Effectiveness of a Real-Time Ventilation Feedback Device for Guiding Adequate Minute Ventilation: A Manikin Simulation Study
Abstract
1. Introduction
2. Methods
2.1. A Real-Time Ventilation Feedback Device
2.2. Device Validation
2.3. Study Design
2.4. Participants
2.5. Study Protocol
2.6. Outcomes
2.7. Statistics
3. Results
3.1. Real-Time Ventilation Feedback Device Validation
3.2. Baseline Characteristics
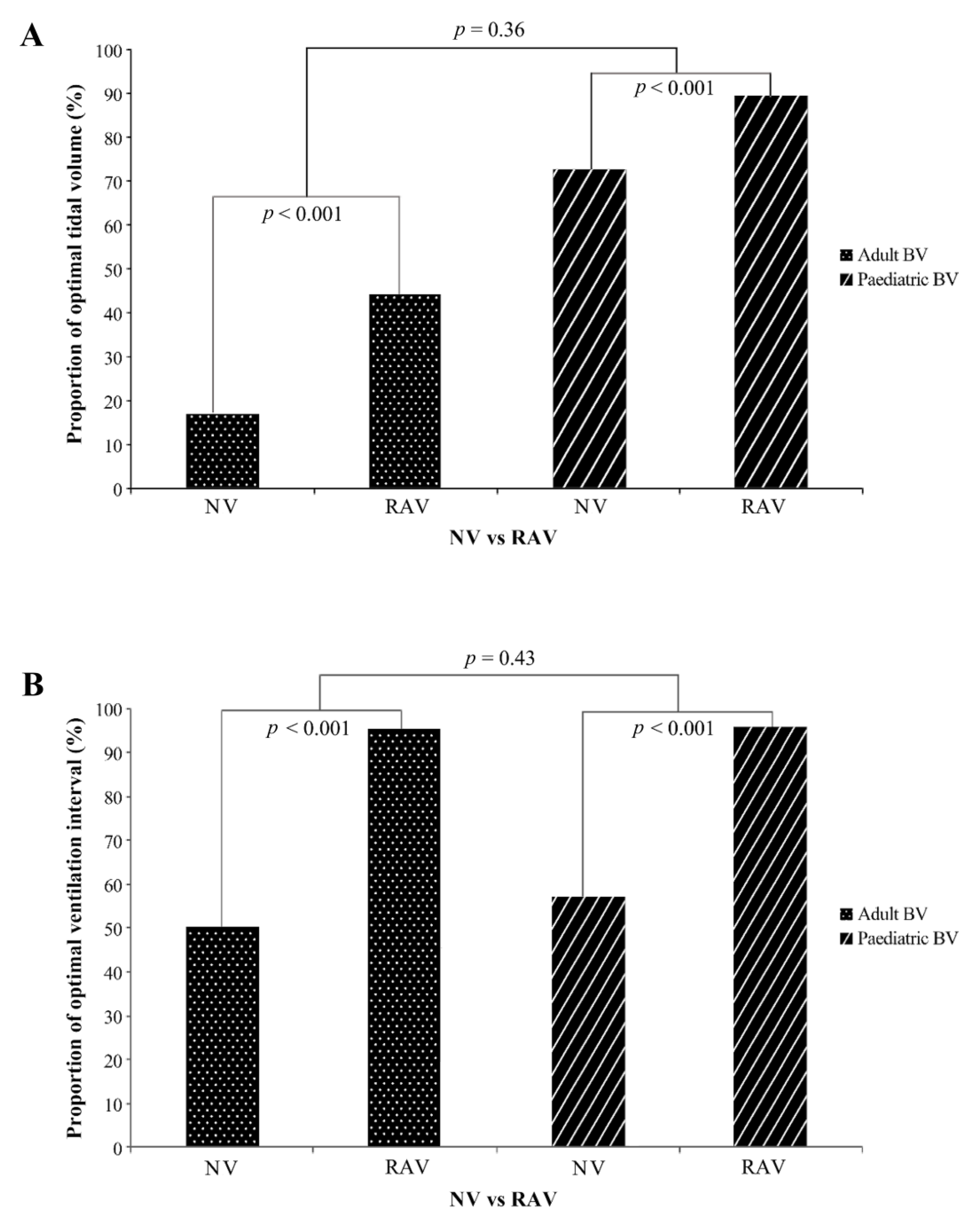
3.3. Results for the Tidal Volume and Ventilation Interval Performance
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Abella, B.S.; Alvarado, J.P.; Myklebust, H.; Edelson, D.P.; Barry, A.; O’Hearn, N.; Hoek, T.L.V.; Becker, L.B. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA 2005, 293, 305–310. [Google Scholar] [CrossRef]
- Eisenberg, M.S.; Mengert, T.J. Cardiac resuscitation. N. Engl. J. Med. 2001, 344, 1304–1313. [Google Scholar] [CrossRef] [PubMed]
- Rea, T.D.; Crouthamel, M.; Eisenberg, M.S.; Becker, L.; Lima, A.R. Temporal patterns in long-term survival after resuscitation from out-of-hospital cardiac arrest. Circulation 2003, 108, 1196–1201. [Google Scholar] [CrossRef] [PubMed]
- Daya, M.; Schmicker, R.H.; Zive, D.M.; Rea, T.D.; Nichol, G.; Buick, J.E.; Brooks, S.; Christenson, J.; Macphee, R.; Craig, A.; et al. Out-of-hospital cardiac arrest survival improving over time: Results from the resuscitation outcomes consortium (ROC). Resuscitation 2015, 91, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Feneley, M.P.; Maier, G.W.; Kern, K.B.; Gaynor, J.W.; Gall, S.A.; Sanders, A.B.; Raessler, K.; Muhlbaier, L.H.; Rankin, J.S.; Ewy, G.A. Influence of compression rate on initial success of resuscitation and 24 hour survival after prolonged manual cardiopulmonary resuscitation in dogs. Circulation 1988, 77, 240–250. [Google Scholar] [CrossRef]
- Meaney, P.A.; Bobrow, B.J.; Mancini, M.E.; Christenson, J.; de Caen, A.R.; Bhanji, F.; Abella, B.S.; Kleinman, M.E.; Edelson, D.P.; Berg, R.A.; et al. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: A consensus statement from the American Heart Association. Circulation 2013, 128, 417–435. [Google Scholar] [CrossRef]
- Kleinman, M.E.; Brennan, E.E.; Goldberger, Z.D.; Swor, R.A.; Terry, M.; Bobrow, B.J.; Gazmuri, R.J.; Travers, A.H.; Rea, T. Part 5: Adult basic life support and cardiopulmonary resuscitation quality: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015, 132, S414–S435. [Google Scholar] [CrossRef]
