A Hospital Protocol for Decision Making in Emergency Admission for Acute Diverticulitis: Initial Results from Small Cohort Series
Abstract
:1. Introduction
2. Materials and Methods
- -
- Personal data (name, age, sex);
- -
- Diagnosis at admission (all cases of AD);
- -
- Degree of AD according to the World Society of Emergency Surgery (WSES) classification;
- -
- Risk classes;
- -
- Time of preoperative hospitalization;
- -
- Time of postoperative hospitalization;
- -
- Therapeutic strategy;
- -
- Type of surgery;
- -
- Outcome of non-operative treatment (NonOP);
- -
- Outcome of the hospitalization.
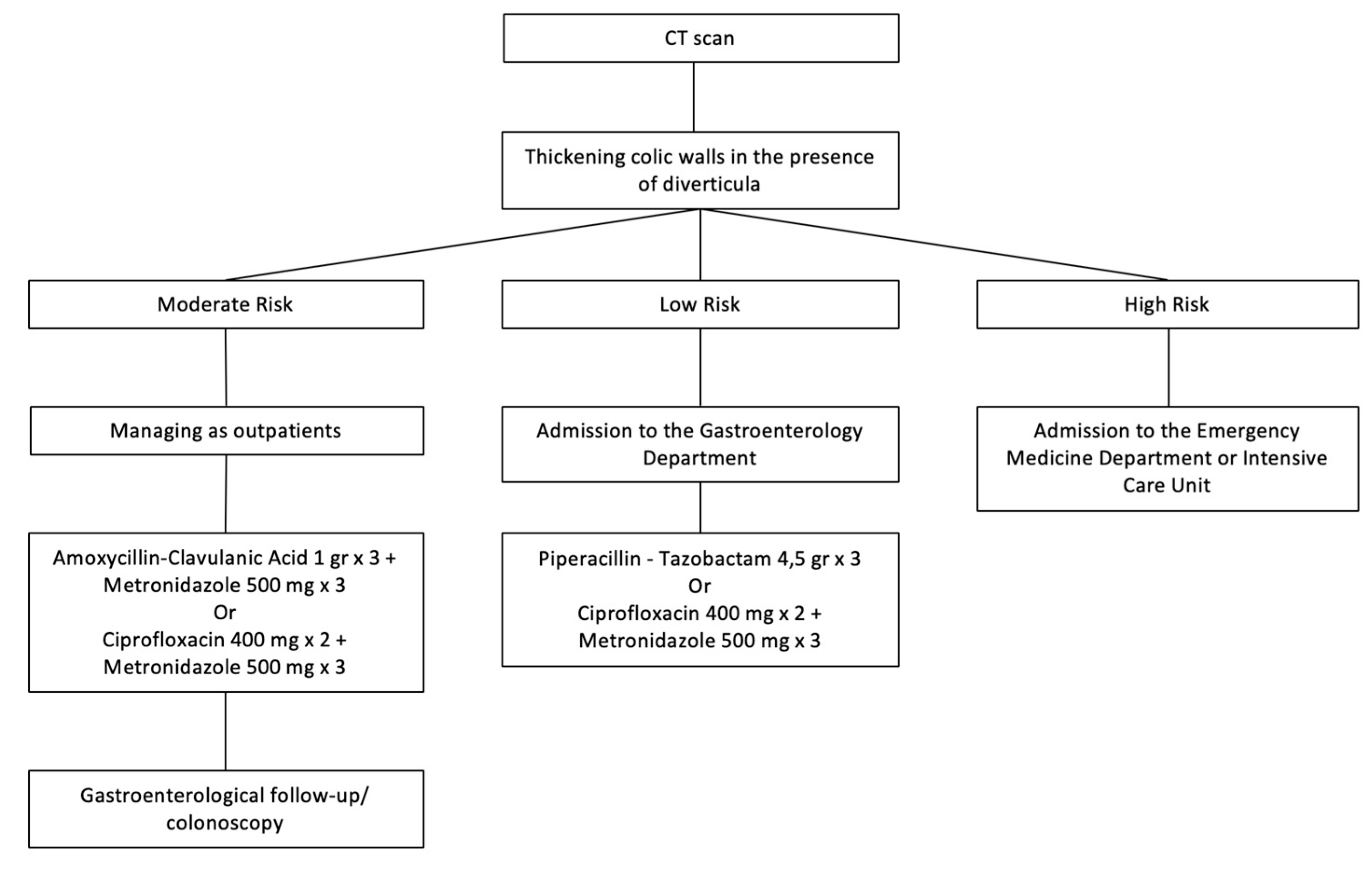
2.1. Acute Uncomplicated Diverticulitis
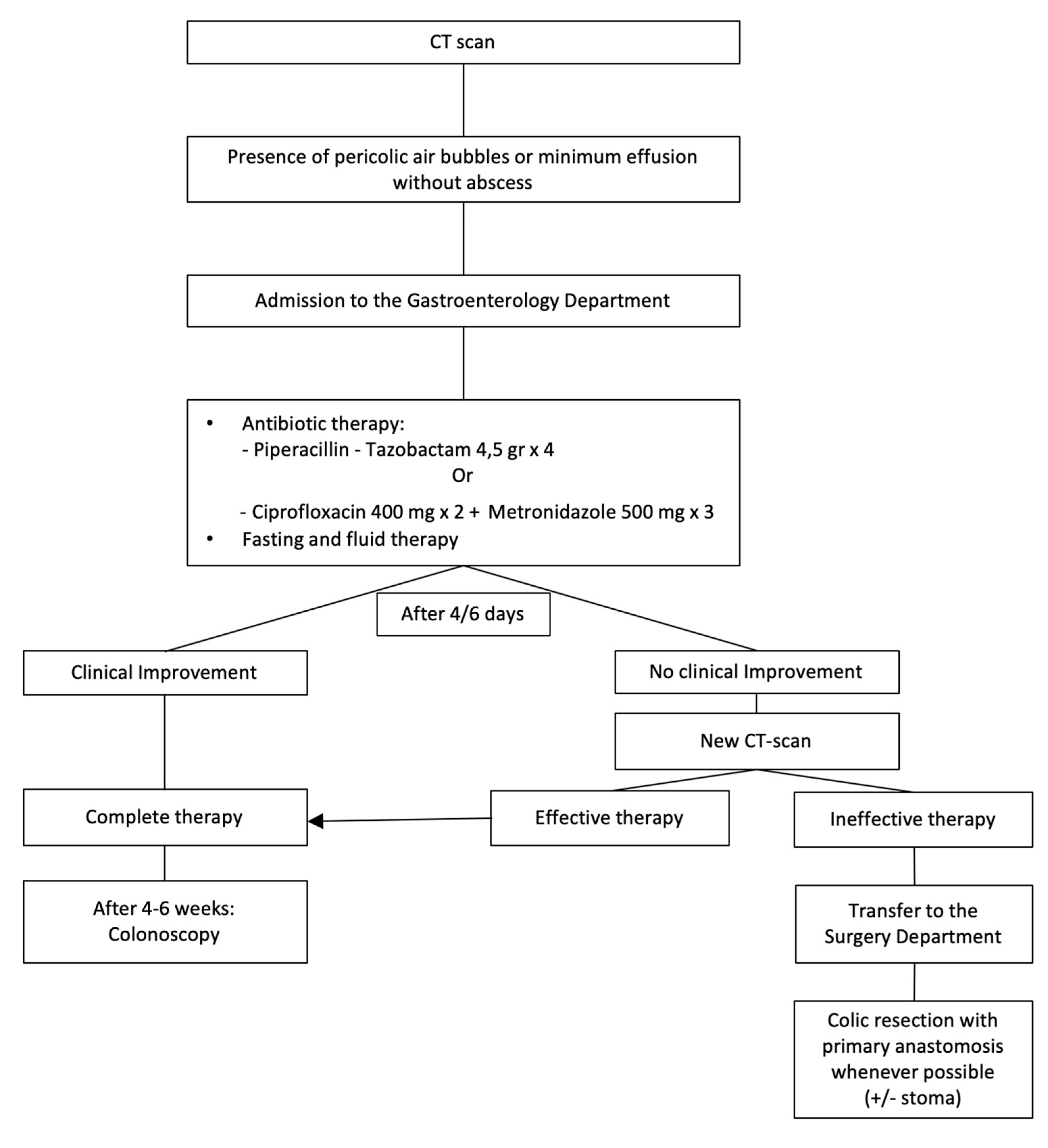
2.2. Acute Complicated Diverticulitis Grade 1A
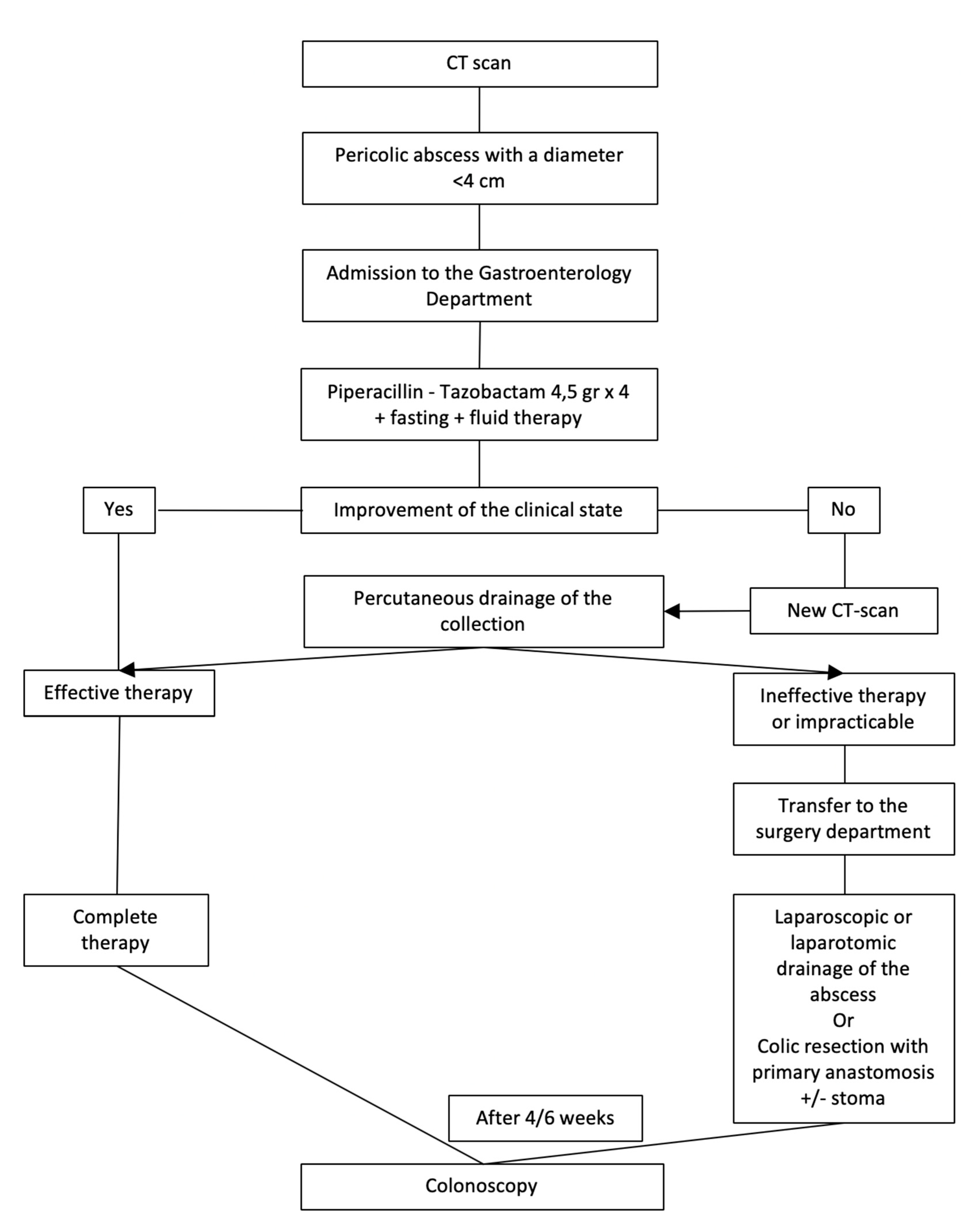
2.3. Acute Complicated Diverticulitis Grade 1B
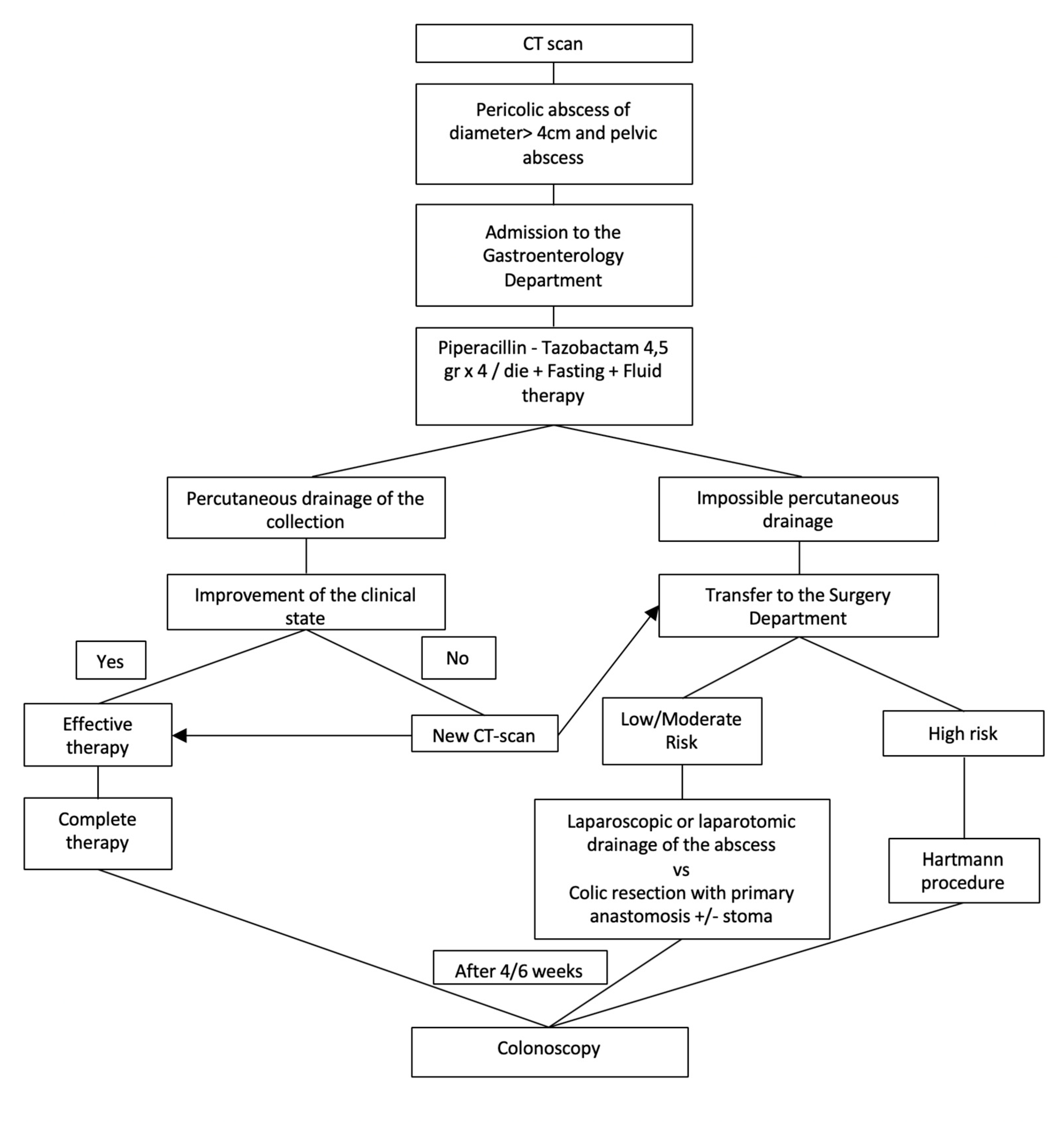
