Emergency Medical Service Directors’ Protocols for Exertional Heat Stroke
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Participants
2.3. Procedure
2.4. Survey Instrument
2.5. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A. Survey Questions
- (a)
- Northeast
- (b)
- South
- (c)
- Midwest
- (d)
- West
- (a)
- <5
- (b)
- 5–9
- (c)
- 10–14
- (d)
- 15–19
- (e)
- 20–24
- (f)
- 25+
- (a)
- No
- (b)
- Yes
- (a)
- No
- (b)
- Yes
- (a)
- No
- (b)
- Yes
- (c)
- Unsure
- (a)
- No
- (b)
- Yes
- (a)
- No
- (b)
- Yes
- (a)
- No
- (b)
- Yes
- (a)
- No
- (b)
- Yes
- (a)
- No
- (b)
- Yes
- (a)
- No
- (b)
- Yes
- (a)
- No
- (b)
- Yes
- (a)
- No
- (b)
- Yes
- (a)
- No
- (b)
- Yes
- (a)
- No
- (b)
- Yes
- (a)
- No
- (b)
- Yes
- (a)
- No
- (b)
- Yes
- (a)
- No
- (b)
- Yes
- (a)
- Cool en-route
- (b)
- Cool on-site until temp hits 102
- (c)
- No current EHS protocol
- (a)
- <5
- (b)
- 5–15
- (c)
- 15–25
- (d)
- 25–35
- (e)
- >35
References
- Kerr, Z.Y.; Casa, D.J.; Marshall, S.W.; Comstock, R.D. Epidemiology of exertional heat illness among, U.S. high school athletes. Am. J. Prev. Med. 2013, 44, 8–14. [Google Scholar] [CrossRef]
- Gaudio, F.G.; Grissom, C.K. Cooling Methods in Heat Stroke. J. Emerg. Med. 2016, 50, 607–616. [Google Scholar] [CrossRef]
- Adams, W.M. Exertional Heat Stroke within Secondary School Athletics. Curr. Sports Med. Rep. 2019, 18, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Gubernot, D.M.; Anderson, G.B.; Hunting, K.L. Characterizing occupational heat-related mortality in the United States, 2000–2010: An analysis using the Census of Fatal Occupational Injuries database. Am. J. Ind. Med. 2015, 58, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Roelofs, C. Without Warning: Worker Deaths From Heat 2014–2016. New Solut. 2018, 28, 344–357. [Google Scholar] [CrossRef] [PubMed]
- American College of Sports Medicine; Armstrong, L.E.; Casa, D.J.; Millard-Stafford, M.; Moran, D.S.; Pyne, S.W.; Roberts, W.O. American College of Sports Medicine position stand. Exertional heat illness during training and competition. Med. Sci. Sports Exerc. 2007, 39, 556–572. [Google Scholar] [CrossRef] [PubMed]
