Associations of Cardiovascular and All-Cause Mortality with Metabolic Syndrome in Hemodialysis Patients: A Prospective Single-Center Study
Abstract
1. Introduction
2. Materials and Methods
- Abdominal (visceral) obesity: waist circumference ≥102 cm in men and 88 cm in women;
- Fasting hyperglycemia ≥5.6 mmol/L or using diabetes medications;
- Fasting triglycerides ≥1.7 mmol/L or taking triglyceride-lowering agents;
- High-density lipoprotein cholesterol (HDL-C) <1.03 mmol/L for men and <1.29 for women or taking cholesterol-lowering agents; and
- Hypertension (systolic blood pressure ≥130, diastolic blood pressure ≥85) or using antihypertensive medication.
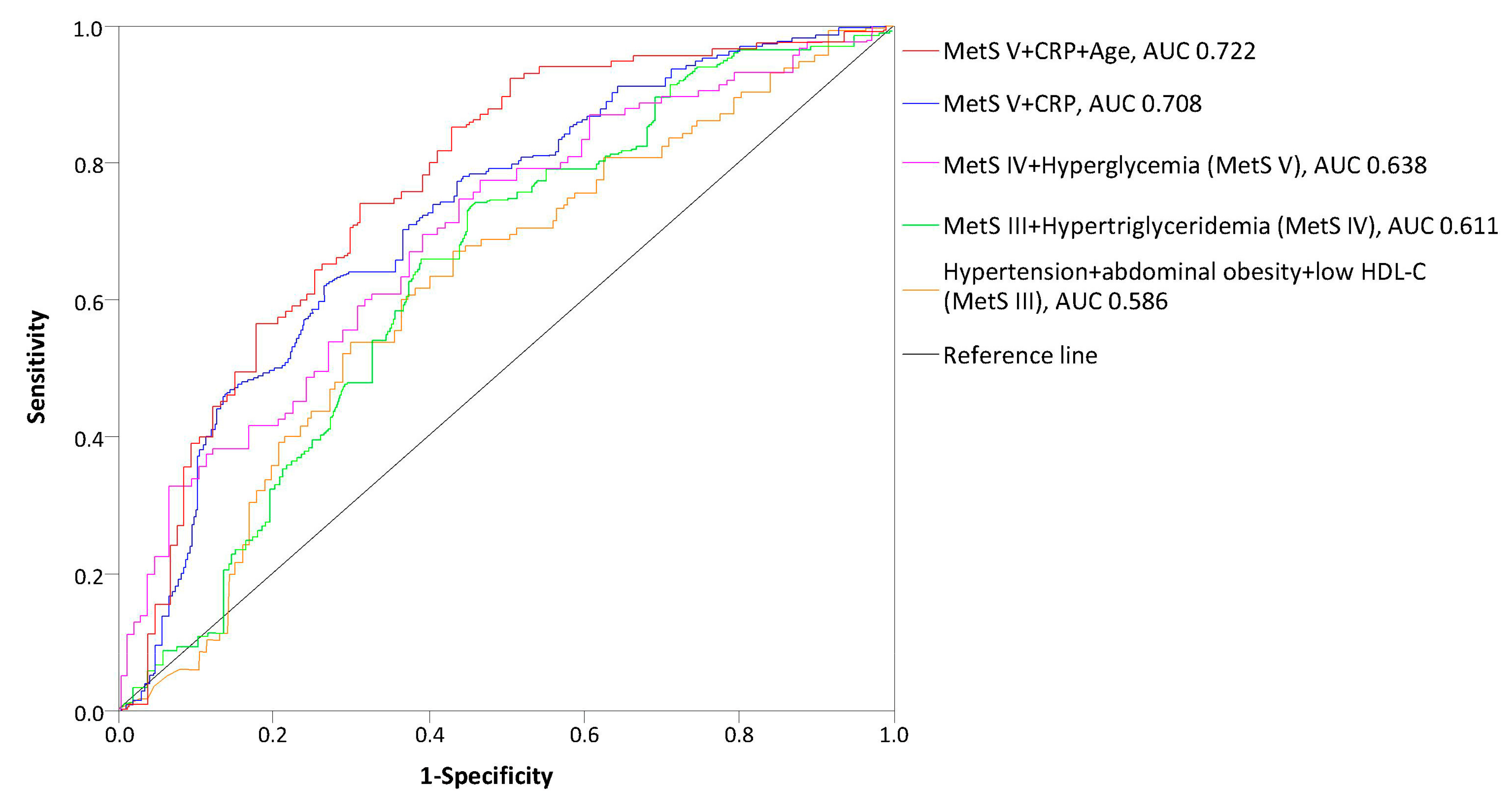
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Shaista, M.; Nathan, D.W.; Stanley, S.F.; Tripthi, V.K.; Gilbert, J.L.; Jose, R.P.; Williams, G.R. Impact of the metabolic syndrome on mortality from coronary heart disease, cardiovascular disease, and all causes in United States adults. Circulation 2004, 110, 1245–1250. [Google Scholar] [CrossRef]
- Harris, M.F. The metabolic syndrome. Aust. Fam. Phys. 2013, 42, 524–527. [Google Scholar]
- National Cholesterol Education Program (NCEP); Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 2002, 106, 3143–3421. [Google Scholar] [CrossRef]
- Alberti, K.G.; Zimmet, P.; Shaw, J. IDF Epidemiology Task Force Consensus Group. The metabolic syndrome—A new worldwide definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef]
- World Health Organization. Definition, Diagnosis and Classification of Diabetes Mellitus and Its Complications: Report of a WHO Consultation. Part 1, Diagnosis and Classification of Diabetes Mellitus; World Health Organization: Geneva, Switzerland, 1999; Available online: http://www.who.int/iris/handle/10665/66040 (accessed on 10 June 2019).
- Chen, J.; Muntner, P.; Hamm, L.L.; Jones, D.W.; Batuman, V.; Fonseca, V.; Whelton, P.K.; He, J. The metabolic syndrome and chronic kidney disease in US adults. Ann. Intern. Med. 2004, 140, 167–174. [Google Scholar] [CrossRef]
- Alswat, K.A.; Althobaiti, A.; Alsaadi, K.; Alkhaldi, A.S.; Alharthi, M.M.; Abuharba, W.A.; Alzaidi, A.A. Prevalence of metabolic syndrome among the end-stage renal disease patients on hemodialysis. J. Clin. Med. Res. 2017, 9, 687–694. [Google Scholar] [CrossRef]
- Townsend, R.R.; Anderson, H.A.; Chen, J.; Gadebegku, C.A.; Fink, J.C.; Go, A.S.; Joffe, M.; Nessel, L.A.; Ojo, A.; Rader, D.J.; et al. Metabolic syndrome, components, and cardiovascular disease prevalence in chronic kidney disease: Findings from the Chronic Renal Insufficiency Cohort (CRIC) Study. Am. J. Nephrol. 2011, 33, 477–484. [Google Scholar] [CrossRef]
