Non-IgE Mediated Hypersensitivity to Food Products or Food Intolerance—Problems of Appropriate Diagnostics
Abstract
:1. Introduction
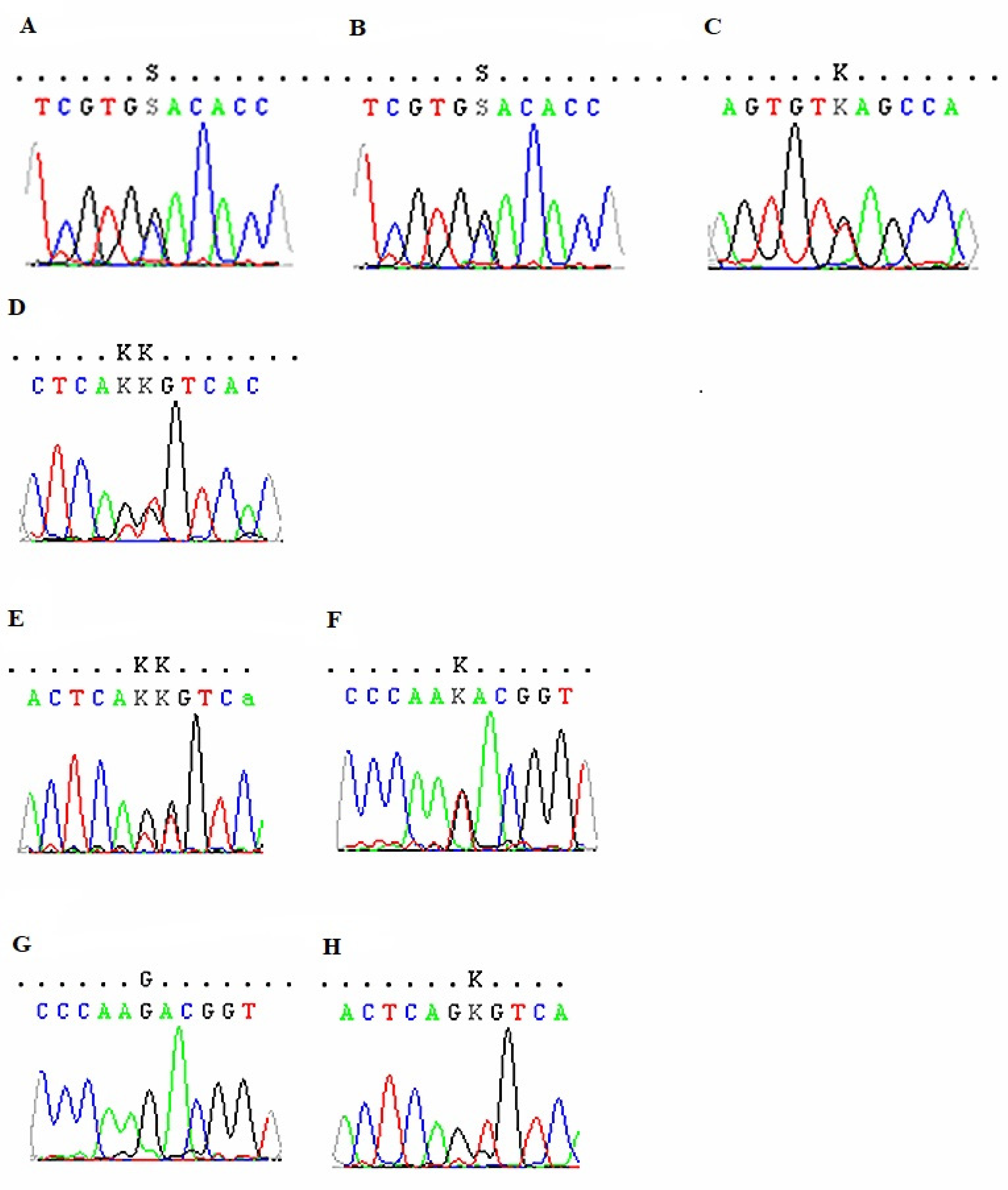
2. Material and Methods
3. Results—Case Reports
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nwaru, B.I.; Hickstein, L.; Panesar, S.S.; Muraro, A.; Werfel, T.; Cardona, V.; Dubois, A.E.J.; Halken, S.; Hoffmann-Sommergruber, K.; Poulsen, L.K.; et al. The epidemiology of food allergy in Europe: A systematic review and meta-analysis. Allergy 2014, 69, 62–75. [Google Scholar] [CrossRef] [Green Version]
- Sampson, H.A.; Aceves, S.; Bock, S.A.; James, J.; Jones, S.; Lang, D.; Nadeau, K.; Nowak-Wegrzyn, A.; Oppenheimer, J.; Perry, T.T.; et al. Food allergy: A practice parameter update—2014. J. Allergy Clin. Immunol. 2014, 134, 1016–1025. [Google Scholar] [CrossRef] [PubMed]
- Boyce, J.A.; Assad, A.; Burks, A.W.; Jones, S.M.; Sampson, H.A.; Wood, R.A.; Plaut, M.; Cooper, S.F.; Fenton, M.J.; Arshad, S.H.; et al. Guidelines for the diagnosis and management of food allergy in the United States: Report of the NIAID-sponsored expert panel. J. Allergy Clin. Immunol. 2010, 126 (Suppl. 6), S1–S58. [Google Scholar] [CrossRef] [PubMed]
- Leśniak, M.; Juda, M.; Dyczek, Ł.; Czarnobilska, M.; Leśniak, M.; Czarnobilska, E. Diagnosis of food allergy. Przegl. Lek. 2016, 73, 245–249. [Google Scholar] [PubMed]
- Bartuzi, Z. Alergia na pokarmy. In Alergologia, 2nd ed.; Obtułowicz, K., Ed.; Wydawnictwo Lekarskie PZWL: Warsaw, Poland, 2016; pp. 307–331. [Google Scholar]
- Bartuzi, Z.; Kaczmarski, M.; Czerwionka-Szaflarska, M.; Małaczyńska, M.; Krogulska, A. The diagnosis and management of food allergies. Position paper of the Food Allergy Section the Polish Society of Allergology. Adv. Dermatol. Allergol. 2017, XXXIV, 391–404. [Google Scholar] [CrossRef] [PubMed]
- Burks, W.; Tang, M.; Sicherer, S.; Muraro, A.; Eigenmann, P.A.; Ebisawa, M.; Fiocchi, A.; Chiang, W.; Beyer, K.; Wood, R.; et al. ICON: Food allergy. J. Allergy Clin. Immunol. 2012, 129, 906–920. [Google Scholar] [CrossRef]
- Pimentel, M.; Lembo, A. Microbiome and Its Role in Irritable Bowel Syndrome. Dig. Dis. Sci. 2020, 65, 829–839. [Google Scholar] [CrossRef] [Green Version]
- Bentz, S.; Hausmann, M.; Piberger, H.; Kellermeier, S.; Paul, S.; Held, L.; Falk, W.; Obermeier, F.; Fried, M.; Schölmerich, J.; et al. Clinical relevance of IgG antibodies against food antigens in Crohn’s disease: A double-blind cross-over diet intervention study. Digestion 2010, 81, 252–264. [Google Scholar] [CrossRef] [Green Version]
