Limb Salvage after Lower-Leg Fracture and Popliteal Artery Transection—The Role of Vessel-First Strategy and Bone Fixation Using the Ilizarov External Fixator Device: A Case Report
Abstract
1. Introduction
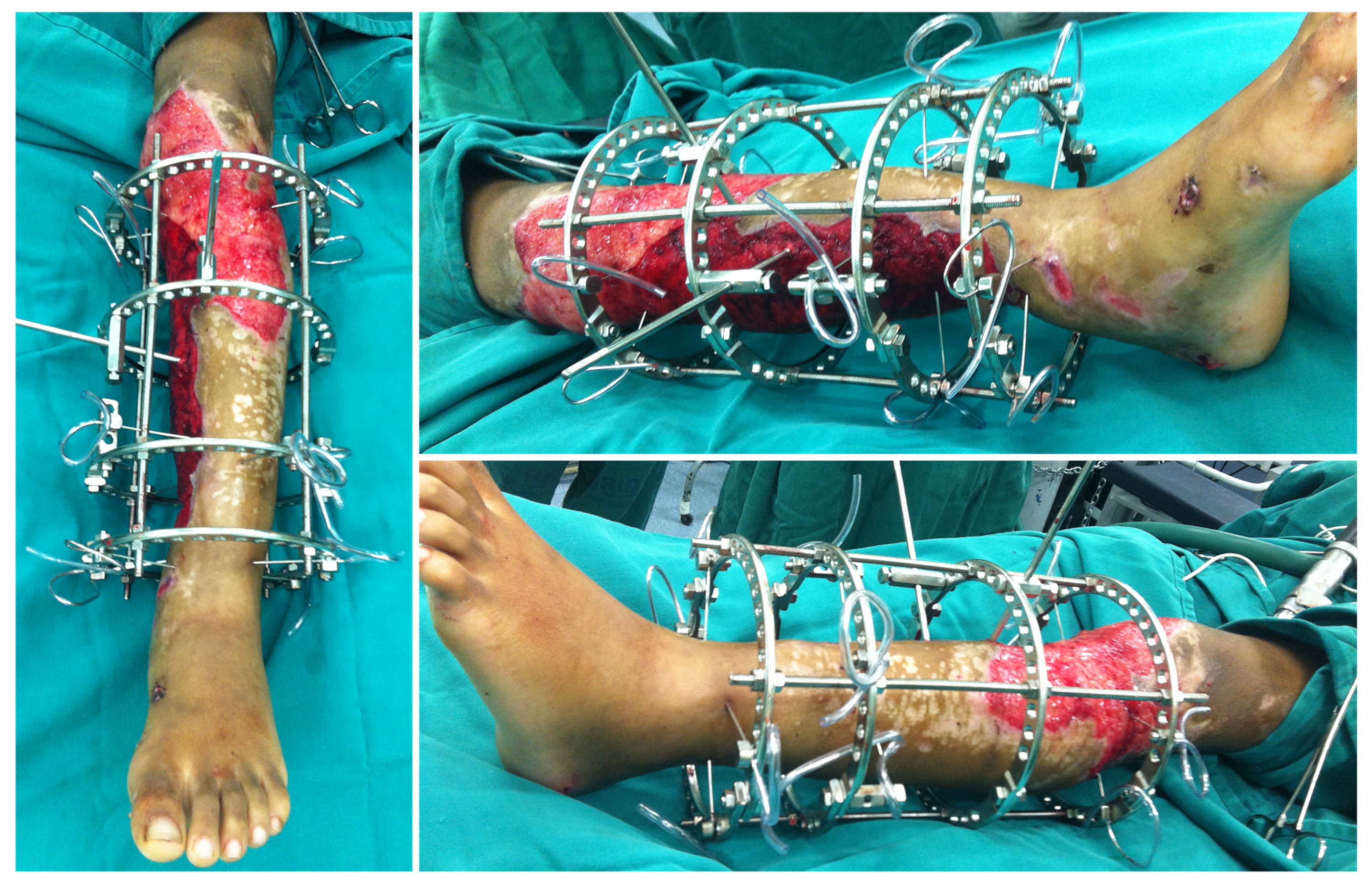
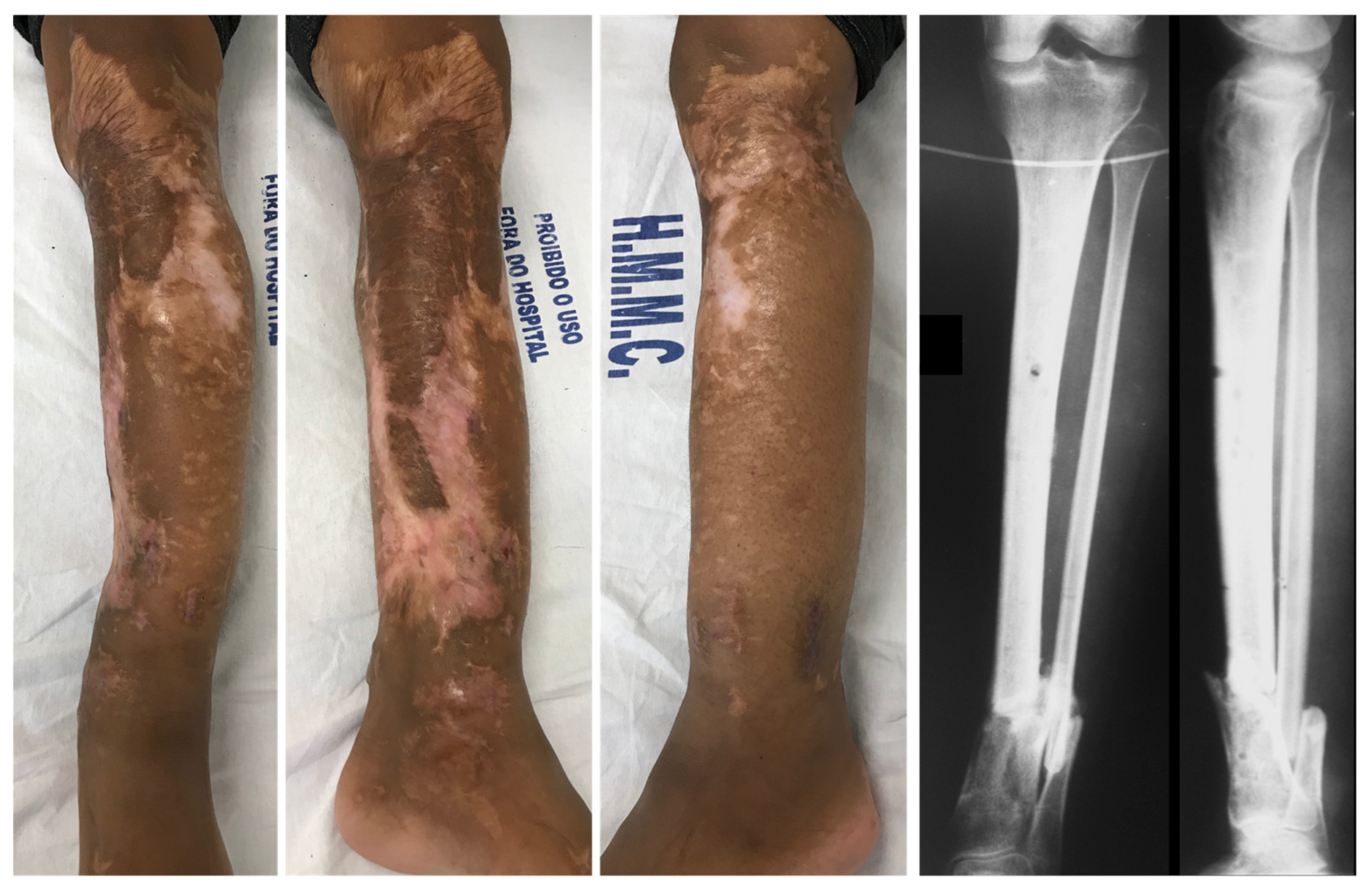
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fairhurst, P.G.; Wyss, T.R.; Weiss, S.; Becker, D.; Schmidli, J.; Makaloski, V. Popliteal Vessel Trauma: Surgical Approaches and the Vessel-First Strategy. Knee 2018, 25, 849–855. [Google Scholar] [CrossRef] [PubMed]
- O’Banion, L.A.; Dirks, R.; Saldana-Ruiz, N.; Farooqui, E.; Yoon, W.J.; Pozolo, C.; Fox, C.J.; Crally, A.; Siada, S.; Nehler, M.R.; et al. Contemporary Outcomes of Traumatic Popliteal Artery Injury Repair from the Popliteal Scoring Assessment for Vascular Extremity Injury in Trauma Study. J. Vasc. Surg. 2021, 74, 1573–1580.e2. [Google Scholar] [CrossRef] [PubMed]
- Perkins, Z.B.; Yet, B.; Glasgow, S.; Cole, E.; Marsh, W.; Brohi, K.; Rasmussen, T.; Tai, N.R.M. Meta-Analysis of Prognostic Factors for Amputation Following Surgical Repair of Lower Extremity Vascular Trauma. BJS 2015, 102, 436–450. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.-W.; Li, Y.-H.; Yu, T.; Yang, T.; Li, Y.; Tan, L. Popliteal Artery Transection Associated with a Minimally Displaced Tibial Plateau Fracture: A Case Report and Review of the Literature. BMC Musculoskelet. Disord. 2020, 21, 59. [Google Scholar] [CrossRef]
- Bliven, E.K.; Greinwald, M.; Hackl, S.; Augat, P. External Fixation of the Lower Extremities: Biomechanical Perspective and Recent Innovations. Injury 2019, 50, S10–S17. [Google Scholar] [CrossRef]
- Hutchinson, B.; McCann, K.; Kirienko, A. The Kickstand Technique for Circular External Fixator Assembly. J. Foot Ankle Surg. 2010, 49, 504–505. [Google Scholar] [CrossRef]
