Current Endoscopic Management of Malignant Biliary Stricture
Abstract
1. Introduction
2. Resectable Malignancy
3. Unresectable Malignancy
3.1. Malignant Distal Biliary Obstruction
3.2. Stent Selection
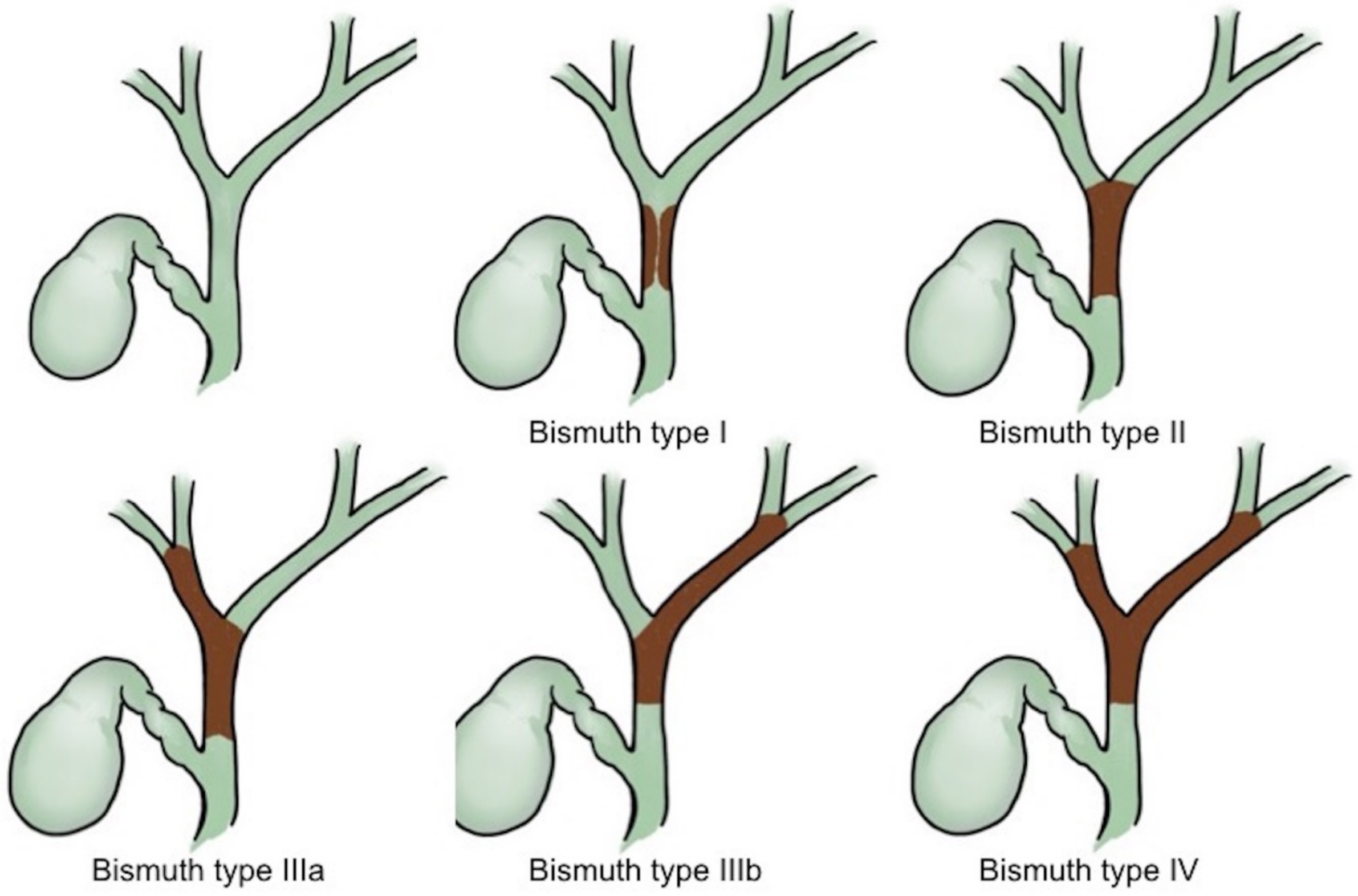
4. Malignant Hilar Biliary Obstruction
4.1. Bilateral or Unilateral Drainage
4.2. Stent Selection
4.3. Rescue Management
5. Summary
Author Contributions
Funding
Conflicts of Interest
Abbreviations
References
- Pinchuk, L.; Magnanini, F.; Nardi, G.; Bosolino, A.; Rubio, H. Percutaneous transhepatic biliary drainage in obstructive jaundice. Acta Gastroenterol. Latinoam 1981, 11, 279–284. [Google Scholar]
- Manegold, B.C. Obstructive jaundice of benign and malignant origin: Endoscopy in diagnosis and therapy. Langenbecks Arch. Chir. 1981, 355, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Safrany, L.; Schott, B.; Krause, S.; Balint, T.; Portocarrero, G. Endoscopic transpapillary bile duct drainage in malignant obstructive jaundice. Dtsch. Med. Wochenschr. 1982, 107, 1867–1871. [Google Scholar] [CrossRef] [PubMed]
- Roque, J.; Ho, S.H.; Goh, K.L. Preoperative drainage for malignant biliary strictures: Is it time for self-expanding metallic stents? Clin. Endosc. 2015, 48, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Tyson, G.L.; Ilyas, J.A.; Duan, Z.; Green, L.K.; Younes, M.; El-Serag, H.B.; Davila, J.A. Secular trends in the incidence of cholangiocarcinoma in the USA and the impact of misclassification. Dig. Dis. Sci. 2014, 59, 3103–3110. [Google Scholar] [CrossRef]
- Bertuccio, P.; Bosetti, C.; Levi, F.; Decarli, A.; Negri, E.; La Vecchia, C. A comparison of trends in mortality from primary liver cancer and intrahepatic cholangiocarcinoma in Europe. Ann. Oncol. 2013, 24, 1667–1674. [Google Scholar] [CrossRef]
- Yadav, D.; Lowenfels, A.B. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology 2013, 144, 1252–1261. [Google Scholar] [CrossRef]
- Simile, M.M.; Bagella, P.; Vidili, G.; Spanu, A.; Manetti, R.; Seddaiu, M.A.; Babudieri, S.; Madeddu, G.; Serra, P.A.; Altana, M.; et al. Targeted Therapies in Cholangiocarcinoma: Emerging Evidence from Clinical Trials. Medicina 2019, 55, 42. [Google Scholar] [CrossRef]
- American Society for Gastrointestinal Endoscopy Standards of Practice Committee; Anderson, M.A.; Appalaneni, V.; Ben-Menachem, T.; Decker, G.A.; Early, D.S.; Evans, J.A.; Fanelli, R.D.; Fisher, D.A.; Fisher, L.R.; et al. The role of endoscopy in the evaluation and treatment of patients with biliary neoplasia. Gastrointest. Endosc. 2013, 77, 167–174. [Google Scholar] [CrossRef]
- De Angelis, C.; Marietti, M.; Bruno, M.; Pellicano, R.; Rizzetto, M. Endoscopic ultrasound in common bile duct dilatation with normal liver enzymes. World J. Gastrointest. Endosc. 2015, 7, 799–805. [Google Scholar] [CrossRef]
- Van der Gaag, N.A.; Rauws, E.A.; van Eijck, C.H.; Bruno, M.J.; van der Harst, E.; Kubben, F.J.; Gerritsen, J.J.; Greve, J.W.; Gerhards, M.F.; de Hingh, I.H.; et al. Preoperative biliary drainage for cancer of the head of the pancreas. N. Engl. J. Med. 2010, 362, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Velanovich, V.; Kheibek, T.; Khan, M. Relationship of postoperative complications from preoperative biliary stents after pancreaticoduodenectomy. A new cohort analysis and meta-analysis of modern studies. JOP 2009, 10, 24–29. [Google Scholar] [PubMed]