- Casa, D.J.; DeMartini, J.K.; Bergeron, M.F.; Csillan, D.; Eichner, E.R.; Lopez, R.M.; Ferrara, M.S.; Miller, K.C.; O’Connor, F.; Sawka, M.N.; et al. National Athletic Trainers’ Association Position Statement: Exertional Heat Illnesses. J. Athl. Train. 2015, 50, 986–1000. [Google Scholar] [CrossRef] [PubMed]
- Casa, D.J.; Armstrong, L.E.; Ganio, M.S.; Yeargin, S.W. Exertional heat stroke in competitive athletes. Curr. Sports Med. Rep. 2005, 4, 309–317. [Google Scholar] [CrossRef]
- Belval, L.N.; Casa, D.J.; Adams, W.M.; Chiampas, G.T.; Holschen, J.C.; Hosokawa, Y.; Jardine, J.; Kane, S.F.; Labotz, M.; Lemieux, R.S.; et al. Consensus Statement-Prehospital Care of Exertional Heat Stroke. Prehosp. Emerg. Care 2018, 22, 392–397. [Google Scholar] [CrossRef]
- Heled, Y.; Rav-Acha, M.; Shani, Y.; Epstein, Y.; Moran, D.S. The “golden hour” for heatstroke treatment. Mil. Med. 2004, 169, 184–186. [Google Scholar] [CrossRef]
- Casa, D.J.; McDermott, B.P.; Lee, E.C.; Yeargin, S.W.; Armstrong, L.E.; Maresh, C.M. Cold water immersion: The gold standard for exertional heatstroke treatment. Exerc. Sport Sci. Rev. 2007, 35, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Demartini, J.K.; Casa, D.J.; Stearns, R.; Belval, L.; Crago, A.; Davis, R.; Jardine, J.J. Effectiveness of cold water immersion in the treatment of exertional heat stroke at the Falmouth Road Race. Med. Sci. Sports Exerc. 2015, 47, 240–245. [Google Scholar] [CrossRef] [PubMed]
- Sloan, B.K.; Kraft, E.M.; Clark, D.; Schmeissing, S.W.; Byrne, B.C.; Rusyniak, D.E. On-site treatment of exertional heat stroke. Am. J. Sports Med. 2015, 43, 823–829. [Google Scholar] [CrossRef] [PubMed]
- Zeller, L.; Novack, V.; Barski, L.; Jotkowitz, A.; Almog, Y. Exertional heatstroke: Clinical characteristics, diagnostic and therapeutic considerations. Eur. J. Intern. Med. 2011, 22, 296–299. [Google Scholar] [CrossRef]
- Casa, D.J.; Becker, S.M.; Ganio, M.S.; Brown, C.M.; Yeargin, S.W.; Roti, M.W.; Siegler, J.; Blowers, J.A.; Glaviano, N.R.; Huggins, R.A.; et al. Validity of devices that assess body temperature during outdoor exercise in the heat. J. Athl. Train. 2007, 42, 333–342. [Google Scholar]
- Ronneberg, K.; Roberts, W.O.; McBean, A.D.; Center, B.A. Temporal artery temperature measurements do not detect hyperthermic marathon runners. Med. Sci. Sports Exerc. 2008, 40, 1373–1375. [Google Scholar] [CrossRef]
