Osimertinib-Associated Toxic Epidermal Necrolysis in a Lung Cancer Patient Harboring an EGFR Mutation—A Case Report and a Review of the Literature
Abstract
1. Introduction
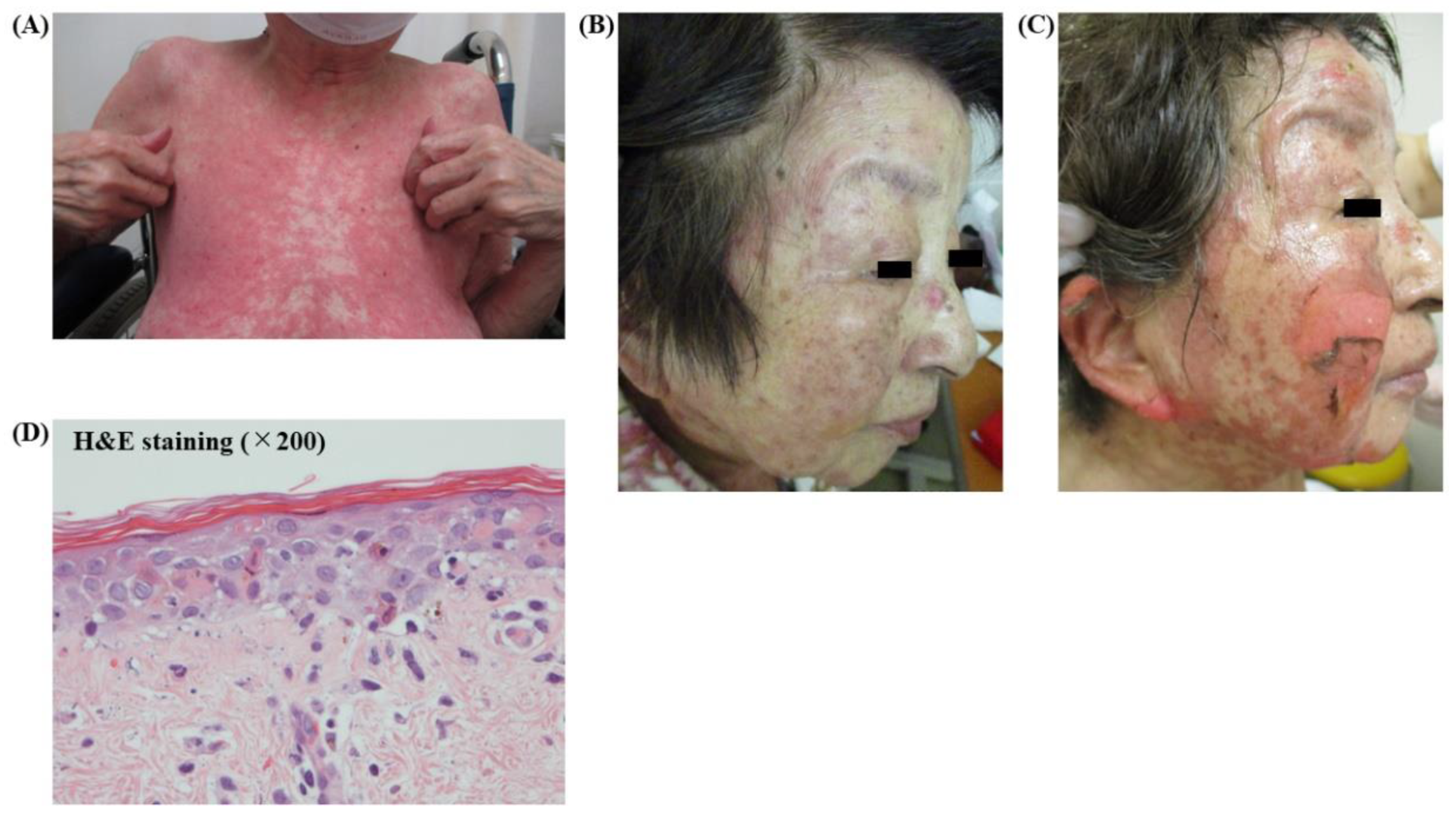
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lynch, T.J.; Bell, D.W.; Sordella, R.; Gurubhagavatula, S.; Okimoto, R.A.; Brannigan, B.W.; Harris, P.L.; Haserlat, S.M.; Supko, J.G.; Haluska, F.G.; et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N. Engl. J. Med. 2004, 350, 2129–2139. [Google Scholar] [CrossRef] [PubMed]
- Paez, J.G. EGFR Mutations in lung cancer: Correlation with clinical response to gefitinib therapy. Science 2004, 304, 1497–1500. [Google Scholar] [CrossRef] [PubMed]
- Takano, T.; Fukui, T.; Ohe, Y.; Tsuta, K.; Yamamoto, S.; Nokihara, H.; Yamamoto, N.; Sekine, I.; Kunitoh, H.; Furuta, K.; et al. EGFR mutations predict survival benefit from gefitinib in patients with advanced lung adenocarcinoma: A historical comparison of patients treated before and after gefitinib approval in Japan. J. Clin. Oncol. 2008, 26, 5589–5595. [Google Scholar] [CrossRef] [PubMed]
- Mok, T.S.; Wu, Y.L.; Ahn, M.J.; Garassino, M.C.; Kim, H.R.; Ramalingam, S.S.; Shepherd, F.A.; He, Y.; Akamatsu, H.; Theelen, W.S.; et al. Osimertinib or platinum-pemetrexed in EGFR T790M-positive lung cancer. N. Engl. J. Med. 2016, 376, 629–640. [Google Scholar] [CrossRef] [PubMed]
- Soria, J.C.; Ohe, Y.; Vansteenkiste, J.; Reungwetwattana, T.; Chewaskulyong, B.; Lee, K.H.; Dechaphunkul, A.; Imamura, F.; Nogami, N.; Kurata, T.; et al. Osimertinib in untreated EGFR-mutated advanced Non–small-cell lung cancer. N. Engl. J. Med. 2018, 378, 113–125. [Google Scholar] [CrossRef] [PubMed]
- Lerch, M.; Mainetti, C.; Beretta-Piccoli, B.T.; Harr, T. Current perspectives on stevens-johnson syndrome and toxic epidermal necrolysis. Clin. Rev. Allergy Immunol. 2017, 54, 147–176. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.T.; Chu, C. Osimertinib-induced Stevens-Johnson syndrome in a patient with EGFR T790M mutation-positive non-small cell lung cancer. Lung Cancer 2019, 129, 110–111. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Cheng, X.; Lu, Y.; Zhou, B. A case report of toxic epidermal necrolysis associated with AZD-9291. Drug Des. Dev. Ther. 2018, 12, 2163–2167. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.J.; Ma, S.