- Muraro, A.; Halken, S.; Arshad, S.H.; Beyer, K.; Dubois, A.E.J.; Du Toit, G.; Eigenmann, P.; Grimshaw, K.; Hoest, A.; Lack, G.; et al. Sheikh A on behalf of EAACI Food Allergy and Anaphylaxis Guidelines Group. EAACI Food Allergy and Anaphylaxis Guidelines. Primary prevention of food allergy. Allergy 2014, 69, 590–601. [Google Scholar] [CrossRef]
- Lis, K.; Bartuzi, Z. Alternatywne metody w diagnostyce alergii pokarmowej./Alternative methods in the diagnostic of food allegy. Alerg. Astma Immunol. 2018, 23, 73–78. [Google Scholar]
- Kurek, M. Ocena testu cytotoksyczności i testu ALCAT w rozpoznawaniu alergii i ustalaniu wskazań do leczenia za pomocą diet eliminacyjnych./Evaluation of the cytotoxic test and the ALCAT test in the diagnosis of allergies and in determining the indications for treatment with elimination diets. Alerg. Astma Immunol. 1997, 2, 193–197. [Google Scholar]
- Mullin, G.E.; Swift, K.M.; Lipski, L.; Turnbull, L.K.; Rampertabet, S.D. Testing for Food Reactions: The Good, the Bad, and the Ugly. Nutr. Clin. Pract. 2010, 25, 192–198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gocki, J.; Bartuzi, Z. Role of immunoglobulin G antibodies in diagnosis of food allergy. Post. Dematol. Alergol. 2016, 33, 253–257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atkinson, W.; Sheldon, T.A.; Shaath, N.; Whorwell, P.J. Food elimination based on IgG antibodies in irritable bowel syndrome: A randomised controlled trial. Gut 2004, 53, 1459–1464. [Google Scholar] [CrossRef] [PubMed]
- Arroyave Hernández, C.M.; Echavarría Pinto, M.; Hernández Montiel, H.L. Food allergy mediated by IgG antibodies associated with migraine in adults. Rev. Alerg. Mex. 2007, 54, 162–168. [Google Scholar] [PubMed]
- Tay, S.S.; Clark, A.T.; Deighton, J.; King, Y.; Ewan, P.W. Patterns of immunoglobulin G responses to egg and peanut allergens are distinct: Ovalbumin-specific immunoglobulin responses are ubiquitous, but peanut-specific immunoglobulin responses are up-regulated in peanut allergy. Clin. Exp. Allergy 2007, 37, 1512–1518. [Google Scholar] [CrossRef]
- Aalberse, R.C.; Stapel, S.O.; Schuurman, J.; Rispens, T. Immunoglobulin G4: An odd antibody. Clin. Exp. Allergy 2009, 39, 469–477. [Google Scholar] [CrossRef] [PubMed]
- Kucharczyk, A.; Korzebska-Gawryluk, R. Znaczenie diagnostyki alergii i nietolerancji pokarmowych w oparciu o wyniki swoistych dla pokarmów immunoglobulin klasy IgG. Stanowisko Europejskiej Akademii Alergologii i Immunologii Klinicznej./ Importance of the diagnosis of food allergies and intolerances based on the results of specific IgG immunoglobulins. Position paper of the European Academy of Allergology and Clinical Immunology. Alergol. Współczesna 2012, 1, 5–10. [Google Scholar]
- Stapel, S.O.; Asero, R.; Ballmer-Weber, B.K.; Knol, E.F.; Strobel, S.; Vieths, S.; Kleine-Tebbe, J. Testing for IgG4 against foods is not recommended as a diagnostics tool: EAACI. Force Report. Allergy 2008, 63, 793–796. [Google Scholar] [CrossRef] [Green Version]
