1. Introduction
Over the last decades, functional endoscopic sinus surgery (FESS) has become the standard of care in paranasal sinus surgery with significant efficacy in the treatment of sinonasal diseases [
1]. Multiplanar high-resolution computed tomography (CT) not only plays a major role in the diagnostic process, but helps to determine the course of treatment as the images clearly show variants in anatomy and the degree of disease. Moreover, CT scans allow the differentiation of inflammatory, benign, and malignant sinonasal pathologies [
2]. In particular, the identification of potentially dangerous anatomical characteristics, such as the depth of the frontal skull base or the course and bony coverage of the optic nerve and internal carotid artery, are of central importance to minimize the risks of the operation [
3,
4,
5,
6,
7,
8,
9].
A profound understanding of the sinonasal anatomy and its variations is indispensable to safely perform FESS. Preoperative CT scans help to precisely plan a surgical roadmap that highlights any potentially hazardous anatomical features, and by delineating the degree of disease, prevent unneeded dissections in disease-free parts of the paranasal sinuses [
6,
7,
8,
10,
11,
12]. Furthermore, even though understanding of sinonasal pathologies, surgical approaches as well as radiological imaging have undergone an evolution in both content and structure [
13], radiologic reporting has just started to evolve over the course of the past years. Structured reporting (SR) has proven to be an auspicious approach compared to the common practice of free text reporting to standardize the content of reporting and thereby improve the report quality of several diagnostic modalities in otorhinolaryngology that are favored by many physicians [
14,
15,
16,
17,
18,
19,
20,
21,
22,
23]. SR templates containing standardized terminology help to reduce the likelihood of missing key structures [
11] and, consequently, may be of valuable help to improve surgical operation planning (SOP), especially for younger physicians in clinical routines [
24,
25].
The purpose of this study was to analyze the effect of SOP on the learning process of FESS. For this purpose, the quality, the time to plan the FESS procedure, and the user convenience of conventional operation planning (COP) using free text reporting in contrast to the structured operation planning of sinus CTs utilizing a specific SR template, were analyzed in the context of a 4-day FESS immersion course at a university medical center.
2. Materials and Methods
This study was conducted in accordance with the STROBE guidelines [
26]. Due to the design of the study, no approval from the local ethics committee needed to be obtained.
As previously described, the anticipated effect size was used to determine the amount of reports needed for this study. At the significance level of α = 0.05, we set the power to be 80%. Therefore, the necessary number of reports demanded within this study was n = 28 (14 COPs and SOPs, respectively).
During a 4-day annual course on FESS at the university medical center in Tübingen, 15 out of 20 (75%) participating physicians agreed to participate in the study. Gender, level of training (resident or consultant), work environment (medical practice, municipal hospital, or university medical center) and individual level of experience in FESS were evaluated using a five-point visual analogue scale (VAS; 1: no experience; 5: highly experienced) (see
Table 1).
Within the immersion course, all participating residents received training to create COP using free texts prior to performing the tasks. For the study, the subjects were requested to create free-text-based COPs of a previously unknown CT scan of the paranasal sinuses that exhibited common pathological features of a chronic unilateral sinusitis for preoperative FESS evaluation, as they would do in their own work environment. Afterwards, the participants were asked to repeat this task while using a specifically designed SOP template. To create this template, an established SR system (Smart Reporting GmbH, Munich, Germany,
https://www.smart-reporting.com/en/, accessed on 3 October 2021, see
Figure S1) was utilized. The template was developed with consideration of the most recent directives for CT-based planning of FESS procedures. A special focus was set to incorporate relevant anatomical structures, adequate terminology, and a wide range of paranasal sinus diseases, both benign and malignant. Additionally, the template was previously validated in routine clinical use [
25].
Time expenditure to plan the operations in seconds was recorded for each approach. Subsequently, each participant completed a specifically designed questionnaire rating user convenience and usability by means of a ten-point VAS.
Anonymized COP and SOP reports were independently assessed, by two highly experienced FESS surgeons, in terms of the completeness of the identified critical anatomical structures and the determination of the extent of the procedure, in addition to legibility (five graded scale ranging from 1 = poor to 5 = very good), using a specifically designed evaluation checklist.
