The Diagnostic–Therapeutic Care Pathway in Psoriasis: Towards ISO 9001:2015 Certification
Abstract
1. Introduction
ISO 9001:2015
2. Materials and Methods
3. Results
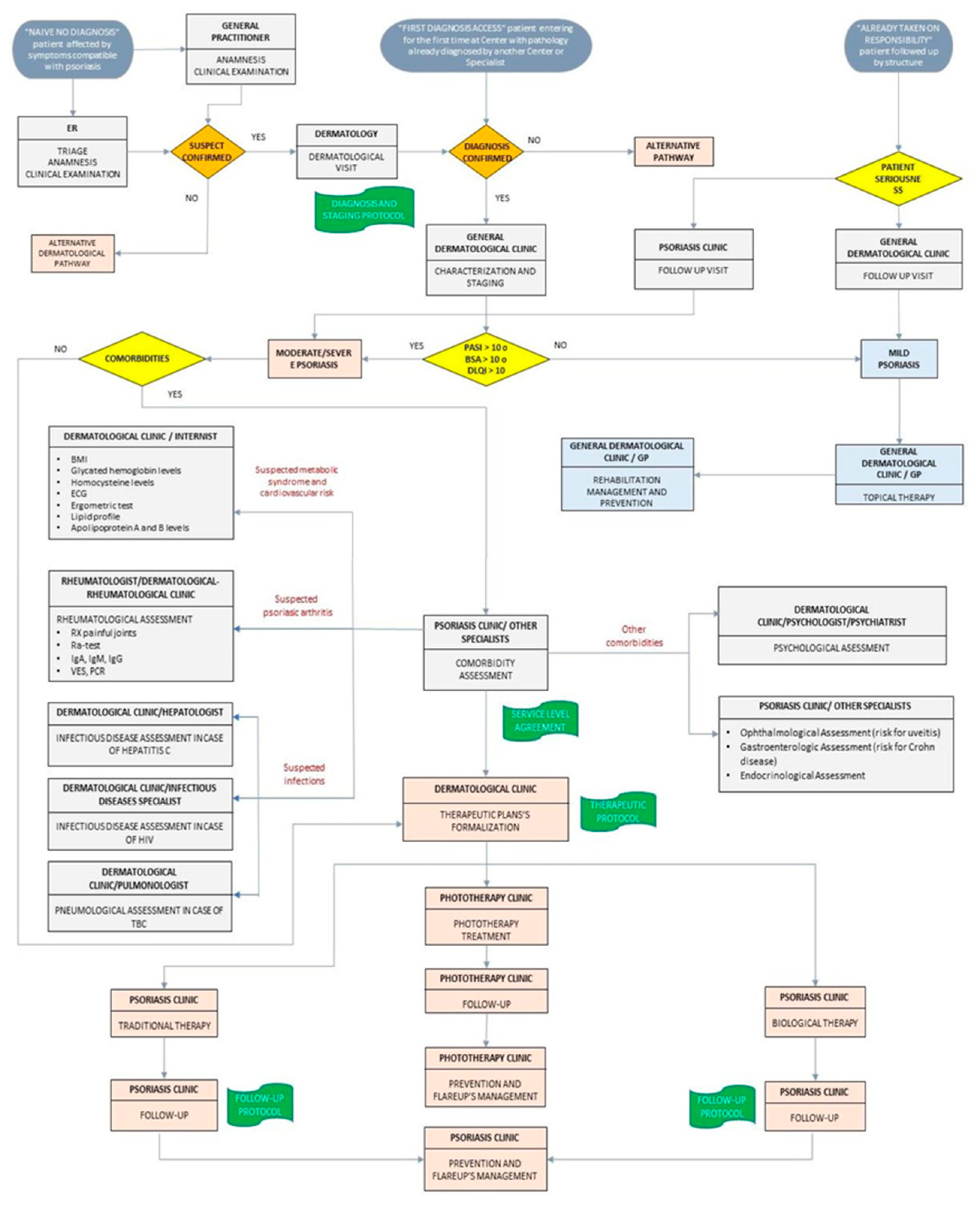
3.1. QMS and the ISO 9001:2015 Certification Process in Psoriasis Care
3.1.1. Analysis of Context
3.1.2. Target Identification
3.1.3. Key Performance Indicator (KPIs)
3.1.4. Service Provider’s Identification
3.1.5. Internal Audit
3.1.6. External Audit
3.1.7. Annual Revision
3.2. Real-Life Experience in QMS and ISO 9001:2015 Certification Process
- For about 10% of Pso patients, the waiting time between the first diagnosis and referral to the dermatologist was of several years. This clearly outlines a need for better patient education regarding the characteristics and the treatment possibilities of this pathology. Toward this end, we aim to draft information brochures on Pso and its comorbidity to be widely distributed to patients [9].
