Exercise Interventions for Improving Flexibility in People with Multiple Sclerosis: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Process
2.2. Selection Procedure and Eligibility Criteria
2.3. Data Extraction
2.4. Assessment of Methodological Quality
2.5. Data Analysis
3. Results
3.1. Designs and Samples
3.2. Quality Assessment
3.3. Interventions
3.4. Effects of the Programs on Flexibility
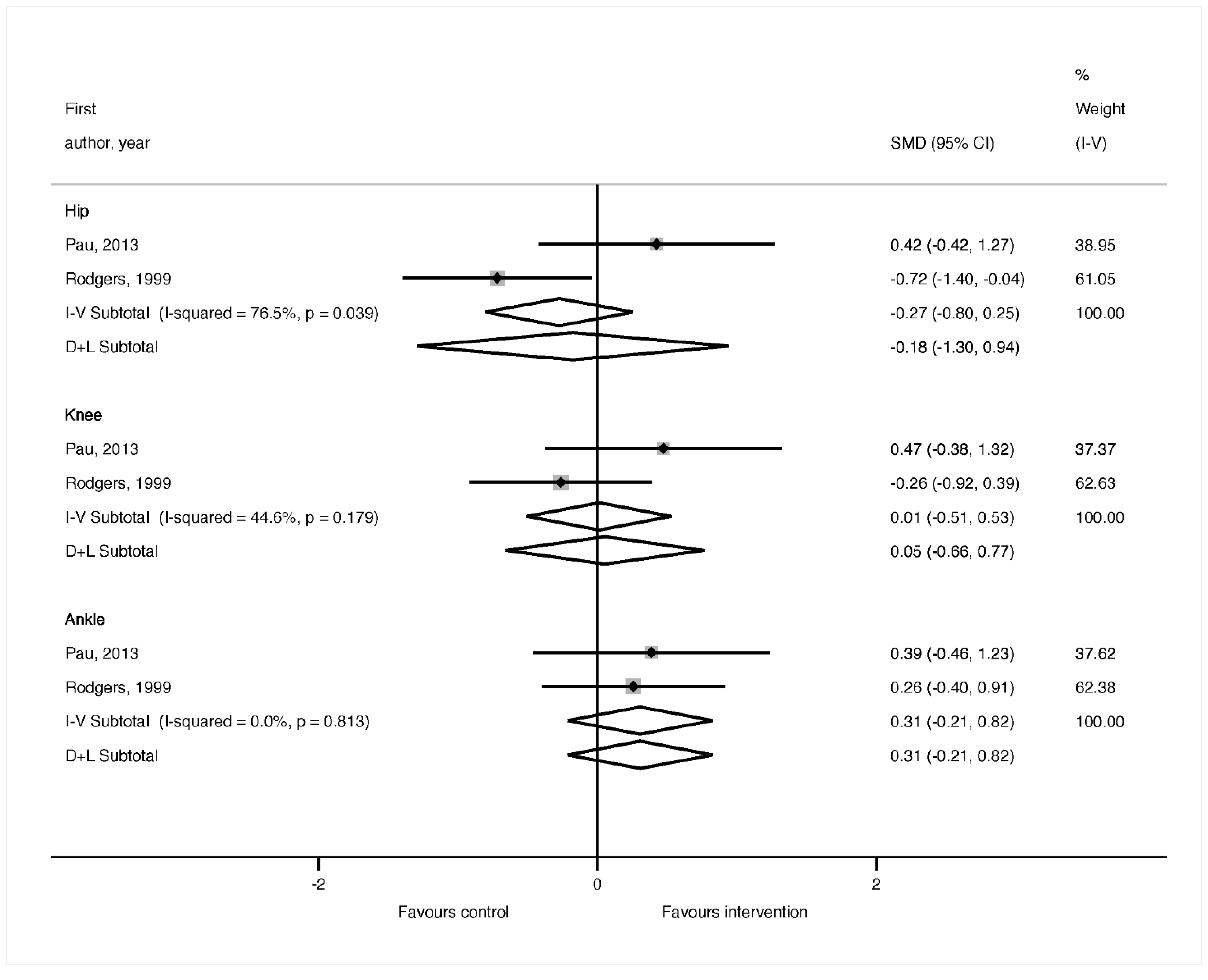
3.4.1. Lower Limb Range of Motion.
3.4.2. Flexibility of the Posterior Kinetic Chain
3.4.3. Upper Limb Range of Motion
3.4.4. Upper Limb Flexibility
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Thompson, A.J.; Baranzini, S.E.; Geurts, J.; Hemmer, B.; Ciccarelli, O. Multiple sclerosis. Lancet 2018, 391, 1622–1636. [Google Scholar] [CrossRef]
- Browne, P.; Chandraratna, D.; Angood, C.; Tremlett, H.; Baker, C.; Taylor, B.V.; Thompson, A.J. Atlas of Multiple Sclerosis 2013: A growing global problem with widespread inequity. Neurology 2014, 83, 1022–1024. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Orton, S.M.; Herrera, B.M.; Yee, I.M.; Valdar, W.; Ramagopalan, S.V.; Sadovnick, A.D.; Ebers, G.C.; Canadian Collaborative Study Group. Sex ratio of multiple sclerosis in Canada: A longitudinal study. Lancet Neurol. 2006, 5, 932–936. [Google Scholar] [CrossRef]
- Gohil, K. Multiple Sclerosis: Progress, but No Cure. Pharm. Ther. 2015, 40, 604–605. [Google Scholar]
- Cerqueira, J.J.; Compston, D.A.S.; Geraldes, R.; Rosa, M.M.; Schmierer, K.; Thompson, A.; Tinelli, M.; Palace, J. Time matters in multiple sclerosis: Can early treatment and long-term follow-up ensure everyone benefits from the latest advances in multiple sclerosis? J. Neurol. Neurosurg. Psychiatry. 2018, 89, 844–850. [Google Scholar] [CrossRef]
- Motl, R.W.; Sandroff, B.M. Benefits of exercise training in multiple sclerosis. Curr. Neurol. Neurosci. Rep. 2015, 15, 62. [Google Scholar] [CrossRef]
- Dodd, K.; Taylor, N.; Shields, N.; Prasad, D.; McDonald, E.; Gillon, A. Progressive resistance training did not improve walking but can improve muscle performance, quality of life and fatigue in adults with multiple sclerosis: A randomized controlled trial. Mult. Scler. 2011, 17, 1362–1374. [Google Scholar] [CrossRef]
- Petajan, J.H.; White, A.T. Recommendations for physical activity in patients with multiple sclerosis. Sports Med. 1999, 27, 179–191. [Google Scholar] [CrossRef]
- Halabchi, F.; Alizadeh, Z.; Sahraian, M.A.; Abolhasani, M. Exercise prescription for patients with multiple sclerosis; potential benefits and practical recommendations. BMC Neurol. 2017, 17, 185. [Google Scholar] [CrossRef]
- White, L.J.; Dressendorfer, R.H. Exercise and multiple sclerosis. Sports Med. 2004, 34, 1077–1100. [Google Scholar] [CrossRef]
- Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef]
- Foley, N.C.; Teasell, R.W.; Bhogal, S.K.; Speechley, M.R. Stroke Rehabilitation Evidence-Based Review: Methodology. Top. Stroke Rehabil. 2003, 10, 1–7. [Google Scholar] [CrossRef]
- National Heart, Lung and Blood Institute (NHLBI). Quality Assessment Tool for Before-After (Pre-Post) Studies with No Control Group. Study Qual Assess Tools. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 9 July 2019).
- Slade, S.C.; Dionne, C.E.; Underwood, M.; Buchbinder, R. Consensus on Exercise Reporting Template (CERT): Explanation and elaboration statement. Br. J. Sports Med. 2016, 50, 1428–1437. [Google Scholar] [CrossRef] [PubMed]
- Valentine, J.C.; Pigott, T.D.; Rothstein, H.R. How Many Studies Do You Need? J. Educ. Behav. Stat. 2010, 35, 215–247. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Cohen, J. A Power Primer; American Psychological Association: Washington, DC, USA, 2003. [Google Scholar]
