Vojta Therapy in Neuromotor Development of Pediatrics Patients with Periventricular Leukomalacia: Case Series
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Objective
2.3. Study Population
2.4. Selection Criteria. Inclusion and Exclusion
- A medical diagnosis of periventricular leukomalacia.
- Age: 0 months–4 years.
- Maturational delay.
- >4 years old.
- Other associated pathologies are not related to periventricular leukomalacia.
- No maturational delay.
2.5. Description of Patients
- PATIENT 1: preterm male patient, age 21 months, corrected age 19 months. Birth weight 1398 kg. He came for consultation at ten months of age, corrected age seven months. He was diagnosed with periventricular leukomalacia. Diagnostic tests: cranial MRI (asymmetric ventricular system with dilatation of both lateral ventricles, more on the right, due to atrophy of the periventricular white matter about leukomalacia). Hyperintense areas in T1, hypointense in T2, and a signal drop in gradient echo sequences related to old hemorrhagic foci. Atrophy of the corpus callosum. All related to hypoxic-ischemic encephalopathy of prematurity.
- PATIENT 2: preterm male patient, 49 months, corrected age 36 months. He came for consultation at 36 months of age, corrected age to 33 months. Birth weight was 1750 kg. He was diagnosed with periventricular leukomalacia. On cranial MRI: bilateral periventricular leukomalacia, especially on the left, approximately 20 × 8 mm sagittal, and AP, the right is smaller, about 10 mm sagittal. Third ventricle and lateral ventricles of standard size and morphology.
- PATIENT 3: premature male patient, 47 months old, corrected age 45 months. He came for consultation at 33 months of age, corrected age to 31 months. Birth weight 1260 kg. Diagnosed with periventricular leukomalacia. Cranial MRI: periventricular leukomalacia, with increased frontal subarachnoid space. Third ventricle and lateral ventricles of normal size and morphology.