- In Italy, about 45% of Pso patients are referred to a specialist hospital by their general practitioner (GP) [9]. However, in our cohort, the majority of Pso patients (62.5%) were referred by other hospital specialists. Therefore, we intend to organize a working group with GPs to facilitate patient referral and early diagnosis.
- In our sample, the average Psoriasis Area Severity Index (PASI) at diagnosis was between 5 and 9, but in the literature this was between 5 and 7.4 [10]. We assume that this variance is due to the delay in referring patients.
- In our sample, psoriatic arthritis represents the most frequently observed comorbidity, followed by inflammatory bowel disease (IBD) and cardiovascular disorders according to the literature [11,12,13,14]. For this reason, we drew up a “Service Level Agreement”, a document in which we identified, for each comorbidity, the referring specialist, the reasons for the visit, and the elapsed time between referral and the visit. In the future, we plan to organize meetings or collegial visits for the management of more complex conditions.
- We switched therapies in about 31% of patients. This indicates our confidence in assessing the severity of the disease from the beginning and in administering the most suitable therapy for the patient, ensuring that our approach is based on the most recent guidelines.
- In our experience, all patients treated with biological medicines maintained the pre-established follow-up intervals of between 3 or 6 months. This demonstrates the patient’s awareness of the importance of the therapy and indicates a high level of satisfaction in our services. Further, this validates the efficiency of communication between specialists and patients.
- However, in our center the waiting time for the first visit was still long (about 100 days). We have planned strategies to reduce the waiting time, mainly through the acquisition of new resources.
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Reid, C.; Griffiths, C.E.M. Psoriasis and treatment: Past, Present and Future aspects. Acta Derm. Venereol. 2020, 100, 70–80. [Google Scholar] [CrossRef] [PubMed]
- Amin, M.; Lee, E.B.; Tsai, T.F.; Wu, J.J. Psoriasis and Co-morbidity. Acta Derm. Venereol. 2020, 100, 81–87. [Google Scholar] [CrossRef] [PubMed]
- AIFA. Trattamento Della Psoriasi con Farmaci Sistemici in Italia; Agenzia Italiana Del Farmaco: Rome, Italy, 2006. Available online: https://www.aifa.gov.it/sites/default/files/111.98170.11653961843060fd0.pdf (accessed on 5 March 2020).
- NICE. Psoriasis: Assessment and Management; The National Institute for Health and Clinical Excellence: London, UK, 2012; Available online: https://www.nice.org.uk/guidance/cg153/evidence/full-guideline-188351533 (accessed on 5 March 2020).
- Celano, A.; Onlus, P.A. Il percorso attuale per i pazienti affetti da PSO, AP, SA. Presented at Sotenibilità e L.E.A. «Il caso delle malattie autoimmuni non oncologiche”. Napoly, Italy. March 2017. Available online: https://www.sifoweb.it/images/pdf/eventi-ed-ecm/corsi-regionali/2017/8._Celano.pdf (accessed on 5 March 2020).
- Gisondi, P.; Altomare, G.; Ayala, F.; Bardazzi, F.; Bianchi, L.; Chiricozzi, A.; Costanzo, A.; Conti, A.; Dapavo, P.; De Simone, C.; et al. Italian guidelines on the systemic treatments of moderate-to-severe plaque psoriasis. J. Eur. Acad. Dermatol. Venereol. 2017, 31, 774–790. [Google Scholar] [CrossRef] [PubMed]
- Betlloch-Mas, I.; Ramon-Sapena, R.; Abellan-Garcia, C.; Pascual-Ramirez, J.C. Implementation and Operation of an Integrated Quality Management System in Accordance with ISO 9001:2015 in a Dermatology Department. Actas. Dermosifiliogr. 2019, 110, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Taylor, M.J.; McNicholas, C.; Nicolay, C.; Darzi, A.; Bell, D.; Reed, J.E. Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual. Saf. 2014, 23, 290–298. [Google Scholar] [CrossRef] [PubMed]
- Naldi, L.; Pini, P.; Girolomoni, G. Gestione Clinica Della Psoriasi; Pacini Editore Srl: Pisa, Italy, 2016; Available online: www.pacinimedicina.it/wp-content/uploads/Layout_4B_Girolomoni.pdf (accessed on 5 March 2020).
