Chronic Intradiploic Organizing Hematoma of the Skull Mimicking Calvarial Tumor Diagnosed Using Zero TE MRI: A Case Report and Review of Literature
Abstract
:1. Introduction
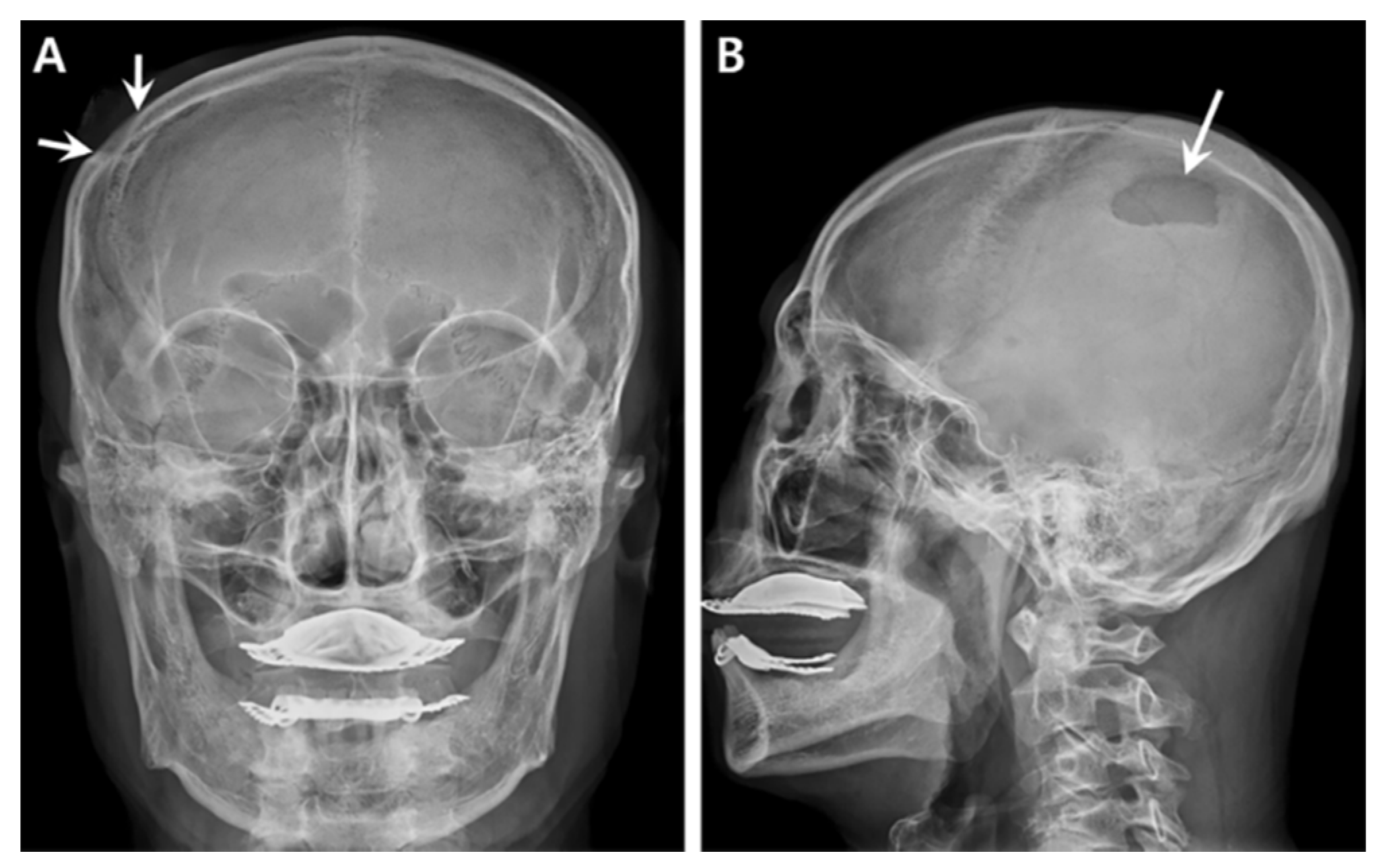
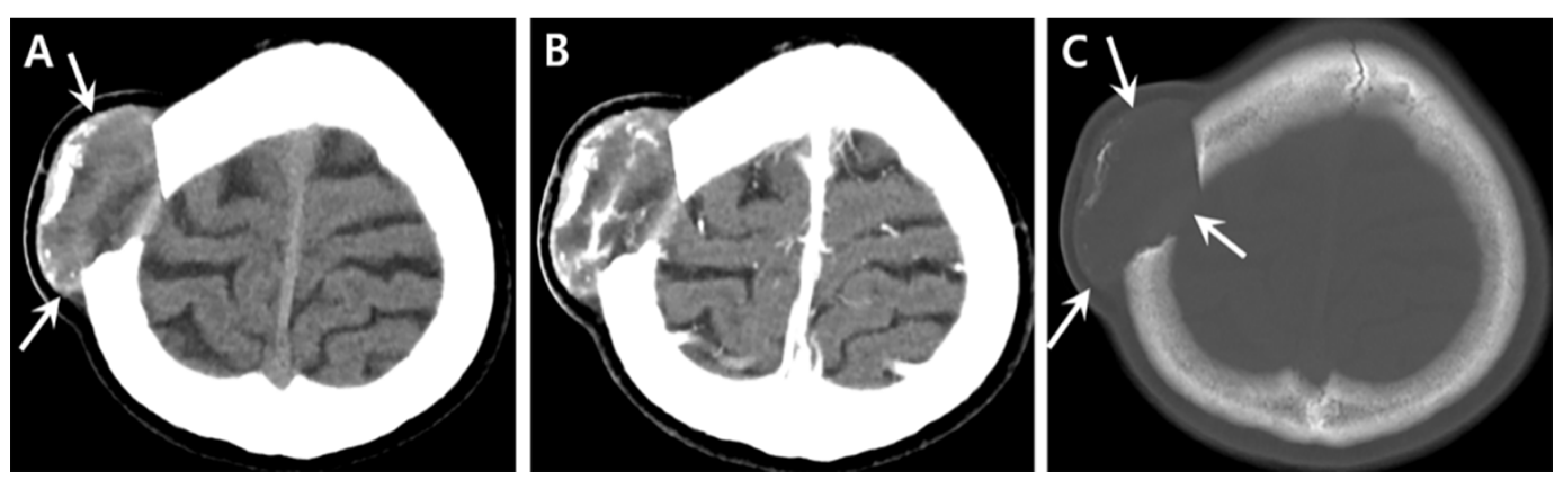
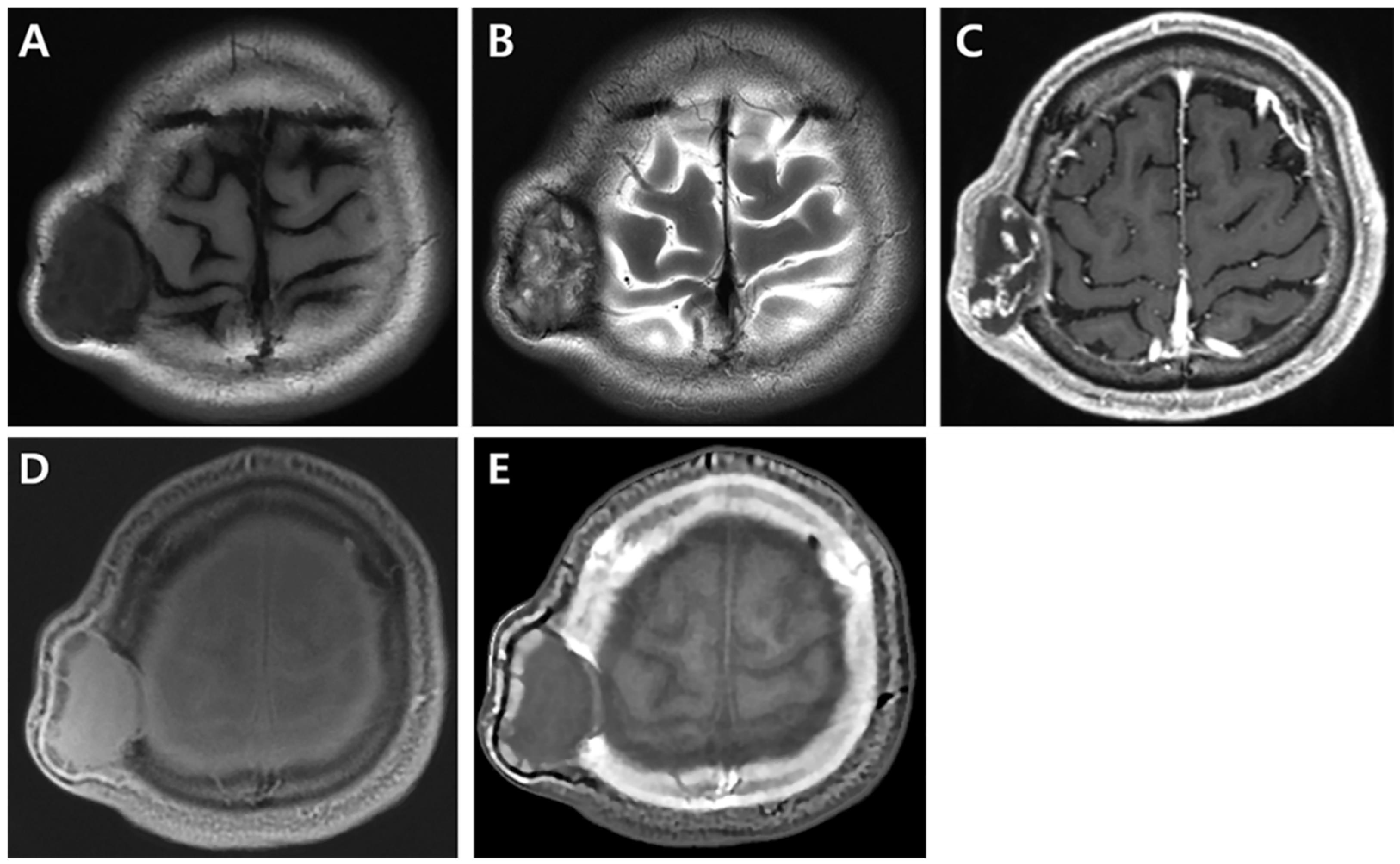
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mobbs, R.J.; Gollapudi, P.R.; Fuller, J.W.; Dahlstrom, J.E.; Chandran, N.K. Intradiploic hematoma after skull fracture: Case report and literature review. Surg. Neurol. 2000, 54, 87–91. [Google Scholar] [CrossRef]
- Sato, K.; Kubota, T.; Kawano, H. Chronic diploic hematoma of the parietal bone. Case report. J. Neurosurg. 1994, 80, 1112–1115. [Google Scholar] [CrossRef] [PubMed]
- Yuasa, H.; Watanabe, H.; Uemura, Y.; Tokito, S. Intraosseous hematoma of the skull: Case report. Neurosurgery 1992, 30, 776–778. [Google Scholar] [CrossRef] [PubMed]
- Uemura, K.; Tsuboi, K.; Nose, T. Intradiploic hematoma. Am. J. Neuroradiol. 1997, 18, 397–398. [Google Scholar] [PubMed]
- Yücesoy, K.; Mertol, T.; Ozer, H.; Ozer, E. An infantile intraosseous hematoma of the skull. Report of a case and review of the literature. Childs Nerv. Syst. 1999, 15, 69–72. [Google Scholar] [CrossRef] [PubMed]
- Goel, A.; Desai, K.; Patil, S. Unusual intradiploic hematoma. J. Neurosurg. 2000, 93, 895–896. [Google Scholar] [CrossRef] [PubMed]
- Nagi, S.; Megdiche, H.; Daoud, H.; Bouchriha, M.; Sebaï, R.; Belghith, L.; Touibi, S. Intradiploic hematoma: Report of two cases and review of literature. Tunis Méd. 2005, 83, 426–428. [Google Scholar] [PubMed]