-X.; Hou, X.; Wang, Z.; Zeng, Y.D.; Qin, T.; Dinglin, X.X.; Chen, L.K. Toxic epidermal necrolysis related to AP (pemetrexed plus cisplatin) and gefitinib combination therapy in a patient with metastatic non-small cell lung cancer. Chin. J. Cancer 2015, 34, 94–98. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Doesch, J.; Debus, D.; Meyer, C.; Papadopoulos, T.; Schultz, E.S.; Ficker, J.H.; Brueckl, W. Afatinib-associated Stevens-Johnson syndrome in an EGFR-mutated lung cancer patient. Lung Cancer 2016, 95, 35–38. [Google Scholar] [CrossRef] [PubMed]
- Otsuka, T.; Tanaka, A.; Azukizawa, H.; Sasaki, S.; Ishijima, M.; Matsuki, T.; Osa, A.; Nakatani, T.; Kuroyama, M.; Hirata, H.; et al. Successful treatment with gefitinib after Stevens–Johnson syndrome associated with afatinib therapy in a patient with adenocarcinoma of the lung. Int. Cancer Conf. J. 2016, 6, 38–41. [Google Scholar] [CrossRef] [PubMed]
- Melosky, B.; Leighl, N.; Rothenstein, J.; Sangha, R.; Stewart, D.; Papp, K. Management of egfr tki–induced dermatologic adverse events. Curr. Oncol. 2015, 22, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Kozuki, T. Skin problems and EGFR-tyrosine kinase inhibitor. Jpn. J. Clin. Oncol. 2016, 46, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Ohe, Y.; Imamura, F.; Nogami, N.; Okamoto, I.; Kurata, T.; Kato, T.; Sugawara, S.; Ramalingam, S.S.; Uchida, H.; Hodge, R.; et al. Osimertinib versus standard-of-care EGFR-TKI as first-line treatment for EGFRm advanced NSCLC: FLAURA Japanese subset. Jpn. J. Clin. Oncol. 2019, 49, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Chung, W.H.; Hung, S.I.; Hong, H.S.; Hsih, M.S.; Yang, L.C.; Ho, H.C.; Wu, J.Y.; Chen, Y.T. Medical genetics: A marker for Stevens-Johnson syndrome. Nature 2004, 428, 486. [Google Scholar] [CrossRef] [PubMed]
- Khoo, A.; Foo, C. Toxic epidermal necrolysis in a burns centre: A 6-year review. Burns 1996, 22, 275–278. [Google Scholar] [CrossRef]
- Roujeau, J.C.; Kelly, J.P.; Naldi, L.; Rzany, B.; Stern, R.S.; Anderson, T.; Auquier, A.; Bastuji-Garin, S.; Correia, O.; Locati, F.; et al. Medication use and the risk of stevens–johnson syndrome or toxic epidermal necrolysis. N. Engl. J. Med. 1995, 333, 1600–1608. [Google Scholar] [CrossRef] [PubMed]
- Lonjou, C.; Thomas, L.; Borot, N.; Ledger, N.; De Toma, C.; LeLouet, H.; Graf, E.; Schumacher, M.; Hovnanian, A.; Mockenhaupt, M.; et al. A marker for Stevens-Johnson syndrome: Ethnicity matters. Pharm. J. 2006, 6, 265–268. [Google Scholar] [CrossRef] [PubMed]