- Link, M.S.; Berkow, L.C.; Kudenchuk, P.J.; Halperin, H.R.; Hess, E.P.; Moitra, V.K.; Neumar, R.W.; O’Neil, B.J.; Paxton, J.H.; Silvers, S.M.; et al. Part 7: Adult advanced cardiovascular life support: 2015 american heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015, 132, S444–S464. [Google Scholar] [CrossRef]
- Perkins, G.D.; Olasveengen, T.M.; Maconochie, I.; Soar, J.; Wyllie, J.; Lockey, R.G.A.; Semeraro, F.; Lott, C.; Monsieurs, K.; Nolan, J.; et al. European resuscitation council guidelines for resuscitation: 2017 update. Resuscitation 2018, 123, 43–50. [Google Scholar] [CrossRef]
- Neumar, R.W.; Shuster, M.; Callaway, C.W.; Gent, L.M.; Atkins, D.L.; Bhanji, F.; Brooks, S.C.; de Caen, A.R.; Donnino, M.W.; Ferrer, J.M.; et al. Part 1: Executive summary: 2015 american heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015, 132, S315–S367. [Google Scholar] [CrossRef]
- Muizelaar, J.P.; Marmarou, A.; Ward, J.D.; Kontos, H.A.; Choi, S.C.; Becker, D.P.; Gruemer, H.; Young, H.F. Adverse effects of prolonged hyperventilation in patients with severe head injury: A randomized clinical trial. J. Neurosurg. 1991, 75, 731–739. [Google Scholar] [CrossRef] [PubMed]
- Sigurdsson, G.; Yannopoulos, D.; McKnite, S.H.; Lurie, K.G. Cardiorespiratory interactions and blood flow generation during cardiac arrest and other states of low blood flow. Curr. Opin. Crit. Care 2003, 9, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Aufderheide, T.P.; Sigurdsson, G.; Pirrallo, R.G.; Yannopoulos, D.; McKnite, S.; Von Briesen, C.; Sparks, C.W.; Conrad, C.J.; Provo, T.A.; Lurie, K.G.; et al. Hyperventilation-Induced Hypotension During Cardiopulmonary Resuscitation. Circulation 2004, 109, 1960–1965. [Google Scholar] [CrossRef]
- Aufderheide, T.P.; Lurie, K.G. Death by hyperventilation: A common and life-threatening problem during cardiopulmonary resuscitation. Crit. Care Med. 2004, 32, S345–S351. [Google Scholar] [CrossRef]
- Kleinman, M.E.; Goldberger, Z.D.; Rea, T.; Swor, R.A.; Bobrow, B.J.; Brennan, E.E.; Terry, M.; Hemphill, R.; Gazmuri, R.J.; Hazinski, M.F.; et al. 2017 american heart association focused update on adult basic life support and cardiopulmonary resuscitation quality: An update to the american heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2018, 137, e7–e13. [Google Scholar] [CrossRef]
- Augustine, J.A.; Seidel, D.R.; McCabe, J.B. Ventilation performance using a self-inflating anesthesia bag: Effect of operator characteristics. Am. J. Emerg. Med. 1987, 5, 267–270. [Google Scholar] [CrossRef]
- Carden, E.; Hughes, T. An evaluation of manually operated self-inflating resuscitation bags. Anesth. Analg. 1975, 54, 133–138. [Google Scholar] [CrossRef]