- McAuley, E.; Wójcicki, T.R.; Learmonth, Y.C.; Roberts, S.A.; Hubbard, E.A.; Kinnett-Hopkins, D.; Fanning, J.; Motl, R.W. Effects of a DVD-delivered exercise intervention on physical function in older adults with multiple sclerosis: A pilot randomized controlled trial Multiple Sclerosis. Mult. Scler. J. Exp. Transl. Clin. 2015, 40, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Duff, W.R.D.; Andrushko, J.W.; Renshaw, D.W.; Chilibeck, P.D.; Farthing, J.P.; Danielson, J.; Evans, C.D. Impact of Pilates exercise in multiple sclerosis: A randomized controlled trial. Int. J. Mult. Scler. Care. 2018, 20, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Pau, M.; Corona, F.; Coghe, G.; Marongiu, E.; Loi, A.; Crisafulli, A.; Concu, A.; Galli, M.; Marrosu, M.G.; Cocco, E. Quantitative assessment of the effects of 6 months of adapted physical activity on gait in people with multiple sclerosis: A randomized controlled trial. Disabil Rehabil. 2018, 40, 144–151. [Google Scholar] [CrossRef]
- Ponzano, M.; Beratto, L.; Mazza, C.; Di Tommaso, S.; Abate Daga, F.; Allois, R.; Gollin, M. Benefits of static stretching, Pilates® and elastic bands resistance training on patients with relapsing-remitting multiple sclerosis: A longitudinal study. J. Neurol. Neurophysiol. 2017, 8, 4. [Google Scholar] [CrossRef]
- Pereira, G.C.; Ferreira Vasconcellos, T.H.; Ferreira, C.M.; Teixeira, D.G. Techniques Combinations of Physical Therapy In the Treatment of Patients With Multiple Sclerosis: Case Series. Rev. Neurociênc. 2012, 20, 494–504. [Google Scholar] [CrossRef]
- Rodgers, M.M.; Mulcare, J.A.; King, D.L.; Mathews, T.; Gupta, S.C.; Glaser, R.M. Gait characteristics of individuals with multiple sclerosis before and after a 6-month aerobic training program. J. Rehabil. Res. Dev. 1999, 36, 183–188. [Google Scholar] [PubMed]
- Husted, C.; Pham, L.; Hekking, A.; Niederman, R. Improving quality of life for people with chronic conditions: The example of t’ai chi and multiple sclerosis. Altern. Ther. Health Med. 1999, 5, 70–74. [Google Scholar] [PubMed]
- Linde, K.; Scholz, M.; Melchart, D.; Willich, S.N. Should systematic reviews include non-randomized and uncontrolled studies? The case of acupuncture for chronic headache. J. Clin. Epidemiol. 2002, 55, 77–85. [Google Scholar] [CrossRef]
- Peinemann, F.; Tushabe, D.A.; Kleijnen, J. Using multiple types of studies in systematic reviews of health care interventions—A systematic review. PLoS ONE 2013, 8, e85035. [Google Scholar] [CrossRef]
- Huisinga, J.M.; Filipi, M.; Stergiou, N. Elliptical exercise improves fatigue ratings and quality of life in patients with multiple sclerosis. J. Rehabil. Res. Dev. 2011, 48, 881–890. [Google Scholar] [CrossRef]
- Moradi, M.; Sahraian, M.A.; Aghsaie, A.; Kordi, M.R.; Meysamie, A.; Abolhasani, M.; Sobhani, V. Effects of eight-week resistance training program in men with multiple sclerosis. Asian J. Sports Med. 2015, 6, e22838. [Google Scholar] [CrossRef]
- Bovend’Eerdt, T.J.; Newman, M.; Barker, K.; Dawes, H.; Minelli, C.; Wade, D.T. The effects of stretching in spasticity: A systematic review. Arch. Phys. Med. Rehabil. 2018, 89, 1395–1406. [Google Scholar] [CrossRef]
- Borenstein, M. Meta-Analysis: Concepts and Applications. In Proceedings of the Statistical Horizons Seminar, Washington, DC, USA, 12–13 December 2013. [Google Scholar]
- Davies, B.L.; Arpin, D.J.; Volkman, K.G.; Corr, B.; Reelfs, H.; Harbourne, R.T.; Healey, K.; Zabad, R.; Kurz, M.J. Neurorehabilitation strategies focusing on ankle control improve mobility and posture in persons with multiple sclerosis. J. Neurol. Phys. Ther. 2015, 39, 225–232. [Google Scholar] [CrossRef]
