Ultrasonographic Evaluation of The Effects of Orthodontic or Functional Orthopaedic Treatment on Masseter Muscles: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.2.1. Population
2.2.2. Intervention
- vertical plane (i.e., dolichocephalic patients whose treatment could include bite-block or rapid/slow palatal expander cemented on permanent or deciduous molars);
- sagittal plane (i.e., patients with Class II malocclusion treated with twin block or any device for mandibular advancement)
- transversal plane (i.e., patients with lateral cross-bite in therapy with quad helix or rapid/slow maxillary expander).
2.2.3. Comparison
2.2.4. Outcomes
2.2.5. Study Design
2.3. Information Sources and Search
2.4. Study Selection
2.5. Data Collection Process
2.6. Outcome
2.7. Risk of Bias in Individual Studies and Quality of Evidence
2.8. Data Synthesis
3. Results
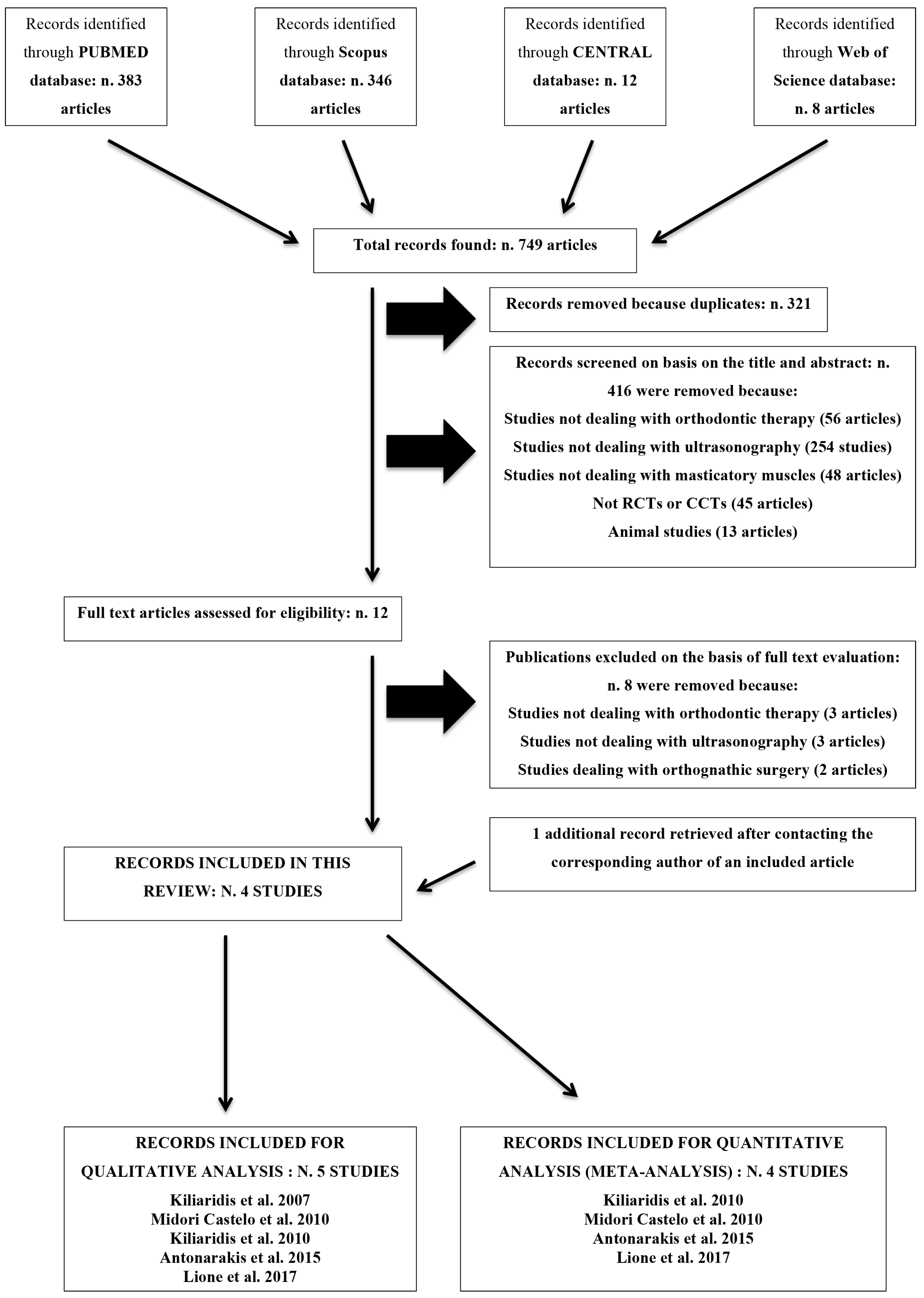
3.1. Results of the Search
3.2. Exclusion of Studies
3.3. Included Studies
3.4. Characteristics of Participants
3.5. Characteristics of Interventions
3.6. Characteristics of Outcome Measures
3.7. Risk of Bias in Included Studies and Strength of Evidence
3.8. Effects of Interventions
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Soyoye, O.A.; Otuyemi, O.D.; Kolawole, K.A.; Ayoola, O.O. Relationship between masseter muscle thickness and maxillofacial morphology in pre-orthodontic treatment patients. Int. Orthod. 2018, 16, 698–711. [Google Scholar] [CrossRef] [PubMed]
- Lione, R.; Franchi, L.; Noviello, A.; Bollero, P.; Fanucci, E.; Cozza, P. Three-dimensional evaluation of masseter muscle in different vertical facial patterns: A cross-sectional study in growing children. Ultrason. Imaging 2013, 35, 307–317. [Google Scholar] [CrossRef] [PubMed]
- Farronato, G.; Giannini, N.; Galbiati, G.; Sesso, G.; Maspero, C. Orthodontic-surgical treatment: Neuromuscular evaluation in skeletal Class II and Class III patients. Prog. Orthod. 2012, 13, 226–236. [Google Scholar] [CrossRef] [PubMed]
- Farronato, G.; Giannini, N.; Riva, R.; Galbiati, G.; Maspero, C. Correlations between malocclusions and dyslalias. Eur. J. Paediatr. Dent. 2012, 13, 13–18. [Google Scholar]
- Farronato, G.; Giannini, N.; Galbiati, G.; Stabilini, S.A.; Sarcina, M.; Maspero, C. Functional evaluation in orthodontic surgical treatment: Long-term stability and predictability. Prog. Orthod. 2015, 16, 30. [Google Scholar] [CrossRef][Green Version]
- Bishara, S.E.; Ziaja, R.R. Functional appliances: A review. Am. J. Orthod. Dentofac. Orthop. 1989, 95, 250–258. [Google Scholar] [CrossRef]
- Türker, K.S. Electromyography: Some methodological problems and issues. Phys. Ther. 1993, 73, 698–710. [Google Scholar] [CrossRef]
- Kiliaridis, S.; Mahboubi, P.H.; Raadsheer, M.C.; Katsaros, C. Ultrasonographic thickness of the masseter muscle in growing individuals with unilateral crossbite. Angle Orthod. 2007, 77, 607–611. [Google Scholar] [CrossRef]
- Midori Castelo, P.; Duarte Gavião, M.B.; Pereira, L.J.; Bonjardim, L.R. Evaluation of changes in muscle thickness, bite force and facial asymmetry during early treatment of functional posterior crossbite. J. Clin. Pediatr. Dent. 2010, 34, 369–374. [Google Scholar] [CrossRef]
