Granulomatosis with Polyangiitis Restricted to the Back Muscle: The First Case Report
Abstract
1. Introduction
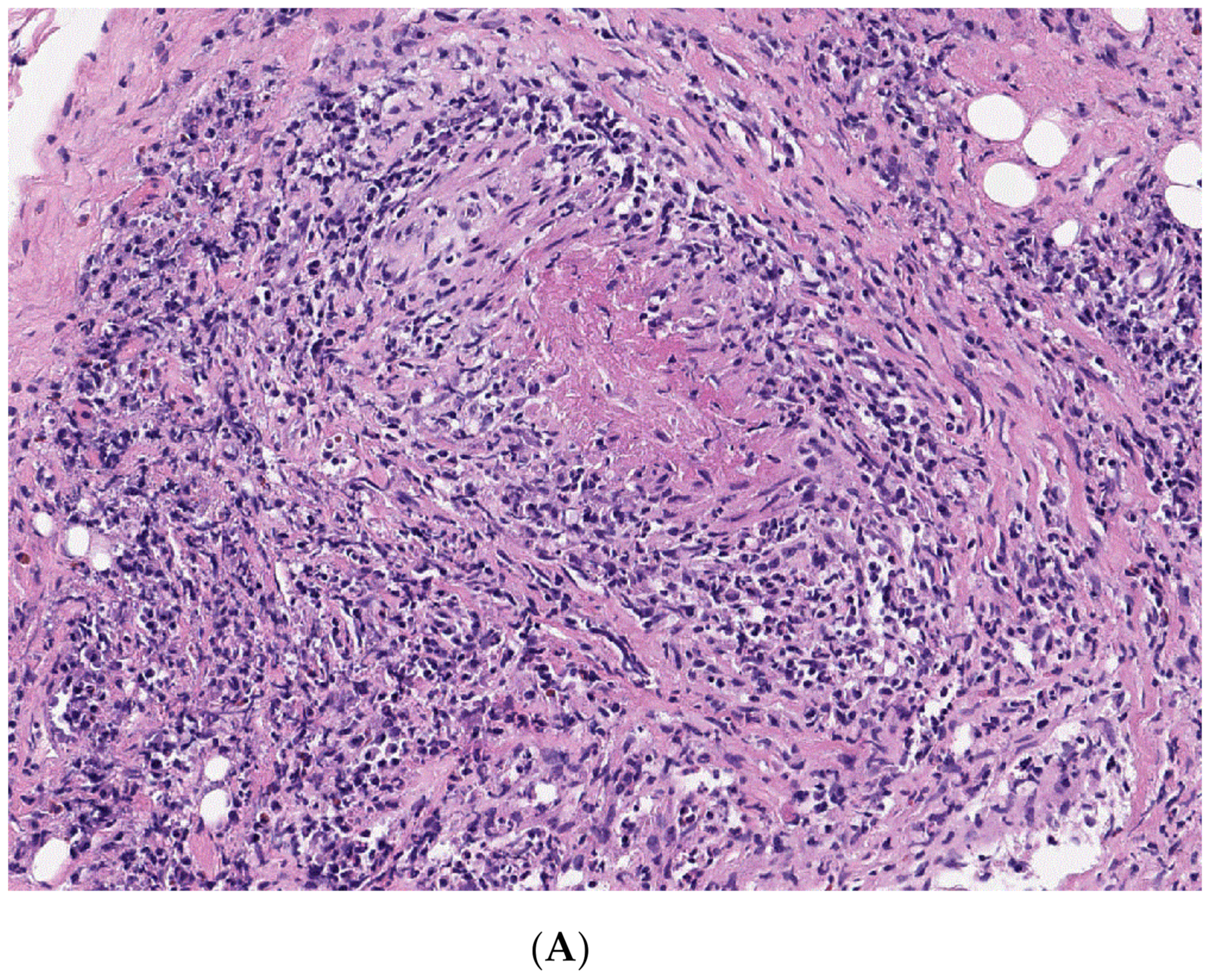
2. Presentation of Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Greco, A.; Marinelli, C.; Fusconi, M.; Macri, G.; Gallo, A.; De Virgilio, A.; Zambetti, G.; De Vincentiis, M. Clinic manifestations in granulomatosis with polyangiitis. Int. J. Immunopathol. Pharmacol. 2015, 29, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, G.S.; Kerr, G.S.; Leavitt, R.Y.; Hallahan, C.W.; Lebovics, R.S.; Rottem, M.; Travis, W.D.; Fauci, A.S. Wegener granulomatosis: An analysis of 158 patients. Ann. Intern. Med. 1992, 116, 488. [Google Scholar] [CrossRef] [PubMed]
- Widdrington, J.D.; Emmerson, I.; Cullinan, M.; Narayanan, M.; Klejnow, E.; Watson, A.; Ong, E.L.C.; Schmid, M.L.; Price, D.A.; Schwab, U.; et al. Duncan Pyogenic Spondylodiscitis: Risk Factors for Adverse Clinical Outcome in Routine Clinical Practice. Med. Sci. 2018, 6, 96. [Google Scholar]
- Jennette, J.C.; Falk, R.J.; Bacon, P.A.; Basu, N.; Cid, M.C.; Ferrario, F.; Flores-Suárez, L.F.; Gross, W.L.; Guillevin, L.; Hagen, E.C.; et al. 2012 revised International Chapel Hill ConsensusConference Nomenclature of Vasculitides. Arthritis Rheum. 2012, 65, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Watts, R.; Lane, S.; Hanslik, T.; Hauser, T.; Hellmich, B.; Koldingsnes, W.; Mahr, A.; Segelmark, M.; Cohen-Tervaert, J.W.; Scott, D. Development and validation of a consensusmethodology for the classification of the ANCA-associated vasculitides and polyarteritis nodosa for epidemiological studies. Ann. Rheum. Dis. 2007, 66, 222–227. [Google Scholar] [CrossRef]
- Bosch, X.; Guilabert, A.; Font, J. Antineutrophil cytoplasmic antibodies. Lancet 2006, 368, 404–418. [Google Scholar] [CrossRef]
- Kallenberg, C.G.; Heeringa, P.; Stegeman, C.A. Mechanisms of disease: Pathogenesis and treatment of ANCA-associated vasculitides. Nat. Clin. Pract. Rheumatol. 2006, 2, 661–670. [Google Scholar] [CrossRef] [PubMed]