- Qiu, Y.D.; Bai, J.L.; Xu, F.G.; Ding, Y.T. Effect of preoperative biliary drainage on malignant obstructive jaundice: A meta-analysis. World J. Gastroenterol. 2011, 17, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Sewnath, M.E.; Karsten, T.M.; Prins, M.H.; Rauws, E.J.; Obertop, H.; Gouma, D.J. A meta-analysis on the efficacy of preoperative biliary drainage for tumors causing obstructive jaundice. Ann. Surg. 2002, 236, 17–27. [Google Scholar] [CrossRef]
- Bismuth, H.; Nakache, R.; Diamond, T. Management strategies in resection for hilar cholangiocarcinoma. Ann. Surg. 1992, 215, 31–38. [Google Scholar] [CrossRef]
- De Bellis, M.; Sherman, S.; Fogel, E.L.; Cramer, H.; Chappo, J.; McHenry, L., Jr.; Watkins, J.L.; Lehman, G.A. Tissue sampling at ERCP in suspected malignant biliary strictures (Part 1). Gastrointest. Endosc. 2002, 56, 552–561. [Google Scholar] [CrossRef]
- Fogel, E.L.; deBellis, M.; McHenry, L.; Watkins, J.L.; Chappo, J.; Cramer, H.; Schmidt, S.; Lazzell-Pannell, L.; Sherman, S.; Lehman, G.A. Effectiveness of a new long cytology brush in the evaluation of malignant biliary obstruction: A prospective study. Gastrointest. Endosc. 2006, 63, 71–77. [Google Scholar] [CrossRef]
- Fukuda, Y.; Tsuyuguchi, T.; Sakai, Y.; Tsuchiya, S.; Saisyo, H. Diagnostic utility of peroral cholangioscopy for various bile-duct lesions. Gastrointest. Endosc. 2005, 62, 374–382. [Google Scholar] [CrossRef]
- Shah, R.J.; Langer, D.A.; Antillon, M.R.; Chen, Y.K. Cholangioscopy and cholangioscopic forceps biopsy in patients with indeterminate pancreaticobiliary pathology. Clin. Gastroenterol. Hepatol. 2006, 4, 219–225. [Google Scholar] [CrossRef]
- Osanai, M.; Itoi, T.; Igarashi, Y.; Tanaka, K.; Kida, M.; Maguchi, H.; Yasuda, K.; Okano, N.; Imaizumi, H.; Itokawa, F. Peroral video cholangioscopy to evaluate indeterminate bile duct lesions and preoperative mucosal cancerous extension: A prospective multicenter study. Endoscopy 2013, 45, 635–642. [Google Scholar] [CrossRef]
- Navaneethan, U.; Hasan, M.K.; Lourdusamy, V.; Njei, B.; Varadarajulu, S.; Hawes, R.H. Single-operator cholangioscopy and targeted biopsies in the diagnosis of indeterminate biliary strictures: A systematic review. Gastrointest. Endosc. 2015, 82, 608–614e602. [Google Scholar] [CrossRef] [PubMed]
- Zaydfudim, V.M.; Clark, C.J.; Kendrick, M.L.; Que, F.G.; Reid-Lombardo, K.M.; Donohue, J.H.; Farnell, M.B.; Nagorney, D.M. Correlation of staging systems to survival in patients with resected hilar cholangiocarcinoma. Am. J. Surg. 2013, 206, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.W.; Hu, B.S.; Chu, Y.J.; Tan, Y.C.; Ji, X.; Chen, K.; Ding, X.M.; Zhang, A.; Chen, F.; Dong, J.H. One-stage resection for Bismuth type IV hilar cholangiocarcinoma with high hilar resection and parenchyma-preserving strategies: A cohort study. World J. Surg. 2013, 37, 614–621. [Google Scholar] [CrossRef] [PubMed]
- Committee ASoP; Eloubeidi, M.A.; Decker, G.A.; Chandrasekhara, V.; Chathadi, K.V.; Early, D.S.; Evans, J.A.; Fanelli, R.D.; Fisher, D.A.; Jue, T.L.; et al. The role of endoscopy in the evaluation and management of patients with solid pancreatic neoplasia. Gastrointest. Endosc. 2016, 83, 17–28. [Google Scholar] [CrossRef]
