Access to Dental Care and Depressive Illness: Results from the Korea National Health Nutrition Examination Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source and Study Population
2.2. Definitions of “Current Depression” and “No-Dental Visit with Care Needs”
2.3. Statistical Analysis
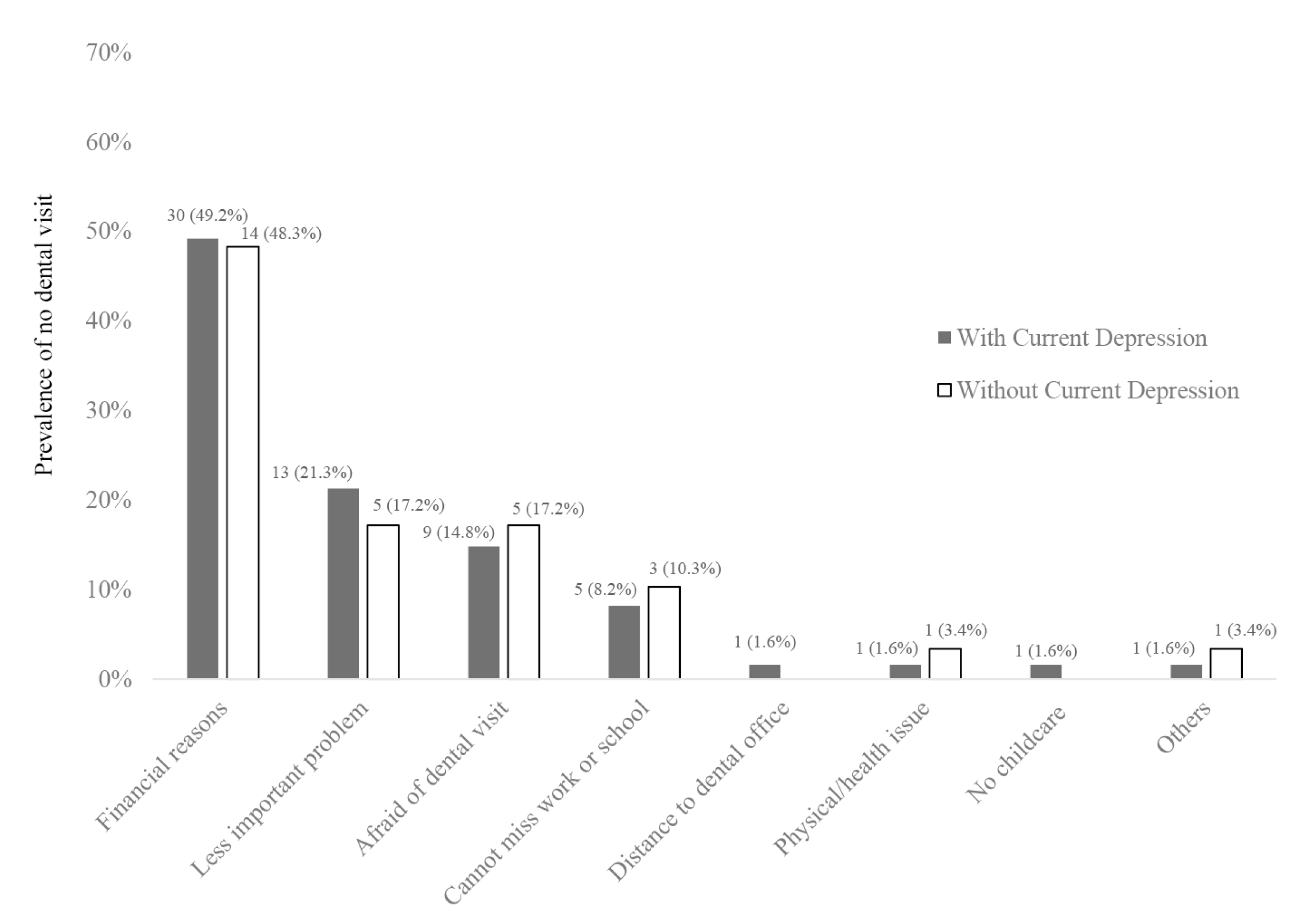
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. Oral Health. Available online: https://www.who.int/health-topics/oral-health/#tab=tab_1 (accessed on 13 April 2020).