2.4. Acute Complicated Diverticulitis Grade 2A
2.5. Acute Complicated Diverticulitis Grade 2B
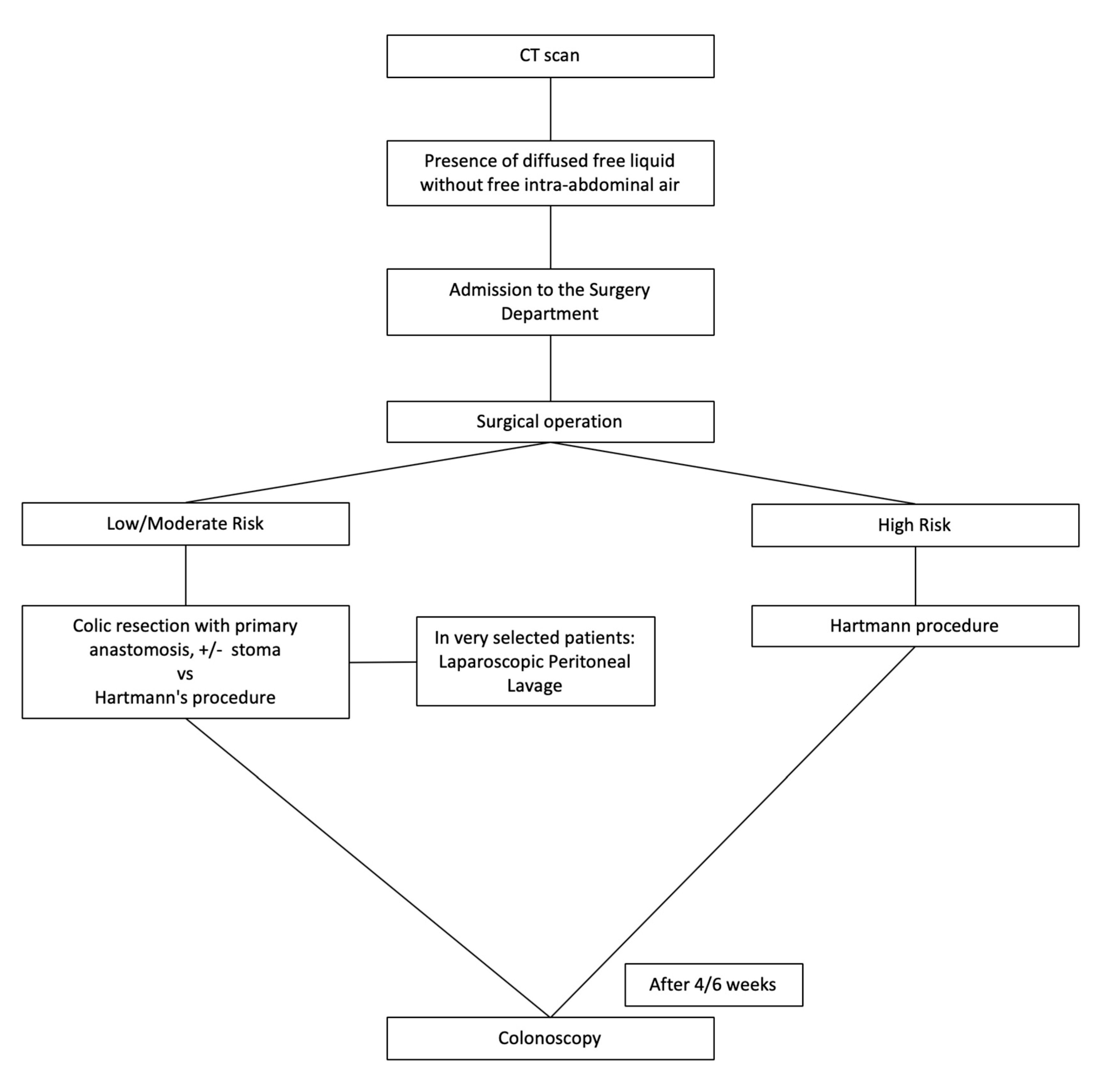
2.6. Acute Complicated Diverticulitis Grade 3
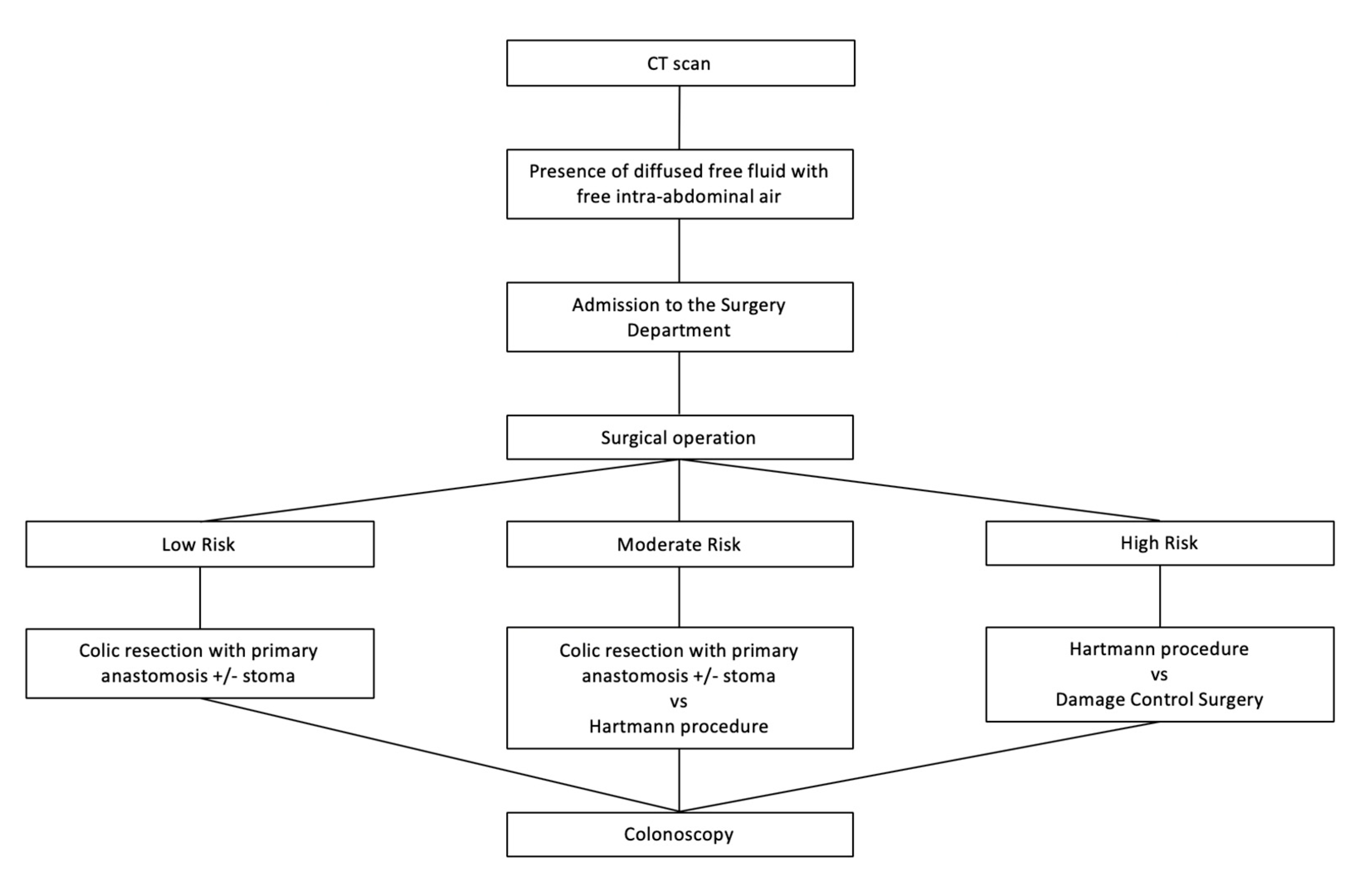
2.7. Acute Complicated Grade 4 Diverticulitis Grade
3. Results
- -
- A patient with low-risk grade 3 acute diverticulitis was treated with laparoscopic peritoneal lavage;
- -
- Seven patients with grade 3 AD, in the moderate risk class, had the following different treatments: one patient received hemicolectomy with protective stomas, five patients underwent resection and anastomosis, and one patient underwent Hartmann’s procedure;
- -
- Patients with high-risk acute grade 3 diverticulitis (13 cases) had the following treatments: three patients underwent Hartmann’s procedure; one underwent patient sub-total colectomy; and nine patients underwent resection and anastomosis.