- Heesen, C.; Böhm, J.; Reich, C.; Kasper, J.; Goebel, M.; Gold, S.M. Patient perception of bodily functions in multiple sclerosis: Gait and visual function are the most valuable. Mult. Scler. 2008, 14, 988–991. [Google Scholar] [CrossRef]
- Johansson, S.; Ytterberg, C.; Claesson, I.M.; Lindberg, J.; Hillert, J.; Andersson, M.; Widén Holmqvist, L.; von Koch, L. High concurrent presence of disability in multiple sclerosis. Associations with perceived health. J. Neurol. 2007, 254, 767–773. [Google Scholar] [CrossRef]
- Paltamaa, J.; Sarasoja, T.; Leskinen, E.; Wikstrom, J.; Malkia, E. Measures of physical functioning predict self-reported performance in self-care, mobility, and domestic life in ambulatory persons with multiple sclerosis. Arch. Phys. Med. Rehabil. 2007, 88, 1649–1657. [Google Scholar] [CrossRef] [PubMed]


| First Author, Year (Design) | Participants | Interventions | Outcomes (Test) | Results |
|---|---|---|---|---|
| McAuley, 2015 [18] (RCT) | n = 48 (75% women) Score EDSS: <6.5 IG: n = 24 (75% women) Score EDSS: NR Age: 59.62 ± 1.43 years Disease duration: 18.10 ± 9.42 years MS type: RR: n = 16 (66.7%) SP: n = 3 (12.5%) PP: n = 1 (4.2%) NR: n = 4 (16.6%) CG: n = 24 (75% women) Score EDSS: NR Age: 59.78 ± 1.50 years Disease duration: 19.85 ± 9.42 years MS type: RR: n = 16 (66.7%) SP: n = 2 (8.3%) PP: n = 0 NR: n = 6 (25%) | Combined Exercises Program: “FlexToBa DVDs” (balance, strength and flexibility) Duration: 6 months Development: - The first two weeks of each month: Volume: 1 to 2 sets of 8 to 10 reps Intensity: Borg 6–20 RPE scale of 10–12 - The last two weeks of the month: Volume: 2 sets of 10 to 12 reps Intensity: Borg 6–20 RPE scale of 13–15 Volume: 6 progressive exercise sessions/Each session containing two sets of 11 to 12 different exercises Frequency: 3 times/week (non-consecutive days) Intensity: All exercises began with the lower resistance band and advanced to the thicker band | Flexibility - Upper body (Back Scratch test) - Lower body (Sit and Reach test) | - Sit and Reach test: Intragroup: IG: Pre: −0.45 cm ± 0.84/Post: 0.62 cm ± 0.95 Post-adjusted: 0.61 cm ± 0.57 CG: Pre: −0.48 cm ± 0.84/Post: 0.44 cm ±0.95 Post-adjusted: 0.27 cm ± 0.57 Intergroup: Not-significant values p-value pre: 0.80/p-value post: 0.68 p-value post- adjusted: 0.68 - Back Scratch test: Intragroup: IG: pre: −4.52 cm ± 1.30/Post: −4.19 cm ± 1.06 Post-adjusted: −4.50 cm ± 0.54 CG: Pre: −5.28 cm ± 1.30/Post: −6.29 cm ± 1.06 Post-adjusted: −6.02 cm ± 0.54 Intergroup: p-value pre: 0.38/p-value post: 0.16 p-value post-adjusted: 0.05 * |
| Duff, 2018 [19] (RCT) | n = 30 (77% women) Score EDSS: NR IG: n = 15 (80% women) Score EDSS: NR Age: 45.7 ± 9.4 years Disease duration: NR MS type: RR: n = 14 (93%) SP: n = 0 PP: n = 1 (7%) CG: n = 15 (73% women) Score EDSS: NR Age: 45.1 ± 7.4 years Disease duration: NR MS type: RR: n = 11 (73%) SP: n = 2 (13%) PP: n = 2 (13%) | “Pilates exercise program and physiotherapy massage” Duration: 12 weeks Development: - Exercises in the standing position on the CoreAlign apparatus and floor mat work - Each session started with a warm-up and ended with a cool-down IG: Pilates + massage Volume: 50 min—Pilates 60 min—massage Frequency: 2 times/week 1 time/week Intensity: Existing exercises progressed in difficulty, and new exercises were introduced over the study period based on each participant’s individual performance. CG: Massage Volume: 60 min—massage Frequency: 1 time/week | Flexibility - Lower body, posterior kinetic chain (Sit and Reach test) | - Sit and Reach test: Intragroup: IG: Pre: 23.4 cm (11.4)/Post: 25.4 cm (11.0) CG: Pre: 28.4 cm (10.8)/Post: 30.3 cm (9.5) Intergroup: IG: 2.0 cm (−1.8 to 5.7) CG:1.9 cm (−2.0 to 5.8) p-value = 0.98 |
