Serum Potassium Levels at Hospital Discharge and One-Year Mortality among Hospitalized Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. Clinical Characteristics
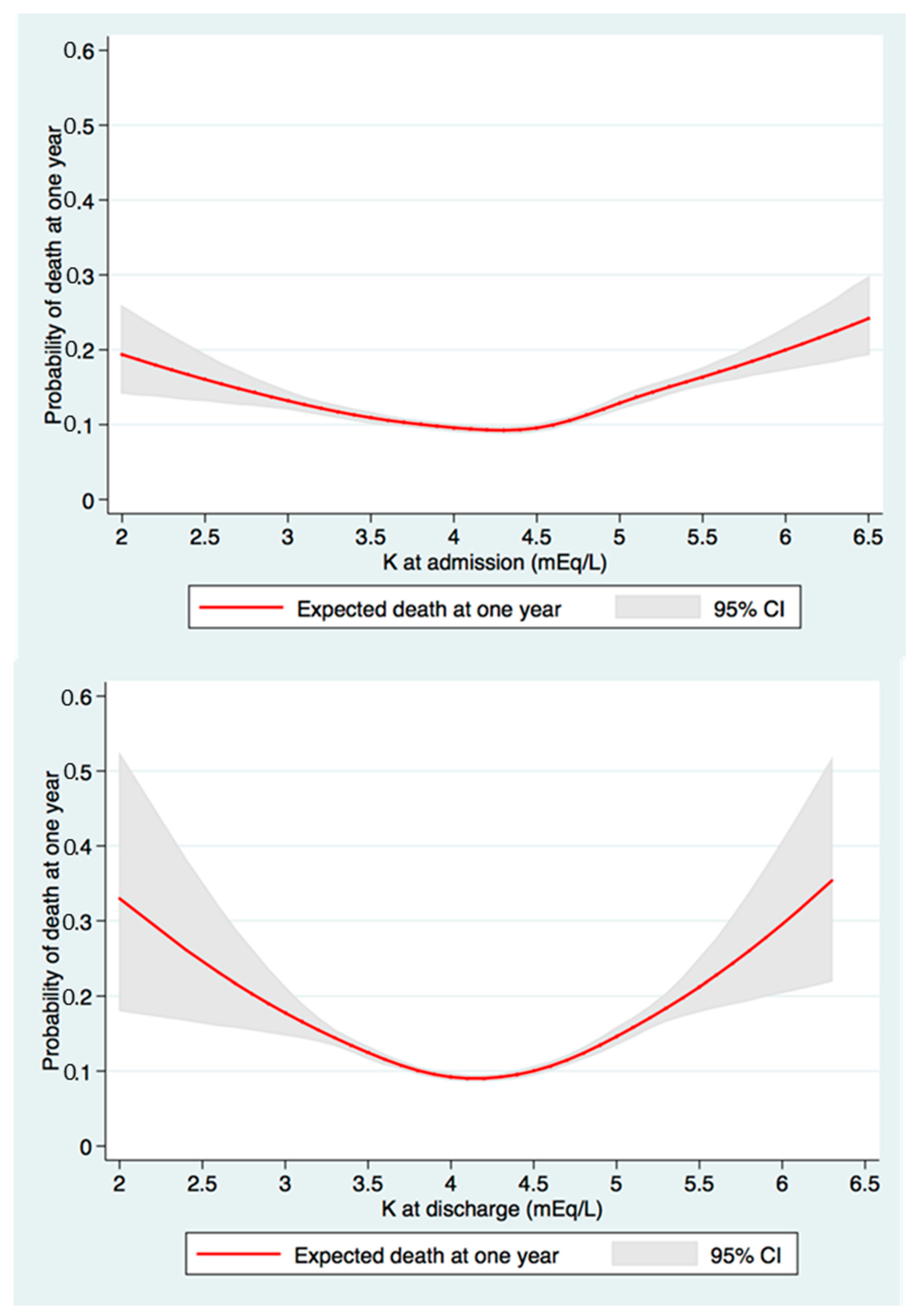
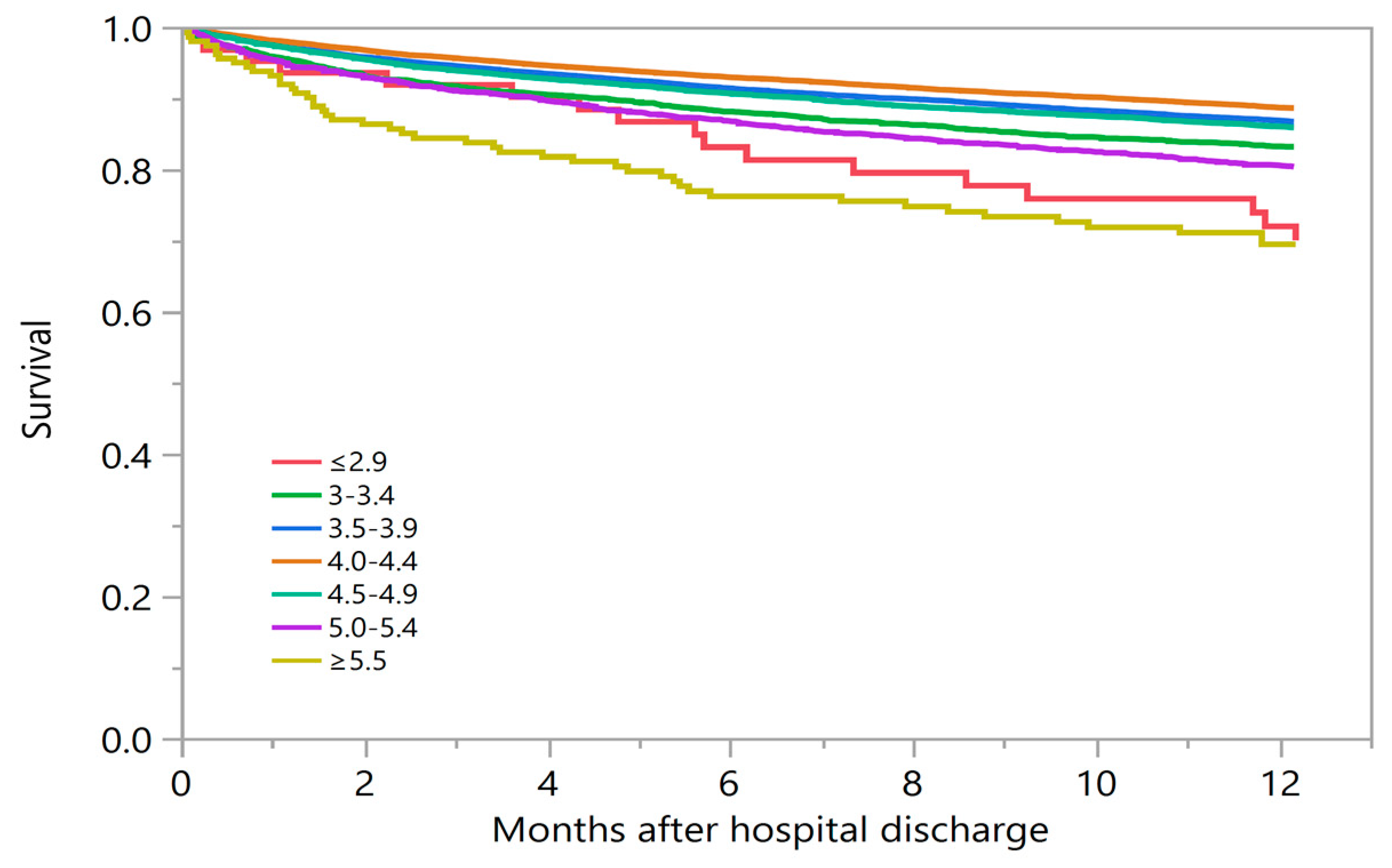
3.2. Discharge Serum Potassium and One-Year Mortality
3.3. Stratified Analysis Based on Admission Serum Potassium
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Thongprayoon, C.; Cheungpasitporn, W.; Chewcharat, A.; Mao, M.A.; Vallabhajosyula, S.; Bathini, T.; Thirunavukkarasu, S.; Kashani, K.B. Risk of respiratory failure among hospitalized patients with various admission serum potassium levels. Hosp. Pract. 2020, 2020, 1–5. [Google Scholar] [CrossRef]
- Palaka, E.; Grandy, S.; Darlington, O.; McEwan, P.; Van Doornewaard, A. Associations between serum potassium and adverse clinical outcomes: A systematic literature review. Int. J. Clin. Pract. 2019, 74. [Google Scholar] [CrossRef] [PubMed]
- Gumz, M.L.; Rabinowitz, L.; Wingo, C.S. An Integrated View of Potassium Homeostasis. N. Engl. J. Med. 2015, 373, 1787–1788. [Google Scholar] [CrossRef] [PubMed]
- Cheungpasitporn, W.; Thongprayoon, C.; Kittanamongkolchai, W.; Sakhuja, A.; Mao, M.A.; Erickson, S.B. Impact of admission serum potassium on mortality in patients with chronic kidney disease and cardiovascular disease. QJM Int. J. Med. 2017, 110, 713–719. [Google Scholar] [CrossRef] [PubMed]
- Thongprayoon, C.; Cheungpasitporn, W.; Hansrivijit, P.; Mao, M.A.; Medaura, J.; Bathini, T.; Chewcharat, A.; Erickson, S. Admission Serum Potassium Levels in Hospitalized Patients and One-Year Mortality. Medicines 2019, 7, 2. [Google Scholar] [CrossRef]
- Goyal, A.; Spertus, J.A.; Gosch, K.; Venkitachalam, L.; Jones, P.G.; Berghe, G.V.D.; Kosiborod, M. Serum Potassium Levels and Mortality in Acute Myocardial Infarction. JAMA 2012, 307, 157–164. [Google Scholar] [CrossRef]
- Hoppe, L.K.; Muhlack, D.C.; Koenig, W.; Carr, P.R.; Brenner, H.; Schöttker, B. Association of Abnormal Serum Potassium Levels with Arrhythmias and Cardiovascular Mortality: A Systematic Review and Meta-Analysis of Observational Studies. Cardiovasc. Drugs Ther. 2018, 32, 197–212. [Google Scholar] [CrossRef]