- Yang, D.; Perbtani, Y.B.; An, Q.; Agarwal, M.; Riverso, M.; Chakraborty, J.; Brar, T.S.; Westerveld, D.; Zhang, H.; Chauhan, S.S.; et al. Survey study on the practice patterns in the endoscopic management of malignant distal biliary obstruction. Endosc. Int. Open 2017, 5, E754–E762. [Google Scholar] [CrossRef]
- Quirk, D.M.; Rattner, D.W.; Fernandez-del Castillo, C.; Warshaw, A.L.; Brugge, W.R. The use of endoscopic ultrasonography to reduce the cost of treating ampullary tumors. Gastrointest. Endosc. 1997, 46, 334–337. [Google Scholar] [CrossRef]
- Hernandez, L.V.; Catalano, M.F. Endoscopic papillectomy. Curr. Opin. Gastroenterol. 2008, 24, 617–622. [Google Scholar] [CrossRef]
- Isayama, H.; Nakai, Y.; Kawakubo, K.; Kogure, H.; Hamada, T.; Togawa, O.; Sasahira, N.; Hirano, K.; Tsujino, T.; Koike, K. Endoscopic retrograde cholangiopancreatography for distal malignant biliary stricture. Gastrointest. Endosc. Clin. N. Am. 2012, 22, 479–490. [Google Scholar] [CrossRef]
- Lee, J.H. Self-expandable metal stents for malignant distal biliary strictures. Gastrointest. Endosc. Clin. N. Am. 2011, 21, 463–480. [Google Scholar] [CrossRef]
- Kahaleh, M.; Tokar, J.; Conaway, M.R.; Brock, A.; Le, T.; Adams, R.B.; Yeaton, P. Efficacy and complications of covered Wallstents in malignant distal biliary obstruction. Gastrointest. Endosc. 2005, 61, 528–533. [Google Scholar] [CrossRef]
- Taylor, M.C.; McLeod, R.S.; Langer, B. Biliary stenting versus bypass surgery for the palliation of malignant distal bile duct obstruction: A meta-analysis. Liver Transpl. 2000, 6, 302–308. [Google Scholar] [CrossRef] [PubMed]
- Moss, A.C.; Morris, E.; Leyden, J.; MacMathuna, P. Malignant distal biliary obstruction: A systematic review and meta-analysis of endoscopic and surgical bypass results. Cancer Treat. Rev. 2007, 33, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.N.; Jeong, S.; Choi, H.J.; Cho, J.H.; Cheon, Y.K.; Park, S.W.; Kim, Y.S.; Lee, D.H.; Moon, J.H. The safety of newly developed automatic temperature-controlled endobiliary radiofrequency ablation system for malignant biliary strictures: A prospective multicenter study. J. Gastroenterol. Hepatol. 2019, 34, 1454–1459. [Google Scholar] [CrossRef] [PubMed]
- Mizandari, M.; Kumar, J.; Pai, M.; Chikovani, T.; Azrumelashvili, T.; Reccia, I.; Habib, N. Interventional radiofrequency ablation: A promising therapeutic modality in the management of malignant biliary and pancreatic duct obstruction. J. Cancer 2018, 9, 629–637. [Google Scholar] [CrossRef]
- Dutta, A.K.; Basavaraju, U.; Sales, L.; Leeds, J.S. Radiofrequency ablation for management of malignant biliary obstruction: A single-center experience and review of the literature. Expert Rev. Gastroenterol. Hepatol. 2017, 11, 779–784. [Google Scholar] [CrossRef]
- Bill, J.G.; Darcy, M.; Fujii-Lau, L.L.; Mullady, D.K.; Gaddam, S.; Murad, F.M.; Early, D.S.; Edmundowicz, S.A.; Kushnir, V.M. A comparison between endoscopic ultrasound-guided rendezvous and percutaneous biliary drainage after failed ERCP for malignant distal biliary obstruction. Endosc. Int. Open 2016, 4, E980–E985. [Google Scholar] [CrossRef]