Data are reported as mean ± standard deviation (SD). To compare assessments of surgical planning and user convenience evaluations, the Wilcoxon signed-rank test for paired nominal data was used, with a p-value of less than 0.05 defined as being statistically significant. All statistical tests were carried out utilizing Prism 9 (GraphPad Software, Inc., San Diego, CA, USA).
3. Results
FESS procedures were planned using COP and SOP by otorhinolaryngologists in training as well as by board-certified otorhinolaryngologists, during a 4-day FESS course at the Department of Otorhinolaryngology, Head and Neck Surgery of the University Hospital of Tübingen, using a previously unknown sinus CT with typical pathologies (chronic unilateral sinusitis). Demographic data and levels of experience of the 15 participating otorhinolaryngologists are shown in
Table 1.
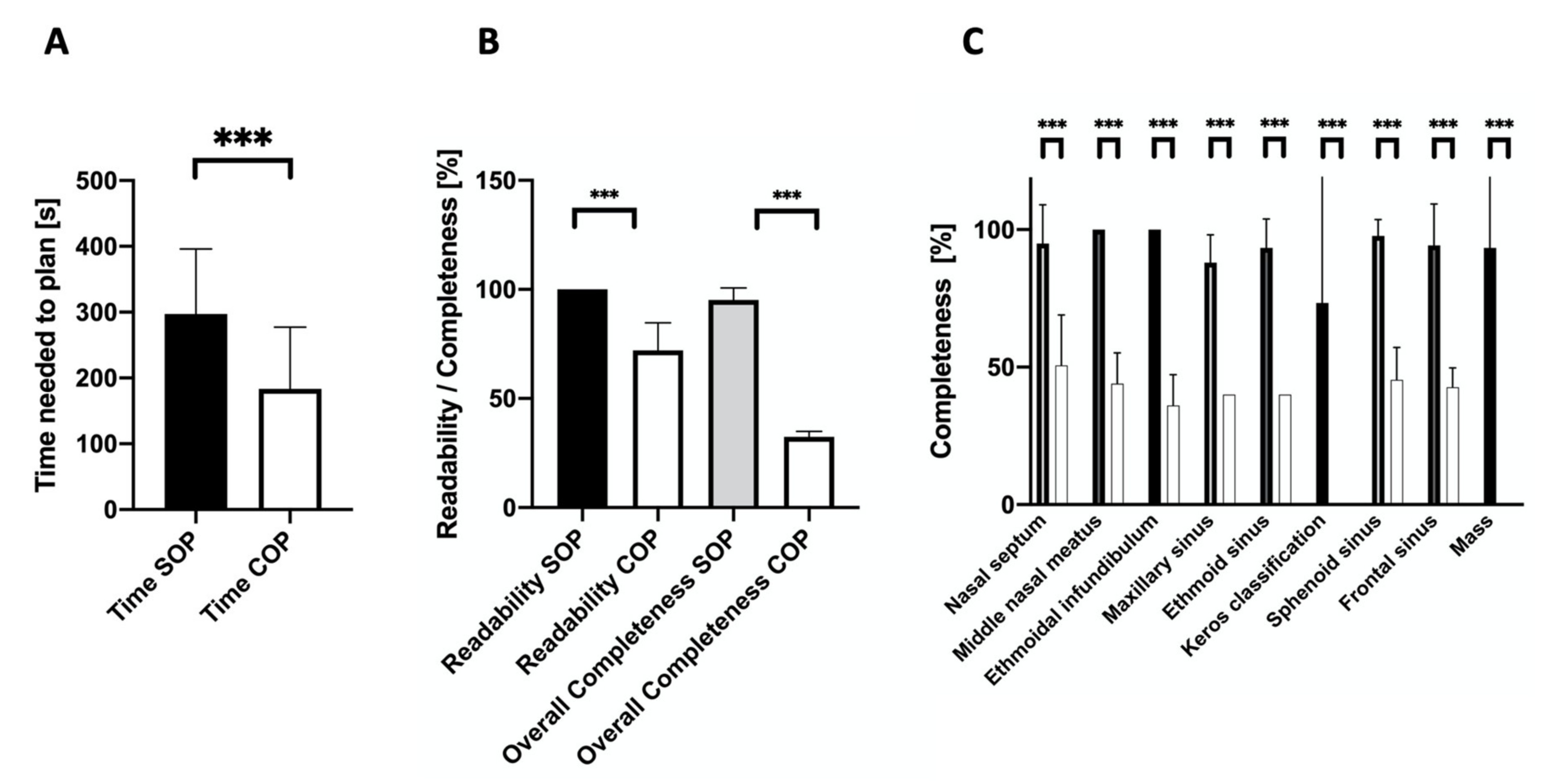
The time expenditure to plan an operation conventionally was significantly shorter than for the respective structured approach (183 s ± 90 vs. 296 s ± 95,
p = 0.0003). Still, SOPs exhibited better legibility (100.0% ± 0 vs. 72.0% ± 12.2,
p < 0.0001) and better overall completeness (95.2% ± 5.3 vs. 32.5% ± 2.4,
p < 0.0001) in comparison to COP (see
Figure 1).