- Garza-Mercado, R.; Cavazos, E.; Hernández-Batres, F. Giant cell reparative granuloma of the cranial vault: Exceptional bone lesion. Neurosurgery 1984, 15, 228–232. [Google Scholar] [CrossRef] [PubMed]
- Murphey, M.D.; Nomikos, G.C.; Flemming, D.J.; Gannon, F.H.; Temple, H.T.; Kransdorf, M.J. Imaging of giant cell tumor and giant cell reparative granuloma of bone: Radiologic-pathologic correlation. Radiographics 2001, 21, 1283–1309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Batista, G.R.; Oliveira, P.C.R.; Alcantara, F.P.; De Teles, I.G.; Najjar, Y.J.S.; Kalil, R.K. Chronic diploic hematoma mimicking malignancy on imaging. Skelet. Radiol. 2011, 40, 475–479. [Google Scholar] [CrossRef] [PubMed]
- Tokmak, M.; Ozek, E.; Iplikçioğlu, C. Chronic intradiploic hematomas of the skull without coagulopathy: Report of two cases. Neurocirugía 2015, 26, 302–306. [Google Scholar] [CrossRef] [PubMed]
- Bradley, W.G., Jr.; Schmidt, P.G. Effect of methemoglobin formation on the MR appearance of subarachnoid hemorrhage. Radiology 1985, 156, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Bush, C.H. The MRI of musculoskeletal hemorrhage. Skelet. Radiol. 2000, 29, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.B.; Baek, H.J.; Ryu, K.H.; Choi, B.H.; Moon, J.I.; Kim, T.B.; Kim, S.K.; Park, H.; Hwang, M.J. Clinical Feasibility of Zero TE Skull MRI in Patients with Head Trauma in Comparison with CT: A Single-Center Study. Am. J. Neuroradiol. 2019, 40, 109–115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Du, J.; Carl, M.; Bydder, M.; Takahashi, A.; Chung, C.B.; Bydder, G. Qualitative and quantitative ultrashort echo time (UTE) imaging of cortical bone. J. Magn. Reson. 2010, 207, 304–311. [Google Scholar] [CrossRef] [PubMed]