- -
- Five unstable patients underwent a smart evaluation that included abdomen X-ray and abdomen ultrasound only. All these patients were in high risk group. In these cases, the surgical procedures adopted were four Hartmann’s procedures and one DCS.
- -
- Eleven stable patients underwent abdominal CT and then underwent Hartmann’s procedure (three moderate-risk patients and 8 high-risk patients).
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| Acute diverticulitis | (AD) |
| Number | (Nr.) |
| Damage control surgery | (DCS) |
| Ultrasonography | (US) |
| World Society of Emergency Surgery | (WSES) |
| Intensive Care Unit | (ICU) |
| American Society of Anesthesiologists | (ASA) |
| Patient | (pt) |
| Magnetic resonance imaging | (MRI) |
| Intra-abdominal sepsis | (IAS) |
| Non-operative treatment | (NonOP) |
| Computed tomography | (CT) |
| Focused Assessment with Sonography for Trauma | (FAST) |
| Laparoscopic peritoneal lavage | (LPL) |
| Male/female | (M/F) |
| Sequential Organ Failure Assessment | (SOFA) |
| American Society of Colon and Rectal Surgeons | (ASCRS) |
| Acute left-sided colonic diverticulitis | (ALCD) |
| C-reactive Protein | (CPR) |
References
- Dixon, M.R.; Trudel, J.L. Diverticular disease of the colon. In Current Surgical Therapy, 9th ed.; Cameron, J.L., Ed.; Elsevier: Philadelphia, PA, USA, 2004; pp. 166–170. [Google Scholar]
- Peery, A.F.; Dellon, E.S.; Lund, J.; Crockett, S.D.; McGowan, C.E.; Bulsiewicz, W.J.; Gangarosa, L.M.; Thiny, M.T.; Stizenberg, K.; Morgan, U.R.; et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology 2012, 143, 1179–1187.e3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ellison, D.L. Acute Diverticulitis Management. Crit. Care Nurs. Clin. N. Am. 2018, 30, 67–74. [Google Scholar] [CrossRef]
- Shah, S.D.; Cifu, A.S. Management of Acute Diverticulitis. JAMA 2017, 318, 291. [Google Scholar] [CrossRef] [PubMed]
- Binda, G.A.; Mataloni, F.; Bruzzone, M.; Carabotti, M.; Cirocchi, R.; Nascimbeni, R.; Gambassi, G.; Amato, A.; Vettoretto, N.; Pinnarelliet, L.; et al. Trends in hospital admission for acute diverticulitis in Italy from 2008 to 2015. Tech. Coloproctol. 2018, 22, 597–604. [Google Scholar] [CrossRef] [PubMed]
- Amato, A.; Mataloni, F.; Bruzzone, M.; Carabotti, M.; Cirocchi, R.; Nascimbeni, R.; Gambassi, G.; Vettoretto, N.P.; Pinnarelli, L.; Cuomo, R.; et al. Hospital admission for complicated diverticulitis is increasing in Italy, especially in younger patients: A national database study. Tech. Coloproctol. 2020, 24, 237–245. [Google Scholar] [CrossRef]
- Emile, S.H.; Elfeki, H.; Sakr, A.; Shalaby, M. Management of acute uncomplicated diverticulitis without antibiotics: A systematic review, meta-analysis, and meta-regression of predictors of treatment failure. Tech. Coloproctol. 2018, 22, 499–509. [Google Scholar] [CrossRef]
- Brook, M.A.; Victorino, G.P. Diverticular disease of the colon. In Abernathy’s Surgical Secrets, 7th ed.; Harken, A.H., Moore, E., Eds.; Elsevier: Philadelphia, PA, USA, 2018; pp. 224–226. [Google Scholar]
- Krukowski, Z.H.; Matheson, N.A. Emergency surgery for diverticular disease complicated by generalized and faecal peritonitis: A review. Br. J. Surg. 1984, 71, 921–927. [Google Scholar] [CrossRef]
- Parisi, A.; Gemini, A.; Desiderio, J.; Petrina, A.; Trastulli, S.; Grassi, V.; Sani, M.; Pironi, D.; Santoro, A. Laparoscopic peritoneal lavage: Our experience and review of the literature. Videosurgery Other Miniinvasive Tech. 2016, 11, 83–87. [Google Scholar] [CrossRef] [Green Version]
- Cirocchi, R.; Popivanov, G.; Corsi, A.; Amato, A.; Nascimbeni, R.; Cuomo, R.; Annibale, B.; Konaktchieva, M.; Binda, G.A. The Trends of Complicated Acute Colonic Diverticulitis—A Systematic Review of the National Administrative Databases. Medicina 2019, 55, 744. [Google Scholar] [CrossRef] [Green Version]
- Stollman, N.; Smalley, W.; Hirano, I.; Adams, M.A.; Dorn, S.D.; Dudley-Brown, S.L.; Flamm, S.L.; Gellad, Z.F.; Gruss, C.B.; Kosinski, L.R.; et al. American Gastroenterological Association Institute Guideline on the Management of Acute Diverticulitis. Gastroenterology 2015, 149, 1944–1949. [Google Scholar] [CrossRef] [Green Version]