Detailed analysis of completeness findings outlined significantly superior results for SOP compared to COP regarding the nasal septum (95.0% ± 13.5 vs. 50.7% ± 17.7,
p = 0.001), the middle nasal meatus (100.0% ± 0 vs. 44.0% ± 10.8,
p < 0.0001), the ethmoidal infundibulum (100.0% ± 0 vs. 36.0% ± 10.8,
p < 0.0001), the maxillary sinus (88.0% ± 9.8 vs. 40.0% ± 0,
p < 0.0001), the ethmoidal sinuses (93.3% ± 10.2 vs. 40.0% ± 0,
p < 0.0001), the sphenoid sinus (97.7% ± 5.7 vs. 45.3% ± 11.5,
p < 0.0001), and the frontal sinus (94.3% ± 14.6 vs. 42.7% ± 6.8,
p < 0.0001). Potentially existing masses within the paranasal sinuses (93.3% ± 24.9 vs. 0%,
p = 0.0001), as well as the depth of the anterior skull base and olfactory fossa (73.3% ± 44.2 vs. 0%,
p = 0.001), measured using the Keros classification, were only considered using SOP (see
Figure 1).
The user convenience analysis, conducted via a VAS-based questionnaire, showed a significant overall preference for SOPs by all participating otorhinolaryngologists (7.9 ± 1.9 vs. 6.9 ± 3.2,
p = 0.0185). Although detailed analysis for usefulness (8.0 ± 1.2 vs. 7.7 ± 2.9,
p = 0.97), usability in everyday practice (8.3 ± 1.2 vs. 7.3 ± 2.9,
p = 0.35), and improvement of the quality of preoperative planning (8.1 ± 1.7 vs. 6.9 ± 3.2,
p = 0.12) showed a tendency towards SOP, these tendencies were not statistically significant. The same applied to the question of whether SOP can save time in the preoperative workup (6.1 ± 2.8 vs. 5.2 ± 3.0,
p = 0.4) and if the additional time is justified (8.0 ± 0.9 vs. 7.2 ± 3.2,
p = 0.53), as well as whether SOP supports unexperienced surgeons in their learning progress (9.2 ± 0.9 vs. 7.3 ± 3.4,
p = 0.11). A graphical illustration of the results of the questionnaire is provided in
Figure 2.
All participants stated that the software for creating SOPs was intuitive, easy to navigate, and easy to learn.
4. Discussion
Precise evaluation of preoperative CT scans and step-by-step planning of the FEES procedure is necessary to achieve good operative long-term results on the one hand and to avoid complications due to overseen anatomical variants on the other hand. Although surgical techniques and equipment have undergone tremendous developments, structured operation planning based on sinus CT-scans by the surgeons themselves has so far not been comprehensively investigated [
27,
28]. This is remarkable because structured, detailed planning of surgical procedures can boost the learning curve and can also increase the confidence of younger physicians in training [
29,
30].
Therefore, the current study evaluated the time expenditure, legibility, completeness, and user convenience of COP in contrast to SOP. The study population consisted of participants of an annual 4-day FESS course at the Department of Otorhinolaryngology, Head and Neck Surgery of the University Hospital of Tübingen, all of whom had been working in the field of ENT for a minimum of 3 years and estimated their expertise in sinus surgery to be average. All of the participants had already assisted in FESS operations and almost half of them had already performed FESS themselves under supervision. Consequently, a profound knowledge on the reporting of sinus CT scans, and also on the planning of FESS procedures, could be presumed. Furthermore, all participants received a special training in sinus CT reporting as part of the course before enrolling in the study.