- Koga, T.; Kawamoto, M. Gender difference in mask ventilation training of anesthesia residents. J. Clin. Anesthesia 2009, 21, 178–182. [Google Scholar] [CrossRef] [PubMed]
- McInnes, A.D.; Sutton, R.; Orioles, A.; Nishisaki, A.; Niles, D.; Abella, B.; Maltese, M.R.; Berg, R.A.; Nadkarni, V. The first quantitative report of ventilation rate during in-hospital resuscitation of older children and adolescents. Resuscitation 2011, 82, 1025–1029. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, J.F.; Deakin, C.D. Do we hyperventilate cardiac arrest patients? Resuscitation 2007, 73, 82–85. [Google Scholar] [CrossRef]
- Kern, K.B.; Stickney, R.E.; Gallison, L.; Smith, R.E. Metronome improves compression and ventilation rates during CPR on a manikin in a randomized trial. Resuscitation 2010, 81, 206–210. [Google Scholar] [CrossRef] [PubMed]
- Wenzel, V.; Keller, C.; Idris, A.H.; Dörges, V.; Lindner, K.H.; Brimacombe, J.R. Effects of smaller tidal volumes during basic life support ventilation in patients with respiratory arrest: Good ventilation, less risk? Resuscitation 1999, 43, 25–29. [Google Scholar] [CrossRef]
- Kroll, M.; Das, J.; Siegler, J. Can altering grip technique and bag size optimize volume delivered with bag-valve-mask by emergency medical service providers? Prehosp. Emerg. Care 2019, 23, 210–214. [Google Scholar] [CrossRef]
- Pirrallo, R.G.; Aufderheide, T.P.; Provo, T.A.; Lurie, K.G. Effect of an inspiratory impedance threshold device on hemodynamics during conventional manual cardiopulmonary resuscitation. Resuscitation 2005, 66, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Thayne, R.C.; Thomas, D.C.; Neville, J.D.; Van Dellen, A. Use of an impedance threshold device improves short-term outcomes following out-of-hospital cardiac arrest. Resuscitation 2005, 67, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Park, S.O. A simulation study for evaluating the efficacy of live-feedback device (Amflow) for delivering correct ventilations during cardiopulmonary resuscitation. J. Korean Soc. Emerg. Med. 2017, 28, 159–166. [Google Scholar]
- You, K.M.; Lee, C.; Kwon, W.Y.; Lee, J.C.; Suh, G.J.; Kim, K.S.; Park, M.J.; Kim, S. Real-time tidal volume feedback guides optimal ventilation during simulated CPR. Am. J. Emerg. Med. 2016, 35, 292–298. [Google Scholar] [CrossRef]
- Ambu® Mark IV-Reusable resuscitator datasheet. Available online: https://www.ambu.com/products/anaesthesia/resuscitators/product/ambu-mark-iv.;2019 (accessed on 10 January 2020).
