Implementation of the Obturator Nerve Block into a Supra-Inguinal Fascia Iliaca Compartment Block Based Analgesia Protocol for Hip Arthroscopy: Retrospective Pre-Post Study
Abstract
:1. Introduction
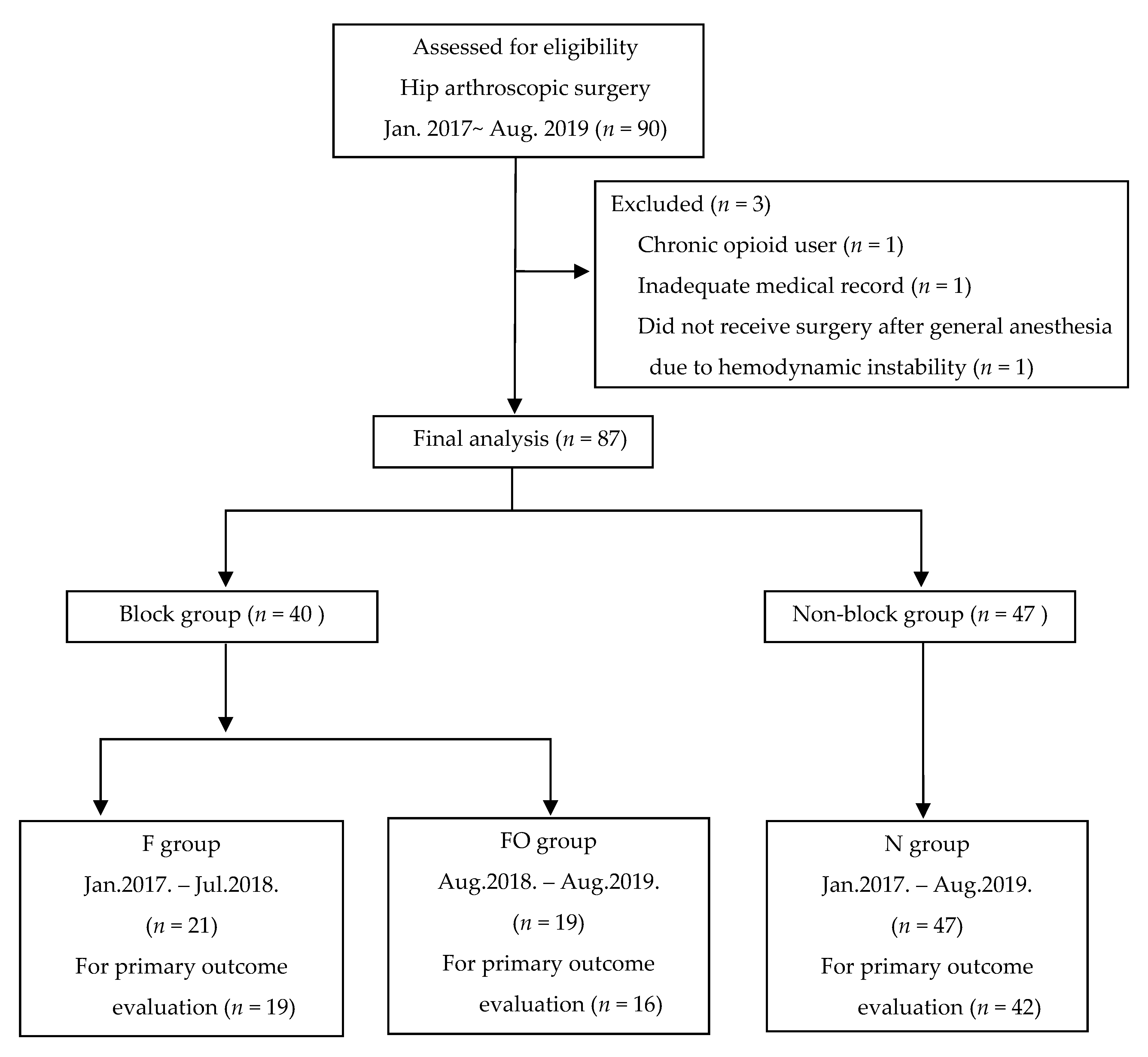
2. Materials and Methods
2.1. Implementation of Subpectineal Obturator Nerve Block
2.2. Data Collection
2.3. Supra-Inguinal Fascia Iliaca Compartment Block and Subpectineal Obturator Nerve Block
2.4. Anesthesia and Surgery
2.5. Outcome Measures
2.6. Sample Size Calculation and Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bedi, A.; Kelly, B.T.; Khanduja, V. Arthroscopic hip preservation surgery: Current concepts and perspective. Bone Joint J. 2013, 95-B, 10–19. [Google Scholar] [CrossRef]
- Ward, J.P.; Albert, D.B.; Altman, R.; Goldstein, R.Y.; Cuff, G.; Youm, T. Are femoral nerve blocks effective for early postoperative pain management after hip arthroscopy? Arthroscopy 2012, 28, 1064–1069. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhu, W.; Zhu, L.; Du, Y. Efficacy of celecoxib for pain management after arthroscopic surgery of hip: A prospective randomized placebo-controlled study. Eur. J. Orthop. Surg. Traumatol. 2014, 24, 919–923. [Google Scholar] [CrossRef]
- Nielsen, K.C.; Steele, S.M. Outcome after regional anaesthesia in the ambulatory setting--is it really worth it? Best Pract. Res. Clin. Anaesthesiol. 2002, 16, 145–157. [Google Scholar] [CrossRef]
- Shin, J.J.; McCrum, C.L.; Mauro, C.S.; Vyas, D. Pain Management After Hip Arthroscopy: Systematic Review of Randomized Controlled Trials and Cohort Studies. Am. J. Sports Med. 2018, 46, 3288–3298. [Google Scholar] [CrossRef] [PubMed]
- Kay, J.; de Sa, D.; Memon, M.; Simunovic, N.; Paul, J.; Ayeni, O.R. Examining the Role of Perioperative Nerve Blocks in Hip Arthroscopy: A Systematic Review. Arthroscopy 2016, 32, 704–715.e1. [Google Scholar] [CrossRef] [PubMed]
- YaDeau, J.T.; Tedore, T.; Goytizolo, E.A.; Kim, D.H.; Green, D.S.; Westrick, A.; Fan, R.; Rade, M.C.; Ranawat, A.S.; Coleman, S.H.; et al. Lumbar plexus blockade reduces pain after hip arthroscopy: A prospective randomized controlled trial. Anesth Analg. 2012, 115, 968–972. [Google Scholar] [CrossRef] [PubMed]
- Birnbaum, K.; Prescher, A.; Hessler, S.; Heller, K.D. The sensory innervation of the hip joint—An anatomical study. Surg. Radiol. Anat 1997, 19, 371–375. [Google Scholar] [CrossRef] [PubMed]
