Cardiac Magnetic Resonance Imaging and Transthoracic Echocardiography: Investigation of Concordance between the Two Methods for Measurement of the Cardiac Chamber
Abstract
:1. Introduction
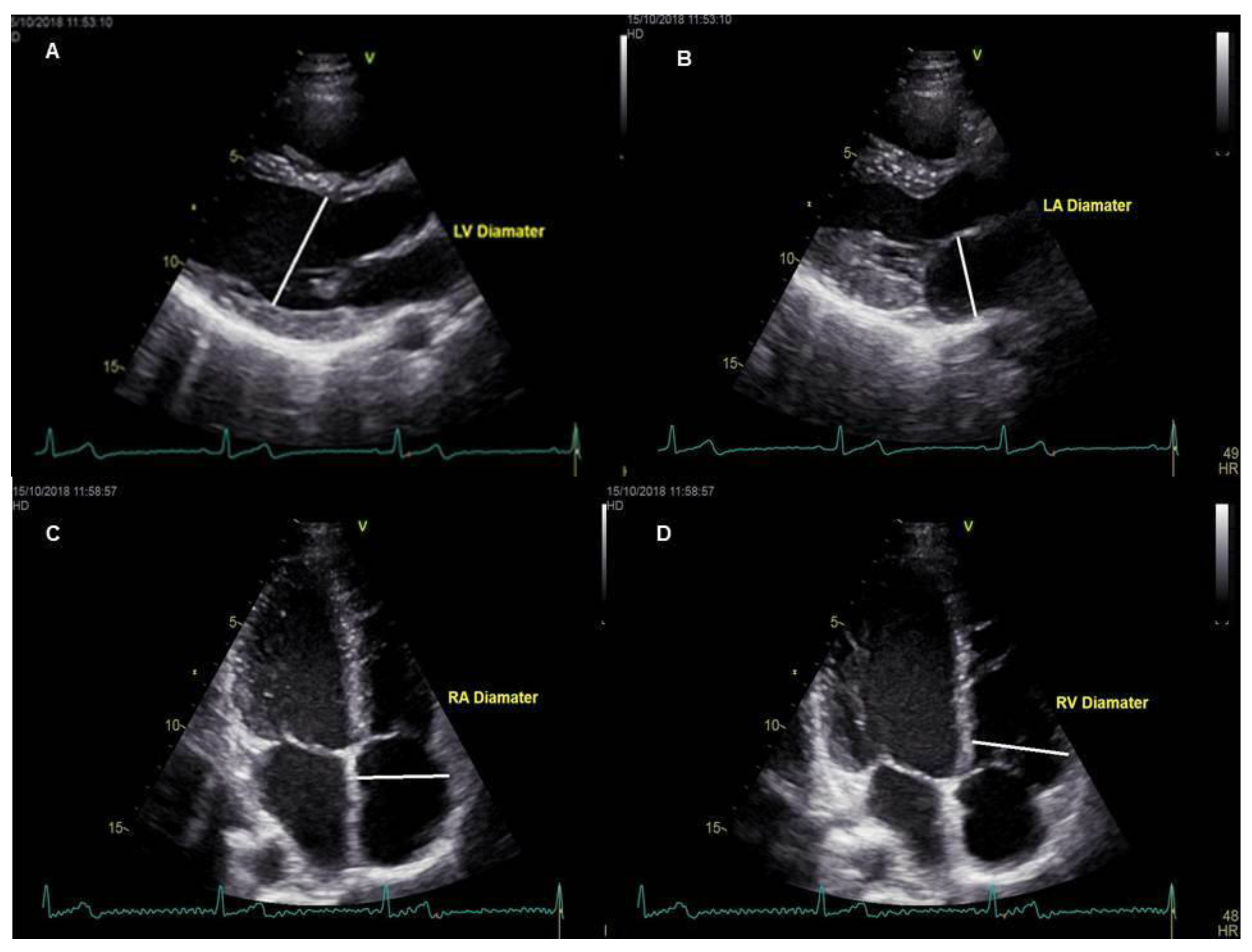
2. Materials and Methods
2.1. Subject Selection and Imaging Protocols
2.2. Statistical Examinations
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Lapinskas, T. Ischemic heart disease: A comprehensive evaluation using cardiovascular magnetic resonance. Medicina (Kaunas) 2013, 49, 97–110. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 28, 1–39. [Google Scholar] [CrossRef] [PubMed]
- Epstein, F.H. MRI of left ventricular function. J. Nucl. Cardiol. 2007, 14, 729–744. [Google Scholar] [CrossRef] [PubMed]
- Salerno, M.; Sharif, B.; Arheden, H.; Kumar, A.; Axel, L.; Li, D. Recent Advances in Cardiovascular Magnetic Resonance: Techniques and Applications. Circ. Cardiovasc. Imaging 2017, 10. [Google Scholar] [CrossRef] [PubMed]
- Kawel-Boehm, N.; Maceira, A.; Valsangiacomo-Buechel, E.R.; Vogel-Claussen, J.; Turkbey, E.B.; Williams, R.; Plein, S.; Tee, M.; Eng, J.; Bluemke, D.A. Normal values for cardiovascular magnetic resonance in adults and children. J. Cardiovasc. Magn. Reson. 2015, 17, 29. [Google Scholar] [CrossRef] [PubMed]
- Aurich, M.; André, F.; Keller, M.; Greiner, S.; Hess, A.; Buss, S.J.; Katus, H.A.; Mereles, D. Assessment of left ventricular volumes with echocardiography and cardiac magnetic resonance imaging: Real-life evaluation of standard versus new semiautomatic methods. J. Am. Soc. Echocardiogr. 2014, 27, 1017–1024. [Google Scholar] [CrossRef] [PubMed]
- Gardner, B.I.; Bingham, S.E.; Allen, M.R.; Blatter, D.D.; Anderson, J.L. Cardiac magnetic resonance versus transthoracic echocardiography for the assessment of cardiac volumes and regional function after myocardial infarction: An intrasubject comparison using simultaneous intrasubject recordings. Cardiovasc. Ultrasound. 2009, 7, 38. [Google Scholar] [CrossRef] [PubMed]
- Hazirolan, T.; Taşbaş, B.; Dağoğlu, M.G.; Canyiğit, M.; Abali, G.; Aytemir, K.; Oto, A.; Balkanci, F. Comparison of short and long axis methods in cardiac MR imaging and echocardiography for left ventricular function. Diagn. Interv. Radiol. 2007, 13, 33–38. [Google Scholar] [PubMed]