- Wu, B.; Fillenbaum, G.G.; Plassman, B.L.; Guo, L. Association Between Oral Health and Cognitive Status: A Systematic Review. J. Am. Geriatr. Soc. 2016, 64, 739–751. [Google Scholar] [CrossRef] [Green Version]
- Barbosa, T.D.S.; Gavião, M.B.D.; Castelo, P.M.; Leme, M.S. Factors Associated with Oral Health-related Quality of Life in Children and Preadolescents: A Cross-sectional Study. Oral Health Prev. Dent. 2016, 14, 137–148. [Google Scholar]
- Corridore, D.; Guerra, F.; La Marra, C.; Di Thiene, D.; Ottolenghi, L. Oral Health Status and Oral Health-Related Quality of Life in Italian Deinstitutionalized Psychiatric Patients. Clin. Ter. 2017, 168, e77–e83. [Google Scholar] [PubMed]
- Ortíz-Barrios, L.B.; Granados-García, V.; Cruz-Hervert, L.P.; Moreno-Tamayo, K.; Heredia-Ponce, E.; Sánchez-García, S. The impact of poor oral health on the oral health-related quality of life (OHRQoL) in older adults: The oral health status through a latent class analysis. BMC Oral Health 2019, 19, 141. [Google Scholar] [CrossRef] [PubMed]
- Scannapieco, F.; Cantos, A. Oral inflammation and infection, and chronic medical diseases: Implications for the elderly. Periodontology 2000 2016, 72, 153–175. [Google Scholar] [CrossRef] [PubMed]
- Linden, G.J.; Lyons, A.; Scannapieco, F.A. Periodontal systemic associations: Review of the evidence. J. Periodontol. 2013, 84 (Suppl. 4), S8–S19. [Google Scholar] [CrossRef]
- Nascimento, S.; González, A.; Roza, B.D.A.; Pimentel, C.; Schirmer, J.; Mucci, S.; Abranches, D. Development of Routine Dental Care for Liver Transplant Outpatients. Transplant. Proc. 2018, 50, 779–783. [Google Scholar] [CrossRef]
- Kossioni, A.E.; Hajto-Bryk, J.; Maggi, S.; McKenna, G.; Petrovic, M.; Roller-Wirnsberger, R.E.; Schimmel, M.; Tamulaitiene, M.; Vanobbergen, J.; Müller, F.; et al. An Expert Opinion from the European College of Gerodontology and the European Geriatric Medicine Society: European Policy Recommendations on Oral Health in Older Adults. J. Am. Geriatr. Soc. 2017, 66, 609–613. [Google Scholar] [CrossRef] [Green Version]
- Kisely, S.; Baghaie, H.; Lalloo, R.; Siskind, D.; Johnson, N.W. A Systematic Review and Meta-Analysis of the Association Between Poor Oral Health and Severe Mental Illness. Psychosom. Med. 2015, 77, 83–92. [Google Scholar] [CrossRef]
- Ross, L.E.; Vigod, S.N.; Wishart, J.; Waese, M.; Spence, J.D.; Oliver, J.; Chambers, J.; Anderson, S.; Shields, R. Barriers and facilitators to primary care for people with mental health and/or substance use issues: A qualitative study. BMC Fam. Pract. 2015, 16, 135. [Google Scholar] [CrossRef] [Green Version]
- Heaton, L.J.; Mancl, L.; Grembowski, D.; Armfield, J.; Milgrom, P. Unmet dental need in community-dwelling adults with mental illness: Results from the 2007 Medical Expenditure Panel Survey. J. Am. Dent. Assoc. 2013, 144, e16–e23. [Google Scholar] [CrossRef] [PubMed]
- Whiteford, H.A.; Degenhardt, L.; Rehm, J.; Baxter, A.; Ferrari, A.J.; Erskine, H.; Charlson, F.; Norman, R.E.; Flaxman, A.D.; Johns, N.; et al. Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. Lancet 2013, 382, 1575–1586. [Google Scholar] [CrossRef]
- Juul, S.H.; Nemeroff, C.B. Psychiatric epidemiology. Handb. Clin. Neurol. 2012, 106, 167–189. [Google Scholar] [PubMed]
- Shippee, N.; Shah, N.D.; Williams, M.D.; Moriarty, J.; Frye, M.A.; Ziegenfuss, J.Y. Differences in demographic composition and in work, social, and functional limitations among the populations with unipolar depression and bipolar disorder: Results from a nationally representative sample. Health Qual. Life Outcomes 2011, 9, 90. [Google Scholar] [CrossRef] [Green Version]
- McCabe, M.P.; Leas, L. A qualitative study of primary health care access, barriers and satisfaction among people with mental illness. Psychol. Health Med. 2008, 13, 303–312. [Google Scholar] [CrossRef] [Green Version]
- Ngo, D.Y.J.; Thomson, W.M.; Subramaniam, M.; Abdin, E.; Ang, K.-Y. The oral health of long-term psychiatric inpatients in Singapore. Psychiatry Res. 2018, 266, 206–211. [Google Scholar] [CrossRef]