- Park, J.K.; Woo, Y.S.; Noh, D.H.; Yang, J.I.; Bae, S.Y.; Yun, H.S.; Lee, J.K.; Lee, K.T.; Lee, K.H. Efficacy of EUS-guided and ERCP-guided biliary drainage for malignant biliary obstruction: Prospective randomized controlled study. Gastrointest. Endosc. 2018, 88, 277–282. [Google Scholar] [CrossRef]
- Paik, W.H.; Lee, T.H.; Park, D.H.; Choi, J.H.; Kim, S.O.; Jang, S.; Kim, D.U.; Shim, J.H.; Song, T.J.; Lee, S.S.; et al. EUS-Guided Biliary Drainage Versus ERCP for the Primary Palliation of Malignant Biliary Obstruction: A Multicenter Randomized Clinical Trial. Am. J. Gastroenterol. 2018, 113, 987–997. [Google Scholar] [CrossRef]
- Lou, X.; Yu, D.; Li, J.; Feng, S.; Sun, J.J. Efficacy of endoscopic ultrasound-guided and endoscopic retrograde cholangiopancreatography-guided biliary drainage for malignant biliary obstruction: A systematic review and meta-analysis. Minerva Med. 2019, 110, 564–574. [Google Scholar] [CrossRef]
- Jaganmohan, S.; Lee, J.H. Self-expandable metal stents in malignant biliary obstruction. Expert Rev. Gastroenterol. Hepatol. 2012, 6, 105–114. [Google Scholar] [CrossRef]
- Knyrim, K.; Wagner, H.J.; Pausch, J.; Vakil, N. A prospective, randomized, controlled trial of metal stents for malignant obstruction of the common bile duct. Endoscopy 1993, 25, 207–212. [Google Scholar] [CrossRef] [PubMed]
- Prat, F.; Chapat, O.; Ducot, B.; Ponchon, T.; Pelletier, G.; Fritsch, J.; Choury, A.D.; Buffet, C. A randomized trial of endoscopic drainage methods for inoperable malignant strictures of the common bile duct. Gastrointest. Endosc. 1998, 47, 1–7. [Google Scholar] [CrossRef]
- Katsinelos, P.; Paikos, D.; Kountouras, J.; Chatzimavroudis, G.; Paroutoglou, G.; Moschos, I.; Gatopoulou, A.; Beltsis, A.; Zavos, C.; Papaziogas, B. Tannenbaum and metal stents in the palliative treatment of malignant distal bile duct obstruction: A comparative study of patency and cost effectiveness. Surg. Endosc. 2006, 20, 1587–1593. [Google Scholar] [CrossRef] [PubMed]
- Soderlund, C.; Linder, S. Covered metal versus plastic stents for malignant common bile duct stenosis: A prospective, randomized, controlled trial. Gastrointest. Endosc. 2006, 63, 986–995. [Google Scholar] [CrossRef] [PubMed]
- Levy, M.J.; Baron, T.H.; Gostout, C.J.; Petersen, B.T.; Farnell, M.B. Palliation of malignant extrahepatic biliary obstruction with plastic versus expandable metal stents: An evidence-based approach. Clin. Gastroenterol. Hepatol. 2004, 2, 273–285. [Google Scholar] [CrossRef]
- Aadam, A.A.; Evans, D.B.; Khan, A.; Oh, Y.; Dua, K. Efficacy and safety of self-expandable metal stents for biliary decompression in patients receiving neoadjuvant therapy for pancreatic cancer: A prospective study. Gastrointest. Endosc. 2012, 76, 67–75. [Google Scholar] [CrossRef]
- Isayama, H.; Komatsu, Y.; Tsujino, T.; Sasahira, N.; Hirano, K.; Toda, N.; Nakai, Y.; Yamamoto, N.; Tada, M.; Yoshida, H.; et al. A prospective randomised study of “covered” versus “uncovered” diamond stents for the management of distal malignant biliary obstruction. Gut 2004, 53, 729–734. [Google Scholar] [CrossRef]
- Park, D.H.; Kim, M.H.; Choi, J.S.; Lee, S.S.; Seo, D.W.; Kim, J.H.; Han, J.; Kim, J.C.; Choi, E.K.; Lee, S.K. Covered versus uncovered wallstent for malignant extrahepatic biliary obstruction: A cohort comparative analysis. Clin. Gastroenterol. Hepatol. 2006, 4, 790–796. [Google Scholar] [CrossRef]
