Severe Case of Delayed Replantation of Avulsed Permanent Central Incisor: A Case Report with Four-Year Follow-Up
Abstract
:1. Introduction
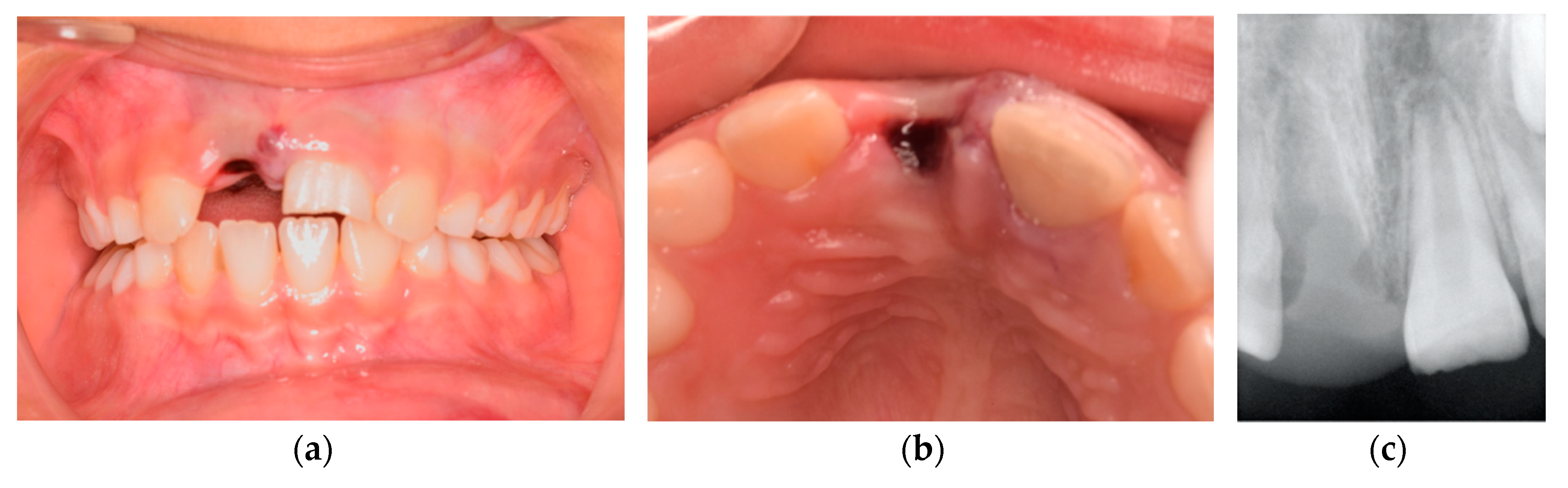
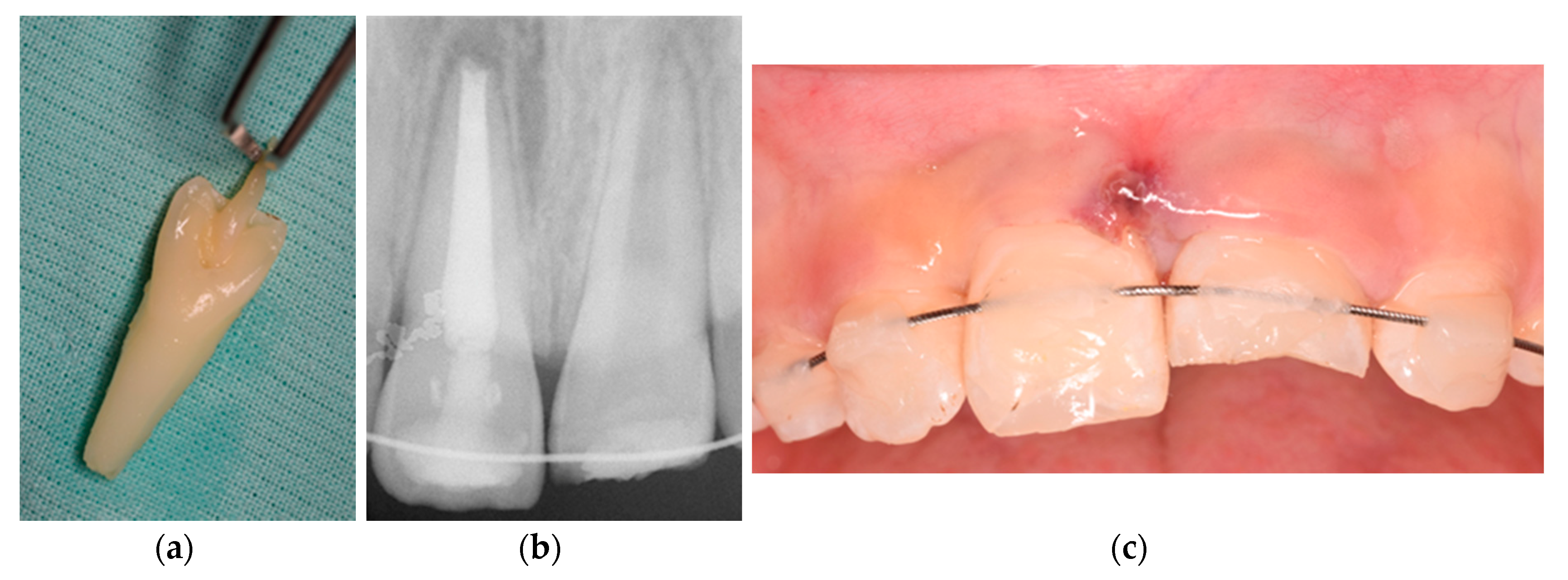
2. Case Presentation
3. Discussion
4. Conclusions and Clinical Implications
Author Contributions
Funding
Conflicts of Interest
References
- Trope, M. Root Resorption due to Dental Trauma. Endod. Top. 2002, 1, 79–100. [Google Scholar] [CrossRef] [Green Version]
- Fouad, A.F.; Abbott, P.V.; Tsilingaridis, G.; Cohenca, N.; Lauridsen, E.; Bourguignon, C.; O’Connell, A.; Flores, M.T.; Day, P.F.; Hicks, L.; et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dent. Traumatol. 2020, 36, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Adnan, S.; Lone, M.M.; Khan, F.R.; Hussain, S.M.; Nagi, S.E. Which is the most recommended medium for the storage and transport of avulsed teeth? A systematic review. Dent. Traumatol. 2018, 34, 59–70. [Google Scholar] [CrossRef] [Green Version]
- Day, P.F.; Duggal, M.; Nazzal, H. Interventions for treating traumatised permanent front teeth: Avulsed (knocked out) and replanted. Cochrane Database Syst. Rev. 2019, 2, 006542. [Google Scholar] [CrossRef]
- Mohamed, R.N.; Basha, S.; Al-Thomali, Y.; Tawfik Enan, E. Enamel matrix derivative (Emdogain) in treatment of replanted teeth—A systematic review. Acta Odontol. Scand. 2019, 77, 168–172. [Google Scholar] [CrossRef]
- Abd-Elmeguid, A.; Elsalhy, M.; Yu, D.C. Pulp canal obliteration after replantation of avulsed immature teeth: A systematic review. Dent. Traumatol. 2015, 31, 437–441. [Google Scholar] [CrossRef]
- Lauridsen, E.; Andreasen, J.O.; Bouaziz, O.; Andersson, L. Risk of ankylosis of 400 avulsed and replanted human teeth in relation to length of dry storage: A re-evaluation of a long-term clinical study. Dent. Traumatol. 2020, 36, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zhang, X.; Gong, Y. Treatment of avulsed immature permanent teeth in Beijing China: A retrospective comparison between 2008 and 2015. Dent. Traumatol. 2020, 36, 498–504. [Google Scholar] [CrossRef] [PubMed]
- Demir, P.; Guler, C.; Kizilci, E.; Keskin, G. Survival of Avulsed Permanent Incisors in Children Following Delayed Replantation. Niger. J. Clin. Pract. 2020, 23, 631–637. [Google Scholar]
- De Brier, N.; Dorien, O.; Borra, V.; Singletary, E.M.; Zideman, D.A.; De Buck, E.; Bendall, J.C.; Berry, D.C.; Carlson, J.N.; Cassan, P.; et al. Storage of an avulsed tooth prior to replantation: A systematic review and meta-analysis. Dent. Traumatol. 2020, 36, 453–476. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Iorio-Siciliano, V.; Alibrandi, A.; Ramaglia, L.; Leonardi, R. Effectiveness of a nutraceutical agent in the non-surgical periodontal therapy: A randomized, controlled clinical trial. Clin. Oral Investig. 2020. [Google Scholar] [CrossRef]