- Elling, R.; Politis, J. An evaluation of emergency medical technicians’ ability to use manual ventilation devices. Ann. Emerg. Med. 1983, 12, 765–768. [Google Scholar] [CrossRef]
- Lee, M.J.; Rho, T.-H.; Kim, H.; Kang, G.H.; Kim, J.S.; Rho, S.G.; Park, H.K.; Oh, D.J.; Oh, S.; Wi, J.; et al. Part 3. Advanced cardiac life support: 2015 Korean Guidelines for Cardiopulmonary Resuscitation. Clin. Exp. Emerg. Med. 2016, 3, S17–S26. [Google Scholar] [CrossRef]
- Khoury, A.; De Luca, A.; Sall, F.; Pazart, L.; Capellier, G. Performance of manual ventilation: How to define its efficiency in bench studies? A review of the literature. Anaesthesia 2015, 70, 985–992. [Google Scholar] [CrossRef]
- Terndrup, T.; Rhee, J. Available ventilation monitoring methods during pre-hospital cardiopulmonary resuscitation. Resuscitation 2006, 71, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Siegler, J.; Kroll, M.; Wojcik, S.; Moy, H.P. Can EMS providers provide appropriate tidal volumes in a simulated adult-sized patient with a pediatric-sized bag-valve-mask? Prehosp. Emerg. Care 2017, 21, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Doerges, V.; Sauer, C.; Ocker, H.; Wenzel, V.; Schmucker, P. Smaller tidal volumes during cardiopulmonary resuscitation: Comparison of adult and paediatric self-inflatable bags with three different ventilatory devices. Resuscitation 1999, 43, 31–37. [Google Scholar] [CrossRef]


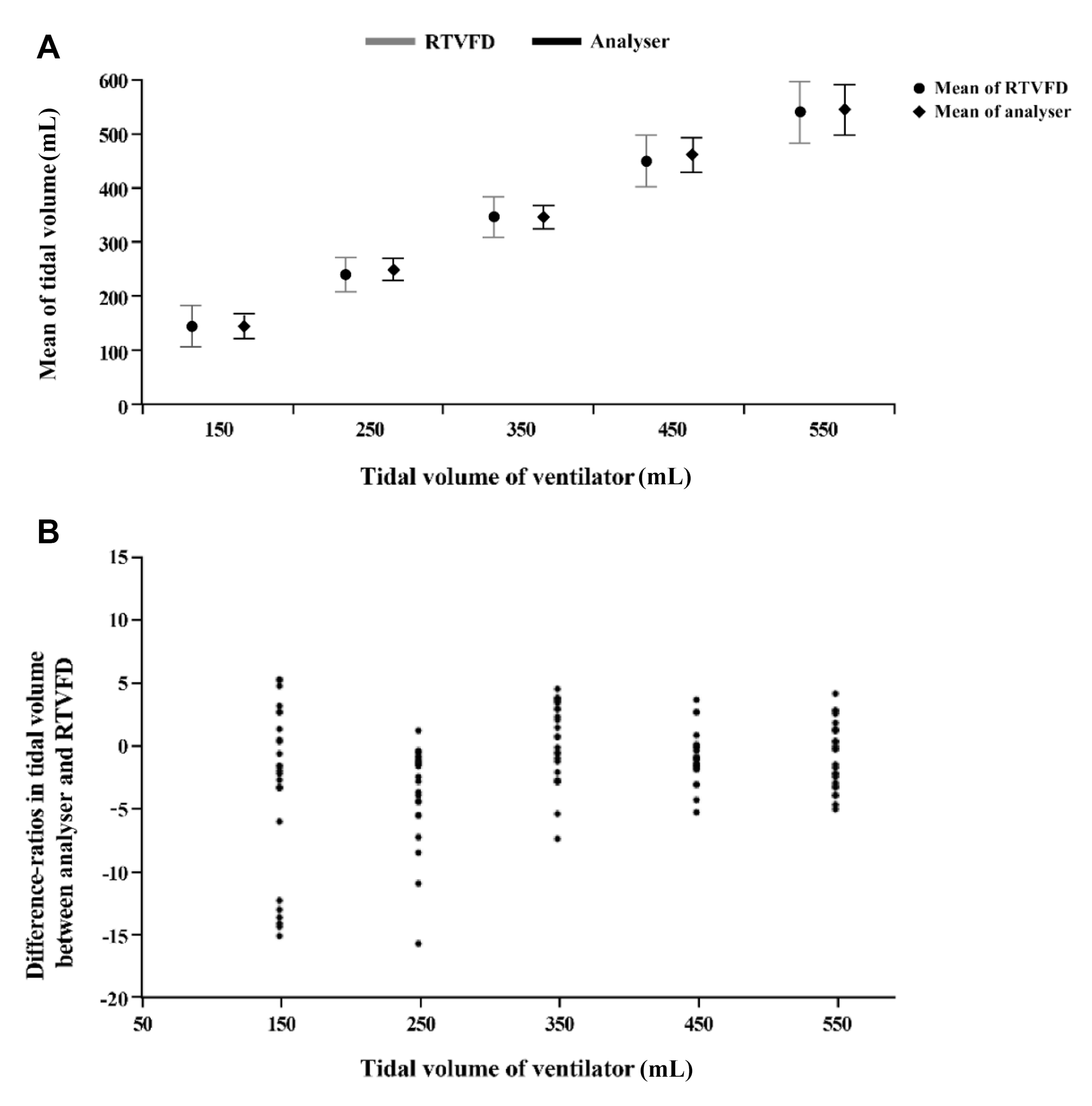
| Set Volume of Mechanical Ventilation, mL | Analyser | RTVFD | p-Value |
|---|---|---|---|
| 150 | 149.4 ± 1.0 | 144 ± 9.8 | 0.008 |
| 250 | 253.9 ± 0.3 | 244.3 ± 9.7 | <0.001 |
| 350 | 348.2 ± 0.6 | 348.0 ± 10.9 | 0.903 |
| 450 | 455.8 ± 1.3 | 450.1 ± 9.1 | 0.005 |