- Kiliaridis, S.; Mills, C.M.; Antonarakis, G.S. Masseter muscle thickness as a predictive variable in treatment outcome of the twin-block appliance and masseteric thickness changes during treatment. Orthod. Craniofac. Res. 2010, 13, 203–213. [Google Scholar] [CrossRef]
- Antonarakis, G.S.; Kiliaridis, S. Predictive value of masseter muscle thickness and bite force on Class II functional appliance treatment: A prospective controlled study. Eur. J. Orthod. 2015, 37, 570–577. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Liberati, A.; Altman, D.J.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Deveraux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef] [PubMed]
- The Nordic Cochrane Center, The Cochrane Collaboration. Review Manager (Rev Man); Version 5.2; The Nordic Cochrane Center, The Cochrane Collaboration: Copenhagen, Denmark, 2013. [Google Scholar]
- Lione, R.; Kiliaridis, S.; Noviello, A.; Franchi, L.; Antonarakis, G.S.; Cozza, P. Evaluation of masseter muscle in relation to treatment with removable bite-blocks in dolichofacial growing subjects: A prospective controlled study. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 1058–1064. [Google Scholar] [CrossRef] [PubMed]
- Becht, M.P.; Mah, J.; Martin, C.; Razmus, T.; Gunel, E.; Ngan, P. Evaluation of masseter muscle morphology in different types of malocclusions using cone beam computed tomography. Int. Orthod. 2014, 12, 32–48. [Google Scholar] [CrossRef] [PubMed]
- Kiliaridis, S.; Georgiakaki, I.; Katsaros, C. Masseter muscle thickness and maxillary dental arch width. Eur. J. Orthod. 2003, 25, 259–263. [Google Scholar] [CrossRef] [PubMed]
- Kitai, N.; Fujii, Y.; Murakami, S.; Furukawa, S.; Kreiborg, S.; Takada, K. Human masticatory muscle volume and zygomatico-mandibular form in adults with mandibular prognathism. J. Dent. Res. 2002, 81, 752–756. [Google Scholar] [CrossRef]
- Antonarakis, G.S.; Kjellberg, H.; Kiliaridis, S. Bite force and its association with stability following Class II/1 functional appliance treatment. Eur. J. Orthod. 2013, 35, 434–441. [Google Scholar] [CrossRef] [PubMed]
- Chintakanon, K.; Türker, K.S.; Sampson, W.; Wilkinson, T.; Townsend, G. Effects of twin-block therapy on protrusive muscle functions. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 392–396. [Google Scholar] [CrossRef]
- Dahl, B.L.; Krogstad, B.S.; Øgaard, B.; Eckersberg, T. Differences in functional variables, fillings, and tooth wear in two groups of 19-year-old individuals. Acta Odontol. Scand. 1989, 47, 35–40. [Google Scholar] [CrossRef]
- Lee, D.H.; Yu, H.S. Masseter muscle changes following orthognathic surgery. A long-term three-dimensional computed tomography follow-up. Angle Orthod. 2012, 82, 792–798. [Google Scholar] [CrossRef]
- Trawitzki, L.V.; Dantas, R.O.; Elias-Júnior, J.; Mello-Filho, F.V. Masseter muscle thickness three years after surgical correction of class III dentofacial deformity. Arch. Oral Biol. 2011, 56, 799–803. [Google Scholar] [CrossRef] [PubMed]
- Patini, R.; Staderini, E.; Gallenzi, P. Multidisciplinary surgical management of Cowden syndrome: Report of a case. J. Clin. Exp. Dent. 2016, 18, 472–474. [Google Scholar] [CrossRef] [PubMed]