2.6. Intervention
2.7. Evaluation
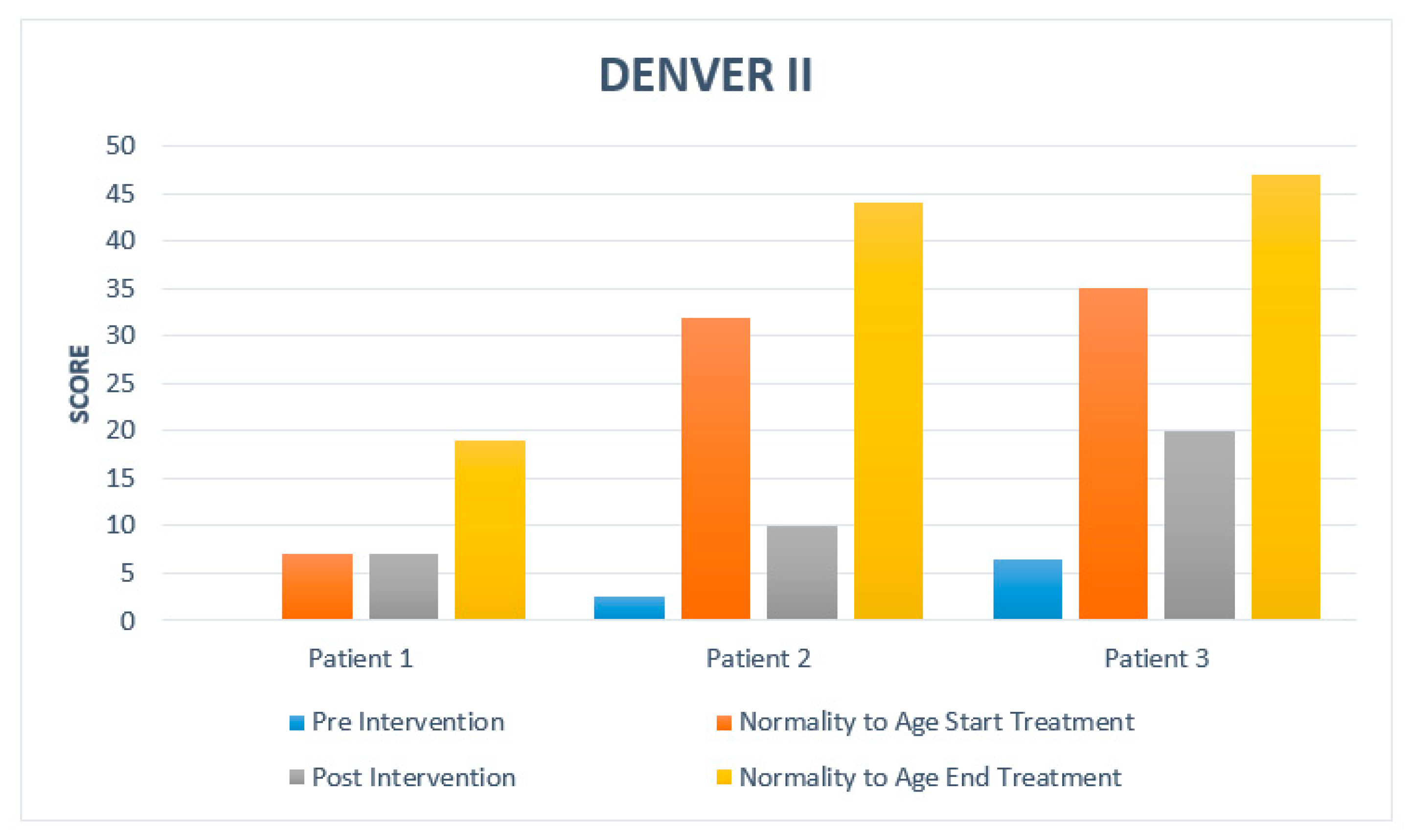
- Denver Developmental Screening Test II (DDST) [14]: The Denver Developmental Screening Test is one of the most widely used instruments to examine children’s developmental progress from birth to 6 years of age. It helps detect possible developmental problems, confirming suspected issues with objective measurement, and monitoring children at risk for developmental problems. Norms indicate when 25%, 50%, 75%, and 90% of children pass each task. Developmental assessment is based on the child’s performance and parent reports in four areas of functioning, fine motor, gross motor, personal-social, and language ability. The child’s exact age is calculated and marked on the assessment sheet, all those tasks that are intersected by the age line are assessed. The score is determined depending on whether the child’s response falls within or outside the expected normal range of success on each task for the age. The number of tasks on which the child falls below the expected range determines whether the child is classified as usual, suspect, or delayed.
- Bayley Scale of Infant Development (BSID) [15]: is a test that evaluates the child’s development in early childhood, from one month to three and a half years of age. With it, we can assess the cognitive, motor, and behavioral levels. Given the subject of the study, the assessment of the motor part has been carried out, this part of the BSID assesses the degree of body control, large muscle coordination, finer manipulatory skills of the hands and fingers, dynamic movement, postural imitation, and the ability to recognize objects by sense of touch. Specifically, items 19 to 50 have been taken as a reference to the capacities and ages of the patients. The aim is to detect motor development delays and act immediately to reduce damage to the central nervous system through cerebral neuroplasticity.