- Kouzelis, A.; Vrachnis, I.N.; Vris, A.; Zampakis, P.; Kokkalis, Z.T.; Panagopoulos, A. A Novel Treatment of a 65-Year-Old Woman with a Neglected Type IIIB Open Fracture of the Tibia with Inadequate Soft Tissue Coverage and Periosteal Stripping Requiring an Ilizarov Approach to Bone and Soft Tissue Lengthening and Reconstruction: A Case Report and Review of the Literature. Am. J. Case Rep. 2020, 21, e926622. [Google Scholar] [CrossRef]
- Reidsma, I.I.; Nolte, P.A.; Marti, R.K.; Raaymakers, E.L.F.B. Treatment of Malunited Fractures of the Ankle. J. Bone Jt. Surgery. Br. Vol. 2010, 92, 66–70. [Google Scholar] [CrossRef]
- Shi, L. The Delayed Management of Main Arterial Injuries in Extremity Trauma: Surgical Challenges and Outcomes. Pak. J. Med. Sci. 2013, 29, 64–67. [Google Scholar] [CrossRef]
- Farber, A.; Tan, T.-W.; Hamburg, N.; Kalish, J.A.; Joglar, F.; Onigman, T.; Rybin, D.; Doros, G.; Eberhardt, R.T. Early Fasciotomy in Patients with Extremity Vascular Injury is Associated with Decreased Risk of Adverse Limb Outcomes: A Review of the National Trauma Data Bank. Injury 2012, 43, 1486–1491. [Google Scholar] [CrossRef]
- Jin, L.; Zhang, S.; Liu, M.; Zhang, Y.; Lin, X.; Feng, D.; Hu, K. Management Algorithm of External Fixation In Lower Leg Arterial Injury For Limb Salvages. medRxiv 2021, 2021.03.01.21252666. [Google Scholar] [CrossRef]
- McHenry, M.T.P.; Holcomb, L.J.B.; Aoki, N.; Lindsey, R.W. Fractures with Major Vascular Injuries from Gunshot Wounds: Implications of Surgical Sequence. J. Trauma Inj. Infect. Crit. Care 2002, 53, 717–721. [Google Scholar] [CrossRef]
- Vielgut, I.; Gregori, M.; Holzer, L.A.; Glehr, M.; Hashemi, S.; Platzer, P. Limb Salvage and Functional Outcomes among Patients with Traumatic Popliteal Artery Injury: A Review of 64 Cases. Wien. Klin. Wochenschr. 2015, 127, 561–566. [Google Scholar] [CrossRef]
- Saleh, M.; Yang, L.; Sims, M. Limb Reconstruction after High Energy Trauma. Br. Med Bull. 1999, 55, 870–884. [Google Scholar] [CrossRef][Green Version]