- Ganio, M.S.; Brown, C.M.; Casa, D.J.; Becker, S.M.; Yeargin, S.W.; McDermott, B.P.; Boots, L.M.; Boots, L.M.; Armstrong, L.E.; Maresh, C.M. Validity and reliability of devices that assess body temperature during indoor exercise in the heat. J. Athl. Train. 2009, 44, 124–135. [Google Scholar] [CrossRef]
- Moran, D.S.; Mendal, L. Core temperature measurement: Methods and current insights. Sports Med. 2002, 32, 879–885. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Kerr, Z.Y.; Marshall, S.W.; Comstock, R.D.; Casa, D.J. Exertional heat stroke management strategies in United States high school football. Am. J. Sports Med. 2014, 42, 70–77. [Google Scholar]
- Mazerolle, S.M.; Scruggs, I.C.; Casa, D.J.; Burton, L.J.; McDermott, B.P.; Armstrong, L.E.; Maresh, C.M. Current knowledge, attitudes, and practices of certified athletic trainers regarding recognition and treatment of exertional heat stroke. J. Athl. Train. 2010, 45, 170–180. [Google Scholar] [CrossRef] [PubMed]
- Mistovich, J.J.; Karren, K.J.; Werman, H.A.; Hafen, B.Q. Prehospital Emergency Care, 11st ed.; Edn Pearson: New York, NY, USA, 2018. [Google Scholar]
- Grundstein, A.; Williams, C.; Phan, M.; Cooper, E. Regional heat safety thresholds for athletics in the contiguous United States. Appl. Geogr. 2015, 56, 55–60. [Google Scholar] [CrossRef]
- Scarneo, S.E.; DiStefano, L.J.; Stearns, R.L.; Register-Mihalik, J.K.; Denegar, C.R.; Casa, D.J. Emergency Action Planning in Secondary School Athletics: A Comprehensive Evaluation of Current Adoption of Best Practice Standards. J. Athl. Train. 2019, 54, 99–105. [Google Scholar] [CrossRef] [PubMed]
| Location | ||
|---|---|---|
| Northeast | 25 (17.2%) | |
| South | 51 (35.2%) | |
| Midwest | 43 (29.7%) | |
| West | 26 (17.9%) | |
| Number of Years Directing | ||
| <5 | 43 (29.7%) | |
| 5–9 | 32 (22.1%) | |
| 10–14 | 16 (11.0%) | |
| 15–19 | 26 (17.9%) | |
| 20–24 | 11 (7.6%) | |
| 25+ | 17 (11.7%) | |
| Approximate Number of EHS Cases | ||
| <5 | 52 (35.9%) | |
| 5–15 | 51 (35.2%) | |
| 15–25 | 22 (15.2%) | |
| 25–35 | 3 (2.0%) | |
| >35 | 17 (11.7%) | |
| EHS Management Strategy/Protocol | ||
| Cool on-site | 31 (21.4%) | |
| Cool en-route | 91 (62.8%) | |
| None | 23 (15.8%) | |
| Work with an Athletic Trainer | ||