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rogers, B.; Msall, M.; Owens, T.; Guernsey, K.; Brody, A.; Buck, G.; Hudak, M. Cystic periventricular leukomalacia and type of cerebral palsy in preterm infants. J. Pediatr. 1994, 125, S1–S8. [Google Scholar] [CrossRef]
- Al Tawil, K.I.; El Mahdy, H.S.; Al Rifai, M.T.; Tamim, H.M.; Ahmed, I.A.; Al Saif, S.A. Risk Factors for Isolated Periventricular Leukomalacia. Pediatr. Neurol. 2012, 46, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Romero-Guzman, G.J.; Lopez-Munoz, F. Prevalencia y factores de riesgo de leucomalacia periventricular en recien nacidos prematuros. Revision sistematica [Prevalence and risk factors for periventricular leukomalacia in preterm infants. A systema-tic review]. Rev. Neurol. 2017, 65, 57–62. (In Spanish) [Google Scholar] [PubMed]
- Armstrong, D.; Norman, M.G. Periventricular leucomalacia in neonates: Complications and sequelae. Arch. Dis. Child. 1974, 49, 367–375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mulas, F.; Smeyers, P.; De Meneses, M.T.; Menor, F. Periventricular leukomalacia: Neurological and radiological sequelae and long term neuropsychological repercussions. Rev. Neurol. 2000, 31, 243–252. [Google Scholar] [PubMed]
- Vojta, V.; Shweizer, E. The Discovery of Ideal Motor Skills; Editorial Morata: Madrid, Spain, 2011; ISBN 978-84-7112-646-7. [Google Scholar]
- Hok, P.; Opavský, J.; Kutín, M.; Tüdös, Z.; Kaňovský, P.; Hluštík, P. Modulation of the sensorimotor system by sustained manual pressure stimulation. Neuroscience 2017, 348, 11–22. [Google Scholar] [CrossRef] [PubMed]
- Sanz-Esteban, I.; Lobo, C.C.; Rios-Lago, M.; Álvarez-Linera, J.; Muñoz-García, D.; Rodríguez-Sanz, D. Mapping the human brain during a specific Vojta’s tactile input. Medicine 2018, 97, e0253. [Google Scholar] [CrossRef] [PubMed]
- Gajewska, E.; Huber, J.; Kulczyk, A.; Lipiec, J.; Sobieska, M. An attempt to explain the Vojta therapy mechanism of action using the surface polyelectromyography in healthy subjects: A pilot study. J. Bodyw. Mov. Ther. 2018, 22, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Czajkowska, M.; Fonfara, A.; Królak-Olejnik, B.; Michnikowski, M.; Gólczewski, T. The impact of early therapeutic intervention on the central pattern generator in premature newborns—A preliminary study and literature review. Dev. Period Med. 2019, 23, 178–183. [Google Scholar] [PubMed]
- Dwornik, M.; Kiebzak, W.; Żurawski, A. Vojta method in the treatment of developmental hip dysplasia—A case report. Ther. Clin. Risk Manag. 2016, 12, 1271–1276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andrzejewska, M.; Sutkowska, E.; Kuciel, N. The rehabilitation of a child with a sotos syndrome. case report. Wiad. Lek. 2018, 71, 1849–1853. (In Polish) [Google Scholar] [PubMed]
- Ha, S.-Y.; Sung, Y.-H. Effects of Vojta approach on diaphragm movement in children with spastic cerebral palsy. J. Exerc. Rehabil. 2018, 14, 1005–1009. [Google Scholar] [CrossRef] [PubMed]
- Frankenburg, W.K.; Dodds, J.; Archer, P.; Shapiro, H.; Bresnick, B. The Denver II: A major revision and restandardization of the Denver Developmental Screening Test. Pediatrics 1992, 89, 91–97. [Google Scholar] [PubMed]
- Rodríguez, M.; Calderón, L.; Cabrera, L.; Ibarra, N.; Moya, P.; Faas, A.E. Internal Consistency Analysis of the Bayley Child Development Scale for the City of Córdoba (First Year of Life). Laboratory of Psychological and Educational Evaluation. Faculty of Psychology. National University of Cordoba (Argentina) ISSN 1515-1867. Available online: https://revistas.unc.edu.ar/index.php/revaluar/article/view/540 (accessed on 1 September 2021).
