Usefulness of Protocolized Point-of-Care Ultrasonography for Patients with Acute Renal Colic Who Visited Emergency Department: A Randomized Controlled Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Selection of Participants
2.3. Randomization and Study Protocol
2.4. Ultrasonography
2.5. Outcome Measures
2.6. Sample Size Calculation and Statistical Analysis
3. Results
3.1. Study Patients and Baseline Characteristics
3.2. Outcome Analysis
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Romero, V.; Akpinar, H.; Assimos, D.G. Kidney stones: A global picture of prevalence, incidence, and associated risk factors. Rev. Urol. 2010, 12, e86–e96. [Google Scholar]
- Tae, B.S.; Balpukov, U.; Cho, S.Y.; Jeong, C.W. Eleven-year Cumulative Incidence and Estimated Lifetime Prevalence of Urolithiasis in Korea: A National Health Insurance Service-National Sample Cohort Based Study. J. Korean Med. Sci. 2017, 33, e13. [Google Scholar] [CrossRef]
- Shoag, J.; Tasian, G.E.; Goldfarb, D.S.; Eisner, B.H. The new epidemiology of nephrolithiasis. Adv. Chronic Kidney Dis. 2015, 22, 273–278. [Google Scholar] [CrossRef]
- Vieweg, J.; Teh, C.; Freed, K.; Leder, R.A.; Smith, R.H.; Nelson, R.H.; Preminger, G.M. Unenhanced helical computerized tomography for the evaluation of patients with acute flank pain. J. Urol. 1998, 160, 679–684. [Google Scholar] [CrossRef]
- Smith, R.C.; Levine, J.; Dalrymple, N.C.; Barish, M.; Rosenfield, A.T. Acute flank pain: A modern approach to diagnosis and management. Semin. Ultrasound CT MRI 1999, 20, 108–135. [Google Scholar] [CrossRef]
- Kartal, M.; Eray, O.; Erdogru, T.; Yilmaz, S. Prospective validation of a current algorithm including bedside US performed by emergency physicians for patients with acute flank pain suspected for renal colic. Emerg. Med. J. 2006, 23, 341–344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luchs, J.S.; Katz, D.S.; Lane, M.J.; Mellinger, B.C.; Lumerman, J.H.; Stillman, C.A.; Meiner, E.M.; Perlmutter, S. Utility of hematuria testing in patients with suspected renal colic: Correlation with unenhanced helical CT results. Urology 2002, 59, 839–842. [Google Scholar] [CrossRef]
- Bhagra, A.; Tierney, D.M.; Sekiguchi, H.; Soni, N.J. Point-of-Care Ultrasonography for Primary Care Physicians and General Internists. Mayo Clin. Proc. 2016, 91, 1811–1827. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Le Coz, J.; Orlandini, S.; Titomanlio, L.; Rinaldi, V.E. Point of care ultrasonography in the pediatric emergency department. Ital. J. Pediatr. 2018, 44, 87. [Google Scholar] [CrossRef]
- Sudah, M.; Vanninen, R.L.; Partanen, K.; Kainulainen, S.; Malinen, A.; Heino, A.; Ala-Opas, M. Patients with Acute Flank Pain: Comparison of MR Urography with Unenhanced Helical CT. Radiology 2002, 223, 98–105. [Google Scholar] [CrossRef]