- Bielecki, K.; Kaminski, P.; Klukowski, M. Large bowel perforation: Morbidity and mortality. Tech. Coloproctol. 2002, 6, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Ryan, O.K.; Ryan, É.J.; Creavin, B.; Boland, M.R.; Kelly, M.E.; Winter, D.C. Systematic review and meta-analysis comparing primary resection and anastomosis versus Hartmann’s procedure for the management of acute perforated diverticulitis with generalised peritonitis. Tech. Coloproctol. 2020, 24, 527–543. [Google Scholar] [CrossRef] [PubMed]
- Hinchey, E.J.; Schaal, P.G.; Richards, G.K. Treatment of perforated diverticular disease of the colon. Adv. Surg. 1978, 12, 85–109. [Google Scholar] [PubMed]
- Kaiser, A.M.; Jiang, J.-K.; Lake, J.P.; Ault, G.; Artinyan, A.; Gonzalez-Ruiz, C.; Essani, R.; Beart, R.W. The Management of Complicated Diverticulitis and the Role of Computed Tomography. Am. J. Gastroenterol. 2005, 100, 910–917. [Google Scholar] [CrossRef]
- Shafi, S.; Priest, E.L.; Crandall, M.L.; Klekar, C.S.; Nazim, A.; Aboutanos, M.; Agarwal, S.; Bhattacharya, B.; Byrge, N.; Dhillon, T.S.; et al. Multicenter validation of American Association for the Surgery of Trauma grading system for acute colonic diverticulitis and its use for emergency general surgery quality improvement program. J. Trauma Acute Care Surg. 2016, 80, 405–411. [Google Scholar] [CrossRef]
- Jacobs, D.O. Clinical practice. Diverticulitis. N. Engl. J. Med. 2007, 357, 2057–2066. [Google Scholar] [CrossRef]
- Andersen, J.C.; Bundgaard, L.; Elbrønd, H.; Laurberg, S.; Walker, L.R.; Støvring, J. Danish national guidelines for treatment of diverticular disease. Dan. Med. J. 2012, 59, C4453. [Google Scholar]
- Vennix, S.; Morton, D.G.; Hahnloser, D.; Lange, J.F.; Bemelman, W.A. The research committee of the European Society of Coloproctocology Systematic review of evidence and consensus on diverticulitis: An analysis of national and international guidelines. Colorectal Dis. 2014, 16, 866–878. [Google Scholar] [CrossRef]
- Jackson, J.D.; Hammond, T. Systematic review: Outpatient management of acute uncomplicated diverticulitis. Int. J. Colorectal Dis. 2014, 29, 775–781. [Google Scholar] [CrossRef]
- Sartelli, M.; Catena, F.; Ansaloni, L.; Coccolini, F.; Griffiths, E.A.; Abu-Zidan, F.M.; Di Saverio, S.; Ulrych, J.; Kluger, Y.; Ben-Ishay, O.; et al. WSES Guidelines for the management of acute left sided colonic diverticulitis in the emergency setting. World J. Emerg. Surg. 2016, 11, 37. [Google Scholar] [CrossRef] [Green Version]
- Kruis, W.; Germer, C.-T.; Leifeld, L. Diverticular Disease: Guidelines of the German Society for Gastroenterology, Digestive and Metabolic Diseases and the German Society for General and Visceral Surgery. Digestion 2014, 90, 190–207. [Google Scholar] [CrossRef] [PubMed]
- Fagenholz, P.J.; De Moya, M.A. Acute Inflammatory Surgical Disease. Surg. Clin. N. Am. 2014, 94, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.W.; Wexner, S.D.; Lowry, A.; Vernava, A.; Burnstein, M.; Denstman, F.; Fazio, V.; Kerner, B.; Moore, R.; Oliver, G.; et al. Practice parameters for the treatment of sigmoid diverticulitis—Supporting documentation. Dis. Colon Rectum 2000, 43, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Kohl, A.; Rosenberg, J.B.; Bock, D.; Bisgaard, D.; Skullman, S.; Thornell, A.; Gehrman, J.; Angenete, E.; Haglind, E. Two-year results of the randomized clinical trial DILALA comparing laparoscopic lavage with resection as treatment for perforated diverticulitis. Br. J. Surg. 2018, 105, 1128–1134. [Google Scholar] [CrossRef]
- Schwesinger, W.; Page, C.P.; Gaskill, H.V.; Steward, R.M.; Chopra, S.; Strodel, W.E.; Sirinek, K.R. Operative management of diverticular emergencies: Strategies and outcomes. Arch. Surg. 2000, 135, 558–562. [Google Scholar] [CrossRef] [Green Version]
- Brandt, D.; Gervaz, P.; Durmishi, Y.; Platon, A.; Morel, P.; Poletti, P.A. Percutaneous CT Scan-Guided Drainage vs. Antibiotherapy Alone for Hinchey II Diverticulitis: A Case-Control Study. Dis. Colon Rectum 2006, 49, 1533–1538. [Google Scholar] [CrossRef]
- Sallinen, V.; Mentula, P.; Leppaniemi, A.K. Nonoperative Management of Perforated Diverticulitis With Extraluminal Air Is Safe and Effective in Selected Patients. Dis. Colon Rectum 2014, 57, 875–881. [Google Scholar] [CrossRef]
- Liang, S.; Russek, K.; Franklin, M.E. Damage control strategy for the management of perforated diverticulitis with generalized peritonitis: Laparoscopic lavage and drainage vs. laparoscopic Hartmann’s procedure. Surg. Endosc. 2012, 26, 2835–2842. [Google Scholar] [CrossRef]