- Olivan-Blázquez, B.; Montero-Marin, J.; Campayo, J.; Vicens-Pons, E.; Serrano-Ripoll, M.J.; Castro, A.; Sarasa-Bosque, M.C.; Mendive-Arbeloa, J.M.; López-Del-Hoyo, Y.; García-Campayo, J. Facilitators and barriers to modifying dietary and hygiene behaviours as adjuvant treatment in patients with depression in primary care: A qualitative study. BMC Psychiatry 2018, 18, 205. [Google Scholar] [CrossRef]
- Teng, P.-R.; Su, J.-M.; Chang, W.-H.; Lai, T.-J. Oral health of psychiatric inpatients: A survey of central Taiwan hospitals. Gen. Hosp. Psychiatry 2011, 33, 253–259. [Google Scholar] [CrossRef]
- Coelho, J.M.F.; Miranda, S.S.; Da Cruz, S.S.; Dos Santos, D.N.; Trindade, S.C.; Cerqueira, E.D.M.M.; Passos-Soares, J.D.S.; Costa, M.D.C.N.; Figueiredo, A.C.M.G.; Hintz, A.M.; et al. Common mental disorder is associated with periodontitis. J. Periodontal Res. 2020, 55, 221–228. [Google Scholar] [CrossRef]
- Nascimento, G.G.; Gastal, M.T.; Leite, F.R.M.; Quevedo, L.A.; Peres, K.G.; Peres, M.A.; Horta, B.L.; Barros, F.C.; Demarco, F.F.; Demarco, F.F. Is there an association between depression and periodontitis? A birth cohort study. J. Clin. Periodontol. 2018, 46. [Google Scholar] [CrossRef] [Green Version]
- Cunha, F.A.; Cota, L.D.M.; Cortelli, S.C.; Miranda, T.B.; Neves, F.S.; Cortelli, J.R.; Costa, F.O. Periodontal condition and levels of bacteria associated with periodontitis in individuals with bipolar affective disorders: A case-control study. J. Periodontal Res. 2018, 54, 63–72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, C.-K.; Wu, Y.-T.; Chang, Y.-C. Association between chronic periodontitis and the risk of Alzheimer’s disease: A retrospective, population-based, matched-cohort study. Alzheimer’s Res. Ther. 2017, 9, 56. [Google Scholar] [CrossRef]
- Isola, G.; Polizzi, A.; Alibrandi, A.; Indelicato, F.; Ferlito, S. Analysis of Endothelin-1 Concentrations in Individuals with Periodontitis. Sci. Rep. 2020, 10, 1652–1658. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Ni, J.; Liu, Y.; Teeling, J.; Takayama, F.; Collcutt, A.; Ibbett, P.; Nakanishi, H. Cathepsin B plays a critical role in inducing Alzheimer’s disease-like phenotypes following chronic systemic exposure to lipopolysaccharide from Porphyromonas gingivalis in mice. Brain Behav. Immun. 2017, 65, 350–361. [Google Scholar] [CrossRef] [PubMed]
- Blas, E.; Kurup, A.S. Equity, Social Determinants and Public Health Programmes; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Park, H.-J.; Lee, J.-H. The effect of socioeconomic status, oral health consciousness and behaviors on the periodontal-health disparities among Korean adults. Korean J. Health Educ. Promot. 2010, 27, 61–69. [Google Scholar]
- Lee, J.-H.; Ahn, E. Factors Affecting Dental Utilization and Dental Expenses in the Economically Active Population: Based on the 2010~2014 Korea Health Panel Data. J. Dent. Hyg. Sci. 2019, 19, 23–30. [Google Scholar] [CrossRef] [Green Version]
- McNeil, D.W.; Hayes, S.E.; Randall, C.L.; Polk, D.E.; Neiswanger, K.; Shaffer, J.R.; Weyant, R.J.; Foxman, B.; Kao, E.; Crout, R.J.; et al. Depression and Rural Environment are Associated With Poor Oral Health Among Pregnant Women in Northern Appalachia. Behav. Modif. 2015, 40, 325–340. [Google Scholar] [CrossRef]
- Skośkiewicz-Malinowska, K.; Malicka, B.; Ziętek, M.; Kaczmarek, U. Oral health condition and occurrence of depression in the elderly. Medicine 2018, 97, e12490. [Google Scholar] [CrossRef]
- Barbosa, A.C.; Pinho, R.C.M.; Vasconcelos, M.M.V.B.; Magalhães, B.G.; Santos, M.T.B.R.; Caldas, A., Jr. Association between symptoms of depression and oral health conditions. Spéc. Care Dent. 2018, 38, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Korea National Health & Nutrition Examination Survey Overview. Available online: https://knhanes.cdc.go.kr/knhanes/eng/index.do (accessed on 24 September 2019).
