Use of Magnetic Resonance Imaging in Evaluating Fetal Brain and Abdomen Malformations during Pregnancy
Abstract
:1. Introduction
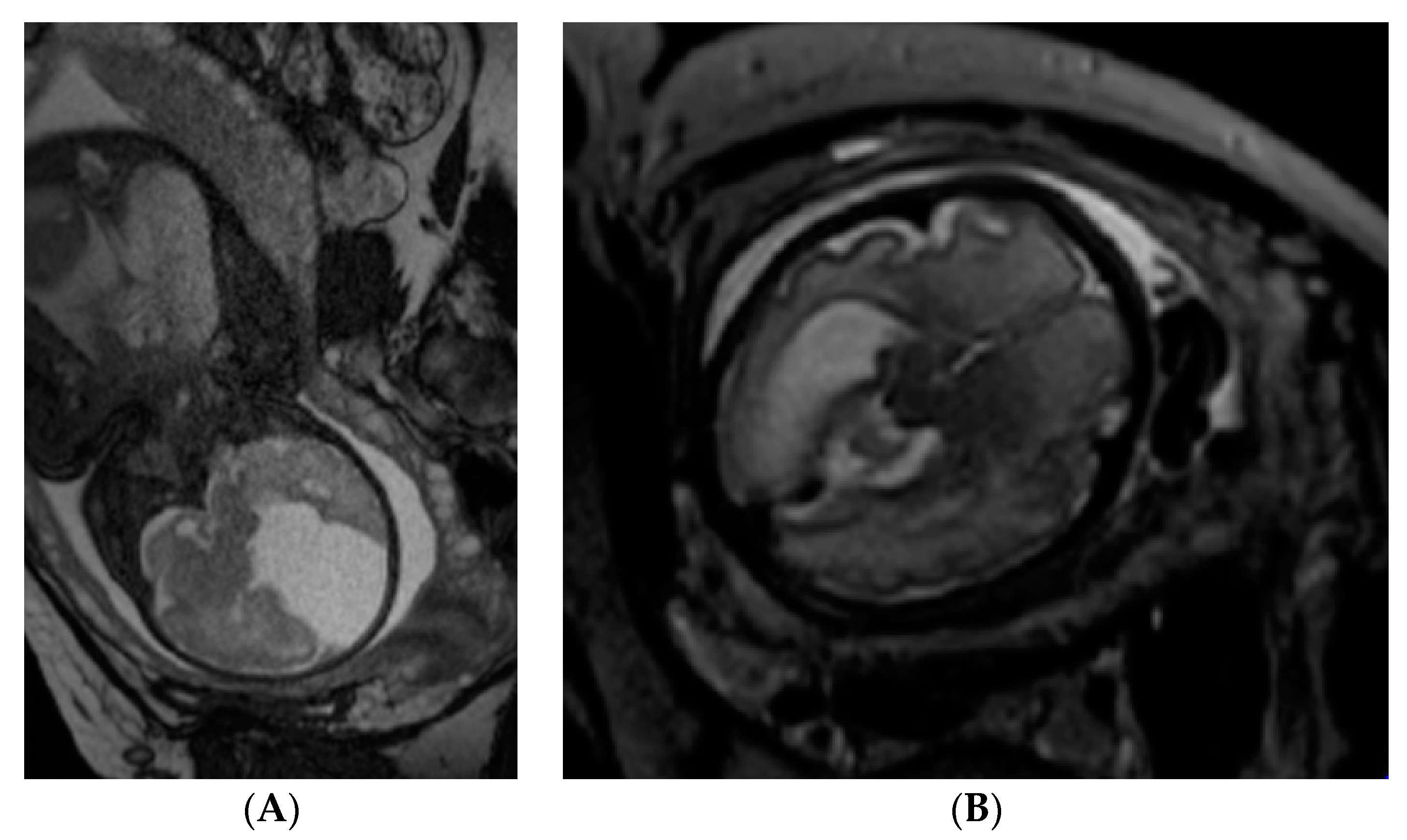
2. Fetal MRI Sequences
3. Evaluating the Fetal Brain
4. Evaluating the Fetal Abdomen
5. Safety
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bulas, D.; Egloff, A. Benefits and risks of MRI in pregnancy. Semin. Perinatol. 2013, 37, 301–304. [Google Scholar] [CrossRef]
- Levine, D. Timing of MRI in pregnancy, repeat exams, access, and physician qualifications. Semin. Perinatol. 2013, 37, 340–344. [Google Scholar] [CrossRef] [PubMed]
- Huisman, T.A.G.M. Fetal Magnetic Resonance Imaging. Semi. Roentgenol. 2008, 43, 314–336. [Google Scholar] [CrossRef] [PubMed]
- Manganaro, L.; Bernardo, S.; Antonelli, A.; Vinci, V.; Saldari, M.; Catalano, C. Fetal MRI of the central nervous system: State-of-the-art. Eur. J. Radiol. 2017, 93, 273–283. [Google Scholar] [CrossRef] [PubMed]
- Saleem, S.N. Fetal MRI: An approach to practice: A review. J. Adv. Res. 2014, 5, 507–523. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glenn, O.A. MR imaging of the fetal brain. Pediatr. Radiol. 2010, 40, 68–81. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, P.; Reeves, M.; Morris, J.; Mason, G.; Russell, S.; Paley, M.; Whitby, E. A Prospective Study of Fetuses with Isolated Ventriculomegaly Investigated by Antenatal Sonography and In Utero MR Imaging. Am. J. Neuroradiol. 2009, 31, 106–111. [Google Scholar] [CrossRef] [Green Version]
- Hetts, S.W.; Sherr, E.H.; Chao, S.; Gobuty, S.; Barkovich, A.J. Anomalies of the Corpus Callosum: An MR Analysis of the Phenotypic Spectrum of Associated Malformations. Am. J. Roentgenol. 2006, 187, 1343–1348. [Google Scholar] [CrossRef]