| Yes | 61 (42.9%) | |
| No | 71 (49.0%) | |
| Unsure | 13 (8.1%) |
| Are Your EMS Service Members Aware of the Different Clinical Presentations of Classic vs. Exertional Heat Stroke? | ||
|---|---|---|
| Yes | No | |
| NE | 20 (18.02%) | 5 (14.70%) |
| S | 45 (40.54%) | 6 (17.65%) |
| MW | 34 (30.63%) | 9 (26.47%) |
| W | 12 (10.81%) | 14 (41.18%) |
| TOTAL | 111 (76.55%) | 34 (23.45%) |
| Does your EMS program offer continuing medical education for exertional heat stroke? | ||
| Yes | No | |
| NE | 15 (16.67%) | 10 (18.18%) |
| S | 35 (38.89%) | 16 (29.09%) |
| MW | 26 (28.89%) | 17 (30.91%) |
| W | 14 (15.56%) | 12 (21.82%) |
| TOTAL | 90 (62.07%) | 55 (37.93%) |
| Do you have a specific treatment protocol for exertional heat stroke? | ||
| Yes | No | |
| NE | 10 (11.63%) | 15 (25.42%) |
| S | 37 (43.02%) | 14 (23.73%) |
| MW | 25 (29.07%) | 18 (30.51%) |
| W | 14 (16.28%) | 12 (20.34%) |
| TOTAL | 86 (59.31%) | 59 (40.69%) |
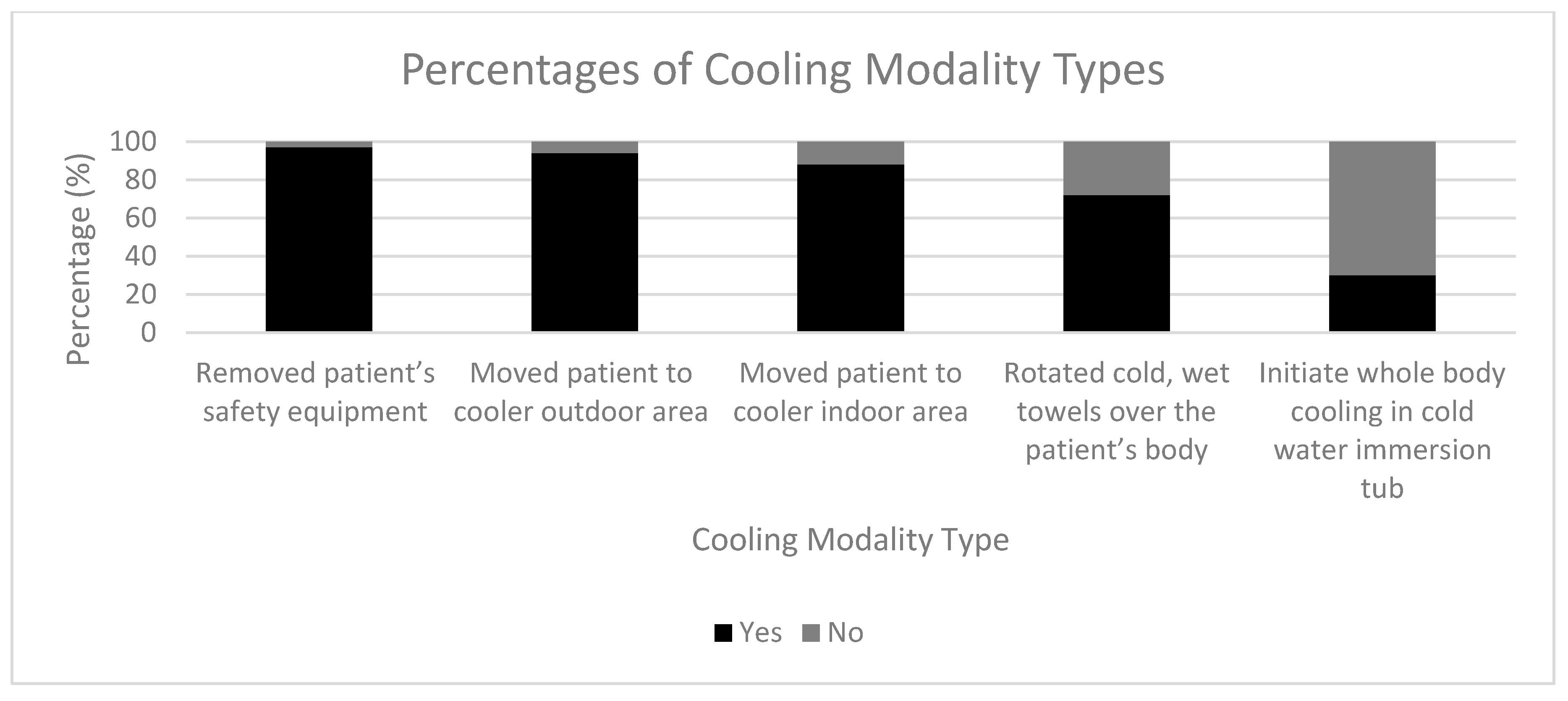
| Do you initiate whole body cooling in cold water immersion tub? | ||
| Yes | No | |
| NE | 8 (18.61%) | 17 (16.67%) |
| S | 15 (34.88%) | 36 (35.29%) |
| MW | 13 (30.23%) | 30 (29.41%) |
| W | 7 (16.28%) | 19 (18.63%) |
| TOTAL | 43 (29.66%) | 102 (70.34%) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szymanski, M.R.; Scarneo-Miller, S.E.; Smith, M.S.; Bruner, M.L.; Casa, D.J. Emergency Medical Service Directors’ Protocols for Exertional Heat Stroke. Medicina 2020, 56, 494. https://doi.org/10.3390/medicina56100494
Szymanski MR, Scarneo-Miller SE, Smith MS, Bruner ML, Casa DJ. Emergency Medical Service Directors’ Protocols for Exertional Heat Stroke. Medicina. 2020; 56(10):494. https://doi.org/10.3390/medicina56100494
Chicago/Turabian StyleSzymanski, Michael R., Samantha E. Scarneo-Miller, M. Seth Smith, Michelle L. Bruner, and Douglas J. Casa. 2020. "Emergency Medical Service Directors’ Protocols for Exertional Heat Stroke" Medicina 56, no. 10: 494. https://doi.org/10.3390/medicina56100494
APA StyleSzymanski, M. R., Scarneo-Miller, S. E., Smith, M. S., Bruner, M. L., & Casa, D. J. (2020). Emergency Medical Service Directors’ Protocols for Exertional Heat Stroke. Medicina, 56(10), 494. https://doi.org/10.3390/medicina56100494