- Riddell, J.; Case, A.; Wopat, R.; Beckham, S.; Lucas, M.; McClung, C.D.; Swadron, S. Sensitivity of emergency bedside ultrasound to detect hydronephrosis in patients with computed tomography-proven stones. West. J. Emerg. Med. 2014, 15, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Kanno, T.; Kubota, M.; Sakamoto, H.; Nishiyama, R.; Okada, T.; Higashi, Y.; Yamada, H. Determining the Efficacy of Ultrasonography for the Detection of Ureteral Stone. Urology 2014, 84, 533–537. [Google Scholar] [CrossRef] [PubMed]
- Shokeir, A.A.; Mahran, M.R.; Abdulmaaboud, M. Renal colic in pregnant women: Role of renal resistive index. Urology 2000, 55, 344–347. [Google Scholar] [CrossRef]
- Rosen, C.L.; Brown, D.F.; Sagarin, M.J.; Chang, Y.; McCabe, C.J.; Wolfe, R.E. Ultrasonography by emergency physicians in patients with suspected ureteral colic. J. Emerg. Med. 1998, 16, 865–870. [Google Scholar] [CrossRef]
- Gaspari, R.J.; Horst, K. Emergency ultrasound and urinalysis in the evaluation of flank pain. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2005, 12, 1180–1184. [Google Scholar] [CrossRef]
- Wong, C.; Teitge, B.; Ross, M.; Young, P.; Robertson, H.L.; Lang, E. The Accuracy and Prognostic Value of Point-of-care Ultrasound for Nephrolithiasis in the Emergency Department: A Systematic Review and Meta-analysis. Acad. Emerg. Med. 2018, 25, 684–698. [Google Scholar] [CrossRef]
- Straub, M.; Strohmaier, W.L.; Berg, W.; Beck, B.; Hoppe, B.; Laube, N.; Lahme, S.; Schmidt, M.; Hesse, A.; Koehrmann, K.U. Diagnosis and metaphylaxis of stone disease. Consensus concept of the National Working Committee on Stone Disease for the upcoming German Urolithiasis Guideline. World J. Urol. 2005, 23, 309–323. [Google Scholar] [CrossRef]
- Chaussy, C. Therapeutic Energy Application in Urology: Standards and Recent Developments; Georg Thieme Verlag: Stuttgart, Germany; New York, NY, USA, 2005; ISBN 1588904288. [Google Scholar]
- Noble, V.E.; Brown, D.F.M. Renal ultrasound. Emerg. Med. Clin. 2004, 22, 641–659. [Google Scholar] [CrossRef]
- Dalziel, P.J.; Noble, V.E. Bedside ultrasound and the assessment of renal colic: A review. Emerg. Med. J. 2013, 30, 3–8. [Google Scholar] [CrossRef]
- Park, Y.H.; Jung, R.B.; Lee, Y.G.; Hong, C.K.; Ahn, J.-H.; Shin, T.Y.; Kim, Y.S.; Ha, Y.R. Does the use of bedside ultrasonography reduce emergency department length of stay for patients with renal colic? A pilot study. Clin. Exp. Emerg. Med. 2016, 3, 197–203. [Google Scholar] [CrossRef]
- Heidenreich, A.; Desgrandschamps, F.; Terrier, F. Modern approach of diagnosis and management of acute flank pain: Review of all imaging modalities. Eur. Urol. 2002, 41, 351–362. [Google Scholar] [CrossRef]