| Pau, 2017 [20] (RCT) | n = 22 (45% women) Score EDSS: NR IG: n = 11 (45% women) Score EDSS: 3.6 ± 0.9 Age: 47.4 ± 10.8 years Disease duration: NR MS type: RR: n = 11 (100%) CG: n = 11 (45% women) Score EDSS: 3.4 ± 1.1 Age: 44.5 ± 13.5 years Disease duration: NR MS type: RR: n = 11 (100%) | “Combined exercises program” (aerobic and strength training) Duration: 24 weeks Development: Total volume: 60 min Frequency: 1 time/week Warm-up: Cycle-ergometer and stretching exercises for upper and lower limbs and trunk muscles Volume: 10 min Intensity: 30% of the maximum workload previously calculated by means of a cardiopulmonary test (CPT) Main Part: (Aerobic training) Volume: 20 min Intensity: 50% of the maximum value calculated for each participant on the basis of his/her CPT and progressively increased every week up to 80% of maximum work rate (Strength training) Volume: 20 min/1 set of 8 reps to progress until 3 sets of 12 reps Intensity: 15% (1RM) to progress until a 30% (1RM). Rest: 2–3 min/sets Cool-down: relaxation, postural control, spine mobility exercises and post-stretching Volume: 10 min | Flexibility - Dynamic ROM of the hip, knee and ankle (goniometer) | - Dynamic ROM during the gait cycle: Hip flexion–extension: Intragroup: IG: Pre: 42.70º ± 9.61/Post: 47.04° ± 10.13 p-value = 0.029 * CG: Pre: 42.71° ± 6.00/Post: 43.54° ± 3.88 Knee flexion–extension: Intragroup: IG: Pre: 52.88° ± 9.60/Post: 57.71° ± 10.06 p-value: 0.047 * CG: Pre: 50.75° ± 14.46/Post: 51.91° ± 12.98 Ankle dorsi–plantar–flexion: Intragroup: IG: Pre: 23.60° ± 5.81/Post: 26.08° ± 6.53 p-value = 0.043 * CG: Pre: 25.06° ± 10.14/Post: 25.17° ± 8.17 |
| Ponzano, 2017 [21] (RCT) | n = 22 (NR %women) Score EDSS: ≤6.5 IG1: n = 8 (NR %women) Score EDSS: 4 ± 2 Age: 50 ± 18 years Disease duration: NR MS type: RR: n = 8 (100%) IG2: n = 7 (NR %women) Score EDSS: 3 ± 2 Age: 52 ± 10 years Disease duration: NR MS type: RR: n = 7 (100%) IG3: n = 7 (NR %women) Score EDSS: 2 ± 2 Age: 45 ± 6 years Disease duration: NR MS type: RR: n = 7 (100%) | Three groups of training: 1. Flexibility training 2. Strength training 3. Pilates program Duration: 16 weeks Development: Each training session began with a warm-up including joint mobility and muscle flexibility exercises IG1: static stretching protocols Volume: 11 exercises/3 sets of 30 s Rest: 30 seg/sets Frequency: 2 times/week IG2: elastic bands Volume: 11 exercises/3 sets of 10 reps Rest: 30 seg/sets Frequency: 2 times/week IG3: Pilates protocol Volume: 12 exercises/2 sets of 8 reps Rest: 30 seg/sets Frequency: 2 times/week | The three groups were tested three times: - T0: after a month - T1: two months after T0 - T2: two months after T1 Flexibility: - Posterior kinetic chain (Sit and Reach test and Spinal Mouse test). | No significant variations concerning unlisted parameters emerged from this research. - Spinal Mouse test: IG1: T0 and T2 (p < 0.05, −55%, ES = 0.67) “Inclination line test between ThSp1 and S1” IG2 and IG3: NR - Sit and Reach test: IG1: T0 and T2 (p < 0.05, +15%, ES = 0.36) IG2: NR IG3: T0 and T2 (p < 0.05, +15%, ES = 0.4) |