- Foley, R.N.; Parfrey, P.S.; Sarnak, M.J. Clinical epidemiology of cardiovascular disease in chronic renal disease. Am. J. Kidney Dis. 1998, 32, S112–S119. [Google Scholar] [CrossRef]
- Sanguankeo, A.; Upala, S. Metabolic syndrome increases mortality risk in dialysis patients: A systematic review and meta-analysis. Int. J. Endocrinol. Metab. 2018, 16, e61201. [Google Scholar] [CrossRef]
- Yang, S.Y.; Chiang, C.K.; Hsu, S.P.; Peng, Y.S.; Pai, M.F.; Ho, T.I.; Hung, K.Y.; Wu, K.D. Metabolic syndrome predicts hospitalization in hemodialysis patients: A prospective Asian cohort study. Blood Purif. 2007, 25, 252–259. [Google Scholar] [CrossRef]
- Xie, Q.; Zhang, A.H.; Chen, S.Y.; Lai, X.; Zhang, F.; He, L.; Zhuang, Z.; Zhu, N.; Fan, M.H.; Wang, T. Metabolic syndrome is associated with better nutritional status, but not with cardiovascular disease or all-cause mortality in patients on haemodialysis. Arch. Cardiovasc. Dis. 2012, 105, 211–217. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wu, C.C.; Liou, H.H.; Su, P.F.; Chang, M.Y.; Wang, H.H.; Chen, M.J.; Hung, S.Y. Abdominal obesity is the most significant metabolic syndrome component predictive of cardiovascular events in chronic hemodialysis patients. Nephrol. Dial. Transplant. 2011, 26, 3689–3695. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Prasad, N.; Sinha, A.; Gupta, A.; Sharma, R.K.; Kaul, A.; Bhadauria, D.; Ranagswamy, D. Effect of metabolic syndrome on clinical outcomes of non-diabetic peritoneal dialysis patients in India. Nephrology 2013, 18, 657–664. [Google Scholar] [CrossRef] [PubMed]
- Park, J.T.; Chang, T.I.; Kim, D.K.; Lee, J.E.; Choi, H.Y.; Kim, H.W.; Chang, J.H.; Park, S.Y.; Kim, E.; Yoo, T.H.; et al. Metabolic syndrome predicts mortality in non-diabetic patients on continuous ambulatory peritoneal dialysis. Nephrol. Dial. Transplant. 2010, 25, 599–604. [Google Scholar] [CrossRef]
- Liao, C.T.; Kao, T.W.; Chou, Y.H.; Wu, M.S.; Chen, Y.M.; Chuang, H.F.; Hung, K.Y.; Chu, T.S.; Wu, K.D.; Tsai, T.J. Associations of metabolic syndrome and its components with cardiovascular outcomes among non-diabetic patients undergoing maintenance peritoneal dialysis. Nephrol. Dial. Transplant. 2011, 26, 4047–4054. [Google Scholar] [CrossRef][Green Version]
- Vogt, B.P.; Souza, P.L.; Minicucci, M.F.; Martin, L.C.; Barretti, P.; Caramori, J.T. Metabolic syndrome criteria as predictors of insulin resistance, inflammation and mortality in chronic hemodialysis patients. Metab. Syndr. Relat. Disord. 2014, 12, 443–449. [Google Scholar] [CrossRef]