- Simons, M.J.; Amin, N.H.; Cushner, F.D.; Scuderi, G.R. Characterization of the Neural Anatomy in the Hip Joint to Optimize Periarticular Regional Anesthesia in Total Hip Arthroplasty. J. Surg. Orthop. Adv. 2015, 24, 221–224. [Google Scholar]
- Wolff, A.B.; Hogan, G.W.; Capon, J.M.; Napoli, A.M.; Smith, H.J.; Gaspar, P.S. Pre-operative lumbar plexus block provides superior post-operative analgesia when compared with fascia iliaca block or general anesthesia alone in hip arthroscopy. J. Hip. Preserv. Surg. 2016, 3, 338–345. [Google Scholar] [CrossRef] [Green Version]
- Hebbard, P.; Ivanusic, J.; Sha, S. Ultrasound-guided supra-inguinal fascia iliaca block: A cadaveric evaluation of a novel approach. Anaesthesia 2011, 66, 300–305. [Google Scholar] [CrossRef] [PubMed]
- Vermeylen, K.; Desmet, M.; Leunen, I.; Soetens, F.; Neyrinck, A.; Carens, D.; Caerts, B.; Seynaeve, P.; Hadzic, A.; Van de Velde, M. Supra-inguinal injection for fascia iliaca compartment block results in more consistent spread towards the lumbar plexus than an infra-inguinal injection: A volunteer study. Reg. Anesth. Pain. Med. 2019. [Google Scholar] [CrossRef] [PubMed]
- Vermeylen, K.; Soetens, F.; Leunen, I.; Hadzic, A.; Van Boxtael, S.; Pomes, J.; Prats-Galino, A.; Van de Velde, M.; Neyrinck, A.; Sala-Blanch, X. The effect of the volume of supra-inguinal injected solution on the spread of the injectate under the fascia iliaca: A preliminary study. J. Anesth. 2018, 32, 908–913. [Google Scholar] [CrossRef] [PubMed]
- Swenson, J.D.; Davis, J.J.; Stream, J.O.; Crim, J.R.; Burks, R.T.; Greis, P.E. Local anesthetic injection deep to the fascia iliaca at the level of the inguinal ligament: The pattern of distribution and effects on the obturator nerve. J. Clin. Anesth. 2015, 27, 652–657. [Google Scholar] [CrossRef]
- Bendtsen, T.F.; Pedersen, E.M.; Peng, P. Course of the obturator nerve. Reg. Anesth. Pain. Med. 2019. [Google Scholar] [CrossRef]
- Short, A.J.; Barnett, J.J.G.; Gofeld, M.; Baig, E.; Lam, K.; Agur, A.M.R.; Peng, P.W.H. Anatomic Study of Innervation of the Anterior Hip Capsule: Implication for Image-Guided Intervention. Reg. Anesth. Pain. Med. 2018, 43, 186–192. [Google Scholar] [CrossRef]
- Badiola, I.; Liu, J.; Huang, S.; Kelly, J.D., IV; Elkassabany, N. A comparison of the fascia iliaca block to the lumbar plexus block in providing analgesia following arthroscopic hip surgery: A randomized controlled clinical trial. J. Clin. Anesth. 2018, 49, 26–29. [Google Scholar] [CrossRef]