The time needed to create COP was less than for SOP (COP 183 s vs. SOP 297 s, p < 0.0001). This aspect inversely correlated with the completeness of findings in the participants’ reports, which was higher in SOP (95.2% ± 5.3 vs. 32.5% ± 2.4, p < 0.0001).
The increased time expenditure in SOP is concordant with the studies of Sluijter and Ernst et al., which showed a decrease in time-efficiency following the implementation of SR [
23,
31]. One reason for this finding in our study may be due to the short duration of training of the participants in the usage of the SR template and the underlying software. One aspect that could be observed during the creation of the SOP by the participants was that even though they had already seen the CT scan of the patient, which was necessary to produce the COP, they checked on it again, specifically and more thoroughly, prior to producing the SOP. Classifications of anatomical findings such as the length of the lateral cribriform lamella (Keros classification) were not mentioned by any of the participants when using COP, but by nearly three-quarters of participants when using SOP. This may have had an even greater impact on the time to complete the task. In consequence, SOP took more time but yielded a higher completeness of findings according to the results of our evaluation. The increase in reporting quality has already been shown in several studies and seems to be one of the main advantages in SR over free text reporting [
14,
15,
16,
17,
19,
23,
31]. In particular, the decrease in the variability of reports of the same findings is of central interest in the context of quality assurance, scientific data analysis, and medical education. This effect may be explained by the structured procedure in which the reporting physician is guided through the relevant anatomy by the underlying decision tree. In addition, it supports inexperienced physicians through the standardization of language and the description of specific pathologies, which may potentially increase the inter-rater-reliability of SOP [
20]. In consequence, the use of SOP may promote information extraction and enhance clinical decision-making. Additionally, there is evidence that a structured approach may reduce interobserver variability [
16,
17,
19]. The COVER survey supports this aspect and states that clinicians welcome the implementation of structured documentation [
21]. Additionally, the American Society of Radiology, the Radiological Society of Northern America, as well as the European Society of Radiology have started action groups to advance SR over the past years [
18,
32,
33].
The template utilized in this study was developed, with the collaboration of otorhinolaryngologists and radiologists with high levels of expertise in the diagnosis and treatment of sinonasal diseases, to promote user-friendliness [
27]. The evaluation of SOP by a user-convenience questionnaire revealed very high ratings and the participants evaluated SOP as a very valuable tool for clinical routines. This finding is supported by previous publications showing that clinicians prefer SR over free text reporting [
14,
15,
16,
19,
23,
34,
35,
36]. Considering the fact that performing FESS requires a trainee surgeon to not only develop new manual dexterity skills, but also to possess a thorough anatomic understanding with spatial orientation [
37,
38,
39], SOP may become a very valuable tool in the training of younger FESS surgeons by offering a systematic and standardized approach to operation planning [
14].
The findings of the study are limited due to the small number of planning procedures. Every participant conducted only one COP and SOP; therefore, time to complete could have been shorter for both options after repeated accomplishment. Bias due to feedback from the template itself was minimized by scheduling COP before SOP. Nevertheless, there was a residual risk of bias due to learning or testing effects.
5. Conclusions
Implementation of a structured approach in operation planning may be a valuable tool in the training process of FESS. Further studies with a larger number of CT examinations are necessary to place the preliminary findings of our study within a broader perspective. In detail, a thorough investigation of the time expenditure required to produce SOP and, therefore, of its time-efficiency, in a population that was not previously trained in COP, will be of great interest to determine the impact of SOP on the learning process.
Author Contributions
Conception and design: S.B., P.G., B.P.E., M.H. (Magnus Haas), M.S., M.F.F., C.B., H.L., B.H., W.H.S. and M.H. (Martin Holderried). Data collection: S.B., P.G., B.P.E., M.H. (Magnus Haas), M.S., M.F.F., C.B., H.L., B.H., W.H.S. and M.H. (Martin Holderried). Data analysis and interpretation: S.B., P.G. and B.P.E. Draft of manuscript: S.B., P.G. and B.P.E. All authors conducted critical revisions of the manuscript, gave final approval to the submitted paper and agreed to be accountable for all aspects of the work. All authors have read and agreed to the published version of the manuscript.
Funding
This study did not receive any funding.
Institutional Review Board Statement
No approval by the local Ethical Committee of the University of Tübingen was needed to perform the study. The study is in accordance with national law and the World Medical Association Declaration of Helsinki (1964) with its ethical principles for medical research involving Human Subjects and subsequent amendments.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. All subjects were physicians. No patient data are published.