- Sim, K.B.; Hong, S.K. Cranial hemophilic pseudotumor: Case report. Neurosurgery 1996, 39, 1239–1342. [Google Scholar] [CrossRef] [PubMed]
- Amaral, L.; Chiurciu, M.; Almeida, J.R.; Ferreira, N.F.; Mendonça, R.; Lima, S.S. MR imaging for evaluation of lesions of the cranial vault: A pictorial essay. Arquivos de Neuro Psiquiatria 2003, 61, 521–532. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Author/Year | Gender/Age | History of Head Trauma | Clinical Features | Location | Imaging Modality and Findings | Treatment |
|---|---|---|---|---|---|---|
| Yuasa et al., (1992) | M/20 y | Presence (minor trauma) | Incidental scalp swelling | Parietal | Conventional radiography: inner table expansion | Excision and cranioplasty |
| Sato et al., (1994) | M/20 y | Presence (minor trauma) | Incidental scalp swelling | Parietal | * Note.: overall poor image quality
| Excision and cranioplasty |
| Uemura et al., (1999) | M/32 y | Presence (minor trauma) | Intermittent headache | Frontal | * Note.: overall poor image quality
| Excision |
| Yücesoy et al., (1999) | M/25 d | Presence (birth trauma) | Scalp swelling | Parietal | * Note.: overall poor image quality
| Excision |
| Mobbs et al., (2000) | M/3 y | Presence (major trauma) | Non-tender scalp swelling | Parietal | * Note.: incongruent MR images and figures (only T2-weighted and FLAIR images without T1-weighted image)