- Johnson, D.W.; Armstrong, K.; Campbell, S.B.; Mudge, D.W.; Hawley, C.M.; Coombes, J.S.; Prins, J.B.; Isbel, N.M. Metabolic syndrome in severe chronic kidney disease: Prevalence, predictors, prognostic significance and effects of risk factor modification. Nephrology 2007, 12, 391–398. [Google Scholar] [CrossRef]
- Tsangalis, G.; Papaconstantinou, S.; Kosmadakis, G.; Valis, D.; Zerefos, N. Prevalence of the metabolic syndrome inhemodialysis. Int. J. Artif. Organs 2007, 30, 118–123. [Google Scholar] [CrossRef]
- Tu, S.F.; Chou, Y.C.; Sun, C.A.; Hsueh, S.C.; Yang, T. The prevalence of metabolic syndrome and factors associated with quality of dialysis among hemodialysis patients in Southern Taiwan. Glob. J. Health Sci. 2012, 4, 53–62. [Google Scholar] [CrossRef][Green Version]
- Young, D.O.; Lund, R.J.; Haynatzki, G.; Dunlay, R.W. Prevalence of the metabolic syndrome in an incident dialysis population. Hemodial. Int. 2007, 11, 86–95. [Google Scholar] [CrossRef]
- Sowers, J.R. Insulin resistance and hypertension. Am. J. Physiol. Heart Circ. Physiol. 2004, 286, H1597–H1602. [Google Scholar] [CrossRef] [PubMed]
- Bonet, J.; Martinez-Castelao, A.; Bayés, B. Metabolic syndrome in hemodialysis patients as a risk factor for new-onset diabetes mellitus after renal transplant: A prospective observational study. Diabetes Metab. Syndr. Obes. 2013, 6, 339–346. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kubrusly, M.; de Oliveira, C.M.C.; Simões, P.S.F.; Lima, R.D.O.; Galdino, P.N.R.; Sousa, P.A.F.; Jerônimo, A.L.K. Prevalence of metabolic syndrome according to NCEP-ATP III and IDF criteria in patients on hemodialysis. J. Braz. Nephrol. 2015, 37, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Wellen, K.E.; Hotamisligil, G.S. Obesity-induced inflammatory changes in adipose tissue. J. Clin. Investig. 2003, 112, 1785–1788. [Google Scholar] [CrossRef]
- Ridker, P.M.; Buring, J.E.; Cook, N.R.; Rifai, N. C-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events: An 8-year follow-up of 14,719 initially healthy American women. Circulation 2003, 107, 391–397. [Google Scholar] [CrossRef]
- Clearfield, M.B. C-reactive protein: A new risk assessment tool for cardiovascular disease. J. Am. Osteopath. Assoc. 2005, 105, 409–416. [Google Scholar]
- Song, Y.; Yang, S.K.; Kim, J.; Lee, D.C. Association between C-reactive protein and metabolic syndrome in Korean adults. Korean J. Fam. Med. 2019, 40, 116–123. [Google Scholar] [CrossRef]
- Kawaguchi, T.; Tong, L.; Robinson, B.M.; Sen, A.; Fukuhara, S.; Kurokawa, K.; Canaud, B.; Lameire, N.; Port, F.K.; Pisoni, R.L. C-reactive protein and mortality in hemodialysis patients: The dialysis outcomes and practice patterns study (DOPPS). Nephron Clin. Pract. 2011, 117, 167–178. [Google Scholar] [CrossRef]