- Schultz, J.K.; Yaqub, S.; Wallon, C.; Blecic, L.; Forsmo, H.M.; Folkesson, J.; Buchwald, P.; Körner, H.; Dahl, F.A.; Øresland, T. Laparoscopic Lavage vs. Primary Resection for Acute Perforated Diverticulitis. JAMA 2015, 314, 1364–1375. [Google Scholar] [CrossRef] [Green Version]
- Binda, G.A.; Karas, J.R.; Serventi, A.; Sökmen, S.; Amato, A.; Hydo, L.; Bergamaschi, R.; for the Study Group on Diverticulitis. Primary anastomosisvsnonrestorative resection for perforated diverticulitis with peritonitis: A prematurely terminated randomized controlled trial. Colorectal Dis. 2012, 14, 1403–1410. [Google Scholar] [CrossRef]
- Regenbogen, S.E.; Hardiman, K.M.; Hendren, S.; Morris, A.M. Surgery for Diverticulitis in the 21st Century. JAMA Surg. 2014, 149, 292. [Google Scholar] [CrossRef] [Green Version]
- Cirocchi, R.; Nascimbeni, R.; Binda, G.A.; Vettoretto, N.; Cuomo, R.; Gambassi, G.; Amato, A.; Annibale, B. Surgical treatment of acute complicated diverticulitis in the elderly. Minerva Chir. 2020, 74, s0026–s4733. [Google Scholar] [CrossRef] [PubMed]
- Wheat, C.L.; Strate, L.L. Trends in Hospitalization for Diverticulitis and Diverticular Bleeding in the United States From 2000 to 2010. Clin. Gastroenterol. Hepatol. 2015, 14, 96–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sartelli, M.; Moore, F.A.; Ansaloni, L.; Di Saverio, S.; Coccolini, F.; Griffiths, E.A.; Coimbra, R.; Agresta, F.; Sakakushev, B.; Ordóñez, C.; et al. A proposal for a CT driven classification of left colon acute diverticulitis. World J. Emerg. Surg. 2015, 10, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weizman, A.V.; Nguyen, G.C. Diverticular disease: Epidemiology and management. Can. J. Gastroenterol. Hepatol. 2011, 25, 385–389. [Google Scholar] [CrossRef]
- You, J.K.; Bendl, R.; Taut, C.; Sullivan, R.; Gachabayov, M.; Bergamaschi, R.; the Study Group on Diverticulitis. Randomized clinical trial of elective resection versus observation in diverticulitis with extraluminal air or abscess initially managed conservatively. Br. J. Surg. 2018, 105, 971–979. [Google Scholar] [CrossRef]
- Cirocchi, R.; Randolph, J.J.; Binda, G.A.; Gioia, S.; Henry, B.M.; Tomaszewski, K.A.; Allegritti, M.; Arezzo, A.; Marzaioli, R.; Ruscelli, P. Is the outpatient management of acute diverticulitis safe and effective? A systematic review and meta-analysis. Tech. Coloproctol. 2019, 23, 87–100. [Google Scholar] [CrossRef]
- Feingold, D.; Steele, S.; Lee, S.; Kaiser, A.; Boushey, R.; Buie, W.D.; Rafferty, J.F. Practice Parameters for the Treatment of Sigmoid Diverticulitis. Dis. Colon Rectum 2014, 57, 284–294. [Google Scholar] [CrossRef] [Green Version]
- Hall, J.; Hardiman, K.; Lee, S.; Lightner, A.; Stocchi, L.; Paquette, I.M.; Steele, S.R.; Feingold, D.L.; Prepared on Behalf of the Clinical Practice Guidelines Committee of the American Society of Colon and Rectal Surgeons. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Treatment of Left-Sided Colonic Diverticulitis. Dis. Colon Rectum 2020, 63, 728–747. [Google Scholar] [CrossRef]
- Sartelli, M.; Weber, D.G.; Kluger, Y.; Ansaloni, L.; Coccolini, F.; Abu-Zidan, F.; Augustin, G.; Ben-Ishay, O.; Biffl, W.L.; Bouliaris, K.; et al. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J. Emerg. Surg. 2020, 15, 18–32. [Google Scholar] [CrossRef]
- Biondo, S. The diminishing role of surgery for acute diverticulitis. Br. J. Surg. 2019, 106, 308–309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Popivanov, G.; Fedeli, P.; Cirocchi, R.; Lancia, M.; Mascagni, D.; Giustozzi, M.; Teodosiev, I.; Kjossev, K.; Konaktchieva, M. Perirectal Hematoma and Intra-Abdominal Bleeding after Stapled Hemorrhoidopexy and STARR—A Proposal for a Decision-Making Algorithm. Medicina 2020, 56, 269. [Google Scholar] [CrossRef] [PubMed]
- Chiarini, S.; Ruscelli, P.; Cirocchi, R.; D’Andrea, V.; Sensi, B.; Santoro, A.; Corsi, A.; Zepponi, F.; Fedeli, P.; Gioia, S. Intersigmoid Hernia: A Forgotten Diagnosis—A Systematic Review of the Literature over Anatomical, Diagnostic, Surgical, and Medicolegal Aspects. Emerg. Med. Int. 2020, 2020, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Horesh, N.; Wasserberg, N.; Zbar, A.P.; Gravetz, A.; Berger, Y.; Gutman, M.; Rosin, D.; Zmora, O. Changing paradigms in the management of diverticulitis. Int. J. Surg. 2016, 33, 146–150. [Google Scholar] [CrossRef]
- Swanson, S.M.; Strate, L.L. Acute Colonic Diverticulitis. Ann. Intern. Med. 2018, 168, ITC65–ITC80. [Google Scholar] [CrossRef]