- Furey, E.A.; Bailey, A.A.; Twickler, D.M. Fetal MR Imaging of Gastrointestinal Abnormalities. RadioGraphics 2016, 36, 904–917. [Google Scholar] [CrossRef]
- Brugger, P.C.; Prayer, D. Fetal abdominal magnetic resonance imaging. Eur. J. Radiol. 2006, 57, 278–293. [Google Scholar] [CrossRef]
- Huisman, T.A.; Kellenberger, C.J. MR imaging characteristics of the normal fetal gastrointestinal tract and abdomen. Eur. J. Radiol. 2008, 65, 170–181. [Google Scholar] [CrossRef] [PubMed]
- Manganaro, L.; Saldari, M.; Bernardo, S.; Vinci, V.; Aliberti, C.; Sollazzo, P.; Giancotti, A.; Capozza, F.; Porpora, M.G.; Cozzi, D.A.; et al. Role of magnetic resonance imaging in the prenatal diagnosis of gastrointestinal fetal anomalies. Radiol. Med. 2014, 120, 393–403. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, M.R.; Ten, P.M.; Pedregosa, J.P.; López, C.B.; Degenhardt, I.T.; Abascal, I.P. Fetal MRI: Thoracic, abdominal and pelvic pathology. EPOS 2012, 76, 9–28. [Google Scholar]
- Mehollin-Ray, A.R.; Cassady, C.I.; Cass, D.L.; Olutoye, O.O. Fetal MR Imaging of Congenital Diaphragmatic Hernia. RadioGraphics 2012, 32, 1067–1084. [Google Scholar] [CrossRef] [PubMed]
- Diagnostic Imaging in Pregnant and Nursing Women—UpToDate. Available online: https://www-uptodate-com.ezproxy.dbazes.lsmuni.lt/contents/diagnostic-imaging-in-pregnant-and-nursing-women?search=Diagnostic%20imaging%20in%20pregnant%20and%20nursing%20women&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1 (accessed on 5 November 2018).