- Yoon, W.J.; Lee, J.K.; Lee, K.H.; Lee, W.J.; Ryu, J.K.; Kim, Y.T.; Yoon, Y.B. A comparison of covered and uncovered Wallstents for the management of distal malignant biliary obstruction. Gastrointest. Endosc. 2006, 63, 996–1000. [Google Scholar] [CrossRef]
- Fumex, F.; Coumaros, D.; Napoleon, B.; Barthet, M.; Laugier, R.; Yzet, T.; Le Sidaner, A.; Desurmont, P.; Lamouliatte, H.; Letard, J.C.; et al. Similar performance but higher cholecystitis rate with covered biliary stents: Results from a prospective multicenter evaluation. Endoscopy 2006, 38, 787–792. [Google Scholar] [CrossRef]
- Petersen, B.T.; Kahaleh, M.; Kozarek, R.A.; Loren, D.; Gupta, K.; Kowalski, T.; Freeman, M.; Chen, Y.K.; Branch, M.S.; Edmundowicz, S.; et al. A multicenter, prospective study of a new fully covered expandable metal biliary stent for the palliative treatment of malignant bile duct obstruction. Gastroenterol. Res. Pract. 2013, 2013, 642428. [Google Scholar] [CrossRef] [PubMed]
- Kitano, M.; Yamashita, Y.; Tanaka, K.; Konishi, H.; Yazumi, S.; Nakai, Y.; Nishiyama, O.; Uehara, H.; Mitoro, A.; Sanuki, T.; et al. Covered self-expandable metal stents with an anti-migration system improve patency duration without increased complications compared with uncovered stents for distal biliary obstruction caused by pancreatic carcinoma: A randomized multicenter trial. Am. J. Gastroenterol. 2013, 108, 1713–1722. [Google Scholar] [CrossRef] [PubMed]
- Yokota, Y.; Fukasawa, M.; Takano, S.; Kadokura, M.; Shindo, H.; Takahashi, E.; Hirose, S.; Kawakami, S.; Fukasawa, Y.; Sato, T.; et al. Partially covered metal stents have longer patency than uncovered and fully covered metal stents in the management of distal malignant biliary obstruction: A retrospective study. BMC Gastroenterol. 2017, 17, 105. [Google Scholar] [CrossRef] [PubMed]
- Kahaleh, M.; Talreja, J.P.; Loren, D.E.; Kowalski, T.E.; Poneros, J.M.; Degaetani, M.; Raijman, I.; Sejpal, D.V.; Patel, S.; Rosenkranz, L.; et al. Evaluation of a fully covered self-expanding metal stent with flared ends in malignant biliary obstruction: A multicenter study. J. Clin. Gastroenterol. 2013, 47, e96–e100. [Google Scholar] [CrossRef]
- Lee, B.S.; Ryu, J.K.; Jang, D.K.; Chung, K.H.; Yoon, W.J.; Kim, J.; Woo, S.M.; Lee, S.H.; Lee, W.J.; Kim, Y.T. Reintervention for occluded metal stent in malignant bile duct obstruction: A prospective randomized trial comparing covered and uncovered metal stent. J. Gastroenterol. Hepatol. 2016, 31, 1901–1907. [Google Scholar] [CrossRef]
- Lee, J.H.; Krishna, S.G.; Singh, A.; Ladha, H.S.; Slack, R.S.; Ramireddy, S.; Raju, G.S.; Davila, M.; Ross, W.A. Comparison of the utility of covered metal stents versus uncovered metal stents in the management of malignant biliary strictures in 749 patients. Gastrointest. Endosc. 2013, 78, 312–324. [Google Scholar] [CrossRef]
- Li, J.; Li, T.; Sun, P.; Yu, Q.; Wang, K.; Chang, W.; Song, Z.; Zheng, Q. Covered versus Uncovered Self-Expandable Metal Stents for Managing Malignant Distal Biliary Obstruction: A Meta-Analysis. PLoS ONE 2016, 11, e0149066. [Google Scholar] [CrossRef]