| 550 | 551.2 ± 2.2 | 545.2 ± 13.7 | 0.040 |
| RAV First Group (n = 13) | NV First Group (n = 13) | p-Value | |
|---|---|---|---|
| Age, median (IQR) | 30 (27–33) | 28 (26–30) | 0.079 |
| Female, N (%) | 9 (69.2%) | 8 (61.5%) | 1.000 |
| Times CPR performed | |||
| Number within 1 week | 0.85 (0.80) | 1.15 (1.46) | 0.512 |
| Number within 1 month | 2.15 (2.27) | 5.31 (7.04) | 0.137 |
| Job, N (%) | 0.665 | ||
| Nurse | 10 (76.9) | 9 (69.2) | |
| EMT | 2 (15.4) | 2 (15.4) | |
| Doctor | 1 (7.7) | 2 (15.4) | |
| Adult BV | p-Value | Paediatric BV | p-Value | |||
|---|---|---|---|---|---|---|
| RAV | NV | RAV | NV | |||
| Tidal volume | <0.001 | <0.001 | ||||
| Tidal volume, mL, mean±SD | 432.0 ± 63.93 | 392.83 ± 136.36 | 144.84 ± 23.07 | 131.74 ± 38.78 | ||
| Optimal tidal volume | <0.001 | <0.001 | ||||
| Optimal ventilation, N (%) | 262 (47.29) | 98 (18.46) | 495 (89.51) | 380 (72.66) | ||
| Hypoventilation, N (%) | 220 (39.71) | 309 (58.19) | 53 (9.58) | 131 (25.05) | ||
| Hyperventilation, N (%) | 72 (13.00) | 124 (23.35) | 5 (0.90) | 12 (2,29) | ||
| Ventilation interval | <0.001 | <0.001 | ||||
| Ventilation interval, sec | 6.84 ± 1.13 | 6.37 ± 3.17 | 6.57 ± 0.99 | 6.29± 2.23 | ||
| Optimal interval | <0.001 | <0.001 | ||||
| Optimal interval, N (%) | 505 (95.64) | 254 (50.20) | 506 (95.83) | 284 (57.14) | ||
| Odds Ratio | 95% CI | p-Value | ||
|---|---|---|---|---|
| Achievement of adequate TV | ||||
| RTVFD assistance (yes vs. no) | 3.90 | 2.95 | 5.15 | <0.001 |
| BV type (paediatric vs. adult BV) | 13.26 | 9.96 | 17.65 | <0.001 |
| RTVFD assistance (in adult BV subgroup) | 3.90 | 2.95 | 5.15 | <0.001 |
| RTVFD assistance (in paediatric BV subgroup) | 3.21 | 2.30 | 4.48 | <0.001 |