- Milner, S.A.; Davis, T.R.; Muir, K.R.; Greenwood, D.C.; Doherty, M. Long-Term Outcome after Tibial Shaft Fracture. J. Bone Jt. Surg. Am. Vol. 2002, 84, 971–980. [Google Scholar] [CrossRef]
- Ramos, T.O.; Karlsson, J.; Eriksson, B.I.; Nistor, L. Treatment of Distal Tibial Fractures with the Ilizarov External Fixator—A Prospective Observational Study in 39 Consecutive Patients. BMC Musculoskelet. Disord. 2013, 14, 30. [Google Scholar] [CrossRef]
- Ganji, S.M.E.; Bahrami, M.; Joukar, F. Ilizarov versus AO External Fixator for the Treatment of Tibia Open Fractures. Iran. Red Crescent Med. J. 2011, 13, 868–872. [Google Scholar]
- Inan, M.; Halici, M.; Ayan, I.; Tuncel, M.; Karaoglu, S. Treatment of type IIIA Open Fractures of Tibial Shaft with Ilizarov External Fixator Versus Unreamed Tibial Nailing. Arch. Orthop. Trauma Surg. 2007, 127, 617–623. [Google Scholar] [CrossRef]
- Van Der Walt, N.; Ferreira, N. An Audit of Circular External Fixation Usage in a Tertiary Hospital in South Africa. SA Orthop. J. 2018, 17, 14–21. [Google Scholar] [CrossRef]
- Giordano, V.; Knackfuss, I.G.; Caldas, C.; Giordano, M.; Metsavaht, L.; Gomes, R.C. Treatment of Malunion of the Tibia by the Ilizarov Method. Rev. Bras. Ortop. 1999, 34, 563–568. [Google Scholar]
- Li, Z.; Wang, P.; Li, L.; Li, C.; Lu, H.; Ou, C. Comparison between Open Reduction with Internal Fixation to Circular External Fixation for Tibial Plateau Fractures: A Systematic Review and Meta-Analysis. PLoS ONE 2020, 15, e0232911. [Google Scholar] [CrossRef]
- Lin, L.; Liu, Y.; Lin, C.; Zhou, Y.; Feng, Y.; Shui, X.; Yu, K.; Lu, X.; Hong, J.; Yu, Y. Comparison of Three Fixation Methods in Treatment of Tibial Fracture in Adolescents. ANZ J. Surg. 2018, 88, E480–E485. [Google Scholar] [CrossRef]
- Aquarius, R.; Van Kampen, A.; Verdonschot, N. Rapid pre-tension loss in the Ilizarov external fixator: An in vitro study. Acta Orthop. 2007, 78, 654–660. [Google Scholar] [CrossRef]
