Transforaminal Epiduroscopic Laser Ablation for Removal of a Postlaminectomy Synovial Cyst: A Case Report
Abstract
:1. Introduction
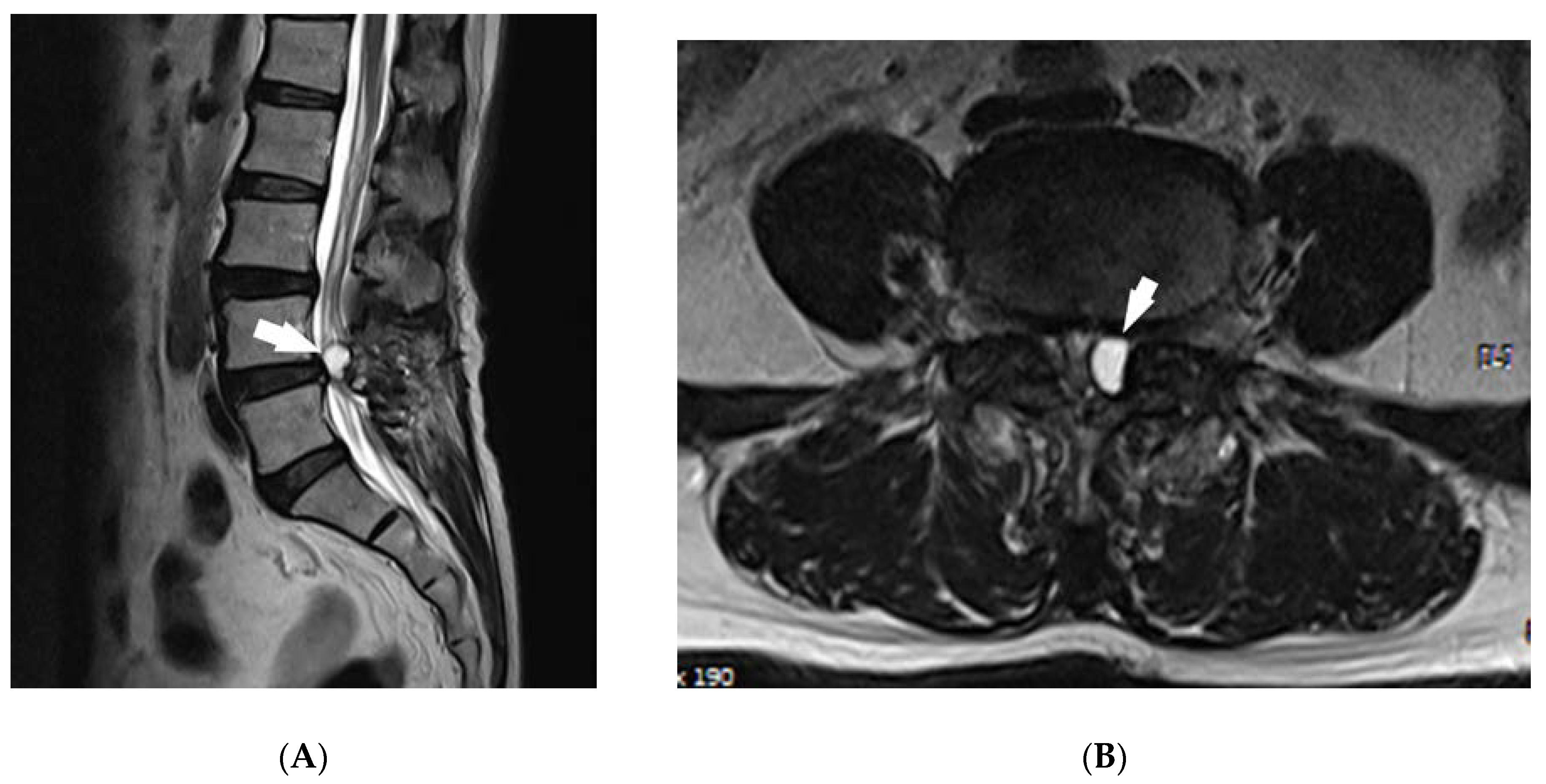
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Daentzer, D.; Stüder, D. Thoracic juxtafacet cyst (JFC) as a rare cause of myelopathy—An additional reference to support the instability theory. Jt. Bone Spine 2010, 77, 178–180. [Google Scholar] [CrossRef] [PubMed]
- Shah, R.V.; Lutz, G.E. Lumbar intraspinal synovial cysts: Conservative management and review of the world’s literature. Spine J. 2003, 3, 479–488. [Google Scholar] [CrossRef]
- Cho, S.I.; Lee, J.H.; Chough, C.K. Postlaminectomy Bilateral Lumbar Intraspinal Synovial Cysts. Korean J. Spine 2016, 13, 157–159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walcott, B.; Coumans, J.-V.C.E. Postlaminectomy synovial cyst formation: A possible consequence of ligamentum flavum excision. J. Clin. Neurosci. 2012, 19, 252–254. [Google Scholar] [CrossRef] [PubMed]
- Parlier-Cuau, C.; Wybier, M.; Nizard, R.; Champsaur, P.; Le Hir, P.; Laredo, J.-D. Symptomatic Lumbar Facet Joint Synovial Cysts: Clinical Assessment of Facet Joint Steroid Injection after 1 and 6 Months and Long-term Follow-up in 30 Patients. Radiol 1999, 210, 509–513. [Google Scholar] [CrossRef] [PubMed]
- Trummer, M.; Flaschka, G.; Tillich, M.; Homann, C.N.; Unger, F.; Eustacchio, S. Diagnosis and surgical management of intraspinal synovial cysts: Report of 19 cases. J. Neurol. Neurosurg. Psychiatry 2001, 70, 74–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wun, K.; Hashmi, S.Z.; Maslak, J.; Schneider, A.; Katchko, K.M.; Singh, G.; Patel, A.A.; Hsu, W.K. The Variability of Lumbar Facet Joint Synovial Cyst Recurrence Requiring Revision Surgery After Decompression-only and Decompression/Fusion. Clin. Spine Surg. 2019, 32, E457–E461. [Google Scholar] [CrossRef] [PubMed]
- Lutz, G.E.; Nicoletti, M.R.; Cyril, G.E.; Harrison, J.; Lutz, C.; Solomon, J.L.; Cooke, P.M.; Wyss, J.F.; Herzog, R.J.; Moley, P.J. Percutaneous Rupture of Zygapophyseal Joint Synovial Cysts: A Prospective Assessment of Nonsurgical Management. PM&R 2017, 10, 245–253. [Google Scholar] [CrossRef]
- Kim, J.-S.; Choi, G.; Jin, S.-R.; Lee, S.-H. Removal of a Discal Cyst Using a Percutaneous Endoscopic Interlaminar Approach: A Case Report. Photomed. Laser Surg. 2009, 27, 365–369. [Google Scholar] [CrossRef] [PubMed]