Data Availability Statement
All the data are available from the corresponding author upon reasonable request.
Acknowledgments
The authors thank the attendees of the 2019 Tübingen course on functional endoscopic sinus surgery for their participation in this study.
Conflicts of Interest
Wieland H. Sommer is the founder and CEO and Matthias F. Froelich is a medical consultant of the company Smart Reporting GmbH, which hosts an online platform for structured reporting. The other authors of this manuscript have no conflict of interest.
References
- Baban, M.I.A.; Mirza, B.; Castelnuovo, P. Radiological and endoscopic findings in patients undergoing revision endoscopic sinus surgery. Surg. Radiol. Anat. 2020, 42, 1003–1012. [Google Scholar] [CrossRef] [PubMed]
- Kandukuri, R.; Phatak, S. Evaluation of Sinonasal Diseases by Computed Tomography. J. Clin. Diagn. Res. 2016, 10, TC09–TC12. [Google Scholar] [CrossRef] [PubMed]
- Grevers, G. Anterior skull base trauma during endoscopic sinus surgery for nasal polyposis preferred sites for iatrogenic injuries. Rhinology 2001, 39, 1–4. [Google Scholar] [PubMed]
- Wu, H.; Shen, T.; Chen, J.; Yan, J. Long-term therapeutic outcome of ophthalmic complications following endoscopic sinus surgery. Medicine 2016, 95, e4896. [Google Scholar] [CrossRef]
- Lum, S.G.; Gendeh, B.S.; Husain, S.; Gendeh, H.S.; Ismail, M.R.; Toh, C.J.; Izaham, A.; Tan, H.J. Internal carotid artery injury during endonasal sinus surgery: Our experience and review of the literature. Acta Otorhinolaryngol. Ital. 2019, 39, 130–136. [Google Scholar] [CrossRef]
- Jaworek-Troc, J.; Walocha, J.A.; Loukas, M.; Tubbs, R.S.; Iwanaga, J.; Zawilinski, J.; Brzegowy, K.; Zarzecki, J.J.; Curlej-Wadrzyk, A.; Kucharska, E.; et al. Extensive pneumatisation of the sphenoid bone—Anatomical investigation of the recesses of the sphenoid sinuses and their clinical importance. Folia Morphol. 2020. [Google Scholar] [CrossRef]
- Jaworek-Troc, J.; Walocha, J.A.; Skrzat, J.; Iwanaga, J.; Tubbs, R.S.; Mazur, M.; Lipski, M.; Curlej-Wadrzyk, A.; Gladysz, T.; Chrzan, R.; et al. A computed tomography comprehensive evaluation of the ostium of the sphenoid sinus and its clinical significance. Folia Morphol. 2021. [Google Scholar] [CrossRef]
- Tesfaye, S.; Hamba, N.; Gerbi, A.; Negeri, Z. Radio-anatomic variability in sphenoid sinus pneumatization with its relationship to adjacent anatomical structures and their impact upon reduction of complications following endonasal transsphenoidal surgeries. Transl. Res. Anat. 2021, 24, 100126. [Google Scholar] [CrossRef]
- Jaworek-Troć, J.; Iwanaga, J.; Chrzan, R.; Zarzecki, J.J.; Żmuda, P.; Pękala, A.; Tomaszewska, I.M.; Tubbs, R.S.; Zawiliński, J.; Zarzecki, M.P. Anatomical variations of the main septum of the sphenoidal sinus and its importance during transsphenoidal approaches to the sella turcica. Transl. Res. Anat. 2020, 21, 100079. [Google Scholar] [CrossRef]
- Vaid, S.; Vaid, N.; Rawat, S.; Ahuja, A.T. An imaging checklist for pre-FESS CT: Framing a surgically relevant report. Clin. Radiol. 2011, 66, 459–470. [Google Scholar] [CrossRef]
- White, P.S.; Maclennan, A.C.; Connolly, A.A.; Crowther, J.; Bingham, B.J. Analysis of CT scanning referrals for chronic rhinosinusitis. J. Laryngol. Otol. 1996, 110, 641–643. [Google Scholar] [CrossRef]
- Varshney, H.; Varshney, J.; Biswas, S.; Ghosh, S.K. Importance of CT Scan of Paranasal Sinuses in the Evaluation of the Anatomical Findings in Patients Suffering from Sinonasal Polyposis. Indian J. Otolaryngol. Head Neck Surg. 2016, 68, 167–172. [Google Scholar] [CrossRef] [Green Version]
