Risk of Breast Cancer in Women with Mastitis: A Retrospective Population-Based Cohort Study
Abstract
:1. Introduction
2. Material and Methods
2.1. Data Sources
2.2. Study Group and Outcome
2.3. Covariates
2.4. Study Covariates
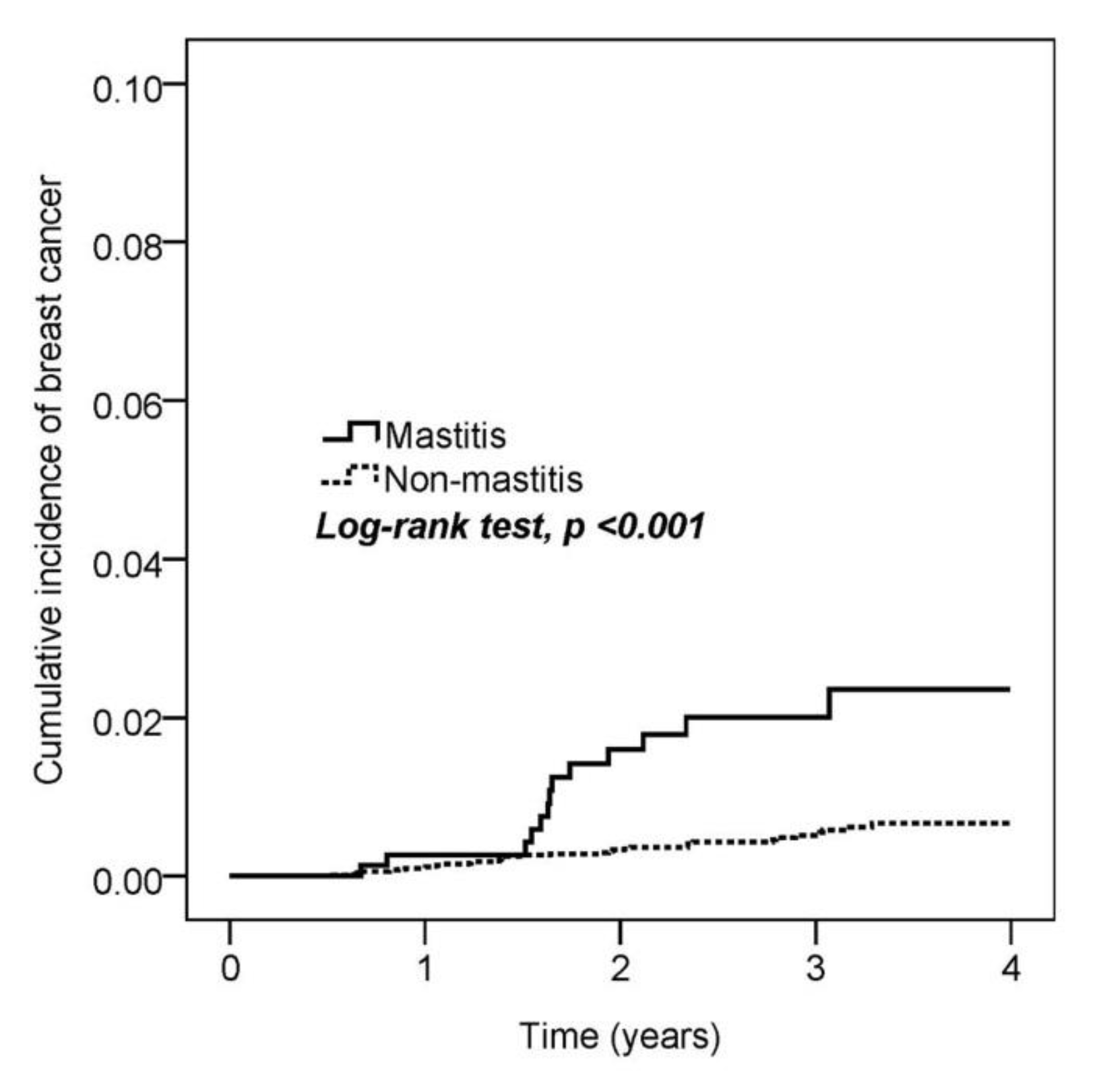
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ghoncheh, M.; Pournamdar, Z.; Salehiniya, H. Incidence and mortality and epidemiology of breast cancer in the world. Asian Pac. J. Cancer Prev. 2016, 17, 43–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghoncheh, M.; Momenimovahed, Z.; Salehiniya, H. Epidemiology, incidence and mortality of breast cancer in asia. Asian Pac. J. Cancer Prev. 2016, 17, 47–52. [Google Scholar] [CrossRef] [Green Version]
- Chang, H.T.; Shi, H.Y.; Wang, B.W.; Yeh, S.J. Breast cancer incidence and predictors of surgical outcome: A nationwide longitudinal study in taiwan. Clin. Oncol. (R. Coll. Radiol.) 2017, 29, 362–369. [Google Scholar] [CrossRef] [PubMed]
- Waldman, R.A.; Finch, J.; Grant-Kels, J.M.; Whitaker-Worth, D. Skin diseases of the breast and nipple: Inflammatory and infectious diseases. J. Am. Acad. Dermatol. 2019, 80, 1483–1494. [Google Scholar] [CrossRef] [PubMed]
- Angelopoulou, A.; Field, D.; Ryan, C.A.; Stanton, C.; Hill, C.; Ross, R.P. The microbiology and treatment of human mastitis. Med. Microbiol. Immunol. 2018, 207, 83–94. [Google Scholar] [CrossRef]
- Co, M.; Cheng, V.C.C.; Wei, J.; Wong, S.C.Y.; Chan, S.M.S.; Shek, T.; Kwong, A. Idiopathic granulomatous mastitis: A 10-year study from a multicentre clinical database. Pathology 2018, 50, 742–747. [Google Scholar] [CrossRef]
- Sun, Y.S.; Zhao, Z.; Yang, Z.N.; Xu, F.; Lu, H.J.; Zhu, Z.Y.; Shi, W.; Jiang, J.; Yao, P.P.; Zhu, H.P. Risk factors and preventions of breast cancer. Int. J. Biol. Sci. 2017, 13, 1387–1397. [Google Scholar] [CrossRef] [Green Version]
- Amitay, E.L.; Carr, P.R.; Jansen, L.; Walter, V.; Roth, W.; Herpel, E.; Kloor, M.; Blaker, H.; Chang-Claude, J.; Brenner, H.; et al. Association of aspirin and nonsteroidal anti-inflammatory drugs with colorectal cancer risk by molecular subtypes. J. Natl. Cancer Inst. 2019, 111, 475–483. [Google Scholar] [CrossRef]
- Kehm, R.D.; Hopper, J.L.; John, E.M.; Phillips, K.A.; MacInnis, R.J.; Dite, G.S.; Milne, R.L.; Liao, Y.; Zeinomar, N.; Knight, J.A.; et al. Regular use of aspirin and other non-steroidal anti-inflammatory drugs and breast cancer risk for women at familial or genetic risk: A cohort study. Breast Cancer Res. 2019, 21, 52. [Google Scholar] [CrossRef]