- Mills, C.M.; McCulloch, K.J. Treatment effects of the twin-block appliance: A cephalometric study. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 24–33. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, J.P.; Grobéty, D. The Class II malocclusion: Differential diagnosis and clinical application of activators, extraoral traction, and fixed appliances. Am. J. Ortohod. 1975, 68, 499–544. [Google Scholar] [CrossRef]
- Pfeiffer, J.P.; Grobéty, D. A philosophy of combined orthopedic-orthodontic treatment. Am. J. Orthod. 1982, 81, 185–201. [Google Scholar] [CrossRef]
- Tulloch, J.F.C.; Medland, W.; Tuncay, O.C. Methods used to evaluate growth modification in Class II malocclusion. Am. J. Orthod. Dentofac. Orthop. 1990, 98, 340–347. [Google Scholar] [CrossRef]
- Woodside, D.G. Do functional appliances have and orthopaedic effect? Am. J. Orthod. Dentofac. Orthop. 1998, 113, 11–14. [Google Scholar] [CrossRef]
- Patini, R.; Gallenzi, P.; Spagnuolo, G.; Cordaro, M.; Cantiani, M.; Amalfitano, A.; Arcovito, A.; Callà, C.A.M.; Mingrone, G.; Nocca, G. Correlation between metabolic syndrome, periodontitis and reactive oxygen species production. A pilot study. Open Dent. J. 2017, 11, 621–627. [Google Scholar] [CrossRef]
- Wieslander, J. Long-term effect of treatment with the headgear-Herbst appliance in the early mixed dentition. Stability or relapse? Am. J. Orthod. Dentofac. Orthop. 1993, 104, 319–329. [Google Scholar] [CrossRef]
- Manfredi, C.; Cimino, R.; Trani, A.; Pancherz, H. Skeletal changes of Herbst appliance therapy investigated with more conventional cephalometric and European norms. Angle Orthod. 2001, 71, 170–176. [Google Scholar]
- Raadsheer, M.C.; Kiliaridis, S.; van Eijden, T.M.G.J.; Van Ginkel, F.C.; Prahl-Andersen, B. Masseter muscle thickness in growing individuals and its relation to facial morphology. Arch. Oral Biol. 1996, 41, 323–332. [Google Scholar] [CrossRef]
- Patini, R.; Staderini, E.; Lajolo, C.; Lopetuso, L.; Mohammed, H.; Rimondini, L.; Rocchetti, V.; Franceschi, F.; Cordaro, M.; Gallenzi, P. Relationship between oral microbiota and periodontal disease: A systematic review. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 5775–5788. [Google Scholar] [PubMed]
- Freeland, T.D. Muscle function during treatment with the functional regulator. Angle Orthod. 1979, 49, 247–258. [Google Scholar] [PubMed]
- Sessle, B.J.; Woodside, D.G.; Bourque, P.; Gurza, S.; Powell, G.; Voudouris, J.; Metaxas, A.; Altuna, G. Effect of functional appliances on jaw muscle activity. Am. J. Orthod. Dentofac. Orthop. 1990, 98, 222–230. [Google Scholar] [CrossRef]
- Miralles, R.; Berger, B.; Bull, R.; Manns, A.; Carvajal, R. Influence of the activator on electromyographic activity of mandibular elevator muscles. Am. J. Orthod. Dentofac. Orthop. 1988, 94, 97–103. [Google Scholar] [CrossRef]
- Patini, R.; Arrica, M.; Di Stasio, E.; Gallenzi, P.; Cordaro, M. The use of magnetic resonance imaging in the evaluation of upper airway structures in paediatric obstructive sleep apnoea syndrome: A systematic review and meta-analysis. Dentomaxillofac. Radiol. 2016, 45, 20160136. [Google Scholar] [CrossRef] [PubMed]