- Reiner, B.I. The challenges, opportunities, and imperative of structured reporting in medical imaging. J. Digit. Imaging 2009, 22, 562–568. [Google Scholar] [CrossRef] [Green Version]
- Ernst, B.P.; Strieth, S.; Katzer, F.; Hodeib, M.; Eckrich, J.; Bahr, K.; Rader, T.; Künzel, J.; Froelich, M.F.; Matthias, C.; et al. The use of structured reporting of head and neck ultrasound ensures time-efficiency and report quality during residency. Eur. Arch. Otorhinolaryngol. 2020, 277, 269–276. [Google Scholar] [CrossRef]
- Ernst, B.P.; Katzer, F.; Künzel, J.; Hodeib, M.; Strieth, S.; Eckrich, J.; Tattermusch, A.; Froelich, M.F.; Matthias, C.; Sommer, W.H.; et al. Impact of structured reporting on developing head and neck ultrasound skills. BMC Med. Educ. 2019, 19, 102. [Google Scholar] [CrossRef] [Green Version]
- Schoeppe, F.; Sommer, W.H.; Norenberg, D.; Verbeek, M.; Bogner, C.; Westphalen, C.B.; Dreyling, M.; Rummeny, E.J.; Fingerle, A.A. Structured reporting adds clinical value in primary CT staging of diffuse large B-cell lymphoma. Eur. Radiol. 2018, 28, 3702–3709. [Google Scholar] [CrossRef]
- Schoeppe, F.; Sommer, W.H.; Haack, M.; Havel, M.; Rheinwald, M.; Wechtenbruch, J.; Fischer, M.R.; Meinel, F.G.; Sabel, B.O.; Sommer, N.N. Structured reports of videofluoroscopic swallowing studies have the potential to improve overall report quality compared to free text reports. Eur. Radiol. 2018, 28, 308–315. [Google Scholar] [CrossRef]
- Morgan, T.A.; Helibrun, M.E.; Kahn, C.E., Jr. Reporting initiative of the Radiological Society of North America: Progress and new directions. Radiology 2014, 273, 642–645. [Google Scholar] [CrossRef] [PubMed]
- Marcovici, P.A.; Taylor, G.A. Journal Club: Structured radiology reports are more complete and more effective than unstructured reports. AJR Am. J. Roentgenol. 2014, 203, 1265–1271. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, L.H.; Panicek, D.M.; Berk, A.R.; Li, Y.; Hricak, H. Improving communication of diagnostic radiology findings through structured reporting. Radiology 2011, 260, 174–181. [Google Scholar] [CrossRef] [Green Version]
- Bosmans, J.M.; Peremans, L.; De Schepper, A.M.; Duyck, P.O.; Parizel, P.M. How do referring clinicians want radiologists to report? Suggestions from the COVER survey. Insights Imaging 2011, 2, 577–584. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, A.J.; Chen, M.Y.; Zapadka, M.E.; Lyders, E.M.; Littenberg, B. Radiology report clarity: A cohort study of structured reporting compared with conventional dictation. J. Am. Coll. Radiol. 2010, 7, 501–506. [Google Scholar] [CrossRef] [PubMed]
- Ernst, B.P.; Hodeib, M.; Strieth, S.; Künzel, J.; Bischof, F.; Hackenberg, B.; Huppertz, T.; Weber, V.; Bahr, K.; Eckrich, J.; et al. Structured reporting of head and neck ultrasound examinations. BMC Med. Imaging 2019, 19, 25. [Google Scholar] [CrossRef] [PubMed]
- Ernst, B.P.; Strieth, S.; Künzel, J.; Hodeib, M.; Katzer, F.; Eckrich, J.; Bahr, K.; Matthias, C.; Sommer, W.H.; Froelich, M.F.; et al. Evaluation of optimal education level to implement structured reporting into ultrasound training. Med. Ultrason. 2020, 22, 445–450. [Google Scholar] [CrossRef] [PubMed]