- Ma, Y.; Yu, P.; Lin, S.; Li, Q.; Fang, Z.; Huang, Z. The association between nonsteroidal anti-inflammatory drugs and skin cancer: Different responses in american and european populations. Pharmacol. Res. 2020, 152, 104499. [Google Scholar] [CrossRef]
- Tomic, T.; Dominguez-Lopez, S.; Barrios-Rodriguez, R. Non-aspirin non-steroidal anti-inflammatory drugs in prevention of colorectal cancer in people aged 40 or older: A systematic review and meta-analysis. Cancer Epidemiol. 2019, 58, 52–62. [Google Scholar] [CrossRef] [PubMed]
- Frisk, G.; Ekberg, S.; Lidbrink, E.; Eloranta, S.; Sund, M.; Fredriksson, I.; Lambe, M.; Smedby, K.E. No association between low-dose aspirin use and breast cancer outcomes overall: A swedish population-based study. Breast Cancer Res. 2018, 20, 142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lambe, M.; Johansson, A.L.; Altman, D.; Eloranta, S. Mastitis and the risk of breast cancer. Epidemiology 2009, 20, 747–751. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.M.; Lin, M.C.; Yin, W.Y. Risk of breast cancer in women with non-lactational mastitis. Sci. Rep. 2019, 9, 15587. [Google Scholar] [CrossRef]
- Nolan, J.; Dunne, S.S.; Mustafa, W.; Sivananthan, L.; Kiely, P.A.; Dunne, C.P. Proposed hypothesis and rationale for association between mastitis and breast cancer. Med. Hypotheses 2020, 144, 110057. [Google Scholar] [CrossRef]
- Chiang, P.H.; Tang, F.H.; Tsai, E.M.; Chang, Y.C.; Yang, C.Y. Hormone therapy as risk factor of breast cancer modulated by diagnostic and lifestyle risk factors in taiwan-a national cohort study. Breast J. 2019, 25, 531–534. [Google Scholar] [CrossRef]
- Jones, M.E.; Schoemaker, M.J.; Wright, L.B.; Ashworth, A.; Swerdlow, A.J. Smoking and risk of breast cancer in the generations study cohort. Breast Cancer Res. 2017, 19, 118. [Google Scholar] [CrossRef]
- Morrison, L.; Laukkanen, J.A.; Ronkainen, K.; Kurl, S.; Kauhanen, J.; Toriola, A.T. Inflammatory biomarker score and cancer: A population-based prospective cohort study. BMC Cancer 2016, 16, 80. [Google Scholar] [CrossRef] [Green Version]
- Stikbakke, E.; Richardsen, E.; Knutsen, T.; Wilsgaard, T.; Giovannucci, E.L.; McTiernan, A.; Eggen, A.E.; Haugnes, H.S.; Thune, I. Inflammatory serum markers and risk and severity of prostate cancer: The proca-life study. Int. J. Cancer 2019. [Google Scholar] [CrossRef] [Green Version]