- The Sixth Korea National Health and Nutrition Examination Survey (KNHANES VI) Guidebook for Surveyor. Available online: https://knhanes.cdc.go.kr/knhanes/sub04/sub04_02_02.do?classType=4 (accessed on 3 February 2020).
- The Sixth Korea National Health and Nutrition Examination Survey (KNHANES VI) Guidebook for Data Users. Available online: https://knhanes.cdc.go.kr/knhanes/sub03/sub03_06_02.do (accessed on 3 February 2020).
- Littlejohn, G.O.; Tymms, K.E.; Smith, T.; Griffiths, H.T. Using big data from real-world Australian rheumatology encounters to enhance clinical care and research. Clin. Exp. Rheumatol. 2019. Epub ahead of print. [Google Scholar]
- Baker, S. Real world evidence. Br. Dent. J. 2012, 213, 490–491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anttila, S.; Knuuttila, M.; Ylöstalo, P.; Joukamaa, M. Symptoms of depression and anxiety in relation to dental health behavior and self-perceived dental treatment need. Eur. J. Oral Sci. 2006, 114, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Delgado-Angulo, E.; Sabbah, W.; Suominen, A.L.; Vehkalahti, M.M.; Knuuttila, M.; Partonen, T.; Nordblad, A.; Sheiham, A.; Watt, R.G.; Tsakos, G. The association of depression and anxiety with dental caries and periodontal disease among Finnish adults. Community Dent. Oral Epidemiol. 2015, 43, 540–549. [Google Scholar] [CrossRef] [PubMed]
- Ababneh, K.; Al Shaar, M.; Taani, D. Depressive symptoms in relation to periodontal health in a Jordanian sample. Int. J. Dent. Hyg. 2010, 8, 16–21. [Google Scholar] [CrossRef]
- Rao, S.R.; Sundararajan, S.; Muthukumar, S. Relationship between depression and chronic periodontitis. J. Indian Soc. Periodontol. 2015, 19, 294–296. [Google Scholar] [CrossRef]
- Cademartori, M.G.; Gastal, M.T.; Nascimento, G.G.; Demarco, F.F.; Correa, M.B. Is depression associated with oral health outcomes in adults and elders? A systematic review and meta-analysis. Clin. Oral Investig. 2018, 22, 2685–2702. [Google Scholar] [CrossRef]
- Anttila, S.S.; Knuuttila, M.L.E.; Sakki, T.K. Depressive symptoms favor abundant growth of salivary lactobacilli. Psychosom. Med. 1999, 61, 508–512. [Google Scholar] [CrossRef]
- Peeters, F. Risks for Oral Health With the Use of Antidepressants. Gen. Hosp. Psychiatry 1998, 20, 150–154. [Google Scholar] [CrossRef]
- Thomson, W.M.; Williams, S.M.; Broadbent, J.M.; Poulton, R.; Locker, D. Long-term dental visiting patterns and adult oral health. J. Dent. Res. 2010, 89, 307–311. [Google Scholar] [CrossRef]
- Slack-Smith, L.; Hearn, L.; Scrine, C.; Durey, A. Barriers and enablers for oral health care for people affected by mental health disorders. Aust. Dent. J. 2017, 62, 6–13. [Google Scholar] [CrossRef] [Green Version]
- Hayashi, K.; Izumi, M.; Mastuda, Y.; Isobe, A.; Akifusa, S. Relationship between anxiety/depression and oral health-related quality of life in inpatients of convalescent hospitals. Odontology 2018, 107, 254–260. [Google Scholar] [CrossRef] [PubMed]
- McKibbin, C.L.; Kitchen–Andren, K.A.; Lee, A.A.; Wykes, T.L.; Bourassa, K.A. Oral Health in Adults with Serious Mental Illness: Needs for and Perspectives on Care. Community Ment. Health J. 2014, 51, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Lenk, M.; Berth, H.; Joraschky, P.; Petrowski, K.; Weidner, K.; Hannig, C. Fear of dental treatment—An underrecognized symptom in people with impaired mental health. Dtsch. Arztebl. Int. 2013, 110, 517–522. [Google Scholar] [PubMed] [Green Version]