- Andersson, L.; Andreasen, J.O.; Day, P.; Heithersay, G.; Trope, M.; DiAngelis, A.J.; Kenny, D.J.; Sigurdsson, A.; Bourguignon, C.; Flores, M.T.; et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dent. Traumatol. 2012, 28, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Peng, X.; Sun, H.; Li, X. Clinical and histopathological characterization of root resorption in replanted teeth: Two case reports. Medicine 2020, 99, e18869. [Google Scholar] [CrossRef] [PubMed]
- Müller, D.D.; Bissinger, R.; Reymus, M.; Bücher, K.; Hickel, R.; Kühnisch, J. Survival and complication analyses of avulsed and replanted permanent teeth. Sci. Rep. 2020, 10, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Najeeb, S.; Al-Quraini, A.A.A.; Almusallam, H.A.A.; Zafar, M.S.; Khurshid, Z. Effect of laser treatment on outcomes of tooth replantation—A systematic review. J. Taibah Univ. Med. Sci. 2020, 15, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Wang, C.; Qin, M. A retrospective study of survival of 196 replanted permanent teeth in children. Dent. Traumatol. 2019, 35, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Coelho-De-Souza, F.H.; Gonçalves, D.S.; Sales, M.P.; Erhardt, M.C.G.; Corrêa, M.B.; Opdam, N.J.M.; Demarco, F.F. Direct anterior composite veneers in vital and non-vital teeth: A retrospective clinical evaluation. J. Dent. 2015, 43, 1330–1336. [Google Scholar] [CrossRef]
- Timmerman, A.; Parashos, P. Bleaching of a Discolored Tooth with Retrieval of Remnants after Successful Regenerative Endodontics. J. Endod. 2018, 44, 93–97. [Google Scholar] [CrossRef] [Green Version]
- Lam, R. Epidemiology and outcomes of traumatic dental injuries: A review of the literature. Aust. Dent. J. 2016, 61, 4–20. [Google Scholar] [CrossRef] [Green Version]
- Osmanovic, A.; Halilovic, S.; Kurtovic-Kozaric, A.; Hadziabdic, N. Evaluation of periodontal ligament cell viability in different storage media based on human PDL cell culture experiments—A systematic review. Dent. Traumatol. 2018, 34, 384–393. [Google Scholar] [CrossRef]
- Shetty, A.; Ghosh, S.; Srirekha, A.; Jaykumar, T.; Chikkamallaiah, C.; Adiga, S. Comparative evaluation of efficacy of platelet-Rich Fibrin and hank’s balanced salt solution as a storage medium for avulsed teeth: An in vitro study. Eur. Endod. J. 2019, 4, 118–121. [Google Scholar] [PubMed]