- Plunk, M.R.; Chapman, T. The Fundamentals of Fetal MR Imaging: Part 1. Curr. Prob. Diagn. Radiol. 2014, 43, 331–346. [Google Scholar] [CrossRef] [PubMed]
- Hand, J.; Li, Y.; Thomas, E.; Rutherford, M.; Hajnal, J. Prediction of specific absorption rate in mother and fetus associated with MRI examinations during pregnancy. Magn. Reson. Med. 2006, 55, 883–893. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strizek, B.; Jani, J.C.; Mucyo, E.; De Keyzer, F.; Pauwels, I.; Ziane, S.; Mansbach, A.-L.; Deltenre, P.; Cos, T.; Cannie, M.M.; et al. Safety of MR Imaging at 1.5 T in Fetuses: A Retrospective Case-Control Study of Birth Weights and the Effects of Acoustic Noise. Radiology 2015, 275, 530–537. [Google Scholar] [CrossRef]
- Bharatha, A.; Ray, J.G.; Vermeulen, M.J.; Montanera, W.J.; Park, A.L. Association Between MRI Exposure During Pregnancy and Fetal and Childhood Outcomes. JAMA 2016, 316, 952–961. [Google Scholar]
- Bouyssi-Kobar, M.; Du Plessis, A.J.; Robertson, R.L.; Limperopoulos, C. Fetal magnetic resonance imaging: Exposure times and functional outcomes at preschool age. Pediatr. Radiol. 2015, 45, 1823–1830. [Google Scholar] [CrossRef]
- Leyendecker, J.R.; Gorengaut, V.; Brown, J.J. MR Imaging of Maternal Diseases of the Abdomen and Pelvis during Pregnancy and the Immediate Postpartum Period. RadioGraphics 2004, 24, 1301–1316. [Google Scholar] [CrossRef]
- Sundgren, P.C.; Leander, P. Is administration of gadolinium-based contrast media to pregnant women and small children justified? J. Magn. Reson. Imaging 2011, 34, 750–757. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woods, M.; Oh, K.Y.; Roberts, V.H.J.; Schabel, M.C.; Grove, K.L.; Frias, A.E. Gadolinium Chelate Contrast Material in Pregnancy: Fetal Biodistribution in the Nonhuman Primate. Radiology 2015, 276, 110–118. [Google Scholar]
- Prola-Netto, J.; Woods, M.; Roberts, V.H.J.; Sullivan, E.L.; Miller, C.A.; Frias, A.E.; Oh, K.Y. Gadolinium Chelate Safety in Pregnancy: Barely Detectable Gadolinium Levels in the Juvenile Nonhuman Primate after in Utero Exposure. Radiology 2017, 286, 122–128. [Google Scholar] [CrossRef] [PubMed]

© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Valevičienė, N.R.; Varytė, G.; Zakarevičienė, J.; Kontrimavičiūtė, E.; Ramašauskaitė, D.; Rutkauskaitė-Valančienė, D. Use of Magnetic Resonance Imaging in Evaluating Fetal Brain and Abdomen Malformations during Pregnancy. Medicina 2019, 55, 55. https://doi.org/10.3390/medicina55020055
Valevičienė NR, Varytė G, Zakarevičienė J, Kontrimavičiūtė E, Ramašauskaitė D, Rutkauskaitė-Valančienė D. Use of Magnetic Resonance Imaging in Evaluating Fetal Brain and Abdomen Malformations during Pregnancy. Medicina. 2019; 55(2):55. https://doi.org/10.3390/medicina55020055
Chicago/Turabian StyleValevičienė, Nomeda Rima, Guoda Varytė, Jolita Zakarevičienė, Eglė Kontrimavičiūtė, Diana Ramašauskaitė, and Dileta Rutkauskaitė-Valančienė. 2019. "Use of Magnetic Resonance Imaging in Evaluating Fetal Brain and Abdomen Malformations during Pregnancy" Medicina 55, no. 2: 55. https://doi.org/10.3390/medicina55020055
APA StyleValevičienė, N. R., Varytė, G., Zakarevičienė, J., Kontrimavičiūtė, E., Ramašauskaitė, D., & Rutkauskaitė-Valančienė, D. (2019). Use of Magnetic Resonance Imaging in Evaluating Fetal Brain and Abdomen Malformations during Pregnancy. Medicina, 55(2), 55. https://doi.org/10.3390/medicina55020055