- Almadi, M.A.; Barkun, A.N.; Martel, M. No benefit of covered vs. uncovered self-expandable metal stents in patients with malignant distal biliary obstruction: A meta-analysis. Clin. Gastroenterol. Hepatol. 2013, 11, 27–37.e21. [Google Scholar] [CrossRef]
- Conio, M.; Mangiavillano, B.; Caruso, A.; Filiberti, R.A.; Baron, T.H.; De Luca, L.; Signorelli, S.; Crespi, M.; Marini, M.; Ravelli, P.; et al. Covered versus uncovered self-expandable metal stent for palliation of primary malignant extrahepatic biliary strictures: A randomized multicenter study. Gastrointest. Endosc. 2018, 88, 283–291.e283. [Google Scholar] [CrossRef]
- Kim, J.Y.; Ko, G.B.; Lee, T.H.; Park, S.H.; Lee, Y.N.; Cho, Y.S.; Jung, Y.; Chung, I.K.; Choi, H.J.; Cha, S.W.; et al. Partially Covered Metal Stents May Not Prolong Stent Patency Compared to Uncovered Stents in Unresectable Malignant Distal Biliary Obstruction. Gut Liver 2017, 11, 440–446. [Google Scholar] [CrossRef]
- Yang, M.J.; Kim, J.H.; Yoo, B.M.; Hwang, J.C.; Yoo, J.H.; Lee, K.S.; Kang, J.K.; Kim, S.S.; Lim, S.G.; Shin, S.J.; et al. Partially covered versus uncovered self-expandable nitinol stents with anti-migration properties for the palliation of malignant distal biliary obstruction: A randomized controlled trial. Scand. J. Gastroenterol. 2015, 50, 1490–1499. [Google Scholar] [CrossRef] [PubMed]
- Levy, M.J.; Heimbach, J.K.; Gores, G.J. Endoscopic ultrasound staging of cholangiocarcinoma. Curr. Opin. Gastroenterol. 2012, 28, 244–252. [Google Scholar] [CrossRef] [PubMed]
- Heimbach, J.K.; Sanchez, W.; Rosen, C.B.; Gores, G.J. Trans-peritoneal fine needle aspiration biopsy of hilar cholangiocarcinoma is associated with disease dissemination. HPB 2011, 13, 356–360. [Google Scholar] [CrossRef] [PubMed]
- Rerknimitr, R.; Angsuwatcharakon, P.; Ratanachu-ek, T.; Khor, C.J.; Ponnudurai, R.; Moon, J.H.; Seo, D.W.; Pantongrag-Brown, L.; Sangchan, A.; Pisespongsa, P.; et al. Asia-Pacific consensus recommendations for endoscopic and interventional management of hilar cholangiocarcinoma. J. Gastroenterol. Hepatol. 2013, 28, 593–607. [Google Scholar] [CrossRef] [PubMed]
- Saluja, S.S.; Gulati, M.; Garg, P.K.; Pal, H.; Pal, S.; Sahni, P.; Chattopadhyay, T.K. Endoscopic or percutaneous biliary drainage for gallbladder cancer: A randomized trial and quality of life assessment. Clin. Gastroenterol. Hepatol. 2008, 6, 944–950.e943. [Google Scholar] [CrossRef] [PubMed]
- Bueno, J.T.; Gerdes, H.; Kurtz, R.C. Endoscopic management of occluded biliary Wallstents: A cancer center experience. Gastrointest. Endosc. 2003, 58, 879–884. [Google Scholar] [CrossRef]
- Katanuma, A.; Irisawa, A.; Itoi, T. Otaru consensus on biliary stenting for unresectable malignant hilar biliary obstruction. Dig. Endosc. 2013, 25 (Suppl. 2), 58–62. [Google Scholar] [CrossRef]
- Vienne, A.; Hobeika, E.; Gouya, H.; Lapidus, N.; Fritsch, J.; Choury, A.D.; Chryssostalis, A.; Gaudric, M.; Pelletier, G.; Buffet, C.; et al. Prediction of drainage effectiveness during endoscopic stenting of malignant hilar strictures: The role of liver volume assessment. Gastrointest. Endosc. 2010, 72, 728–735. [Google Scholar] [CrossRef]
- Perdue, D.G.; Freeman, M.L.; DiSario, J.A.; Nelson, D.B.; Fennerty, M.B.; Lee, J.G.; Overby, C.S.; Ryan, M.E.; Bochna, G.S.; Snady, H.W.; et al. Plastic versus self-expanding metallic stents for malignant hilar biliary obstruction: A prospective multicenter observational cohort study. J. Clin. Gastroenterol. 2008, 42, 1040–1046. [Google Scholar] [CrossRef]