- Wang, R.C. Managing Urolithiasis. Ann. Emerg. Med. 2016, 67, 449–454. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Watkins, S.; Bowra, J.; Sharma, P.; Holdgate, A.; Giles, A.; Campbell, L. Validation of emergency physician ultrasound in diagnosing hydronephrosis in ureteric colic. Emerg. Med. Australas. 2007, 19, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Hernandez, N.; Gee, M.S.; Noble, V.E.; Eisner, B.H. Can ureteral stones cause pain without causing hydronephrosis? World J. Urol. 2016, 34, 1285–1288. [Google Scholar] [CrossRef] [PubMed]
- Goertz, J.K.; Lotterman, S. Can the degree of hydronephrosis on ultrasound predict kidney stone size? Am. J. Emerg. Med. 2010, 28, 813–816. [Google Scholar] [CrossRef]
- Gottlieb, M.; Long, B.; Koyfman, A. The evaluation and management of urolithiasis in the ED: A review of the literature. Am. J. Emerg. Med. 2018, 36, 699–706. [Google Scholar] [CrossRef]
- Coursey, C.A.; Casalino, D.D.; Remer, E.M.; Arellano, R.S.; Bishoff, J.T.; Dighe, M.; Fulgham, P.; Goldfarb, S.; Israel, G.M.; Lazarus, E.; et al. ACR Appropriateness Criteria(R) acute onset flank pain—Suspicion of stone disease. Ultrasound Q. 2012, 28, 227–233. [Google Scholar] [CrossRef]
- Trzeciak, S.; Rivers, E.P. Emergency department overcrowding in the United States: An emerging threat to patient safety and public health. Emerg. Med. J. EMJ 2003, 20, 402–405. [Google Scholar] [CrossRef]
- Di Somma, S.; Paladino, L.; Vaughan, L.; Lalle, I.; Magrini, L.; Magnanti, M. Overcrowding in emergency department: An international issue. Intern. Emerg. Med. 2015, 10, 171–175. [Google Scholar] [CrossRef]
- Van der Linden, M.C.C.; van Ufford, H.; van der Linden, N.N. The impact of a multimodal intervention on emergency department crowding and patient flow. Int. J. Emerg. Med. 2019, 12, 21. [Google Scholar] [CrossRef]
- Aksel, G.; Bildik, F.; Demircan, A.; Keles, A.; Kilicaslan, I.; Guler, S.; Corbacioglu, S.K.; Turkay, A.; Bekgoz, B.; Dogan, N.O. Effects of fast-track in a university emergency department through the National Emergency Department Overcrowding Study. J. Pak. Med. Assoc. 2014, 64, 791–797. [Google Scholar] [PubMed]


| Conventional Group (n = 74) | Ultrasound Group (n = 73) | p-Value | |
|---|---|---|---|
| Male | 42 (57) | 49 (67) | 0.196 |
| Age (years) | 55 (42–62) | 48 (38–59) | 0.164 |
| Previous medical history | |||
| Hypertension | 9 (12) | 10 (14) | 0.781 |
| Diabetes | 1 (2) | 4 (6) | 0.209 |
| Cardiac, Lung, Kidney disease | 0 | 0 | 0.999 |
| Malignancy | 2 (3) | 3 (4) | 0.681 |
| Liver disease | 1 (2) | 3 (4) | 0.304 |
| Ureter stone history (before 30 days) | 18 (24) | 22 (30) | 0.429 |