- Hagg, D.; Sundstrom, A.; Eriksson, M.; Schmitt-Egenolf, M. Severity of Psoriasis Differs Between Men and Women: A Study of the Clinical Outcome Measure Psoriasis Area and Severity Index (PASI) in 5438 Swedish Register Patients. Am. J. Clin. Dermatol 2017, 18, 583–590. [Google Scholar] [CrossRef] [PubMed]
- Gladman, D.D.; Antoni, C.; Mease, P.; Clegg, D.O.; Nash, P. Psoriatic arthritis: Epidemiology, clinical features, course, and outcome. Ann. Rheum. Dis. 2005, 64, 14–17. [Google Scholar] [CrossRef] [PubMed]
- Soltani-Arabshahi, R.; Wong, B.; Feng, B.J.; Goldgar, D.E.; Duffin, K.C.; Krueger, G.G. Obesity in early adulthood as a risk factor for psoriatic arthritis. Arch. Dermatol. 2010, 146, 721–726. [Google Scholar] [CrossRef] [PubMed]
- Kolliker Frers, R.A.; Cosentino, V.; Tau, J.; Kerzberg, E.M.; Urdapilleta, A.; Chiocconi, M.; Krogan, E.; Otero-Losada, M.; Capani, F. Immune-Mediated Inflammation Promotes Subclinical Atherosclerosis in Recent-Onset Psoriatic Arthritis Patients without Conventional Cardiovascular Risk Factors. IJC Metab. Endocr. 2018, 9, 139. [Google Scholar]
- Vlachos, C.; Gaitanis, G.; Katsanos, K.H.; Christodoulou, D.K.; Tsianos, E.; Bassukas, I.D. Psoriasis and inflammatory bowel disease: Links and risks. Psoriasis (Auckl) 2016, 6, 73–92. [Google Scholar] [PubMed]



|
|
|
| Targets | Indicators | Actions/Commitments | Responsible Party |
|---|---|---|---|
| Reduction of the waiting time from referral to first visit through an improvement of appropriateness in access to the psoriasis center | Time difference between referral and the first visit | Create a document for general practitioners and territorial specialists which serves as guideline for correct identification of psoriasis patients for the center | Working group |
| Improved treatment adherence | Proportion of patients lost to follow-up | Raise awareness of the importance of treatment adherence. Create a survey to evaluate patients’ comprehension. | Working group |
| Implementation of a dedicated nurse | Obtained dedicated nursing staff | Communicate to the medical director the need for dedicated nursing staff. | Medical director and hospital medical management |
| Increased resources for medical students and residents | Number of participants at national and international courses Number of publications | Involve students and residents in clinical and basic research activities. | Working group |
| Increased participation in clinical trials | Number of clinical trials | Identify barriers to clinical trial participation to enable interventions that could help to increase participation. | Working group |
| Structural Indicators (Activity, Diagnosis and Appropriateness) | Outcome Indicators | Process Indicators |
|---|---|---|
|
|
|
| Action | Times | Responsible Party |
|---|---|---|
| Attracting the interest of staff regarding report policy disclosure in accordance with company policy | July 2019 | Medical director |
| Attracting interest of staff regarding ministerial recommendations through periodic meetings | December 2019 | Medical director |
| Sharing, with all the staff, performance indicators of the psoriasis center | December 2019 | Medical director and working group |
| Sharing, with colleagues inside the hospital and with those in the district, the certification obtained by the center | December 2019 | Medical director and working group |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Veronese, F.; Graziola, F.; Cammarata, E.; Andreassi, M.; Mazzoletti, V.; Taglietti, C.; Navarra, G.; Savoia, P.; Tiberio, R. The Diagnostic–Therapeutic Care Pathway in Psoriasis: Towards ISO 9001:2015 Certification. Medicina 2020, 56, 253. https://doi.org/10.3390/medicina56050253
Veronese F, Graziola F, Cammarata E, Andreassi M, Mazzoletti V, Taglietti C, Navarra G, Savoia P, Tiberio R. The Diagnostic–Therapeutic Care Pathway in Psoriasis: Towards ISO 9001:2015 Certification. Medicina. 2020; 56(5):253. https://doi.org/10.3390/medicina56050253
Chicago/Turabian StyleVeronese, Federica, Francesca Graziola, Edoardo Cammarata, Marco Andreassi, Vanessa Mazzoletti, Camilla Taglietti, Gaia Navarra, Paola Savoia, and Rossana Tiberio. 2020. "The Diagnostic–Therapeutic Care Pathway in Psoriasis: Towards ISO 9001:2015 Certification" Medicina 56, no. 5: 253. https://doi.org/10.3390/medicina56050253
APA StyleVeronese, F., Graziola, F., Cammarata, E., Andreassi, M., Mazzoletti, V., Taglietti, C., Navarra, G., Savoia, P., & Tiberio, R. (2020). The Diagnostic–Therapeutic Care Pathway in Psoriasis: Towards ISO 9001:2015 Certification. Medicina, 56(5), 253. https://doi.org/10.3390/medicina56050253