- Lutalo, P.M.K.; D’Cruz, D.P. Diagnosis and classification of granulomatosis with polyangiitis (aka Wegener’s granulomatosis). J. Autoimmun. 2014, 48–49, 94–98. [Google Scholar] [CrossRef] [PubMed]
- Fauci, A.S. Wegener’s granulomatosis: Prospective clinical and therapeutic experience with 85 patients for 21 years. Ann. Intern. Med. 1983, 98, 76. [Google Scholar] [CrossRef] [PubMed]
- Puéchal, X. Antineutrophil cytoplasmic antibody-associated vasculitides. Jt. Bone Spine 2007, 74, 427–435. [Google Scholar] [CrossRef] [PubMed]
- Khellaf, M.; Hamidou, M.; Pagnoux, C.; Michel1, M.; Brisseau, J.M.; Chevallier, X.; Cohen, P.; Guillevin, L.; Godeau, B. Vasculitis restricted to the lower limbs: A clinical and histopathological study. Ann. Rheum. Dis. 2007, 66, 554–556. [Google Scholar] [CrossRef] [PubMed]
- Benz, N.; Daikeler, T.; Frank, S.; Mehling, M.; Tyndall, A.; Trendelenburg, M. Three cases of primary small vessel vasculitis of the skeletal muscle-an own entity. BMJ Case Rep. 2011, 20, 2–5. [Google Scholar] [CrossRef] [PubMed]



© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, Y.-M.; Chung, S.W. Granulomatosis with Polyangiitis Restricted to the Back Muscle: The First Case Report. Medicina 2020, 56, 431. https://doi.org/10.3390/medicina56090431
Lee Y-M, Chung SW. Granulomatosis with Polyangiitis Restricted to the Back Muscle: The First Case Report. Medicina. 2020; 56(9):431. https://doi.org/10.3390/medicina56090431
Chicago/Turabian StyleLee, Yu-Mi, and Sang Wan Chung. 2020. "Granulomatosis with Polyangiitis Restricted to the Back Muscle: The First Case Report" Medicina 56, no. 9: 431. https://doi.org/10.3390/medicina56090431
APA StyleLee, Y.-M., & Chung, S. W. (2020). Granulomatosis with Polyangiitis Restricted to the Back Muscle: The First Case Report. Medicina, 56(9), 431. https://doi.org/10.3390/medicina56090431