- Deviere, J.; Baize, M.; de Toeuf, J.; Cremer, M. Long-term follow-up of patients with hilar malignant stricture treated by endoscopic internal biliary drainage. Gastrointest. Endosc. 1988, 34, 95–101. [Google Scholar] [CrossRef]
- Inal, M.; Akgul, E.; Aksungur, E.; Seydaoglu, G. Percutaneous placement of biliary metallic stents in patients with malignant hilar obstruction: Unilobar versus bilobar drainage. J. Vasc. Interv. Radiol. 2003, 14, 1409–1416. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Park, J.K.; Yoon, W.J.; Lee, J.K.; Ryu, J.K.; Yoon, Y.B.; Kim, Y.T. Optimal biliary drainage for inoperable Klatskin’s tumor based on Bismuth type. World J. Gastroenterol. 2007, 13, 3948–3955. [Google Scholar] [CrossRef] [PubMed]
- Rerknimitr, R.; Kladcharoen, N.; Mahachai, V.; Kullavanijaya, P. Result of endoscopic biliary drainage in hilar cholangiocarcinoma. J. Clin. Gastroenterol. 2004, 38, 518–523. [Google Scholar] [CrossRef] [PubMed]
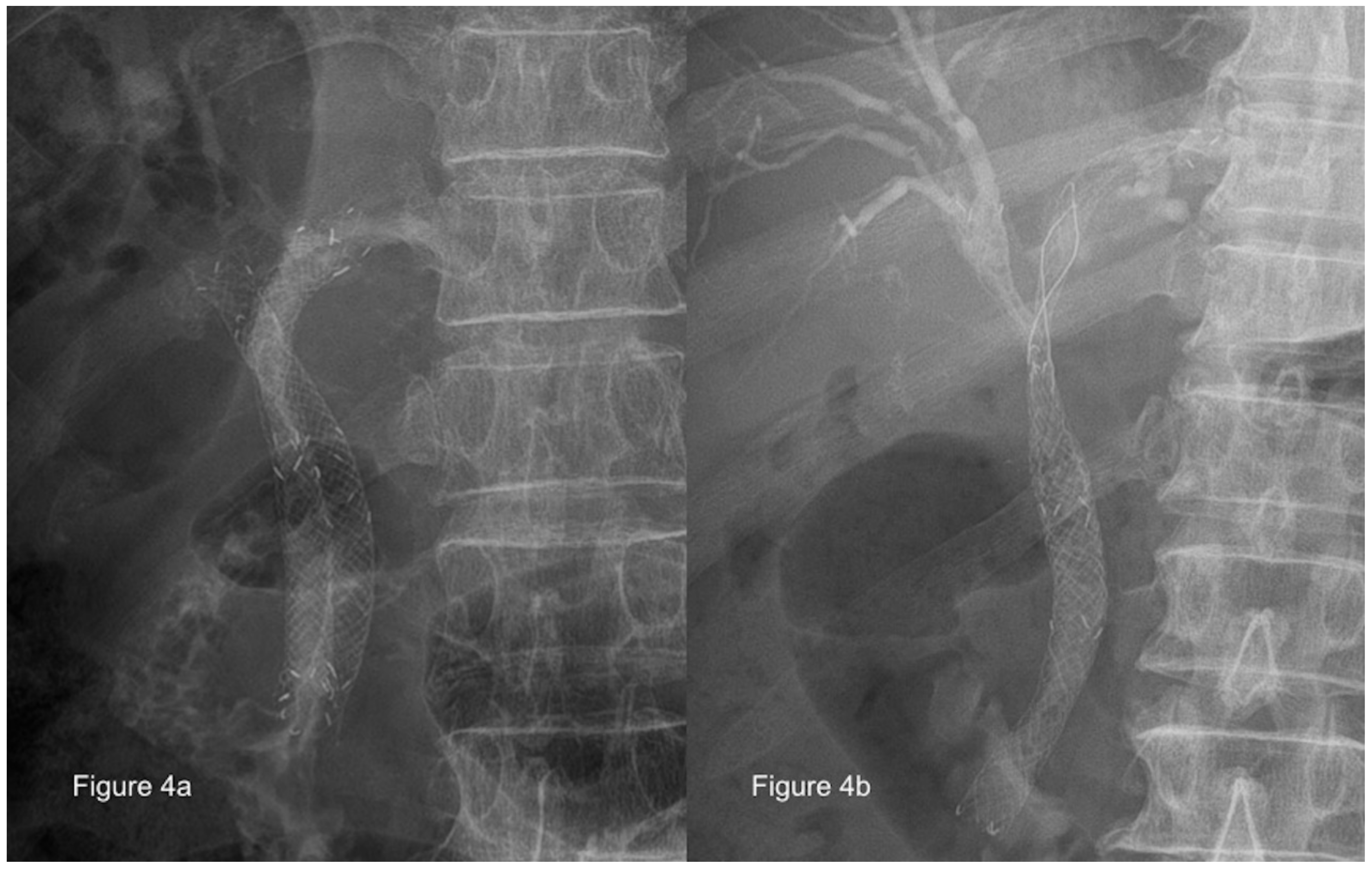
- Paik, W.H.; Park, Y.S.; Hwang, J.H.; Lee, S.H.; Yoon, C.J.; Kang, S.G.; Lee, J.K.; Ryu, J.K.; Kim, Y.T.; Yoon, Y.B. Palliative treatment with self-expandable metallic stents in patients with advanced type III or IV hilar cholangiocarcinoma: A percutaneous versus endoscopic approach. Gastrointest. Endosc. 2009, 69, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Chahal, P.; Baron, T.H. Expandable metal stents for endoscopic bilateral stent-within-stent placement for malignant hilar biliary obstruction. Gastrointest. Endosc. 2010, 71, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Kogure, H.; Isayama, H.; Kawakubo, K.; Sasaki, T.; Yamamoto, N.; Hirano, K.; Sasahira, N.; Tsujino, T.; Tada, M.; Koike, K. Endoscopic bilateral metallic stenting for malignant hilar obstruction using newly designed stents. J. Hepatobiliary Pancreat. Sci. 2011, 18, 653–657. [Google Scholar] [CrossRef]
- Hwang, J.C.; Kim, J.H.; Lim, S.G.; Kim, S.S.; Yoo, B.M.; Cho, S.W. Y-shaped endoscopic bilateral metal stent placement for malignant hilar biliary obstruction: Prospective long-term study. Scand. J. Gastroenterol. 2011, 46, 326–332. [Google Scholar] [CrossRef]
- Kogure, H.; Isayama, H.; Nakai, Y.; Tsujino, T.; Ito, Y.; Yamamoto, K.; Mizuno, S.; Yagioka, H.; Kawakubo, K.; Sasaki, T.; et al. Newly designed large cell Niti-S stent for malignant hilar biliary obstruction: A pilot study. Surg. Endosc. 2011, 25, 463–467. [Google Scholar] [CrossRef]
- Saleem, A.; Baron, T.H.; Gostout, C.J. Large-diameter therapeutic channel duodenoscope to facilitate simultaneous deployment of side-by-side self-expandable metal stents in hilar cholangiocarcinoma. Gastrointest. Endosc. 2010, 72, 628–631. [Google Scholar] [CrossRef]
- Park, D.H.; Lee, S.S.; Moon, J.H.; Choi, H.J.; Cha, S.W.; Kim, J.H.; Seo, D.W.; Lee, S.K.; Park, S.H.; Lee, M.S.; et al. Newly designed stent for endoscopic bilateral stent-in-stent placement of metallic stents in patients with malignant hilar biliary strictures: Multicenter prospective feasibility study (with videos). Gastrointest. Endosc. 2009, 69, 1357–1360. [Google Scholar] [CrossRef]