| Pereira, 2012 [22] (Descriptive longitudinal quantitative) | n = 4 (100% women) Score EDSS: NR Age: 45.5 years (between 33–53 years) Disease duration: 7 years MS type: RR: n = 4 (100%) | “Combined exercises program” by physiotherapy (strength, flexibility and balance) Duration: 30 sets Development: Home session; exercises of strength, flexibility and balance Volume: 60 min Frequency: 1 time/week Type of exercise to improve ROM: - 10 joint mobilizations (shoulder, elbow, wrist, hip, knee and ankle) - 3 muscle stretching maintained for 30 s - The same pattern was followed on the contralateral side | Flexibility in three different measurements: - ROM of the ankle, knee, hip, shoulder, elbow and wrist during active movements performed in dorsal decubitus, ventral, sitting and orthodontic, respectively (goniometer) | - ROM (First, second, third measurement): Ankle dorsi-flexion: Right: 7.5°, 10°, 15° Left: 10°, 17.5°, 20° Ankle plantar-flexion: Right: 30°, 37.5°, 42.5° * Left: 40°, 42.5°, 45° Knee flexion: Right: 105°, 112.5°, 117.5° * Left: 92.5°, 112.5°, 122.5° * Hip flexion: Right: 25°, 40°, 57.5° * Left: 25°, 47.5°, 55° * Hip extension: Right: 17.5°, 20°, 25° Left: 20°, 17.5°, 20° Hip abduction: Right: 27.5°, 30°, 32.5° Left: 25°, 32.5°, 40° * Shoulder flexion: Right: 142.5°, 140°, 165° Left: 147.5°, 150°, 160° Shoulder extension: Right: 60°, 65°, 70° * Left: 52.5°, 62.5°, 70° * Shoulder abduction: Right: 142.5°, 150°, 170° * Left: 160°, 162.5°, 170° * Elbow flexion: Right: 127.5°, 132.5°, 135° * Left: 130°, 140°, 140° * Wrist flexion: Right: 80°, 82.5°, 87.5° Left: 70°, 75°, 82.5° Wrist extension: Right: 57.5°, 62.5°, 65° * Left: 67.5°, 67.5°, 70° |
| Rodgers, 1999 [23] (Non-randomized, non-controlled) | n = 18 (77.7% women) Score EDSS: 3.6 ± 2.1 Age: 43.2 ± 10.8 years Disease duration: NR MS type: NR | “Aerobic exercise program” Duration: 6 months Development: Cycle ergometry protocol (upright or recumbent ergometer depending on their ability level) Volume: 30 min Intensity: 65–70% age-predicted maximal heart rate Frequency: 3 times/week | Measurements of flexibility: - Range of motion during walking (ROM gait) - Passive Range of motion (PROM) “Using goniometers (°) and standard techniques (ankle, knee, and hip)” | - ROM during the gait cycle, mean (SD): Ankle dorsi-flexion: Pre: 7.1 (5.3)/Post: 77.0 (8.1)/p-value = 0.0007 * Ankle plantar-flexion: Pre: 101.0 (8.7)/Post: 108.9 (8.3)/p-value = 0.0001 * Ankle dorsi-plantar-flexion: Pre: 29.8 (7.1)/Post: 31.9 (8.8)/p-value = 0.204 Ankle angle at contact: Pre: 89.2 (5.3)/Post: 97.0 (7.3)/p-value = 0.0001 * Ankle angle at toe-off: Pre: 92.9 (9.1)/Post: 99.5 (10.7)/p-value = 0.003 * Knee flexion: Pre: 122.5 (9.3)/Post: 124.3 (11.0)/p-value = 0.178 Knee extension: Pre: 172.0 (6.4)/Post: 171.0 (6.1)/p-value = 0.339 Knee (flexo-extension): Pre: 49.5 (10.2)/Post: 46.6 (11.3)/p-value = 0.023 * Knee angle at contact: Pre: 165.1 (8.0)/Post: 165.6 (8.0)/p-value = 0.736 Knee angle at toe off: Pre: 142.4 (7.9)/Post: 143.4 (11.8)/p-value = 0.644 Hip extension: Pre: 176.0 (6.8)/Post: 172.0 (6.5)/p-value = 0.020 * Hip flexion: Pre: 151.1 (8.6)/Post: 151.0 (8.7)/p-value = 0.949 Hip flexo-extension: Pre: 24.9 (6.0)/Post: 21.0 (4.5)/p-value = 0.0029 * Hip angle at contact, flexo-extension: Pre: 156.6 (8.3)/Post: 157.8 (9.3)/p-value = 0.431 Hip angle at toe off, flexo-extension: Pre: 169.6 (6.9)/Post: 166.4 (7.3)/p-value = 0.052 Hip adduction: Pre: 189.3 (6.8)/Post: 196.7 (4.7)/p-value = 0.000 * Hip abduction: Pre: 172.2 (6.7)/182.2 (4.5)/p-value = 0.000 * Hip adduction-abduction: Pre: 16.5 (6.8)/Post: 13.0 (6.1)/p-value = 0.0712 Hip angle at contact, adduction-abduction: Pre: 180.5 (6.0)/Post: 189.9 (7.7)/p-value = 0.000 * Hip angle at toe off, adduction-abduction: Pre: 182.1 (8.0)/Post: 187.3 (10.7)/p-value = 0.071 - Passive ROM, mean (SD): Hip flexion (knee extended): Pre: 93.8 (11.4)/Post: 100.3 (7.0)/p-value = 0.034 * Hip flexion (knee flexed): Pre: 128.8 (9.1)/Post: 126.0 (10.6)/p-value = 0.154 Hip