- Puntmann, V.O.; Gebker, R.; Duckett, S.; Mirelis, J.; Schnackenburg, B.; Graefe, M.; Razavi, R.; Fleck, E.; Nagel, E. Left ventricular chamber dimensions and wall thickness by cardiovascular magnetic resonance: Comparison with transthoracic echocardiography. Eur. Heart J. Cardiovasc. Imaging 2013, 14, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Gopal, A.S.; Chukwu, E.O.; Iwuchukwu, C.J.; Katz, A.S.; Toole, R.S.; Schapiro, W.; Reichek, N. Normal values of right ventricular size and function by real-time 3-dimensional echocardiography: Comparison with cardiac magnetic resonance imaging. J. Am. Soc. Echocardiogr. 2007, 20, 445–455. [Google Scholar] [CrossRef] [PubMed]
- Ripley, D.P.; Musa, T.A.; Dobson, L.E.; Plein, S.; Greenwood, J.P. Cardiovascular magnetic resonance imaging: What the general cardiologist should know. Heart 2016, 102, 1589–1603. [Google Scholar] [CrossRef] [PubMed]
- Galderisi, M.; Cosyns, B.; Edvardsen, T.; Cardim, N.; Delgado, V.; Di Salvo, G.; Donal, E.; Sade, L.E.; Ernande, L.; Garbi, M.; et al. Standardization of adult transthoracic echocardiography reporting in agreement with recent chamber quantification, diastolic function, and heart valve disease recommendations: An expert consensus document of the European Association of Cardiovascular Imaging. Eur. Heart. J. Cardiovasc. Imaging 2017, 18, 1301–1310. [Google Scholar] [PubMed]
- Kramer, C.M.; Barkhausen, J.; Flamm, S.D.; Kim, R.J.; Nagel, E. Society for Cardiovascular Magnetic Resonance Board of Trustees Task Force on Standardized Protocols. Standardized cardiovascular magnetic resonance (CMR) protocols 2013 update. J. Cardiovasc. Magn. Reson. 2013, 15, 91. [Google Scholar] [CrossRef]
- Hudsmith, L.E.; Petersen, S.E.; Francis, J.M.; Robson, M.D.; Neubauer, S. Normal human left and right ventricular and left atrial dimensions using steady state free precession magnetic resonance imaging. J. Cardiovasc. Magn. Reson. 2005, 7, 775–782. [Google Scholar] [CrossRef] [PubMed]