- Stolić, R.; Trajković, G.; Perić, V.; Jovanović, A.; Stolić, D.; Sovtić, S.; Subarić-Gorgieva, G. Frequency and characteristics of metabolic disorders in patients on haemodialysis. Vojnosanit. Pregl. 2008, 65, 205–209. [Google Scholar] [CrossRef]
- Chen, J.; Gu, D.; Chen, C.S.; Wu, X.; Lee, H.L.; Muntner, P. Association between the metabolic syndrome and chronic kidney disease in Chinese adults. Nephrol. Dial. Transplant. 2007, 22, 1100–1106. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Kamineni, A.; Prineas, R.J.; Siscovick, D.S. Metabolic syndrome and mortality in older adults: The cardiovascular health study. Arch. Intern. Med. 2008, 168, 969–978. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.D.; Woods, H.F. Insulin resistance, the metabolic syndrome and renal failure—Is there a special problem for patients treated with peritoneal dialysis? Eur. Endocrinol. 2006, 2, 29–32. [Google Scholar] [CrossRef]
- Bakker, S.J.; Gansevoort, R.T.; de Zeeuw, D. Metabolic syndrome: A fata morgana? Nephrol. Dial. Transplant. 2007, 22, 15–20. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Regitz-Zagrosek, V.; Lehmkuhl, E.; Weickert, M.O. Gender differences in the metabolic syndrome and their role for cardiovascular disease. Clin. Res. Cardiol. 2006, 95, 136–147. [Google Scholar] [CrossRef]
- Fezeu, L.; Balkau, B.; Kengne, A.P.; Sobngwi, E.; Mbanya, J.C. Metabolic syndrome in a sub-Saharan African setting: Central obesity may be the key determinant. Atherosclerosis 2006, 193, 70–76. [Google Scholar] [CrossRef]
- De José, A.P.P.; Verdalles-Guzmán, Ú.; Abad, S.; Vega, A.; Reque, J.; Panizo, N.; Rincón, A.; Yuste, C.; Arroyo, D.; López-Gómez, J.M. Metabolic syndrome is associated with cardiovascular events in hemodialysis. Nefrologia 2014, 34, 69–75. [Google Scholar] [CrossRef]
- Li, Z.; Yang, X.; Yang, J.; Yang, Z.; Wang, S.; Sun, F.; Zhan, S. The cohort study on prediction of incidence of all-cause mortality by metabolic syndrome. PLoS ONE 2016, 11, e0154990. [Google Scholar] [CrossRef]
- Liu, L.; Miura, K.; Fujiyoshi, A.; Kadota, A.; Miyagawa, N.; Nakamura, Y.; Ohkubo, T.; Okayama, A.; Okamura, T.; Ueshima, H. Impact of metabolic syndrome on the risk of cardiovascular disease mortality in the United States and in Japan. Am. J. Cardiol. 2014, 113, 84–89. [Google Scholar] [CrossRef]
- Amouzegar, A.; Mehran, L.; Hasheminia, M.; Rahimabad, P.K.; Azizi, F. The predictive value of metabolic syndrome for cardiovascular and all-cause mortality: Tehran lipid and glucose study. Diabetes Metab. Res. Rev. 2017, 33, e2819. [Google Scholar] [CrossRef]


| At Baseline | |
|---|---|
| Age (years) | 64.78 ±11.33 |
| Men (%) | 82 (59.4%) |
| Dialysis vintage (months) | 67.74 ± 53.09 |