| Author, Reported Year | Age | Sex | Nationality | EGFR-TKI | SJS/TEN | Onset | Treatment and Outcome |
|---|---|---|---|---|---|---|---|
| Huang, et al., 2015. [9] | 42 | female | Chinese | gefitinib | TEN | 8 days | mPSL and IVIG, recovery after 40 days |
| Doesch, et al., 2016. [10] | 79 | female | German | afatinib | SJS | 64 days | PSL, recovery after 60 days |
| Otsuka, et al., 2016. [11] | 65 | female | Japanese | afatinib | SJS | 32 days | mPSL and IVIG, recovery after 60 days |
| Wang et al., 2018. [8] | 51 | male | Chinese | osimertinib | TEN | 21 days | mPSL and IVIG, recovery after 30 days |
| Lin et al., 2019. [7] | 57 | female | Taiwanese | osimertinib | SJS | 22 days | PSL, recovery after 60 days |
| Current case. 2020. | 80 | female | Japanese | osimertinib | TEN | 32 days | PSL and IVIG, recovery after 80 days |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sato, I.; Mizuno, H.; Kataoka, N.; Kunimatsu, Y.; Tachibana, Y.; Sugimoto, T.; Tani, N.; Ogura, Y.; Hirose, K.; Takeda, T. Osimertinib-Associated Toxic Epidermal Necrolysis in a Lung Cancer Patient Harboring an EGFR Mutation—A Case Report and a Review of the Literature. Medicina 2020, 56, 403. https://doi.org/10.3390/medicina56080403
Sato I, Mizuno H, Kataoka N, Kunimatsu Y, Tachibana Y, Sugimoto T, Tani N, Ogura Y, Hirose K, Takeda T. Osimertinib-Associated Toxic Epidermal Necrolysis in a Lung Cancer Patient Harboring an EGFR Mutation—A Case Report and a Review of the Literature. Medicina. 2020; 56(8):403. https://doi.org/10.3390/medicina56080403
Chicago/Turabian StyleSato, Izumi, Hiroki Mizuno, Nobutaka Kataoka, Yusuke Kunimatsu, Yusuke Tachibana, Takumi Sugimoto, Nozomi Tani, Yuri Ogura, Kazuki Hirose, and Takayuki Takeda. 2020. "Osimertinib-Associated Toxic Epidermal Necrolysis in a Lung Cancer Patient Harboring an EGFR Mutation—A Case Report and a Review of the Literature" Medicina 56, no. 8: 403. https://doi.org/10.3390/medicina56080403
APA StyleSato, I., Mizuno, H., Kataoka, N., Kunimatsu, Y., Tachibana, Y., Sugimoto, T., Tani, N., Ogura, Y., Hirose, K., & Takeda, T. (2020). Osimertinib-Associated Toxic Epidermal Necrolysis in a Lung Cancer Patient Harboring an EGFR Mutation—A Case Report and a Review of the Literature. Medicina, 56(8), 403. https://doi.org/10.3390/medicina56080403