- Engelhardt, L.J.; Balzer, F.; Müller, M.C.; Grunow, J.J.; Spies, C.D.; Christopher, K.B.; Weber-Carstens, S.; Wollersheim, T. Association between potassium concentrations, variability and supplementation, and in-hospital mortality in ICU patients: A retrospective analysis. Ann. Intensiv. Care 2019, 9, 100–111. [Google Scholar] [CrossRef]
- Paltiel, O.; Salakhov, E.; Ronen, I.; Berg, D.; Israeli, A. Management of severe hypokalemia in hospitalized patients: A study of quality of care based on computerized databases. Arch. Intern. Med. 2001, 161, 1089–1095. [Google Scholar] [CrossRef][Green Version]
- Eliacik, E.; Yildirim, T.; Sahin, U.; Kizilarslanoglu, M.C.; Tapan, U.; Aybal-Kutlugun, A.; Hasçelik, G.; Arici, M. Potassium abnormalities in current clinical practice: Frequency, causes, severity and management. Med. Princ. Pract. 2015, 24, 271–275. [Google Scholar] [CrossRef]
- Xu, H.; Faxén, J.; Szummer, K.; Trevisan, M.; Kovesdy, C.P.; Jernberg, T.; Carrero, J.-J. Dyskalemias and adverse events associated with discharge potassium in acute myocardial infarction. Am. Heart J. 2018, 205, 53–62. [Google Scholar] [CrossRef] [PubMed]
- Charytan, D.; Goldfarb, D.S. Indications for hospitalization of patients with hyperkalemia. Arch. Intern. Med. 2000, 160, 1605–1611. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F.; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A New Equation to Estimate Glomerular Filtration Rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef] [PubMed]
- Section 2: AKI Definition. Kidney Int. Suppl. 2012, 2, 19–36. [CrossRef] [PubMed]
- Giebisch, G.; Wang, W. Potassium transport: From clearance to channels and pumps. Kidney Int. 1996, 49, 1624–1631. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Alderman, M.H. New Onset Diabetes During Antihypertensive Therapy. Am. J. Hypertens. 2008, 21, 493–499. [Google Scholar] [CrossRef]
- Pun, P.H.; Goldstein, B.A.; Gallis, J.A.; Middleton, J.P.; Svetkey, L.P. Serum Potassium Levels and Risk of Sudden Cardiac Death Among Patients with Chronic Kidney Disease and Significant Coronary Artery Disease. Kidney Int. Rep. 2017, 2, 1122–1131. [Google Scholar] [CrossRef]