- Prakken, N.H.; Teske, A.J.; Cramer, M.J.; Mosterd, A.; Bosker, A.C.; Mali, W.P.; Doevendans, P.A.; Velthuis, B.K. Head-to-head comparison between echocardiography and cardiac MRI in the evaluation of the athlete’s heart. Br. J. Sports Med. 2012, 46, 348–354. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Maceira, A.M.; Cosín-Sales, J.; Roughton, M.; Prasad, S.K.; Pennell, D.J. Reference left atrial dimensions and volumes by steady state free precession cardiovascular magnetic resonance. J. Cardiovasc. Magn. Reson. 2010, 12, 65. [Google Scholar] [CrossRef] [PubMed]
- von Knobelsdorff-Brenkenhoff, F.; Tkachenko, V.; Winter, L.; Rieger, J.; Thalhammer, C.; Hezel, F.; Graessl, A.; Dieringer, M.A.; Niendorf, T.; Schulz-Menger, J.; et al. Assessment of the right ventricle with cardiovascular magnetic resonance at 7 Tesla. Journal of cardiovascular magnetic resonance: Official. J. Soc. Cardiovasc. Magn. Reson. 2013, 15, 23. [Google Scholar] [CrossRef]
- Motevali, M.; Siahi, Z.; Mohammadzadeh, A.; Sangi, A. Cardiac Magnetic Resonance Imaging (MRI) Findings in Arrhythmogenic Right Ventricular Dysplasia (ARVD) Compared with Echocardiography. Med. Sci. (Basel) 2018, 6, 80. [Google Scholar] [CrossRef]
- Weber, O.M.; Higgins, C.B. MR evaluation of cardiovascular physiology in congenital heart disease: Flow and function. J. Cardiovasc. Magn. Reson. 2006, 8, 607–617. [Google Scholar] [CrossRef]
- Genovese, D.; Mor-Avi, V.; Palermo, C.; Muraru, D.; Volpato, V.; Kruse, E.; Yamat, M.; Aruta, P.; Addetia, K.; Badano, L.P.; et al. Comparison Between Four-Chamber and Right Ventricular-Focused Views for the Quantitative Evaluation of Right Ventricular Size and Function. J. Am. Soc. Echocardiogr. 2019, 24. [Google Scholar] [CrossRef] [PubMed]
- Alfakih, K.; Plein, S.; Bloomer, T.; Jones, T.; Ridgway, J.; Sivananthan, M. Comparison of right ventricular volume measurements between axial and short axis orientation using steady-state free precession magnetic resonance imaging. J. Magn. Reson. Imaging. 2003, 18, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Rudski, L.G.; Lai, W.W.; Afilalo, J.; Hua, L.; Handschumacher, M.D.; Chandrasekaran, K.; Solomon, S.D.; Louie, E.K.; Schiller, N.B. Guidelines for the echocardiographic assessment of the right heart in adults: A report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J. Am. Soc. Echocardiogr. 2010, 23, 685–713. [Google Scholar] [PubMed]


| Chambers | R1 | R2 | C | p Value | ||
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | R1–R2 | R1–C | R2–C | |