- Kisely, S.; Sawyer, E.; Siskind, D.; Lalloo, R. The oral health of people with anxiety and depressive disorders —A systematic review and meta-analysis. J. Affect. Disord. 2016, 200, 119–132. [Google Scholar] [CrossRef] [PubMed]
- D’Mello, D.A. Are your patients depressed? Implications for dental practice. J. Mich. Dent. Assoc. 2003, 85, 26–32. [Google Scholar] [PubMed]
- Wilson, N.H.; Soni, A. Interprofessional working: A spearhead opportunity for dentistry and pharmacy. Br. Dent. J. 2016, 221, 607–608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farmer, J.; Ramraj, C.; Azarpazhooh, A.; Dempster, L.; Ravaghi, V.; Quiñonez, C. Comparing self-reported and clinically diagnosed unmet dental treatment needs using a nationally representative survey. J. Public Health Dent. 2017, 77, 295–301. [Google Scholar] [CrossRef]

| Characteristics | Unweighted n (%) | Weighted n (%) * | |
|---|---|---|---|
| Total participants | 5976 (100.0) | 40,767,232 (100.0) | |
| Age (years) | 19–34 | 1186 (19.8) | 11,530,548 (28.3) |
| 35–49 | 1571 (26.3) | 12,343,891(30.3) | |
| 50–64 | 1633 (27.3) | 10,507,234 (25.8) | |
| 65 and over | 1586 (26.5) | 6,385,559 (15.7) | |
| Gender | Female | 3292 (58.0) | 20,625,518 (50.6) |
| Male | 2385 (42.0) | 20,141,714 (49.4) | |
| Education | Middle school or less | 1757 (35.2) | 9,188,642 (25.8) |
| High school graduate | 1644 (32.9) | 13,614,618 (38.3) | |
| College graduate or higher | 1589 (31.9) | 12,755,125 (35.9) | |
| Marital status | Single | 902 (15.1) | 8,834,862 (22.0) |
| Married | 5073 (84.9) | 31,914,132 (78.0) | |
| Health Insurance | Self-employed | 1834 (32.9) | 13,196,940 (33.0) |
| Workplace | 3532 (63.3) | 25,537,110 (63.8) | |
| Others § | 210 (3.8) | 1,313,596 (3.3) | |
| No-dental visit with care needs † | Yes | 1655 (27.7) | 11,907,286 (29.2) |
| Participant Characteristics | Unadjusted OR (95% CI) * | Adjusted OR (95% CI) * |
|---|---|---|
| Current depression † | ||
| No | 1 | 1 |
| Yes | 2.033 (1.027–4.027) § | 2.262 (1.138–4.497) § |
| Age (years) | ||
| 19–34 | 1 | 1 |
| 35–49 | 0.996 (0.818–1.214) | 0.587 (0.184–1.875) |
| 50–64 | 0.905 (0.757–1.080) | 1.705 (0.536–5.426) |
| 65 and over | 0.648 (0.536–0.784)§ | 0.827 (0.212–3.232) |
| Gender | ||
| Female | 1 | 1 |
| Male | 0.817 (0.710–0.941)§ | 0.424 (0.167–1.078) |
| Education | ||
| Elementary school | 1 | 1 |
| Middle school | 1.098(0.861–1.400) | 0.355 (0.124–1.015) |
| High school | 1.098 (0.919–1.312) | 1.081 (0.453–2.580) |
| College graduate or higher | 1.033 (0.862–1.240) | 0.589 (0.199–1.744) |
| Marital status | ||
| Single | 1 | 1 |
| Married | 0.947 (0.779–1.153) | 0.490 (0.139–1.736) |
| Health Insurance | ||
| Workplace (employment) | 1 | 1 |
| Self-employed (community) | 1.126 (0.846–1.499) | 1.053 (0.427–2.601) |
| Others ** | 1.048 (0.906–1.213) | 1.866 (0.884–3.941) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, K.H.; Shin, S.; Lee, E.; Lee, S.-W. Access to Dental Care and Depressive Illness: Results from the Korea National Health Nutrition Examination Survey. Medicina 2020, 56, 189. https://doi.org/10.3390/medicina56040189
Choi KH, Shin S, Lee E, Lee S-W. Access to Dental Care and Depressive Illness: Results from the Korea National Health Nutrition Examination Survey. Medicina. 2020; 56(4):189. https://doi.org/10.3390/medicina56040189
Chicago/Turabian StyleChoi, Kyung Hee, Sangyoon Shin, Euni Lee, and Seok-Woo Lee. 2020. "Access to Dental Care and Depressive Illness: Results from the Korea National Health Nutrition Examination Survey" Medicina 56, no. 4: 189. https://doi.org/10.3390/medicina56040189