- Dowsett, J.F.; Vaira, D.; Hatfield, A.R.; Cairns, S.R.; Polydorou, A.; Frost, R.; Croker, J.; Cotton, P.B.; Russell, R.C.; Mason, R.R. Endoscopic biliary therapy using the combined percutaneous and endoscopic technique. Gastroenterology 1989, 96, 1180–1186. [Google Scholar] [CrossRef]
- Bismuth, H. Surgical anatomy and anatomical surgery of the liver. World J. Surg. 1982, 6, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Moy, B.T.; Birk, J.W. An Update to Hepatobiliary Stents. J. Clin. Transl. Hepatol. 2015, 3, 67–77. [Google Scholar] [CrossRef] [PubMed]
- Wagner, H.J.; Knyrim, K.; Vakil, N.; Klose, K.J. Plastic endoprostheses versus metal stents in the palliative treatment of malignant hilar biliary obstruction. A prospective and randomized trial. Endoscopy 1993, 25, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Gupta, K.; Mallery, S.; Li, R.; Kinney, T.; Freeman, M.L. Endoscopic ultrasound rendezvous for bile duct access using a transduodenal approach: Cumulative experience at a single center. A case series. Endoscopy 2010, 42, 496–502. [Google Scholar] [CrossRef] [PubMed]
- Dhir, V.; Bhandari, S.; Bapat, M.; Maydeo, A. Comparison of EUS-guided rendezvous and precut papillotomy techniques for biliary access (with videos). Gastrointest. Endosc. 2012, 75, 354–359. [Google Scholar] [CrossRef] [PubMed]
- Will, U.; Thieme, A.; Fueldner, F.; Gerlach, R.; Wanzar, I.; Meyer, F. Treatment of biliary obstruction in selected patients by endoscopic ultrasonography (EUS)-guided transluminal biliary drainage. Endoscopy 2007, 39, 292–295. [Google Scholar] [CrossRef]
- Park, D.H.; Song, T.J.; Eum, J.; Moon, S.H.; Lee, S.S.; Seo, D.W.; Lee, S.K.; Kim, M.H. EUS-guided hepaticogastrostomy with a fully covered metal stent as the biliary diversion technique for an occluded biliary metal stent after a failed ERCP (with videos). Gastrointest. Endosc. 2010, 71, 413–419. [Google Scholar] [CrossRef]
- Komaki, T.; Kitano, M.; Sakamoto, H.; Kudo, M. Endoscopic ultrasonography-guided biliary drainage: Evaluation of a choledochoduodenostomy technique. Pancreatology 2011, 11 (Suppl. 2), 47–51. [Google Scholar] [CrossRef]
- Dhir, V.; Itoi, T.; Khashab, M.A.; Park, D.H.; Yuen Bun Teoh, A.; Attam, R.; Messallam, A.; Varadarajulu, S.; Maydeo, A. Multicenter comparative evaluation of endoscopic placement of expandable metal stents for malignant distal common bile duct obstruction by ERCP or EUS-guided approach. Gastrointest. Endosc. 2015, 81, 913–923. [Google Scholar] [CrossRef]



© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, C.-C.; Yang, T.-W.; Sung, W.-W.; Tsai, M.-C. Current Endoscopic Management of Malignant Biliary Stricture. Medicina 2020, 56, 114. https://doi.org/10.3390/medicina56030114
Wang C-C, Yang T-W, Sung W-W, Tsai M-C. Current Endoscopic Management of Malignant Biliary Stricture. Medicina. 2020; 56(3):114. https://doi.org/10.3390/medicina56030114
Chicago/Turabian StyleWang, Chi-Chih, Tzu-Wei Yang, Wen-Wei Sung, and Ming-Chang Tsai. 2020. "Current Endoscopic Management of Malignant Biliary Stricture" Medicina 56, no. 3: 114. https://doi.org/10.3390/medicina56030114
APA StyleWang, C.-C., Yang, T.-W., Sung, W.-W., & Tsai, M.-C. (2020). Current Endoscopic Management of Malignant Biliary Stricture. Medicina, 56(3), 114. https://doi.org/10.3390/medicina56030114