- Ugge, H.; Downer, M.K.; Carlsson, J.; Bowden, M.; Davidsson, S.; Mucci, L.A.; Fall, K.; Andersson, S.O.; Andren, O. Circulating inflammation markers and prostate cancer. Prostate 2019, 79, 1338–1346. [Google Scholar] [CrossRef]
- Tsoi, K.K.F.; Ho, J.M.W.; Chan, F.C.H.; Sung, J.J.Y. Long-term use of low-dose aspirin for cancer prevention: A 10-year population cohort study in hong kong. Int. J. Cancer 2019, 145, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Hwang, D.; Scollard, D.; Byrne, J.; Levine, E. Expression of cyclooxygenase-1 and cyclooxygenase-2 in human breast cancer. J. Natl. Cancer Inst. 1998, 90, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Ricciotti, E.; FitzGerald, G.A. Prostaglandins and inflammation. Arterioscler. Thromb Vasc. Biol. 2011, 31, 986–1000. [Google Scholar] [CrossRef] [PubMed]
- Howe, L.R. Inflammation and breast cancer. Cyclooxygenase/prostaglandin signaling and breast cancer. Breast Cancer Res. 2007, 9, 210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aggarwal, A.; Al-Rohil, R.N.; Batra, A.; Feustel, P.J.; Jones, D.M.; DiPersio, C.M. Expression of integrin α3β1 and cyclooxygenase-2 (cox2) are positively correlated in human breast cancer. BMC Cancer 2014, 14, 459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Majumder, M.; Dunn, L.; Liu, L.; Hasan, A.; Vincent, K.; Brackstone, M.; Hess, D.; Lala, P.K. Cox-2 induces oncogenic micro rna mir655 in human breast cancer. Sci. Rep. 2018, 8, 327. [Google Scholar] [CrossRef] [Green Version]
- Jiang, W.G.; Watkins, G.; Douglas-Jones, A.; Mansel, R.E. Reduction of isoforms of 15-lipoxygenase (15-lox)-1 and 15-lox-2 in human breast cancer. Prostaglandins Leukot. Essent. Fat. Acids 2006, 74, 235–245. [Google Scholar] [CrossRef]
- Singh, A.K.; Singh, R.; Naz, F.; Chauhan, S.S.; Dinda, A.; Shukla, A.A.; Gill, K.; Kapoor, V.; Dey, S. Structure based design and synthesis of peptide inhibitor of human lox-12: In vitro and in vivo analysis of a novel therapeutic agent for breast cancer. PLoS ONE 2012, 7, e32521. [Google Scholar] [CrossRef] [Green Version]
- Pucci, S.; Polidoro, C.; Greggi, C.; Amati, F.; Morini, E.; Murdocca, M.; Biancolella, M.; Orlandi, A.; Sangiuolo, F.; Novelli, G. Pro-oncogenic action of lox-1 and its splice variant lox-1δ4 in breast cancer phenotypes. Cell Death Dis. 2019, 10, 53. [Google Scholar] [CrossRef] [Green Version]