- Sellahewa, T.; Weerasinghe, C.; Silva, P. Biomechanical Evaluation Method to Optimize External Fixator Configuration in Long Bone Fractures—Conceptual Model and Experimental Validation Using Pilot Study. Appl. Sci. 2021, 11, 8481. [Google Scholar] [CrossRef]
- Ali., A.; Ullah, H.; Khan, M.S.; Ali, I.; Mufti, A.J.; Azem, Q.; Essa, A. Common Complications of Ilizarov External Fixator. J. Pak. Orthop. Assoc. 2018, 30, 39–43. [Google Scholar]
- Szelerski, Ł.; Kozłowska, A.P.; Żarek, S.; Górski, R.; Mochocki, K.; Dejnek, M.; Urbański, W.; Reichert, P.; Morasiewicz, P. A New Criterion for Assessing Ilizarov Treatment Outcomes in Nonunion of the Tibia. Arch. Orthop. Trauma Surg. 2021, 141, 879–889. [Google Scholar] [CrossRef]







Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giordano, V.; Souza, F.S.; Belangero, W.D.; Pires, R.E. Limb Salvage after Lower-Leg Fracture and Popliteal Artery Transection—The Role of Vessel-First Strategy and Bone Fixation Using the Ilizarov External Fixator Device: A Case Report. Medicina 2021, 57, 1220. https://doi.org/10.3390/medicina57111220
Giordano V, Souza FS, Belangero WD, Pires RE. Limb Salvage after Lower-Leg Fracture and Popliteal Artery Transection—The Role of Vessel-First Strategy and Bone Fixation Using the Ilizarov External Fixator Device: A Case Report. Medicina. 2021; 57(11):1220. https://doi.org/10.3390/medicina57111220
Chicago/Turabian StyleGiordano, Vincenzo, Felipe Serrão Souza, William Dias Belangero, and Robinson Esteves Pires. 2021. "Limb Salvage after Lower-Leg Fracture and Popliteal Artery Transection—The Role of Vessel-First Strategy and Bone Fixation Using the Ilizarov External Fixator Device: A Case Report" Medicina 57, no. 11: 1220. https://doi.org/10.3390/medicina57111220
APA StyleGiordano, V., Souza, F. S., Belangero, W. D., & Pires, R. E. (2021). Limb Salvage after Lower-Leg Fracture and Popliteal Artery Transection—The Role of Vessel-First Strategy and Bone Fixation Using the Ilizarov External Fixator Device: A Case Report. Medicina, 57(11), 1220. https://doi.org/10.3390/medicina57111220