- Okada, C.; Yamaguchi, S.; Watanabe, Y.; Watanabe, M.; Hattori, Y. Evaluation of masticatory activity during unilateral single tooth clenching using muscle functional magnetic resonance imaging. J. Oral Rehabil. 2016, 43, 583–590. [Google Scholar] [CrossRef]
- Yamaguchi, S.; Itoh, S.; Watanabe, Y.; Tsuboi, A.; Watanabe, M. Quantitative analysis of masticatory activity during unilateral mastication using muscle fMRI. Oral Dis. 2011, 17, 407–413. [Google Scholar] [CrossRef]
- Staderini, E.; Patini, R.; De Luca, M.; Gallenzi, P. Three-dimensional stereophotogrammetric analysis of nasolabial soft tissue effects of rapid maxillary expansion: A systematic review of clinical trials. Acta Otorhinolaryngol. Italica 2018, 38, 399–408. [Google Scholar]

| References | Rationale for Exclusion |
|---|---|
| Becht et al. [15] | Not dealing with orthodontic therapy |
| Kiliaridis et al. [16] | Not dealing with orthodontic therapy |
| Kitai et al. [17] | Not dealing with orthodontic therapy |
| Antonarakis et al. [18] | Not dealing with ultrasonography |
| Chintakanon et al. [19] | Not dealing with ultrasonography |
| Dahl et al. [20] | Not dealing with ultrasonography |
| Lee et al. [21] | Dealing with orthognathic surgery |
| Trawitzki et al. [22] | Dealing with orthognathic surgery |
| Title | Author (Year) | Type of Study | Sample Size | Mean Age at Start of Treatment in Years (SD, Range) | Mean Duration of Therapy in Months (SD, Range) | Type of Ultrasonography |
|---|---|---|---|---|---|---|
| Ultrasonographic thickness of the masseter muscle in growing individuals with unilateral crossbite. | Kiliaridis et al. (2007) | Controlled clinical trial | 38 (17 M and 21 F) in untreated group; 18 (9 M and 9 F) in treated group; 28 (No information about sex.) in age-adjusted control group. | 11.9 (NR, 8.1–17.8) in untreated group; 16.3 (NR, 12.0–22.0) in treated group; 16.1 (NR, 15.2–18.2) in age-adjusted control group. | NR | Scanner 480, 7.5 MHz. Pie Medical, Maastricht, The Netherlands. |
| Evaluation of changes in muscle thickness, bite force and facial asymmetry during early treatment of functional posterior crossbite. | Midori Castelo et al. (2010) | Controlled clinical trial | 23 (9 M and 14 F). | 5 (0.4, NR) in deciduous dentition group; 6 (0.6, NR) in mix dentition group. | 13.64 (5.07, NR) in deciduous dentition group; 16.25 (5.40, NR) in mix dentition group. | Just Vision, 56 mm/10 MHz. Toshiba Co., Minato-ku, Tokio, Japan. |
| Masseter muscle thickness as a predictive variable in treatment outcome of the twin-block appliance and masseteric thickness changes during treatment. | Kiliaridis et al. (2010) | Controlled clinical trial | 22 (8 M and 14 F) in treated group; 22 (12 M and 10 F) in control group. | 9.4 (NR, 8–12) in treated group; 9.8 (NR, 8–12) in control group. | 13.5 (NR, 11–17) | Scanner 480, 7.5 MHz. Pie Medical, Maastricht, The Netherlands. |
| Predictive value of masseter muscle thickness and bite force on Class II functional appliance treatment: a prospective controlled study. | Antonarakis et al. (2015) | Controlled clinical trial | 20 in treated group and 20 in control group. No information about sex. | 11.4 (1.3, 9–13) in treated group; 11.2 (1.9, 9–13) in control group. | 12 (NR, NR) | FALCO 100, 6–8 MHz, Pie Medical, Maastricht, The Netherlands. |