- Hammond, C.; Lieberman, J.A. Unproven Diagnostic Tests for Food Allergy. Immunol. Allergy Clin. N. Am. 2018, 38, 153–163. [Google Scholar] [CrossRef]
- Ansotegui, I.J.; Melioli, G.; Canonica, G.W.; Caraballo, L.; Villa, E.; Ebisawa, M.; Passalacqua, G.; Savi, E.; Ebo, D.; Gómez, R.M.; et al. IgE allergy diagnostics and other relevant tests in allergy, a World Allergy Organization position paper. World Allergy Organ. J. 2020, 13, 100080. [Google Scholar] [CrossRef] [PubMed]
- Ghada, A.; Rasheed, Z.; Salama, R.H.; Salem, T.; Ahmed, A.A.; Zedan, K.; El-Moniem, A.A.; Elkholy, M.; Al Robaee, A.A.; Alzolibani, A.A.; et al. Filaggrin, major basic protein and leukotriene B4: Biomarkers for adult patients of bronchial asthma, atopic dermatitis and allergic rhinitis. Intractable Rare Dis. Res. 2018, 7, 264–270. [Google Scholar] [CrossRef] [Green Version]
- Paller, A.S.; Spergel, J.M.; Mina-Osorio, P.; Irvine, A.D. The Atopic March and Atopic Multimorbidity: Many Trajectories, Many Pathways. J. Allergy Clin. Immunol. 2019, 143, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Marenholz, I.; Kerscher, T.; Bauerfeind, A.; Esparza-Gordillo, J.; Nickel, R.; Keil, T.; Lau, S.; Rohde, K.; Wahn, U.; Lee, Y.-A. An interaction between filaggrin mutations and early food sensitization improves the prediction of childhood asthma. Mech. Allergy Clin. Immunol. 2009, 123, 911–916. [Google Scholar] [CrossRef]
- Ogrodowczyk, A.; Markiewicz, L.; Wróblewska, B. Mutations in the filaggrin gene and food allergy. Prz. Gastroenterol. 2014, 9, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Walker, M.T.; Green, J.E.; Ferrie, R.P.; Queener, A.M.; Kaplan, M.H.; Cook-Mills, J.M. Mechanism for initiation of food allergy: Dependence on skin barrier mutations and environmental allergen co-stimulation. J. Allergy Clin. Immunol. 2018, 141, 1711–1725.e9. [Google Scholar] [CrossRef] [Green Version]
- Pereira Santos, M.C.; Lourenco, T.; Pedro, E.; Pereira Barbosa, M.; Ferreira, M.B. Evaluation of Api m10 specific IgE and IgG4 after one year of bee venom immunotherapy. Eur. Ann. Allergy Clin. Immunol. 2020, 52, 175–181. [Google Scholar] [CrossRef] [Green Version]
- Sandilands, A.; Terron-Kwiatkowski, A.; Hull, P.R.; O’Regan, G.M.; Clayton, T.H.; Watson, R.M.; Carrick, T.; Evans, A.T.; Liao, H.; Zhao, Y.; et al. Comprehensive analysis of the gene encoding filaggrin uncovers prevalent and rare mutations in ichthyosis vulgaris and atopic eczema. Nat. Genet. 2007, 39, 650–654. [Google Scholar] [CrossRef]
- Human Gene Mutation Database (HGMD). 2020. Available online: http://www.hgmd.cf.ac.uk (accessed on 15 December 2020).