extension: Pre: 16.1 (3.8)/Post: 14.0 (2.5)/p-value = 0.092 Hip abduction: Pre: 32.6 (9.2)/Post: 40.0 (10.8)/p-value = 0.0006 * Hip adduction: Pre: 24.6 (9.7)/Post: 37.0 (13.0)/p-value = 0.001 * Hip external rotation: Pre: 31.0 (5.6)/Post: 40.6 (6.9)/p-value = 0.000 * Hip internal rotation: Pre: 34.3 (7.9)/Post: 37.8 (7.2)/p-value = 0.109 Knee flexion: Pre: 139.4 (6.4)/Post: 140.6 (4.7)/p-value = 0.125 Ankle plantar-flexion: Pre: 48.8 (6.0)/Post: 47.6 (3.6)/p-value = 0.503 Ankle dorsi-flexion: Pre: 10.2 (3.3)/Post: 11.5 (3.8)/p-value = 0.155 Subtalar inversion: Pre: 11.0 (2.3)/Post: 11.7 (2.6)/p-value = 0.263 Subtalar eversion: Pre: 8.2 (3.2)/Post: 9.3 (1.9)/p-value = 0.227 |
| Husted, 1999 [24] (Non-randomized, non-controlled) | n = 19 (84.2% women) Score EDSS: NR Age: NR Disease duration: NR MS type: RR: n = 11 (58%) PP: n = 5 (26%) NR: n = 4 (16%) | “Tai Chi program” Duration: 8 weeks Development: Volume: 1 h Frequency: 2 times/week | Flexibility: - Posterior kinetic chain (Hamstring flexibility test) | - Hamstring flexibility test: Pre: −5.3 cm/Post: −3.8 cm Change: 28% |
| First Author, Year | ||||
|---|---|---|---|---|
| Criteria (1–11) | McAuley, 2015 [18] | Duff, 2018 [19] | Pau, 2017 [20] | Ponzano, 2017 [21] |
| 1. Eligibility criteria | YES * | YES * | YES * | YES * |
| 2. Random allocation | YES | YES | YES | YES |
| 3. Concealed allocation | YES | NO | YES | NO |
| 4. Baseline comparability | YES | YES | YES | NO |
| 5. Blind subjects | NO | NO | NO | NO |
| 6. Blind therapists | YES | NO | NO | NO |
| 7. Blind assessors | YES | YES | NO | NO |
| 8. Key outcome (+85% subjects) | YES | YES | YES | YES |
| 9. Intention-to-treat-analysis | YES | YES | YES | NO |
| 10. Between-group comparisons | YES | YES | YES | NO |
| 11. Point estimates and variability | YES | YES | YES | YES |
| Score (0–10) | 9/10 | 7/10 | 7/10 | 3/10 |
| First Author, Year | |||
|---|---|---|---|
| Criteria (1–12) | Pereira, 2012 [22] | Rodger, 1999 [23] | Husted, 1999 [24] |
| 1. Was the study question or objective clearly stated? | YES | YES | NO |
| 2. Were eligibility/selection criteria for the study population prespecified and clearly described? | YES | NO | NO |
| 3. Were the participants in the study representative of those who would be eligible for the test/service/intervention in the general or clinical population of interest? | CD | CD | CD |
| 4. Were all the eligible participants that met the prespecified entry criteria enrolled? | YES | YES | YES |
| 5. Was the sample size sufficiently large to provide confidence in the findings? | NO | NO | NO |
| 6. Was the test/service/intervention clearly described and delivered consistently across the study population? | YES | YES | NO |
| 7. Were the outcome measures prespecified, clearly defined, valid, reliable, and assessed consistently across all study participants? | YES | YES | YES |
| 8. Were the people assessing the outcomes blinded to the participants’ exposures/interventions? | NO | NO | NO |
| 9. Was the loss to follow-up after baseline 20% or less? Were those lost to follow-up accounted for in the analysis? | NO | NO | NO |
| 10. Did the statistical methods examine changes in outcome measures from before to after the intervention? Were statistical tests done that provided p-values for the pre-to-post changes? | YES | YES | NO |
| 11. Were outcome measures of interest taken multiple times before the intervention and multiple times after the intervention (i.e., did they use and interrupted time-series design)? | YES | NO | NO |