- Raza, U.; Asif, M.R.; Rehman, A.B.; Sheikh, A. Hyperlipidemia and hyper glycaemia in breast cancer patients is related to disease stage. Pak. J. Med. Sci. 2018, 34, 209–214. [Google Scholar] [CrossRef]
- Potluri, R.; Carter, P.R.; Lavu, D.; Bainey, K.R. The interplay between cholesterol and breast cancer: Is there a potential role for statin therapy? Future Oncol. 2018, 14, 1885–1888. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borgquist, S.; Giobbie-Hurder, A.; Ahern, T.P.; Garber, J.E.; Colleoni, M.; Lang, I.; Debled, M.; Ejlertsen, B.; von Moos, R.; Smith, I.; et al. Cholesterol, cholesterol-lowering medication use, and breast cancer outcome in the big 1–98 study. J. Clin. Oncol. 2017, 35, 1179–1188. [Google Scholar] [CrossRef] [PubMed]
- Buss, L.A.; Dachs, G.U. The role of exercise and hyperlipidaemia in breast cancer progression. Exerc. Immunol. Rev. 2018, 24, 10–25. [Google Scholar]
- Ardalan, A.; Bungum, T. Gestational age and the risk of maternal breast cancer: A population-based case-control study. Breast J. 2016, 22, 657–661. [Google Scholar] [CrossRef] [PubMed]
- Lambertini, M.; Santoro, L.; Del Mastro, L.; Nguyen, B.; Livraghi, L.; Ugolini, D.; Peccatori, F.A.; Azim, H.A., Jr. Reproductive behaviors and risk of developing breast cancer according to tumor subtype: A systematic review and meta-analysis of epidemiological studies. Cancer Treat. Rev. 2016, 49, 65–76. [Google Scholar] [CrossRef] [PubMed]

| Mastitis (N = 734) | Non-Mastitis (N = 7900) | ||||
|---|---|---|---|---|---|
| n | % | n | % | p-Value | |
| Age | 0.272 | ||||
| 40–50 | 390 | 53.1 | 4364 | 55.2 | |
| ≥50 | 344 | 46.9 | 3536 | 44.8 | |
| Mean ± SD | 51.1 ± 8.7 | 50.7 ± 8.8 | 0.195 | ||
| Hypertension | 151 | 20.6 | 1393 | 17.6 | 0.047 |
| Hyperlipidemia | 118 | 16.1 | 937 | 11.9 | 0.001 |
| Diabetes | 67 | 9.1 | 653 | 8.3 | 0.419 |
| Hyperthyroidism | 13 | 1.8 | 115 | 1.5 | 0.499 |
| Hypothyroidism | 10 | 1.4 | 73 | 0.9 | 0.244 |
| Autoimmune diseases | 18 | 2.5 | 183 | 2.3 | 0.815 |
| No. of Breast Cancer Events | Observed Person-Years | ID | CrudeHR | 95% CI | p Value | aHR † | 95% CI | p Value | |
|---|---|---|---|---|---|---|---|---|---|
| Mastitis | |||||||||
| No | 36 | 20,576 | 1.7 | 1 | 1 | ||||
| Yes | 13 | 1918 | 6.8 | 3.87 | 2.05–7.3 | <0.001 | 3.71 | 1.96–7.02 | <0.001 |
| Age | |||||||||
| 40–50 | 26 | 12,250 | 2.1 | 1 | 1 | ||||
| ≥50 | 23 | 10,245 | 2.2 | 1.06 | 0.61–1.86 | 0.831 | 1.17 | 0.65–2.10 | 0.594 |