- ClinVar. 2020. Available online: http://www.ncbi.nlm.nih.gov/clinvar (accessed on 15 December 2020).
- Niggemann, B.; Grüber, C. Unproven diagnostic procedures in IgE-mediated allergic diseases. Allergy 2004, 59, 806–808. [Google Scholar] [CrossRef]
- Schnedl, W.J.; Lackner, S.; Enko, D.; Schenk, M.; Mangge, H.; Holasek, S.J. Non-celiac gluten sensitivity: People without celiac disease avoiding gluten-is it due to histamine intolerance? Inflamm. Res. 2018, 67, 279–284. [Google Scholar] [CrossRef]
- Valenti, S.; Corica, D.; Ricciardi, L.; Romano, C. Gluten-related disorders: Certainties, questions and doubts. Ann. Med. 2017, 49, 569–581. [Google Scholar] [CrossRef]
- Kaličanin, D.; Brčić, L.; Barić, A.; Zlodre, S.; Barbalić, M.; Torlak Lovrić, V.; Punda, A.; Perica, V.B. Evaluation of correlations between food-specific antibodies and clinical aspects of Hashimoto’s Thyroiditis. J. Am. Coll. Nutr. 2019, 38, 259–266. [Google Scholar] [CrossRef]
- Zeng, Q.; Dong, S.Y.; Wu, L.X.; Li, H.; Sun, Z.-J.; Li, J.-B.; Jiang, H.-X.; Chen, Z.-H.; Wang, Q.-B.; Chen, W.-W. Variable food-specific IgG antibody levels in healthy and symptomatic Chinese adults. PLoS ONE 2013, 8, e53612. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zuo, X.L.; Li, Y.Q.; Li, W.J.; Guo, Y.T.; Lu, X.F.; Li, J.M.; Desmond, P.V. Alterations of food antigen-specific serum immunoglobulins G and E antibodies in patients with irritable bowel syndrome and functional dyspepsia. Clin. Exp. Allergy 2007, 37, 823–830. [Google Scholar] [CrossRef]
- Martins, T.B.; Bandhauer, M.E.; Wilcock, D.M.; Hill, H.R.; Slev, P.R. Specific Immunoglobulin (Ig) G Reference Intervals for Common Food, Insect, and Mold Allergens. Ann. Clin. Lab. Sci. 2016, 46, 635–638. [Google Scholar] [PubMed]
- Szilagyi, A.; Ishayek, N. Lactose Intolerance, Dairy Avoidance, and Treatment Options. Nutrients 2018, 10, 1994. [Google Scholar] [CrossRef] [Green Version]
- Stenson, P.D.; Mort, M.; Ball, E.V.; Chapman, M.; Evans, K.; Azevedo, L.; Hayden, M.; Heywood, S.; Millar, D.S.; Phillips, A.D.; et al. The Human Gene Mutation Database (HGMD®): Optimizing its use in a clinical diagnostic or research setting. Hum. Genet. 2020, 139, 1197–1207. [Google Scholar] [CrossRef]
- Kim, M.; Yoo, J.; Kim, J.; Park, J.; Han, E.; Jang, W.; Chae, H.; Lee, J.H.; Park, Y.M.; Kim, Y. Association of FLG single nucleotide variations with clinical phenotypes of atopic dermatitis. PLoS ONE 2017, 12, e0190077. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kiritsi, D.; Valari, M.; Forgugno, P.; Hausser, I.; Lykopoulou, L.; Zambruno, G.; Fischer, J.; Bruckner-Tuderman, L.; Jakob, T.; Has, C. Whole-exome sequencing in patients with ichthyosis reveals modifiers associated with increased IgE levels and allergic sensitizations. J. Allergy Clin. Immunol. 2014, 135, 280–283. [Google Scholar] [CrossRef] [PubMed]
- Astolfi, A.; Cipriani, F.; Messelodi, D.; De Luca, M.; Indio, V.; Di Chiara, C.; Giannetti, A.; Ricci, L.; Neri, I.; Patrizi, A.; et al. Filaggrin loss-of-funcion mutations are risk factors for severe food allergy in children with atopic dermatitis. J. Clin. Med. 2021, 10, 233. [Google Scholar] [CrossRef] [PubMed]