| Pain score (Numeric rating scale) | 6 (4–7) | 5 (4–7) | 0.584 |
| Vital sign | |||
| SBP (mmHg) | 139 (120–157) | 134 (120–155) | 0.173 |
| DBP (mmHg) | 83 (74–97) | 83 (75–93) | 0.651 |
| Heart rate (beats per minute) | 73 (66–81) | 74 (66–79) | 0.744 |
| Body temperature (°C) | 36.5 (36.3–36.9) | 36.6 (36.2–36.8) | 0.889 |
| Laboratory test | |||
| Serum creatinine | 0.93 (0.78–1.02) | 0.97 (0.76–1.49) | 0.258 |
| Urine analysis | |||
| Presence of Hematuria | 56 (76) | 63 (86) | 0.101 |
| Nitrite | 3 (4) | 3 (4) | 0.999 |
| Leukocyte esterase | 15 (20) | 16 (22) | 0.807 |
| Admission | 0 | 0 | 0.999 |
| Final diagnosis of ureter stone | 61 (83) | 67 (92) | 0.139 |
| Conventional Group (n = 74) | Ultrasound Group (n = 73) | p-Value | |||
|---|---|---|---|---|---|
| Mean (±SD) | 95% CI | Mean (±SD) | 95% CI | ||
| ED LOS (min) | 234 (±76) | (216–252) | 172 (±92) | (151–194) | <0.001 |
| Time from CT to discharge (min) | 104 (±60) | (91–118) | 125 (±70) | (104–141) | 0.065 |
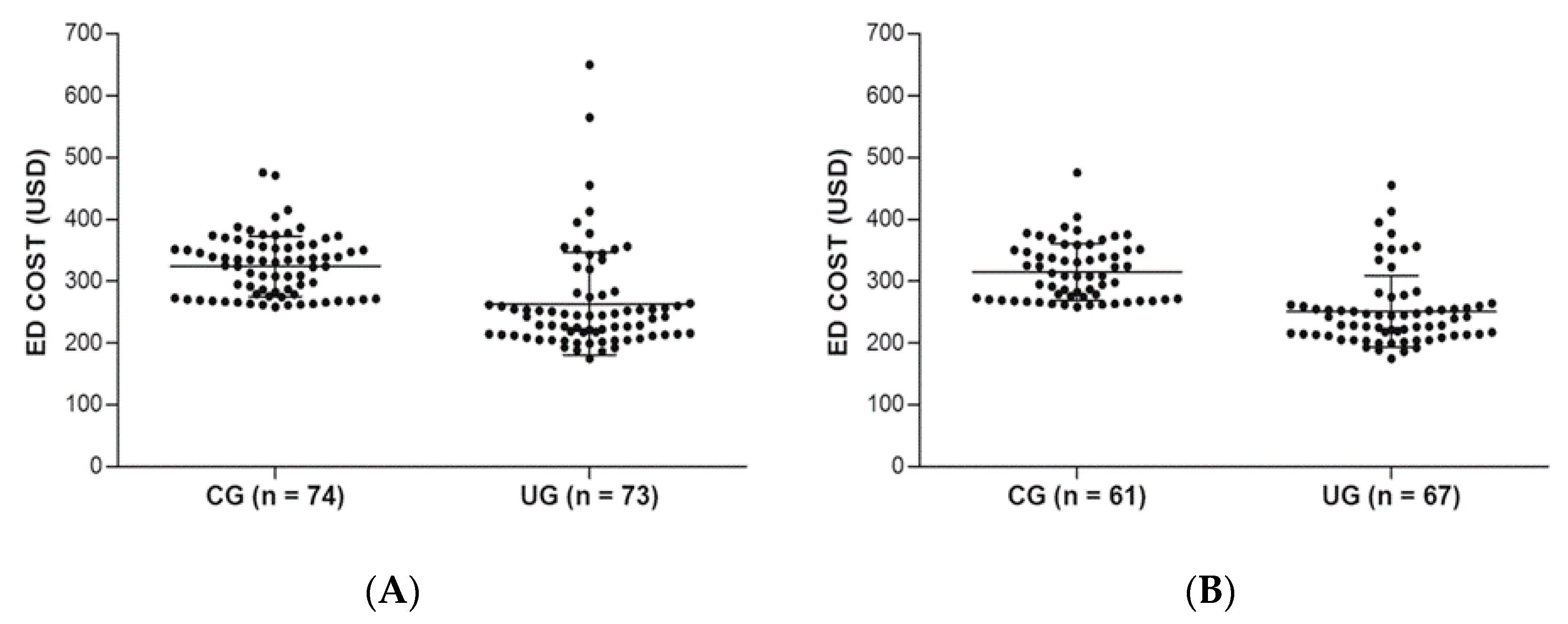
| ED Cost (USD) | 319 (±48) | (308–330) | 259 (±81) | (240–278) | <0.001 |
| Diagnosed as Ureter stone | CG (n = 61) | UG (n = 67) | |||
| ED LOS (min) | 231 (±78) | (211–251) | 157 (±57) | (144–171) | <0.001 |
| Time from CT to discharge (min) | 104 (±62) | (88–119) | 118 (±50) | (106–130) | 0.154 |
| ED Cost (USD) | 310 (±46) | (298–322) | 247 (±57) | (233–260) | <0.001 |
| Follow-up | |||||
| ESWL | 14 (23) | 14 (21) | 0.813 | ||
| AKI | 0 (0) | 1 (2) | 0.999 | ||
| UTI | 0 (0) | 1 (2) | 0.999 | ||
| Other hospital follow-up | 6 (10) | 7 (11) | 0.886 | ||
| Missed diagnosis | 0 | 0 | |||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.G.; Jo, I.J.; Kim, T.; Hwang, S.Y.; Park, J.H.; Shin, T.G.; Sim, M.S.; Cha, W.C.; Yoon, H. Usefulness of Protocolized Point-of-Care Ultrasonography for Patients with Acute Renal Colic Who Visited Emergency Department: A Randomized Controlled Study. Medicina 2019, 55, 717. https://doi.org/10.3390/medicina55110717
Kim SG, Jo IJ, Kim T, Hwang SY, Park JH, Shin TG, Sim MS, Cha WC, Yoon H. Usefulness of Protocolized Point-of-Care Ultrasonography for Patients with Acute Renal Colic Who Visited Emergency Department: A Randomized Controlled Study. Medicina. 2019; 55(11):717. https://doi.org/10.3390/medicina55110717
Chicago/Turabian StyleKim, Seok Goo, Ik Joon Jo, Taerim Kim, Sung Yeon Hwang, Joo Hyun Park, Tae Gun Shin, Min Seob Sim, Won Chul Cha, and Hee Yoon. 2019. "Usefulness of Protocolized Point-of-Care Ultrasonography for Patients with Acute Renal Colic Who Visited Emergency Department: A Randomized Controlled Study" Medicina 55, no. 11: 717. https://doi.org/10.3390/medicina55110717






