |
| All Patients | Idiopathic Pericarditis | Viral Pericarditis | p Value | |
|---|---|---|---|---|
| CRP (mg/L) | 122.31 ± 56.09 | 114.64 ± 48.29 | 160.67 ± 77.66 | 0.02 |
| ESR (mm/h) | 50.73 ± 18.20 | 48.71 ± 17.36 | 59.80 ± 20.06 | 0.08 |
| WBC (× 109) | 16.33 ± 4.07 | 15.52 ± 3.83 | 19.96 ± 3.12 | 0.001 |
| Fever (C) | 37.47 ± 2.42 | 37.16 ± 2.52 | 38.89 ± 1.20 | 0.04 |
| Aetiology | Treatment of Acute Pericarditis | Number of Patients (No) | Recurrence (No) | p-Value |
|---|---|---|---|---|
| Idiopathic | NSAID | 26 | 0 | 0.03 |
| NSAID + CS | 20 | 4 | ||
| Viral | NSAID | 3 | 2 | 0.5 |
| NSAID + CS | 7 | 2 |
| First Recurrence Treatment | No (%) of Patients with First Recurrence | No of Patients with Additional ROPs | No (Median and IQR) of Additional ROPs |
|---|---|---|---|
| NSAID + COLCHICINE | 4 (50%) | 1/4 | 0 (IQR: 0–0.75) |
| NSAID + CORTICOSTEROID | 4 (50%) | 4/4 * | 5 (IQR: 2–15) |
| Total | 8 (100%) | 5/8 | 1 (IQR: 0–2.5) |
| p Value | OR | CI | |
|---|---|---|---|
| Viral acute pericarditis | 0.01 | 31.46 | 2.24–441.02 |
| Lack of myocardial involvement | 0.03 | 29.15 | 1.39–609.37 |
| Treatment (NSAID + CS) | 0.02 | 29.02 | 1.51–557.21 |
| ESR ≥ 50 mm/L | 0.03 | 25.23 | 1.36–468.86 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vukomanovic, V.; Prijic, S.; Krasic, S.; Borovic, R.; Ninic, S.; Nesic, D.; Bjelakovic, B.; Popovic, S.; Stajević, M.; Petrović, G. Does Colchicine Substitute Corticosteroids in Treatment of Idiopathic and Viral Pediatric Pericarditis? Medicina 2019, 55, 609. https://doi.org/10.3390/medicina55100609
Vukomanovic V, Prijic S, Krasic S, Borovic R, Ninic S, Nesic D, Bjelakovic B, Popovic S, Stajević M, Petrović G. Does Colchicine Substitute Corticosteroids in Treatment of Idiopathic and Viral Pediatric Pericarditis? Medicina. 2019; 55(10):609. https://doi.org/10.3390/medicina55100609
Chicago/Turabian StyleVukomanovic, Vladislav, Sergej Prijic, Stasa Krasic, Ruzica Borovic, Sanja Ninic, Dejan Nesic, Bojko Bjelakovic, Sasa Popovic, Mila Stajević, and Gordana Petrović. 2019. "Does Colchicine Substitute Corticosteroids in Treatment of Idiopathic and Viral Pediatric Pericarditis?" Medicina 55, no. 10: 609. https://doi.org/10.3390/medicina55100609
APA StyleVukomanovic, V., Prijic, S., Krasic, S., Borovic, R., Ninic, S., Nesic, D., Bjelakovic, B., Popovic, S., Stajević, M., & Petrović, G. (2019). Does Colchicine Substitute Corticosteroids in Treatment of Idiopathic and Viral Pediatric Pericarditis? Medicina, 55(10), 609. https://doi.org/10.3390/medicina55100609