- An, J.N.; Lee, J.P.; Jeon, H.J.; Kim, D.H.; Oh, Y.K.; Kim, Y.S.; Lim, C. Severe hyperkalemia requiring hospitalization: Predictors of mortality. Crit. Care 2012, 16, R225. [Google Scholar] [CrossRef]
- Evans, K.J.; Reddan, N.N.; Szczech, L.A. Review Articles: Nondialytic Management of Hyperkalemia and Pulmonary Edema Among End-Stage Renal Disease Patients: An Evaluation of the Evidence. Semin. Dial. 2004, 17, 22–29. [Google Scholar] [CrossRef]
- Colombo, M.; Kirchberger, I.; Amann, U.; Heier, M.; Thilo, C.; Kuch, B.; Peters, A.; Meisinger, C. Admission serum potassium concentration and long-term mortality in patients with acute myocardial infarction: Results from the MONICA/KORA myocardial infarction registry. BMC Cardiovasc. Disord. 2017, 17, 198. [Google Scholar] [CrossRef]
- Shiyovich, A.; Gilutz, H.; Plakht, Y. Serum potassium levels and long-term post-discharge mortality in acute myocardial infarction. Int. J. Cardiol. 2014, 172, e368–e370. [Google Scholar] [CrossRef] [PubMed]
- Ruanpeng, D.; Cheungpasitporn, W.; Thongprayoon, C.; Hennessey, J.V.; Shrestha, R.T. Systematic Review and Meta-analysis of the Impact of Noninvasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features (NIFTP) on Cytological Diagnosis and Thyroid Cancer Prevalence. Endocr. Pathol. 2019, 30, 189–200. [Google Scholar] [CrossRef] [PubMed]
- Aldahl, M.; Jensen, A.-S.C.; Davidsen, L.; Eriksen, M.A.; Hansen, S.M.; Nielsen, B.J.; Krogager, M.; Køber, L.; Torp-Pedersen, C.; Søgaard, P. Associations of serum potassium levels with mortality in chronic heart failure patients. Eur. Hear. J. 2017, 38, 2890–2896. [Google Scholar] [CrossRef] [PubMed]
- Weir, M.R.; Espaillat, R. Clinical perspectives on the rationale for potassium supplementation. Postgrad. Med. 2015, 127, 539–548. [Google Scholar] [CrossRef]
- Núñez, J.; Bayes-Genis, A.; Zannad, F.; Rossignol, P.; Núñez, E.; Bodí, V.; Miñana, G.; Santas, E.; Chorro, F.J.; Mollar, A.; et al. Long-Term Potassium Monitoring and Dynamics in Heart Failure and Risk of Mortality. Circulation 2018, 137, 1320–1330. [Google Scholar] [CrossRef]
- Gao, X.; Zheng, C.-F.; Liao, M.-Q.; He, H.; Liu, Y.; Jing, C.; Zeng, F.-F.; Chen, Q.-S. Admission serum sodium and potassium levels predict survival among critically ill patients with acute kidney injury: A cohort study. BMC Nephrol. 2019, 20, 311. [Google Scholar] [CrossRef]