| Arteriovenous fistula (%) | 83.3 |
| Kt/V | 1.36 ± 0.70 |
| Dry weight (kg) | 65.3 ± 13.7 |
| Interdialtic weight gain (kg) | 2.6 ± 2.1 |
| Body Mass Index (kg/m2) | 24.6 ± 3.9 |
| Waist circumference (cm) | 94.1 ± 13.1 |
| Systolic blood pressure (mmHg) | 134.4 ± 31.6 |
| Diastolic blood pressure (mmHg) | 92.2 ± 11.3 |
| Hypertension (%) | 103 (73.91%) |
| Diabetes mellitus (%) | 31 (22.46%) |
| Hyperlipidemia (%) | 44 (31.88%) |
| Hgb (g/L) | 104.22 ± 5.10 |
| Cholesterol (mmol/L) | 5.1 ± 1.2 |
| Triglycerides (mmol/L) | 2.9 ± 1.9 |
| LDL-C (mmol/L) | 3.1 ± 0.5 |
| HDL-C (mmol/L) | 1.3 ± 0.7 |
| s. Albumins (g/L) | 33.00 ± 4.89 |
| Total protein (g/L) | 69.91 ± 7.87 |
| s. Creatinine (μmol/L) | 842.94 ± 189.38 |
| CRP (mg/L) | 3.94 ± 2.84 |
| PTH (pg/mL) | 339.34 ± 225.97 |
| Number of Patients | |||
|---|---|---|---|
| Metabolic Syndrome (n, %) | Yes 79 (57.24%) | No 59 (42.76%) | p Value * |
| ATP III MS Criteria | |||
| Hypertension | 72 (91.14%) | 50 (84.7%) | <0.05 |
| Increased waist circumference | 66 (83.54%) | 20 (33.89%) | <0.05 |
| Low HDL-C | 61 (77.21%) | 19 (32.20%) | <0.001 |
| High triglycerides | 52 (65.82%) | 8 (13.55%) | <0.001 |
| Hyperglycemia | 36 (45.57%) | 11 (18.64%) | <0.001 |
| Age (years) | 56.2 ± 12.4 | 49.1 ± 15.3 | 0.022 |
| Gender (%) | |||
| Men | 27.4 | 72.6 | <0.001 |
| Women | 51.8 | 48.2 | 0.71 |
| Dialysis vintage (months) | 52.3 ± 44.6 | 69.3 ± 42.7 | <0.05 |
| Dry weight (kg) | 71 ± 29 | 56 ± 18.2 | <0.001 |
| Interdialytic weight gain (kg) | 3.2 ± 1.3 | 2.2 ± 0.9 | <0.001 |
| Body Mass Index (kg/m2) | 29.1 ± 2.18 | 23.1 ± 1.8 | <0.001 |
| Waist circumference (cm) | 108.3 ± 12.6 | 75.2 ± 14.3 | <0.001 |
| Obesity | 27 (34.17%) | 11 (13.92%) | <0.05 |
| Diastolic blood pressure (mmHg) | 83.2 ± 9.2 | 72.3 ± 11.4 | <0.05 |
| Hgb (g/L) | 101.2 ± 7.6 | 103.1 ± 4.2 | 0.66 |
| Blood glucose level (mmol/L) | 10.6 ± 4.3 | 6.2 ± 2.8 | <0.05 |
| Cholesterol (mmol/L) | 4.64 ± 1.13 | 3.36 ± 1.86 | <0.05 |
| Triglycerides (mmol/L) | 2.96 ± 1.3 | 1.88 ± 0.96 | <0.001 |
| LDL-C (mmol/L) | 3.14 ± 1.7 | 2.16 ± 1.8 | <0.05 |
| HDL-C (mmol/L) | 0.79 ± 0.56 | 1.02 ± 0.3 | <0.05 |
| s. Albumin (g/L) | 34.2 ± 4.8 | 35.3 ±8.3 | 0.82 |
| Total protein (g/L) | 72.2 ± 4.6 | 71.3 ± 6.2 | 0.44 |
| s. Creatinine (μmol/L) | 726.2 ± 108.3 | 699.5 ± 159.5 | 0.39 |
| CRP (mg/L) | 7.01 ± 2.8 | 2.3 ± 2.1 | <0.001 |
| PTH (pg/mL) | 319.86 ± 101.3 | 298.2 ± 179.3 | 0.18 |
| Metabolic Syndrome | OR (CI 95%) | p Value | ||
|---|---|---|---|---|
| Yes | No | |||
| Gender (%) | <0.001 | |||
| Male | 27.4 | 72.6 | reference | |
| Female | 51.8 | 48.2 | 1.66 (1.23–2.14) | |
| Age (%) | 0.021 | |||
| <45 years | 12.2 | 87.8 | reference | |