- Ruetten, S.; Meyer, O.; Godolias, G. Application of Holmium:YAG Laser in Epiduroscopy: Extended Practicabilities in the Treatment of Chronic Back Pain Syndrome. J. Clin. Laser Med. Surg. 2002, 20, 203–206. [Google Scholar] [CrossRef] [PubMed]
- Park, C.H.; Lee, K.K.; Lee, S.H. Efficacy of transforaminal laser annuloplasty versus intradiscal radiofrequency annuloplasty for discogenic low back pain. Korean J. Pain 2019, 32, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Moon, B.J.; Lee, H.Y.; Kim, K.N.; Yi, S.; Ha, Y.; Yoon, D.H.; Shin, D.A. Experimental Evaluation of Percutaneous Lumbar Laser Disc Decompression Using a 1414 nm Nd:YAG Laser. Pain Physician 2015, 18, 1091–1099. [Google Scholar]
- Jayasree, R.S.; Gupta, A.K.; Bodhey, N.K.; Mohanty, M. Effect of 980-nm Diode Laser and 1064-nm Nd:YAG Laser on the Intervertebral Disc—In Vitroandin VivoStudies. Photomed. Laser Surg. 2009, 27, 547–552. [Google Scholar] [CrossRef] [PubMed]
- Shearer, T.R.; Kinsley, M.A.; Pease, A.P.; Patterson, J.S. Development of a minimally invasive approach to equine cervical articular facet joints for placement of an ND:YAG LASER. Can. Vet. J. 2017, 58, 1181–1186. [Google Scholar]
- Eshraghi, Y.; Desai, V.; Cajigal, C.C.; Tabbaa, K. Outcome of Percutaneous Lumbar Synovial Cyst Rupture in Patients with Lumbar Radiculopathy. Pain Physician 2016, 19. [Google Scholar]
- Finkelstein, S.D.; Sayegh, R.; Watson, P.; Knuckey, N. Juxta-facet cysts. Report of two cases and review of clinicopathologic features. Spine 1993, 18, 779–782. [Google Scholar] [CrossRef] [PubMed]
- Imai, K.; Nakamura, K.; Inokuchi, K.; Oda, H. Aspiration of intraspinal synovial cyst: Recurrence after temporal improvement. Arch. Orthop. Trauma Surg. 1998, 118, 103–105. [Google Scholar] [CrossRef] [PubMed]


© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, H.Y.; Kim, S.Y.; Lee, C.H.; Park, S.W. Transforaminal Epiduroscopic Laser Ablation for Removal of a Postlaminectomy Synovial Cyst: A Case Report. Medicina 2020, 56, 209. https://doi.org/10.3390/medicina56050209
Kang HY, Kim SY, Lee CH, Park SW. Transforaminal Epiduroscopic Laser Ablation for Removal of a Postlaminectomy Synovial Cyst: A Case Report. Medicina. 2020; 56(5):209. https://doi.org/10.3390/medicina56050209
Chicago/Turabian StyleKang, Hee Yong, So Yeon Kim, Chung Hun Lee, and Sung Wook Park. 2020. "Transforaminal Epiduroscopic Laser Ablation for Removal of a Postlaminectomy Synovial Cyst: A Case Report" Medicina 56, no. 5: 209. https://doi.org/10.3390/medicina56050209