- Chewcharat, A.; Thongprayoon, C.; Cheungpasitporn, W.; Mao, M.A.; Thirunavukkarasu, S.; Kashani, K.B. Trajectories of Serum Sodium on In-Hospital and 1-Year Survival among Hospitalized Patients. Clin. J. Am. Soc. Nephrol. 2020, 15, 600–607. [Google Scholar] [CrossRef]
| Variables | All | Discharge Serum Potassium Level (mEq/L) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| ≤2.9 | 3.0–3.4 | 3.5–3.9 | 4.0–4.4 | 4.5–4.9 | 5.0–5.4 | ≥5.5 | p | ||
| N | 57,874 | 71 | 2666 | 16,789 | 24,493 | 11,370 | 2307 | 178 | |
| Age (years) | 63 ± 17 | 62 ± 17 | 63 ± 17 | 62 ± 18 | 63 ± 17 | 64 ± 17 | 65 ± 16 | 64 ± 16 | < 0.001 |
| Male | 30,964 (54) | 24 (34) | 1113 (42) | 8153 (49) | 13,543 (55) | 6647 (17) | 1637 (59) | 117 (66) | < 0.001 |
| Caucasian | 53,971 (93) | 67 (94) | 2454 (92) | 15,549 (93) | 22,897 (94) | 10,663 (94) | 2181 (95) | 160 (90) | < 0.001 |
| eGFR at admission (mL/min/1.73m2) | 78 ± 26 | 82 ± 27 | 80 ± 28 | 81 ± 26 | 79 ± 26 | 74 ± 27 | 70 ± 28 | 62 ± 28 | < 0.001 |
| eGFR at discharge (mL/min/1.73m2) | 81.3 ± 26.3 | 87.6 ± 27.1 | 85.6 ± 27.1 | 85.4 ± 25.7 | 81.5 ± 25.8 | 76.1 ± 26.4 | 70.1 ± 27.4 | 63.6 ± 28.3 | < 0.001 |
Principal diagnosis
| 14,393 (25) 1547 (3) 5889 (10) 8685 (15) 1925 (3) 2548 (4) 9101 (16) 13,786 (24) | 9 (13) 8 (11) 14 (20) 11 (16) 5 (7) 1 (1) 7 (10) 16 (23) | 375 (14) 114 (4) 463 (17) 438 (16) 150 (6) 107 (4) 425 (16) 594 (22) | 3446 (21) 458 (3) 2177 (13) 2516 (15) 707 (4) 699 (4) 2772 (17) 4014 (24) | 6571 (27) 553 (2) 2228 (9) 3552 (15) 656 (3) 1011 (4) 3912 (16) 6010 (25) | 3278 (29) 325 (3) 808 (7) 1769 (16) 343 (3) 557 (5) 1649 (15) 2641 (23) | 675 (29) 79 (3) 181 (8) 369 (16) 63 (3) 154 (7) 314 (14) 472 (21) | 39 (22) 10 (6) 18 (10) 30 (17) 1 (1) 19 (11) 22 (12) 39 (22) | < 0.001 |
| Charlson score | 1.8 ± 2.4 | 2.3 ± 2.7 | 2.0 ± 2.6 | 1.8 ± 2.4 | 1.8 ± 2.3 | 1.9 ± 2.4 | 2.3 ± 2.6 | 2.9 ± 2.8 | < 0.001 |
Comorbidities