| Curettage |
| Goel et al., (2000) | M/58 y | Presence (minor trauma) | Swelling and ptosis | Frontal | * Note.: poor image quality of conventional radiography
| Excision |
| Batista et al., (2011) | M/45 y | Presence (recurrent traumas due to epilepsy) | Slow-growing painless mass | Parietal and occipital | * Note.: poor image quality of MRI
| Excision |
| Tokmak et al., (2015) | M/16 y | Presence (minor trauma) | Non-tender scalp swelling | Frontal | * Note.: poor image quality
| Excision |
| M/64 y | Presence (minor trauma) | headache and visual disturbance | Frontal | * Note.: poor image quality
| Curettage |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, H.; Nam, I.C.; Baek, H.J.; Ryu, K.H.; Cho, E.; Kim, S.S.; An, H.J. Chronic Intradiploic Organizing Hematoma of the Skull Mimicking Calvarial Tumor Diagnosed Using Zero TE MRI: A Case Report and Review of Literature. Medicina 2021, 57, 18. https://doi.org/10.3390/medicina57010018
Park H, Nam IC, Baek HJ, Ryu KH, Cho E, Kim SS, An HJ. Chronic Intradiploic Organizing Hematoma of the Skull Mimicking Calvarial Tumor Diagnosed Using Zero TE MRI: A Case Report and Review of Literature. Medicina. 2021; 57(1):18. https://doi.org/10.3390/medicina57010018
Chicago/Turabian StylePark, Hyun, In Chul Nam, Hye Jin Baek, Kyeong Hwa Ryu, Eun Cho, Seung Soo Kim, and Hyo Jung An. 2021. "Chronic Intradiploic Organizing Hematoma of the Skull Mimicking Calvarial Tumor Diagnosed Using Zero TE MRI: A Case Report and Review of Literature" Medicina 57, no. 1: 18. https://doi.org/10.3390/medicina57010018