| 12. If the intervention was conducted at a group level (e.g., a whole hospital, a community, etc.) did the statistical analysis take into account the use of individual-level data to determine effects at the group level? | NO | NO | NO |
| Score (0–12) | 7/12 | 5/12 | 2/12 |
| Criteria (1–16) | First Author, Year | ||||||
|---|---|---|---|---|---|---|---|
| McAuley, 2015 [18] | Duff, 2018 [19] | Pau, 2017 [20] | Ponzano, 2017 [21] | Pereira, 2012 [22] | Rodgers, 1999 [23] | Husted, 1999 [24] | |
| 1. Description of the type of exercise equipment | YES | YES | YES | YES | YES | YES | NO |
| 2. Description of the qualifications, expertise and/or training | YES | YES | YES | NO | NO | NO | NO |
| 3. Describe: exercises are individual or in a group | YES | YES | YES | NO | YES | YES | YES |
| 4. Describe: exercises are supervised or unsupervised; how they are delivered | YES | YES | YES | NO | YES | NO | YES |
| 5. Detailed description of how adherence to exercise is measured and reported | YES | NO | NO | NO | YES | NO | NO |
| 6. Detailed description of motivation strategies | YES | NO | NO | NO | NO | NO | NO |
| 7a. Detailed description of the decision rule(s) for determining exercise progression | YES | YES | YES | NO | YES | NO | NO |
| 7b. Detailed description of how the exercise program was progressed | YES | NO | YES | NO | YES | NO | NO |
| 8. Detailed description of each exercise to enable replication | YES | NO | YES | YES | YES | NO | NO |
| 9. Detailed description of any home program component | YES | NO | YES | YES | NO | NO | NO |
| 10. Describe whether there are any non-exercise components | YES | YES | NO | NO | NO | NO | NO |
| 11. Describe the type and number of adverse events that occur during exercise | NO | YES | YES | NO | YES | NO | NO |
| 12. Describe the setting in which the exercises are performed | YES | YES | YES | NO | YES | YES | YES |
| 13. Detailed description of the exercise intervention | YES | YES | YES | YES | YES | YES | YES |
| 14a. Describe whether the exercises are generic (one size fits all) or tailored | YES | YES | YES | YES | YES | YES | YES |
| 14b. Detailed description of how exercises are tailored to the individual | YES | NO | YES | NO | YES | YES | NO |
| 15. Describe the decision rule for determining the starting level | NO | NO | YES | YES | NO | NO | NO |
| 16a. Describe how adherence or fidelity is assessed/measured | YES | NO | YES | NO | NO | NO | NO |
| 16b. Describe the extent to which the intervention was delivered as planned | YES | YES | YES | YES | YES | YES | YES |
| Score (0–19) | 17/19 | 11/19 | 16/19 | 7/19 | 13/19 | 7/19 | 6/19 |
| First Author, Year | Variable | Group Comparison | Cohen’s d | 95% CI | |
|---|---|---|---|---|---|
| Lower Limit | Upper Limit | ||||
| McAuley, 2015 [18] | Sit and reach test | IG pre vs post | 0.19 | −0.38 | 0.75 |
| CG pre vs post | −0.06 | −0.62 | 0.51 | ||
| IG vs CG | −0.25 | −0.82 | 0.31 | ||
| Back Scratch test | IG pre vs post | −0.27 | −0.84 | 0.30 | |
| CG pre vs post | 0.85 | 0.26 | 1.44 | ||
| IG vs CG | 1.12 | 0.51 | 1.73 | ||
| Duff, 2018 [19] | Sit and Reach test | IG pre vs post | 0.17 | −0.54 | 0.89 |
| CG pre vs post | 0.19 | −0.53 | 0.90 | ||
| IG vs CG | −0.01 | −0.73 | 0.71 | ||
| Pau, 2017 [20] | ROM gait Hip flexion–extension | IG pre vs post | 0.42 | −0.42 | 1.27 |
| CG pre vs post | 0.16 | −0.67 | 1.00 | ||
| IG vs CG | 0.44 | −0.40 | 1.29 | ||
| ROM gait Knee flexion–extension | IG pre vs post | 0.47 | −0.38 | 1.32 | |
| CG pre vs post | 0.08 | −0.75 | 0.92 | ||
| IG vs CG | 0.31 | −0.54 | 1.15 | ||
| ROM gait Ankle dorsi–plantar–flexion | IG pre vs post | 0.39 | −0.46 | 1.23 | |
| CG pre vs post | 0.01 | −0.82 | 0.85 | ||
| IG vs CG | 0.30 | −0.54 | 1.14 | ||