| 4565 (8) 4251 (7) 1836 (3) 4469 (8) 11,770 (20) 5334 (9) 1501 (3) | 2 (3) 1 (1) 0 (0) 5 (7) 13 (18) 2 (3) 3 (4) | 163 (6) 159 (6) 73 (3) 183 (7) 504 (19) 222 (8) 94 (4) | 1097 (7) 1117 (7) 431 (3) 1187 (7) 3116 (19) 1370 (8) 440 (3) | 1957 (8) 1768 (7) 772 (3) 1910 (8) 4830 (20) 2140 (9) 579 (2) | 1060 (9) 958 (8) 434 (4) 961 (9) 2614 (23) 1268 (11) 286 (3) | 267 (12) 231 (10) 113 (5) 203 (9) 636 (28) 299 (13) 90 (4) | 19 (11) 17 (10) 13 (7) 20 (11) 57 (32) 33 (19) 9 (5) | < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 |
| Acute kidney injury in hospital | 12,039 (21) | 14 (20) | 602 (23) | 3075 (18) | 4769 (20) | 2746 (24) | 751 (33) | 82 (46) | < 0.001 |
| Renal replacement therapy in hospital | 243 (0.4) | 0 (0) | 8 (0.3) | 58 (0.3) | 97 (0.4) | 57 (0.5) | 20 (0.9) | 3 (1.7) | 0.001 |
| Mechanical ventilation in hospital | 9178 (16) | 5 (7) | 393 (15) | 2625 (16) | 3934 (16) | 1796 (16) | 397 (17) | 28 (16) | 0.08 |
| Vasopressor use in hospital | 4949 (9) | 2 (3) | 190 (7) | 1353 (8) | 2154 (9) | 1005 (9) | 227 (10) | 18 (10) | 0.001 |
| Admission serum potassium (mEq/L) | 4.2 ± 0.6 | 3.7 ± 0.7 | 3.8 ± 0.5 | 4.0 ± 0.5 | 4.2 ± 0.5 | 4.4 ± 0.6 | 4.6 ± 0.6 | 4.8 ± 0.7 | < 0.001 |
| Serum Potassium Level (mEq/L) | One-Year Mortality (%) | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|---|
| HR (95% CI) | p | Adjusted HR # (95 % CI) | p | ||
| At admission | |||||
| ≤2.9 | 18.5% | 1.67 (1.38–2.03) | <0.001 | 1.58 (1.30–1.92) | <0.001 |
| 3.0–3.4 | 14.8% | 1.30 (1.17–1.45) | <0.001 | 1.20 (1.07–1.33) | 0.001 |
| 3.5–3.9 | 13.1% | 1.14 (1.07–1.22) | <0.001 | 1.14 (1.07–1.22) | <0.001 |
| 4.0–4.4 | 11.6% | 1 (ref) | - | 1 (ref) | - |
| 4.5–4.9 | 13.1% | 1.14 (1.07–1.22) | <0.001 | 1.04 (0.97–1.11) | 0.28 |
| 5.0–5.4 | 17.3% | 1.57 (1.42–1.72) | <0.001 | 1.19 (1.07–1.31) | 0.001 |
| ≥5.5 | 22.6% | 2.16 (1.90–2.47) | <0.001 | 1.43 (1.25–1.64) | <0.001 |
| At discharge | |||||
| ≤2.9 | 29.8% | 2.78 (1.73–4.48) | <0.001 | 2.36 (1.46–3.82) | <0.001 |
| 3.0–3.4 | 16.9% | 1.57 (1.41–1.75) | <0.001 | 1.39 (1.24–1.55) | <0.001 |
| 3.5–3.9 | 13.3% | 1.19 (1.12–1.26) | <0.001 | 1.15 (1.08–1.23) | <0.001 |
| 4.0–4.4 | 11.4% | 1 (ref) | - | 1 (ref) | - |
| 4.5–4.9 | 14.2% | 1.27 (1.19–1.36) | <0.001 | 1.18 (1.11–1.27) | <0.001 |
| 5.0–5.4 | 19.7% | 1.84 (1.65–2.06) | <0.001 | 1.50 (1.34–1.67) | <0.001 |
| ≥5.5 | 30.4% | 3.10 (2.31–4.15) | <0.001 | 2.22 (1.65–2.98) | <0.001 |