- Behrends, M.; Yap, E.N.; Zhang, A.L.; Kolodzie, K.; Kinjo, S.; Harbell, M.W.; Aleshi, P. Preoperative Fascia Iliaca Block Does Not Improve Analgesia after Arthroscopic Hip Surgery, but Causes Quadriceps Muscles Weakness: A Randomized, Double-blind Trial. Anesthesiology 2018, 129, 536–543. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gotzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M.; Initiative, S. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Int. J. Surg. 2014, 12, 1500–1524. [Google Scholar] [CrossRef] [Green Version]
- Schwenk, E.S.; Mariano, E.R. Designing the ideal perioperative pain management plan starts with multimodal analgesia. Korean J. Anesthesiol. 2018, 71, 345–352. [Google Scholar] [CrossRef]
- Taha, A.M. Brief reports: Ultrasound-guided obturator nerve block: A proximal interfascial technique. Anesth. Analg. 2012, 114, 236–239. [Google Scholar] [CrossRef] [PubMed]
- Bech, N.H.; Hulst, A.H.; Spuijbroek, J.A.; van Leuken, L.L.; Haverkamp, D. Perioperative pain management in hip arthroscopy: What options are there? J. Hip. Preserv. Surg. 2016, 3, 181–189. [Google Scholar] [CrossRef] [Green Version]
- Desmet, M.; Vermeylen, K.; Van Herreweghe, I.; Carlier, L.; Soetens, F.; Lambrecht, S.; Croes, K.; Pottel, H.; Van de Velde, M. A Longitudinal Supra-Inguinal Fascia Iliaca Compartment Block Reduces Morphine Consumption After Total Hip Arthroplasty. Reg. Anesth. Pain. Med. 2017, 42, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Acharya, R.; Sriramka, B.; Panigrahi, S. Comparison of 4 mg dexamethasone versus 8 mg dexamethasone as an adjuvant to levobupivacaine in fascia iliaca block-a prospective study. Korean J. Pain 2018, 31, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Shariat, A.N.; Hadzic, A.; Xu, D.; Shastri, U.; Kwofie, K.; Gandhi, K.; McCally, C.M.; Gratenstein, K.; Vandepitte, C.; Gadsden, J.; et al. Fascia lliaca block for analgesia after hip arthroplasty: A randomized double-blind, placebo-controlled trial. Reg. Anesth. Pain. Med. 2013, 38, 201–205. [Google Scholar] [CrossRef] [PubMed]
- Kumar, K.; Pandey, R.K.; Bhalla, A.P.; Kashyap, L.; Garg, R.; Darlong, V.; Malhotra, R.; Yadav, C.S. Comparison of conventional infrainguinal versus modified proximal suprainguinal approach of Fascia Iliaca Compartment Block for postoperative analgesia in Total Hip Arthroplasty. A prospective randomized study. Acta Anaesthesiol. Belg. 2015, 66, 95–100. [Google Scholar]