| Hypertension | 2 | 3979 | 0.5 | 0.20 | 0.05–0.82 | 0.025 | 0.14 | 0.03–0.58 | 0.007 |
| Hyperlipidemia | 10 | 2725 | 3.7 | 1.87 | 0.93–3.74 | 0.078 | 2.53 | 1.15–5.57 | 0.021 |
| Diabetes | 4 | 1871 | 2.1 | 0.99 | 0.35–2.74 | 0.980 | 0.89 | 0.29–2.74 | 0.835 |
| Hypothyroidism | 1 | 224 | 4.5 | 2.07 | 0.29–15.02 | 0.471 | 1.59 | 0.22–11.76 | 0.649 |
| Autoimmune diseases | 1 | 523 | 1.9 | 0.87 | 0.12–6.33 | 0.894 | 0.93 | 0.13–6.77 | 0.945 |
| Mastitis | Non-Mastitis | ||||||
|---|---|---|---|---|---|---|---|
| N | No. of Breast Cancer Events | N | No. of Breast Cancer Events | HR | 95% CI | p Value | |
| Age | |||||||
| 20–50 | 390 | 5 | 4364 | 21 | 2.66 | 1.00–7.05 | 0.049 |
| ≥50 | 344 | 8 | 3536 | 15 | 5.46 | 2.31–12.87 | <0.001 |
| Hypertension | |||||||
| No | 583 | 12 | 6507 | 35 | 3.84 | 2.00–7.41 | <0.001 |
| Yes | 151 | 1 | 1393 | 1 | 9.10 | 0.57–145.52 | 0.118 |
| Hyperlipidemia | |||||||
| No | 616 | 9 | 6963 | 30 | 3.41 | 1.62–7.19 | 0.001 |
| Yes | 118 | 4 | 937 | 6 | 4.88 | 1.38–17.31 | 0.014 |
| Diabetes | |||||||
| No | 667 | 10 | 7247 | 35 | 3.09 | 1.53–6.25 | 0.002 |
| Yes | 67 | 3 | 653 | 1 | 28.45 | 2.96–273.49 | 0.004 |
| Hyperthyroidism | |||||||
| No | 721 | 13 | 7785 | 36 | 3.88 | 2.06–7.31 | <0.001 |
| Yes | 13 | 0 | 115 | 0 | NA | NA | NA |
| Hypothyroidism | |||||||
| No | 724 | 13 | 7827 | 35 | 4.00 | 2.12–7.56 | <0.001 |
| Yes | 10 | 0 | 73 | 1 | NA | NA | NA |
| Autoimmune diseases | |||||||
| No | 716 | 13 | 7717 | 35 | 4.00 | 2.12–7.56 | <0.001 |
| Yes | 18 | 0 | 183 | 1 | NA | NA | NA |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.-C.; Chan, C.-H.; Lim, Y.-B.; Yang, S.-F.; Yeh, L.-T.; Wang, Y.-H.; Chou, M.-C.; Yeh, C.-B. Risk of Breast Cancer in Women with Mastitis: A Retrospective Population-Based Cohort Study. Medicina 2020, 56, 372. https://doi.org/10.3390/medicina56080372
Chen Y-C, Chan C-H, Lim Y-B, Yang S-F, Yeh L-T, Wang Y-H, Chou M-C, Yeh C-B. Risk of Breast Cancer in Women with Mastitis: A Retrospective Population-Based Cohort Study. Medicina. 2020; 56(8):372. https://doi.org/10.3390/medicina56080372
Chicago/Turabian StyleChen, Ying-Cheng, Chi-Ho Chan, Yu-Bing Lim, Shun-Fa Yang, Liang-Tsai Yeh, Yu-Hsun Wang, Ming-Chih Chou, and Chao-Bin Yeh. 2020. "Risk of Breast Cancer in Women with Mastitis: A Retrospective Population-Based Cohort Study" Medicina 56, no. 8: 372. https://doi.org/10.3390/medicina56080372