| Rodgers, 1999 [23] | ROM gait Ankle dorsi-flexion | IG pre vs post | 0.84 | 0.16 | 1.53 |
| ROM gait Ankle plantar-flexion | IG pre vs post | 0.91 | 0.22 | 1.60 | |
| ROM gait Ankle (dorsi-plantar-flexion) | IG pre vs post | 0.26 | −0.40 | 0.91 | |
| ROM gait Ankle angle at contact | IG pre vs post | 1.20 | 0.48 | 1.91 | |
| ROM gait Ankle angle at toe-off | IG pre vs post | 0.65 | −0.02 | 1.32 | |
| ROM gait Knee flexion | IG pre vs post | 0.17 | −0.48 | 0.83 | |
| ROM gait Knee extension | IG pre vs post | −0.14 | −0.80 | 0.51 | |
| ROM gait Knee (flexo-extension) | IG pre vs post | −0.26 | −0.92 | 0.39 | |
| ROM gait Knee angle at contact | IG pre vs post | 0.06 | −0.59 | 0.72 | |
| ROM gait Knee angle at toe off | IG pre vs post | 0.10 | −0.56 | 0.75 | |
| ROM gait Hip extension | IG pre vs post | −0.59 | −1.26 | 0.08 | |
| ROM gait Hip flexion | IG pre vs post | −0.01 | −0.67 | 0.64 | |
| ROM gait Hip (flexo-extension) | IG pre vs post | −0.72 | −1.40 | −0.04 | |
| ROM gait Hip angle at contact (flexo-extension) | IG pre vs post | 0.13 | −0.52 | 0.79 | |
| ROM gait Hip angle at toe off (flexo-extension) | IG pre vs post | −0.44 | −1.10 | 0.22 | |
| ROM gait Hip adduction | IG pre vs post | 1.24 | 0.52 | 1.96 | |
| ROM gait Hip abduction | IG pre vs post | 2.06 | 1.23 | 2.88 | |
| ROM gait Hip (adduction–abduction) | IG pre vs post | −0.53 | −1.20 | 0.14 | |
| ROM gait Hip angle at contact (adduc–abduc) | IG pre vs post | 1.33 | 0.60 | 2.06 | |
| ROM gait Hip angle at toe off (adduction–abduction) | IG pre vs post | 0.54 | 0.13 | 1.21 | |
| PROM Hip flexion (knee extended) | IG pre vs post | 0.67 | 0.00 | 1.35 | |
| PROM Hip flexion (knee flexed) | IG pre vs post | −0.28 | −0.93 | 0.38 | |
| PROM Hip extension | IG pre vs post | −0.64 | −1.31 | 0.03 | |
| PROM Hip abduction | IG pre vs post | 0.72 | 0.04 | 1.40 | |
| PROM Hip adduction | IG pre vs post | 1.06 | 0.35 | 1.76 | |
| PROM Hip external rotation | IG pre vs post | 1.49 | 0.75 | 2.24 | |
| PROM Hip internal rotation | IG pre vs post | 0.45 | −0.21 | 1.12 | |
| PROM Knee flexion | IG pre vs post | 0.21 | −0.45 | 0.86 | |
| PROM Ankle plantar-flexion | IG pre vs post | −0.24 | −0.89 | 0.42 | |
| PROM Ankle dorsi-flexion | IG pre vs post | 0.36 | −0.30 | 1.02 | |
| PROM Subtalar inversion | IG pre vs post | 0.28 | −0.38 | 0.94 | |
| PROM Subtalar eversion | IG pre vs post | 0.41 | −0.25 | 1.07 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Torres-Pareja, M.; Sánchez-Lastra, M.A.; Iglesias, L.; Suárez-Iglesias, D.; Mendoza, N.; Ayán, C. Exercise Interventions for Improving Flexibility in People with Multiple Sclerosis: A Systematic Review and Meta-Analysis. Medicina 2019, 55, 726. https://doi.org/10.3390/medicina55110726
Torres-Pareja M, Sánchez-Lastra MA, Iglesias L, Suárez-Iglesias D, Mendoza N, Ayán C. Exercise Interventions for Improving Flexibility in People with Multiple Sclerosis: A Systematic Review and Meta-Analysis. Medicina. 2019; 55(11):726. https://doi.org/10.3390/medicina55110726
Chicago/Turabian StyleTorres-Pareja, Marta, Miguel A. Sánchez-Lastra, Laura Iglesias, David Suárez-Iglesias, Nuria Mendoza, and Carlos Ayán. 2019. "Exercise Interventions for Improving Flexibility in People with Multiple Sclerosis: A Systematic Review and Meta-Analysis" Medicina 55, no. 11: 726. https://doi.org/10.3390/medicina55110726
APA StyleTorres-Pareja, M., Sánchez-Lastra, M. A., Iglesias, L., Suárez-Iglesias, D., Mendoza, N., & Ayán, C. (2019). Exercise Interventions for Improving Flexibility in People with Multiple Sclerosis: A Systematic Review and Meta-Analysis. Medicina, 55(11), 726. https://doi.org/10.3390/medicina55110726