- Alrayashi, W.; Zurakowski, D.; Sullivan, C.A.; Berde, C.B.; Askins, N.; Sinnott, S.; Cravero, J.P. The effect of suprainguinal fascia iliaca block on the recovery of patients after arthroscopic hip surgery. Paediatr. Anaesth. 2019, 29, 829–834. [Google Scholar] [CrossRef]
- Eastburn, E.; Hernandez, M.A.; Boretsky, K. Technical success of the ultrasound-guided supra-inguinal fascia iliaca compartment block in older children and adolescents for hip arthroscopy. Paediatr. Anaesth. 2017, 27, 1120–1124. [Google Scholar] [CrossRef]
- Bouaziz, H.; Vial, F.; Jochum, D.; Macalou, D.; Heck, M.; Meuret, P.; Braun, M.; Laxenaire, M.C. An evaluation of the cutaneous distribution after obturator nerve block. Anesth. Analg. 2002, 94, 445–449. [Google Scholar] [CrossRef]
- Nielsen, T.D.; Moriggl, B.; Soballe, K.; Kolsen-Petersen, J.A.; Borglum, J.; Bendtsen, T.F. A Cadaveric Study of Ultrasound-Guided Subpectineal Injectate Spread Around the Obturator Nerve and Its Hip Articular Branches. Reg. Anesth. Pain. Med. 2017, 42, 357–361. [Google Scholar] [CrossRef]
- Giron-Arango, L.; Peng, P.W.H.; Chin, K.J.; Brull, R.; Perlas, A. Pericapsular Nerve Group (PENG) Block for Hip Fracture. Reg. Anesth. Pain. Med. 2018, 43, 859–863. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, N.D.; Greher, M.; Moriggl, B.; Hoermann, R.; Nielsen, T.D.; Borglum, J.; Bendtsen, T.F. Spread of injectate around hip articular sensory branches of the femoral nerve in cadavers. Reg. Anesth. Pain. Med. 2018, 62, 1001–1006. [Google Scholar] [CrossRef] [PubMed]
| F (N = 21) | FO (N = 19) | N (N = 47) | |
|---|---|---|---|
| Sex | |||
| - Female | 10 (47.6%) | 10 (52.6%) | 22 (46.8%) |
| - Male | 11 (52.4%) | 9 (47.4%) | 25 (53.2%) |
| Age | 37.0 (27.0;52.0) | 38.0 (25.5;45.0) | 39.0 (26.0;47.0) |
| Weight (kg) | 69.2 (61.2;77.0) | 67.9 (63.1;72.3) | 67.3 (57.6;77.6) |
| Height (cm) | 166.0 (161.4;173.6) | 166.6 (161.0;171.2) | 167.1 (162.8;176.0) |
| BMI (kg/m2) | 24.7 (23.3;26.8) | 24.8 (23.1;26.7) | 23.7 (21.8;25.8) |
| Anesthesia time (min) | 165.7 ± 29.2 | 184.2 ± 29.9 | 178.0 ± 26.8 |
| Operation time (min) | 138.0 ± 28.6 | 158.1 ± 27.6 | 156.5 ± 27.6 |
| Hypertension | 1 (4.8%) | 2 (10.5%) | 7 (14.9%) |
| F (N = 19) | FO (N = 16) | N (N = 42) | Overall p | FO vs. F (p adj.) | FO vs. N (p adj.) | F vs. N (p. adj.) | |
|---|---|---|---|---|---|---|---|