- Bauer, H.; Appaji, G.; Mundt, D. VOJTA neurophysiologic therapy. Indian J. Pediatr. 1992, 59, 37–51. [Google Scholar] [CrossRef] [PubMed]
- Vojta, V. Infantile Brain Motor Disorders. Early Diagnosis and Treatment; Editorial Morata: Madrid, Spain, 2004; ISBN 84-7112-496-3. [Google Scholar]
- Adolph, K.E.; Hoch, J.E. Motor development; Embodied, Embedded, Enculturated and enabling. Ann. Rev. Psychol. 2019, 70, 141–164. [Google Scholar] [CrossRef] [PubMed]
- Cioni, G.; Sgandurra, G. Normal psychomotor development. Handb. Clin. Neurol. 2013, 111, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Lim, H.; Kim, T. Effects of Vojta Therapy on Gait of Children with Spastic Diplegia. J. Phys. Ther. Sci. 2013, 25, 1605–1608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jung, M.W.; Landenberger, M.; Jung, T.; Lindenthal, T.; Philippi, H. Vojta therapy and neurodevelopmental treatment in children with infantile postural asymmetry: A randomised controlled trial. J. Phys. Ther. Sci. 2017, 29, 301–306. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| No. Patient | Medical Diagnosis | Date of Birth | Age Corrected End of Treatment | Age Corrected Start of Treatment | Birth Weight | Sex |
|---|---|---|---|---|---|---|
| 1 | Leukomalacia | 20 January 2019 | 19 months | 7 months | 1398 Kg | Male |
| 2 | Leukomalacia | 8 October 2016 | 44 months | 32 months | 1750 Kg | Male |
| 3 | Leukomalacia | 26 December 2016 | 47 months | 35 months | 1260 Kg | Male |
| No. Patient | 1st Evaluation | Last Evaluation | Number of Sessions |
|---|---|---|---|
| 1 | 18 November 2019 | 11 November 2020 | 53 |
| 2 | 25 November 2019 | 12 November 2020 | 52 |
| 3 | 30 October 2019 | 19 November 2020 | 59 |
| No. Patient | Age Start Treatment | Age End of Treatment | DENVER II Pre | DENVER II Post | Bayley Scale Pre | Bayley Scale Post |
|---|---|---|---|---|---|---|
| 1 | 7 | 19 | 0 months | 7 months | 0 | 15 |
| 2 | 32 | 44 | 2.5 months | 10 months | 4 | 25 |
| 3 | 35 | 47 | 6.5 months | 20 months | 21 | 31 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De-La-Barrera-Aranda, E.; Gonzalez-Gerez, J.J.; Saavedra-Hernandez, M.; Fernandez-Bueno, L.; Rodriguez-Blanco, C.; Bernal-Utrera, C. Vojta Therapy in Neuromotor Development of Pediatrics Patients with Periventricular Leukomalacia: Case Series. Medicina 2021, 57, 1149. https://doi.org/10.3390/medicina57111149
De-La-Barrera-Aranda E, Gonzalez-Gerez JJ, Saavedra-Hernandez M, Fernandez-Bueno L, Rodriguez-Blanco C, Bernal-Utrera C. Vojta Therapy in Neuromotor Development of Pediatrics Patients with Periventricular Leukomalacia: Case Series. Medicina. 2021; 57(11):1149. https://doi.org/10.3390/medicina57111149
Chicago/Turabian StyleDe-La-Barrera-Aranda, Elena, Juan Jose Gonzalez-Gerez, Manuel Saavedra-Hernandez, Laura Fernandez-Bueno, Cleofas Rodriguez-Blanco, and Carlos Bernal-Utrera. 2021. "Vojta Therapy in Neuromotor Development of Pediatrics Patients with Periventricular Leukomalacia: Case Series" Medicina 57, no. 11: 1149. https://doi.org/10.3390/medicina57111149
APA StyleDe-La-Barrera-Aranda, E., Gonzalez-Gerez, J. J., Saavedra-Hernandez, M., Fernandez-Bueno, L., Rodriguez-Blanco, C., & Bernal-Utrera, C. (2021). Vojta Therapy in Neuromotor Development of Pediatrics Patients with Periventricular Leukomalacia: Case Series. Medicina, 57(11), 1149. https://doi.org/10.3390/medicina57111149