| LVED | 51.81 ± 8.72 | 49.24 ± 8.33 | 48.92 ± 6.13 | <0.001 * | 0.075 | 1.000 |
| LVES | 34.43 ± 8.47 | 32.89 ± 8.64 | 33.56 ± 7.23 | 0.046 * | 0.531 | 0.922 |
| LAAP | 36.48 ± 6.93 | 36.60 ± 7.29 | 37.97 ± 6.30 | 1.000 | 0.040 * | 0.089 |
| RV | 41.03 ± 6.27 | 40.57 ± 6.55 | 38.26 ± 6.19 | 0.192 | <0.001 * | <0.001 * |
| RA | 46.58 ± 10.25 | 46.15 ± 10.19 | 42.49 ± 7.08 | 0.181 | <0.001 * | <0.001 * |
| Chambers | R1–R2 | R1–C | R2–C | |||
|---|---|---|---|---|---|---|
| ICC | 95% CI | ICC | 95% CI | ICC | 95% CI | |
| LVED | 0.957 | 0.918–0.978 | 0.849 | 0.709–0.922 | 0.836 | 0.684–0.915 |
| LVES | 0.933 | 0.870–0.965 | 0.929 | 0.863–0.963 | 0.931 | 0.867–0.964 |
| LAAP | 0.994 | 0.989–0.997 | 0.903 | 0.816–0.947 | 0.901 | 0.788–0.943 |
| RV | 0.985 | 0.971–0.992 | 0.869 | 0.755–0.930 | 0.892 | 0.799–0.942 |
| RA | 0.995 | 0.99–0.007 | 0.838 | 0.687–0.916 | 0.841 | 0.694–0.918 |
| Chambers | R1–R2 | R1–C | R2–C | |||
|---|---|---|---|---|---|---|
| r | p * | r | p * | r | p * | |
| LVED | 0.942 | <0.0001 | 0.808 | <0.0001 | 0.752 | <0.0001 |
| LVES | 0.890 | <0.001 | 0.881 | <0.001 | 0.886 | <0.001 |
| LAAP | 0.989 | <0.001 | 0.847 | <0.001 | 0.844 | <0.001 |
| RV | 0.972 | <0.001 | 0.851 | <0.001 | 0.863 | <0.001 |
| RA | 0.991 | <0.0001 | 0.870 | <0.0001 | 0.854 | <0.0001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gürdoğan, M.; Ustabaşıoğlu, F.E.; Kula, O.; Korkmaz, S. Cardiac Magnetic Resonance Imaging and Transthoracic Echocardiography: Investigation of Concordance between the Two Methods for Measurement of the Cardiac Chamber. Medicina 2019, 55, 260. https://doi.org/10.3390/medicina55060260
Gürdoğan M, Ustabaşıoğlu FE, Kula O, Korkmaz S. Cardiac Magnetic Resonance Imaging and Transthoracic Echocardiography: Investigation of Concordance between the Two Methods for Measurement of the Cardiac Chamber. Medicina. 2019; 55(6):260. https://doi.org/10.3390/medicina55060260
Chicago/Turabian StyleGürdoğan, Muhammet, Fethi Emre Ustabaşıoğlu, Osman Kula, and Selçuk Korkmaz. 2019. "Cardiac Magnetic Resonance Imaging and Transthoracic Echocardiography: Investigation of Concordance between the Two Methods for Measurement of the Cardiac Chamber" Medicina 55, no. 6: 260. https://doi.org/10.3390/medicina55060260