| Evaluation of masseter muscles in relation to treatment with removable bite-blocks in dolichofacial growing subjects: a prospective controlled study. | Lione et al. (2017) | Controlled clinical trial | 21 (9 M and 12 F) in treated group; 21 (9 M and 12 F) in control group. | 9.9 (1.4, 8.5–11.1) in treated group; 9.6 (1.6, NR) in control group. | 12 (NR, NR) | NR |
| Title | Author (Year) | Selection | Comparability | Exposure | Number of Stars | Risk of Bias |
|---|---|---|---|---|---|---|
| Ultrasonographic thickness of the masseter muscle in growing individuals with unilateral crossbite. | Kiliaridis et al. (2007) | * | * | * | 3 | High |
| Evaluation of changes in muscle thickness, bite force and facial asymmetry during early treatment of functional posterior crossbite. | Midori Castelo et al. (2010) | **** | ** | ** | 8 | Low |
| Masseter muscle thickness as a predictive variable in treatment outcome of the twin-block appliance and masseteric thickness changes during treatment. | Kiliaridis et al. (2010) | *** | 0 | ** | 5 | Medium |
| Predictive value of masseter muscle thickness and bite force on Class II functional appliance treatment: a prospective controlled study. | Antonarakis et al. (2015) | *** | ** | ** | 7 | Medium |
| Evaluation of masseter muscles in relation to treatment with removable bite-blocks in dolichofacial growing subjects: a prospective controlled study. | Lione et al. (2017) | ** | ** | ** | 6 | Medium |
| Quality Assessment, Outcome: Masseter Muscle Thickness during Orthodontic Therapy | ||||||
|---|---|---|---|---|---|---|
| Question: Will the Use of Orthodontic Appliances Have an Effect on Masseter Muscle Thickness? | ||||||
| Number of Studies According to Meta-Analysis | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Publication Bias |
| 4 (Figure 2) | Clinical Controlled Trials | Not Serious | Serious a | Not Serious | Serious b | Undetected |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patini, R.; Gallenzi, P.; Lione, R.; Cozza, P.; Cordaro, M. Ultrasonographic Evaluation of The Effects of Orthodontic or Functional Orthopaedic Treatment on Masseter Muscles: A Systematic Review and Meta-Analysis. Medicina 2019, 55, 256. https://doi.org/10.3390/medicina55060256
Patini R, Gallenzi P, Lione R, Cozza P, Cordaro M. Ultrasonographic Evaluation of The Effects of Orthodontic or Functional Orthopaedic Treatment on Masseter Muscles: A Systematic Review and Meta-Analysis. Medicina. 2019; 55(6):256. https://doi.org/10.3390/medicina55060256
Chicago/Turabian StylePatini, Romeo, Patrizia Gallenzi, Roberta Lione, Paola Cozza, and Massimo Cordaro. 2019. "Ultrasonographic Evaluation of The Effects of Orthodontic or Functional Orthopaedic Treatment on Masseter Muscles: A Systematic Review and Meta-Analysis" Medicina 55, no. 6: 256. https://doi.org/10.3390/medicina55060256
APA StylePatini, R., Gallenzi, P., Lione, R., Cozza, P., & Cordaro, M. (2019). Ultrasonographic Evaluation of The Effects of Orthodontic or Functional Orthopaedic Treatment on Masseter Muscles: A Systematic Review and Meta-Analysis. Medicina, 55(6), 256. https://doi.org/10.3390/medicina55060256