| Serum Potassium Level at Discharge (mEq/L) | One-Year Mortality (%) | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|---|
| HR (95% CI) | p | Adjusted HR# (95 % CI) | p | ||
| Admission serum potassium ≤ 3.9 mEq/L | |||||
| ≤3.9 | 14.6% | 1.29 (1.17–1.42) | <0.001 | 1.23 (1.11–1.36) | <0.001 |
| 4.0–4.4 | 11.7% | 1 (ref) | - | 1 (ref) | - |
| ≥4.5 | 15.4% | 1.35 (1.18–1.54) | <0.001 | 1.27 (1.11–1.45) | <0.001 |
| Admission serum potassium 4.0–4.9 mEq/L | |||||
| ≤3.9 | 13.1% | 1.23 (1.14–1.34) | <0.001 | 1.19 (1.10–1.29) | <0.001 |
| 4.0–4.4 | 10.8% | 1 (ref) | - | 1 (ref) | - |
| ≥4.5 | 13.5% | 1.28 (1.18–1.39) | <0.001 | 1.20 (1.11–1.31) | <0.001 |
| Admission serum potassium ≥ 5.0 mEq/L | |||||
| ≤3.9 | 16.6% | 1.05 (0.83–1.31) | 0.69 | 0.99 (0.79–1.25) | 0.94 |
| 4.0–4.4 | 15.6% | 1 (ref) | - | 1 (ref) | - |
| ≥4.5 | 21.8% | 1.46 (1.25–1.71) | <0.001 | 1.44 (1.23–1.69) | <0.001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thongprayoon, C.; Cheungpasitporn, W.; Thirunavukkarasu, S.; Petnak, T.; Chewcharat, A.; Bathini, T.; Vallabhajosyula, S.; Mao, M.A.; Erickson, S.B. Serum Potassium Levels at Hospital Discharge and One-Year Mortality among Hospitalized Patients. Medicina 2020, 56, 236. https://doi.org/10.3390/medicina56050236
Thongprayoon C, Cheungpasitporn W, Thirunavukkarasu S, Petnak T, Chewcharat A, Bathini T, Vallabhajosyula S, Mao MA, Erickson SB. Serum Potassium Levels at Hospital Discharge and One-Year Mortality among Hospitalized Patients. Medicina. 2020; 56(5):236. https://doi.org/10.3390/medicina56050236
Chicago/Turabian StyleThongprayoon, Charat, Wisit Cheungpasitporn, Sorkko Thirunavukkarasu, Tananchai Petnak, Api Chewcharat, Tarun Bathini, Saraschandra Vallabhajosyula, Michael A. Mao, and Stephen B. Erickson. 2020. "Serum Potassium Levels at Hospital Discharge and One-Year Mortality among Hospitalized Patients" Medicina 56, no. 5: 236. https://doi.org/10.3390/medicina56050236
APA StyleThongprayoon, C., Cheungpasitporn, W., Thirunavukkarasu, S., Petnak, T., Chewcharat, A., Bathini, T., Vallabhajosyula, S., Mao, M. A., & Erickson, S. B. (2020). Serum Potassium Levels at Hospital Discharge and One-Year Mortality among Hospitalized Patients. Medicina, 56(5), 236. https://doi.org/10.3390/medicina56050236