| >45years | 35.3 | 64.7 | 4.92 (3.23–9.18) | |
| Body Mass Index (%) | <0.001 | |||
| <20 | 18.2 | 81.8 | 0.38 | |
| 21–25 | 41.1 | 58.9 | reference | |
| 26–30 | 73.5 | 26.5 | 4.22 (2.3–7.14) | |
| >30 | 81.8 | 18.2 | 8.91 (6.34–10.2) | |
| CRP (mg/L) (%) | 0.038 | |||
| <5 | 20.1 | 79.9 | reference | |
| 5–10 | 38.6 | 61.4 | 1.71 (1.13–3.19) | |
| Number of Deaths | Cardiovascular Mortality | All-Cause Mortality | ||
|---|---|---|---|---|
| 24 (72.7) | 9 (27.3) | |||
| HR (95%) | p Value | HR (95%) | p Value | |
| MetS components | ||||
| Hypertension | 1.58 (1.24–1.94) a | <0.001 | 1.70 (1.24–2.76) a | 0.036 |
| Abdominal obesity | 1.52 (1.13–1.84) a | <0.001 | 1.12 (0.77–1.81) a | 0.28 |
| Low HDL-C | 0.69 (0.56–1.09) a | 0.033 | 1.17 (0.75–1.66) a | 0.053 |
| Hypertriglyceridemia | 1.15 (0.82-1.53) | 0.08 | 1.21 (0.77–1.63) a | 0.49 |
| Hyperglycemia | 0.89 (0.56–1.42) a | 0.23 | 1.19 (0.70–1.75) a | 0.55 |
| Number of MetS components | ||||
| 0 | 1.00 | 0 | 1.00 | 0 |
| 1 | 0.88 (0.58–1.46) | 0.75 | 0.60 (0.33–1.07) | 0.21 |
| 2 | 0.94 (0.70–1.55) | 0.44 | 0.60 (0.41–1.22) | 0.33 |
| 3 | 1.81 (1.21–2.33) | <0.001 | 1.37 (0.88–2.59) | 0.66 |
| 4 | 1.90 (1.19–2.99) | 0.05 | 1.62 (0.90–3.01) | 0.38 |
| 5 | 2.88 (1.76–4.17) | <0.001 | 1.81 (0.76–4.31) | 0.19 |
| No (<3 components) | 1.00 | |||
| Yes (≥3 components) | 2.51 (1.25–3.83) b | <0.001 | 1.99 (1.42–2.97) b | <0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dimitrijevic, Z.; Jovanovic, A.; Cvetkovic, M.; Vrecic, T.; Kostic, E.; Mitic, B. Associations of Cardiovascular and All-Cause Mortality with Metabolic Syndrome in Hemodialysis Patients: A Prospective Single-Center Study. Medicina 2019, 55, 694. https://doi.org/10.3390/medicina55100694
Dimitrijevic Z, Jovanovic A, Cvetkovic M, Vrecic T, Kostic E, Mitic B. Associations of Cardiovascular and All-Cause Mortality with Metabolic Syndrome in Hemodialysis Patients: A Prospective Single-Center Study. Medicina. 2019; 55(10):694. https://doi.org/10.3390/medicina55100694
Chicago/Turabian StyleDimitrijevic, Zorica, Andriana Jovanovic, Mina Cvetkovic, Tamara Vrecic, Emina Kostic, and Branka Mitic. 2019. "Associations of Cardiovascular and All-Cause Mortality with Metabolic Syndrome in Hemodialysis Patients: A Prospective Single-Center Study" Medicina 55, no. 10: 694. https://doi.org/10.3390/medicina55100694
APA StyleDimitrijevic, Z., Jovanovic, A., Cvetkovic, M., Vrecic, T., Kostic, E., & Mitic, B. (2019). Associations of Cardiovascular and All-Cause Mortality with Metabolic Syndrome in Hemodialysis Patients: A Prospective Single-Center Study. Medicina, 55(10), 694. https://doi.org/10.3390/medicina55100694