- Isola, G.; Alibrandi, A.; Currò, M.; Matarese, M.; Ricca, S.; Matarese, G.; Ientile, R.; Kocher, T. Evaluation of salivary and serum asymmetric dimethylarginine (ADMA) levels in patients with periodontal and cardiovascular disease as subclinical marker of cardiovascular risk. J. Periodontol. 2020, 91, 1076–1084. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Santonocito, S.; Alibrandi, A.; Ferlito, S. Expression of salivary and serum malondialdehyde and lipid profile of patients with periodontitis and coronary heart disease. Int. J. Mol. Sci. 2019, 20, 6061. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lou, Q.; Zhu, Y.; Wang, X. Fourteen Years After Delayed Replantation of an Avulsed Permanent Tooth: Clinical Features and Outcomes. J. Craniofac. Surg. 2019, 30, e692–e694. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Ashlenazi, M.; Karawan, M.; Teich, S.T.; Gutmacher, Z. Management of Ankylotic Root Resorption Following Dental Trauma: A Short Review and Proposal of a Treatment Protocol. Oral Health Prev. Dent. 2017, 15, 467–474. [Google Scholar]
- Antov, H.; Duggal, M.; Nazzal, H. Management of discolouration following revitalization endodontic procedures: A case series. Int. Endod. J. 2019, 52, 1660–1670. [Google Scholar] [CrossRef]
- Ree, M.; Schwartz, R. Long-term Success of Nonvital, Immature Permanent Incisors Treated With a Mineral Trioxide Aggregate Plug and Adhesive Restorations: A Case Series from a Private Endodontic Practice. J. Endod. 2017, 43, 1370–1377. [Google Scholar] [CrossRef]
- Albuquerque, P.; Moreno, M.; Nishida, A.; Rodrigues, E.; Kiyohara, C.; Francci, C. Prefabricated resin veneer: A case report of a simplified restorative technique. J. Dent. Res. Dent. Clin. Dent. Prospect. 2019, 12, 140–145. [Google Scholar] [CrossRef] [Green Version]
- Limly Bal, T.; Chakravarthy, D.; SN, P.; Vijayaraja, S.; Jayadevan, A.; Dimple, N. Indirect Resin Composite Restorations—A Narrative Review. Jacobs J. Dent. Res. 2019, 5, 41. [Google Scholar]

© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lopes, L.B.; Botelho, J.; Machado, V. Severe Case of Delayed Replantation of Avulsed Permanent Central Incisor: A Case Report with Four-Year Follow-Up. Medicina 2020, 56, 503. https://doi.org/10.3390/medicina56100503
Lopes LB, Botelho J, Machado V. Severe Case of Delayed Replantation of Avulsed Permanent Central Incisor: A Case Report with Four-Year Follow-Up. Medicina. 2020; 56(10):503. https://doi.org/10.3390/medicina56100503
Chicago/Turabian StyleLopes, Luísa Bandeira, João Botelho, and Vanessa Machado. 2020. "Severe Case of Delayed Replantation of Avulsed Permanent Central Incisor: A Case Report with Four-Year Follow-Up" Medicina 56, no. 10: 503. https://doi.org/10.3390/medicina56100503