- Adibelli, Z.H.; Unal, G.; Gul, E.; Uslu, F.; Kocak, U.; Abali, Y. Differentiation of benign and malignant cervical lymph nodes: Value of B-mode and color Doppler sonography. Eur. J. Radiol. 1998, 28, 230–234. [Google Scholar] [CrossRef]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13, S31–S34. [Google Scholar] [CrossRef]
- Ernst, B.P.; Reissig, M.R.; Strieth, S.; Eckrich, J.; Hagemann, J.H.; Döge, J.; Matthias, C.; Gouveris, H.; Rübenthaler, J.; Weiss, R.; et al. The role of structured reporting and structured operation planning in functional endoscopic sinus surgery. PLoS ONE 2020, 15, e0242804. [Google Scholar] [CrossRef]
- Khanna, A.; Sama, A. New instrumentations in the operating room for sinus surgery. Curr. Opin. Otolaryngol. Head Neck Surg. 2018, 26, 13–20. [Google Scholar] [CrossRef]
- Hey, S.Y.; Koo Ng, N.K.F.; McGarry, G.W. Endoscopic Sphenopalatine Artery Ligation: General Applicability in a Teaching Unit. Ear Nose Throat J. 2019, 98, 85–88. [Google Scholar] [CrossRef] [Green Version]
- Mladina, R.; Skitarelic, N.; Cingi, C.; Chen, L.; Bayar Muluk, N. The Validity of Training Endoscopic Sinus and Skull Base Surgery Techniques on the Experimental Head Model. J. Craniofac. Surg. 2018, 29, 498–501. [Google Scholar] [CrossRef]
- Sluijter, C.E.; van Lonkhuijzen, L.R.; van Slooten, H.J.; Nagtegaal, I.D.; Overbeek, L.I. The effects of implementing synoptic pathology reporting in cancer diagnosis: A systematic review. Virchows Arch. 2016, 468, 639–649. [Google Scholar] [CrossRef] [Green Version]
- Dunnick, N.R.; Langlotz, C.P. The radiology report of the future: A summary of the 2007 Intersociety Conference. J. Am. Coll. Radiol. 2008, 5, 626–629. [Google Scholar] [CrossRef]
- European Society of Radiology (ESR). Good practice for radiological reporting. Guidelines from the European Society of Radiology (ESR). Insights Imaging 2011, 2, 93–96. [Google Scholar] [CrossRef] [Green Version]
- Norenberg, D.; Sommer, W.H.; Thasler, W.; D’Haese, J.; Rentsch, M.; Kolben, T.; Schreyer, A.; Rist, C.; Reiser, M.; Armbruster, M. Structured Reporting of Rectal Magnetic Resonance Imaging in Suspected Primary Rectal Cancer: Potential Benefits for Surgical Planning and Interdisciplinary Communication. Investig. Radiol. 2017, 52, 232–239. [Google Scholar] [CrossRef]
- Brook, O.R.; Brook, A.; Vollmer, C.M.; Kent, T.S.; Sanchez, N.; Pedrosa, I. Structured reporting of multiphasic CT for pancreatic cancer: Potential effect on staging and surgical planning. Radiology 2015, 274, 464–472. [Google Scholar] [CrossRef]
- Gassenmaier, S.; Armbruster, M.; Haasters, F.; Helfen, T.; Henzler, T.; Alibek, S.; Pforringer, D.; Sommer, W.H.; Sommer, N.N. Structured reporting of MRI of the shoulder—Improvement of report quality? Eur. Radiol. 2017, 27, 4110–4119. [Google Scholar] [CrossRef]
- Bakker, N.H.; Fokkens, W.J.; Grimbergen, C.A. Investigation of training needs for functional endoscopic sinus surgery (FESS). Rhinology 2005, 43, 104–108. [Google Scholar]
- Braun, T.; Betz, C.S.; Ledderose, G.J.; Havel, M.; Stelter, K.; Kuhnel, T.; Strauss, G.; Waschke, J.; Kirchner, T.; Briner, H.R.; et al. Endoscopic sinus surgery training courses: Benefit and problems—A multicentre evaluation to systematically improve surgical training. Rhinology 2012, 50, 246–254. [Google Scholar] [CrossRef] [Green Version]
- Burge, S.D.; Bunegin, L.; Weitzel, E.K.; McMains, K.C. The validation of an endoscopic sinus surgery skills training model: A pilot study. Am. J. Rhinol. Allergy 2012, 26, 409–413. [Google Scholar] [CrossRef]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).