- Balasubramanian, I.; Fleming, C.; Mohan, H.M.; Schmidt, K.; Haglind, E.; Winter, D.C. Out-Patient Management of Mild or Uncomplicated Diverticulitis: A Systematic Review. Dig. Surg. 2016, 34, 151–160. [Google Scholar] [CrossRef]
- Stollman, N.; Raskin, J.B. Diverticular disease of the colon. Lancet 2004, 363, 631–639. [Google Scholar] [CrossRef] [Green Version]
- Schmidt, S.; Ismail, T.; Puhan, M.A.; Soll, C.; Fuchs, J. Meta-Analysis of surgical strategies in perforated left colonic diverticulitis with generalized peritonitis. Langenbeck’s Arch. Surg. 2018, 403, 425–433. [Google Scholar] [CrossRef] [Green Version]
- Reynolds, I.S.; O’Connell, E.; Heaney, R.M.; Khan, W.; Waldron, R.; Barry, K. Adherence to clinical guidelines and the potential economic benefits of admission avoidance for acute uncomplicated diverticulitis. Ir. J. Med. Sci. 2017, 187, 59–64. [Google Scholar] [CrossRef]

| Grade 1A | presence of pericolic air bubbles or minimum effusion without abscess |
| Grade 1B | presence of pericolic abscess with a diameter < 4 cm |
| Grade 2A | pericolic abscess of diameter > 4 cm and pelvic abscess |
| Grade 2B | presence of free intra-abdominal air > 5 cm away from the inflamed viscera |
| Grade 3 | presence of diffused free liquid without free intra-abdominal air |
| Grade 4 | presence of diffused free fluid with free intra-abdominal air |
| Low Risk | Patient Without a Higher Risk Class |
| Moderate risk |
|
| High risk | Sepsis complicated by the dysfunction of one or more of the following organs or systems:
|
| Male/female (n) | 23/30 |
| Age (years) mean | 64 |
| ASA score (mean) | 3 |
| Quick SOFA (mean) | 1.7 |
| CT scan (n. patients) | 48 |
| “Smart” ultrasonography evaluation (n. patients) | 5 |
| Non-operative treatment (n. patients) | 16 |
| Surgery as a first therapeutic approach (n. patients) | 37 |
| Intra-operative mortality | 0% |
| Post-operative mortality | 5.8% |
| Average total hospital stay (days) | 11 |
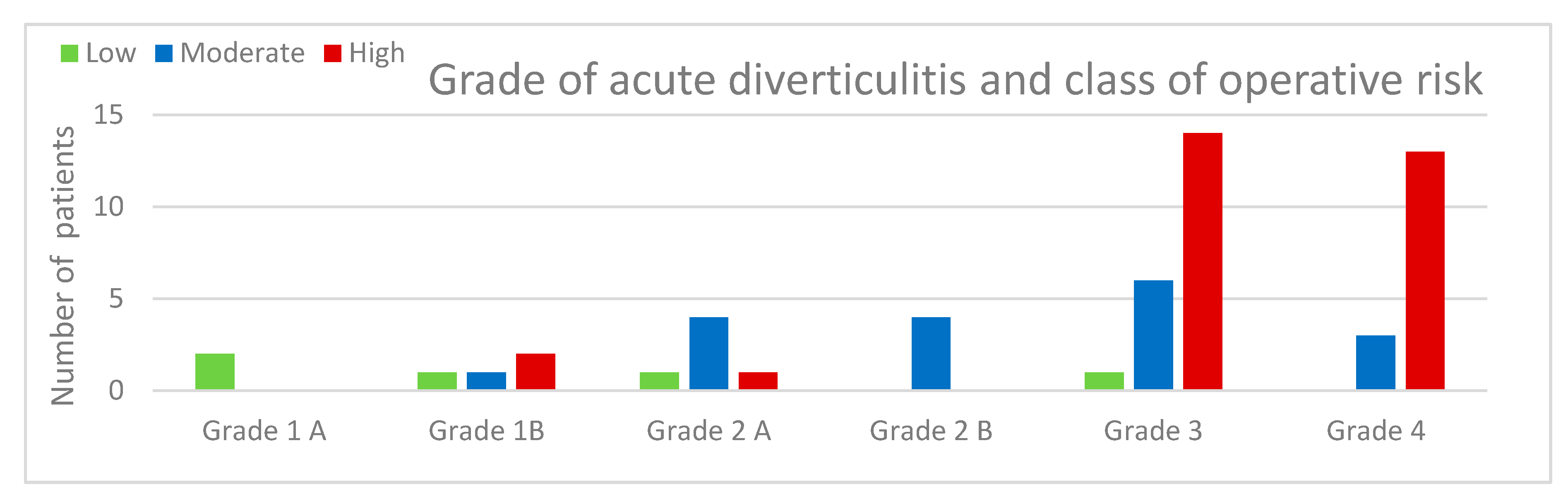
| Acute complicated diverticulitis grade 1A | 2 pt (3.7%) | Class of risk low | 2 pt 3.7% |
| Acute complicated diverticulitis grade 1B | 4 pt (7.5%) | Class of risk low | 1 pt 1.9% |
| Class of risk moderate | 1 pt 1.9% | ||
| Class of risk high | 2 pt 3.7% | ||
| Acute complicated diverticulitis grade 2A | 6 pt (11.3%) | Class of risk low | 1 pt 1.9% |
| Class of risk moderate | 4 pt 7.5% | ||
| Class of risk high | 1 pt 1.9% | ||
| Acute complicated diverticulitis grade 2B | 4 pt (7.5%) | Class of risk moderate | 4 pt 7.5% |
| Acute complicated diverticulitis grade 3 | 21 pt (39.6%) | Class of risk low | 1 pt 1.9% |
| Class of risk moderate | 7 pt 13.2% | ||
| Class of risk high | 13 pt 24.5% | ||
| Acute complicated diverticulitis grade 4 | 16 pt (30.2%) | Class of risk moderate | 3 pt 5.7% |
| Class of risk high | 13 pt 24.5% |
| NON-OPERATIVE TREATMENT (16 PATIENTS) | |||
|---|---|---|---|
| ONLY ANTIBIOTIC THERAPY (8 PATIENTS) | PERCUTANEOUS DRAINAGE (8 PATIENTS) | ||
| 2 patients in group 1A | 2 pt low risk | 2 patients in group 1B | 2 pt high risk |
| 2 patients in group 1B | 1 pt low risk | 6 patients in group 2A | 1 pt low risk |
| 1 pt moderate risk | 4 pt moderate risk | ||
| 4 patients in group 2B | 4 pt moderate risk | 1 pt high risk | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruscelli, P.; Cirocchi, R.; Gemini, A.; Bruzzone, P.; Campanale, M.; Rimini, M.; Santella, S.; Anaia, G.; Graziosi, L.; Donini, A. A Hospital Protocol for Decision Making in Emergency Admission for Acute Diverticulitis: Initial Results from Small Cohort Series. Medicina 2020, 56, 371. https://doi.org/10.3390/medicina56080371
Ruscelli P, Cirocchi R, Gemini A, Bruzzone P, Campanale M, Rimini M, Santella S, Anaia G, Graziosi L, Donini A. A Hospital Protocol for Decision Making in Emergency Admission for Acute Diverticulitis: Initial Results from Small Cohort Series. Medicina. 2020; 56(8):371. https://doi.org/10.3390/medicina56080371
Chicago/Turabian StyleRuscelli, Paolo, Roberto Cirocchi, Alessandro Gemini, Paolo Bruzzone, Michelangelo Campanale, Massimiliano Rimini, Sergio Santella, Gabriele Anaia, Luigina Graziosi, and Annibale Donini. 2020. "A Hospital Protocol for Decision Making in Emergency Admission for Acute Diverticulitis: Initial Results from Small Cohort Series" Medicina 56, no. 8: 371. https://doi.org/10.3390/medicina56080371