| Cumulative postoperative fentanyl consumption (µg) | |||||||
| 6 hours | 249.6 (161.3;350.3) | 163.0 (108.0;341.5] | 293.0 (210.6;385.0) | 0.028 | 0.256 | 0.028 | 0.258 |
| 12 hours | 372.6 (297.0;458.0) | 256.2 (186.1;420.0] | 402.0 (300.0;582.0) | 0.024 | 0.207 | 0.020 | 0.289 |
| 24 hours | 636.0 (426.8;803.0) | 482.8 (305.8;635.0] | 678.5 (444.0;890.0) | 0.018 | 0.066 | 0.014 | 0.598 |
| F (N = 21) | FO (N = 19) | N (N = 47) | |||||
| Intraoperative remifentanil dose (µg/kg/min) | 0.069 (0.056;0.075) | 0.059 (0.055;0.068] | 0.089 (0.069;0.102) | 0.001 | 0.320 | 0.003 | 0.004 |
| F (N = 21) | FO (N = 19) | N (N = 47) | p | |
|---|---|---|---|---|
| Pain score during postoperative 24 hours | ||||
| PACU | 4.0 (3.0;5.0) | 3.0 (2.0;4.0) | 4.0 (3.0;6.0) | 0.039 |
| Lowest | 2.0 (2.0;2.0) | 2.0 (1.0;2.0) | 2.0 (2.0;2.5) | 0.039 |
| Highest | 4.0 (3.0;6.0) | 5.0 (3.5;5.5) | 5.0 (4.0;7.0) | 0.124 |
| Additional Demerol usage | 4 (19.0%) | 7 (36.8%) | 15 (31.9%) | 0.426 |
| Hypertension | 2 (9.5%) | 0 (0.0%) | 2 (4.3%) | 0.352 |
| Hypotension | 7 (33.3%) | 10 (52.6%) | 16 (34.0%) | 0.327 |
| Phenylephrine (0/1/2/3) | 14/5/1/1 | 9/7/3/0 | 32/9/4/2 | 0.551 |
| Nicardipine (0/1/2/3) | 19/2/0/0 | 17/2/0/0 | 43/1/1/2 | 0.556 |
| PONV | 7 (33.3%) | 6 (31.6%) | 14 (29.8%) | 0.957 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.; Hwang, J.-M.; Lee, S.; Eom, H.; Oh, C.; Chung, W.; Ko, Y.-K.; Lee, W.; Hong, B.; Hwang, D.-S. Implementation of the Obturator Nerve Block into a Supra-Inguinal Fascia Iliaca Compartment Block Based Analgesia Protocol for Hip Arthroscopy: Retrospective Pre-Post Study. Medicina 2020, 56, 150. https://doi.org/10.3390/medicina56040150
Lee S, Hwang J-M, Lee S, Eom H, Oh C, Chung W, Ko Y-K, Lee W, Hong B, Hwang D-S. Implementation of the Obturator Nerve Block into a Supra-Inguinal Fascia Iliaca Compartment Block Based Analgesia Protocol for Hip Arthroscopy: Retrospective Pre-Post Study. Medicina. 2020; 56(4):150. https://doi.org/10.3390/medicina56040150
Chicago/Turabian StyleLee, Seounghun, Jung-Mo Hwang, Sangmin Lee, Hongsik Eom, Chahyun Oh, Woosuk Chung, Young-Kwon Ko, Wonhyung Lee, Boohwi Hong, and Deuk-Soo Hwang. 2020. "Implementation of the Obturator Nerve Block into a Supra-Inguinal Fascia Iliaca Compartment Block Based Analgesia Protocol for Hip Arthroscopy: Retrospective Pre-Post Study" Medicina 56, no. 4: 150. https://doi.org/10.3390/medicina56040150