| Interaction (RTVFD assistance & BV type) | 0.82 | 0.54 | 1.25 | 0.364 |
| Achievement of adequate VI | ||||
| RTVFD assistance (yes vs. no) | 21.78 | 13.71 | 34.61 | <0.001 |
| BV type (paediatric vs. adult BV) | 1.32 | 1.08 | 1.62 | 0.007 |
| RTVFD assistance (in adult BV subgroup) | 21.78 | 13.71 | 34.61 | <0.001 |
| RTVFD assistance (in paediatric BV subgroup) | 17.25 | 10.80 | 27.56 | <0.001 |
| Interaction (RTVFD assistance & BV type) | 0.79 | 0.44 | 1.41 | 0.430 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heo, S.; Yoon, S.Y.; Kim, J.; Kim, H.S.; Kim, K.; Yoon, H.; Hwang, S.Y.; Cha, W.C.; Kim, T. Effectiveness of a Real-Time Ventilation Feedback Device for Guiding Adequate Minute Ventilation: A Manikin Simulation Study. Medicina 2020, 56, 278. https://doi.org/10.3390/medicina56060278
Heo S, Yoon SY, Kim J, Kim HS, Kim K, Yoon H, Hwang SY, Cha WC, Kim T. Effectiveness of a Real-Time Ventilation Feedback Device for Guiding Adequate Minute Ventilation: A Manikin Simulation Study. Medicina. 2020; 56(6):278. https://doi.org/10.3390/medicina56060278
Chicago/Turabian StyleHeo, Sejin, Sun Young Yoon, Jongchul Kim, Hye Seung Kim, Kyunga Kim, Hee Yoon, Sung Yeon Hwang, Won Chul Cha, and Taerim Kim. 2020. "Effectiveness of a Real-Time Ventilation Feedback Device for Guiding Adequate Minute Ventilation: A Manikin Simulation Study" Medicina 56, no. 6: 278. https://doi.org/10.3390/medicina56060278
APA StyleHeo, S., Yoon, S. Y., Kim, J., Kim, H. S., Kim, K., Yoon, H., Hwang, S. Y., Cha, W. C., & Kim, T. (2020). Effectiveness of a Real-Time Ventilation Feedback Device for Guiding Adequate Minute Ventilation: A Manikin Simulation Study. Medicina, 56(6), 278. https://doi.org/10.3390/medicina56060278