| Kind of Food | Case 1 | Case 2 | Case 3 | Case 4 | ||||
|---|---|---|---|---|---|---|---|---|
| Cytotoxic Test (Metabolic Code 203) | IgG4 (mgA/l) | Cytotoxic Test (Metabolic Code 203) | IgG4 (mgA/l) | Test ImuPro | IgG4 (mgA/l) | Test ImuPro | IgG4 (mgA/l) | |
| Peach | 0 | 2.68 | 0 | 4.1 | No test | 0.51 | No test | 1.53 |
| Egg | 0 | 23.1 | +2 | 3.41 | Extremely high >20 mg IgG/ml | 5.46 | +1 (7.54–12.49 mg IgG/mL) | 1.44 |
| Cow milk (casein *) | +1 | 1.26 | +3 | 0.81 | Increased >7.5 mg IgG/ml | 1.49 | Not increased | 0.36 |
| Peanuts | No test; +2 (walnuts), +3 (hazel) | 0.05 | +3 +2 (walnuts) | 0.03 | No test | 1.07 | +2 (12.5–19.9 mg IgG/mL) | 0.01 |
| Grains (omega-5-gliadine *) | +3 (wheat) | 0.01 | +2 (wheat) | 0.01 | Only wheat-increased | 0.03 | +3 (gluten) (20–49.9 mg IgG/mL) +3 (wheat) (20–49.9 mg IgG/mL) | 0.01 |
| Fish | +1/+3 (different genera) | 0.00 | +1/+3 (different genera) | 0.01 | No test | 0.01 | +1 (plaice) | 0.00 |
| Symptoms Severity after Food Consumption before Elimination and after Products Reintroduction | ||||||||
|---|---|---|---|---|---|---|---|---|
| Case 1 | Case 2 | Case 3 | Case 4 | |||||
| Food Products (Allergens *) | Before Elimination | After Reintroduction | Before Elimination | After Reintroduction | Before Elimination | After Reintroduction | Before Elimination | After Reintroduction |
| Peach | No symptoms | No elimination | No symptoms | No symptoms (OAS possible) | No symptoms | No elimination | No symptoms | No symptoms |
| Egg | No symptoms | No symptoms | No symptoms | No symptoms | Symptoms | Symptoms (slight) | No symptoms | No symptoms |
| Cow milk (casein *) | Symptoms | Symptoms | Symptoms | No elimination | Symptoms | Symptoms | Symptoms | Symptoms (slight) |
| Peanuts | No symptoms | No elimination | No symptoms | No elimination | No symptoms | No elimination | No symptoms | No elimination |
| Grains (omega-5-gliadine *) | Symptoms | Symptoms | Symptoms | Symptoms | Symptoms | No elimination | Symptoms | Symptoms (slight) |
| Fish | No symptoms | No elimination | No symptoms | No elimination | No symptoms | No elimination | No symptoms | No elimination |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Myszkowska, D.; Zapała, B.; Bulanda, M.; Czarnobilska, E. Non-IgE Mediated Hypersensitivity to Food Products or Food Intolerance—Problems of Appropriate Diagnostics. Medicina 2021, 57, 1245. https://doi.org/10.3390/medicina57111245
Myszkowska D, Zapała B, Bulanda M, Czarnobilska E. Non-IgE Mediated Hypersensitivity to Food Products or Food Intolerance—Problems of Appropriate Diagnostics. Medicina. 2021; 57(11):1245. https://doi.org/10.3390/medicina57111245
Chicago/Turabian StyleMyszkowska, Dorota, Barbara Zapała, Małgorzata Bulanda, and Ewa Czarnobilska. 2021. "Non-IgE Mediated Hypersensitivity to Food Products or Food Intolerance—Problems of Appropriate Diagnostics" Medicina 57, no. 11: 1245. https://doi.org/10.3390/medicina57111245
APA StyleMyszkowska, D., Zapała, B., Bulanda, M., & Czarnobilska, E. (2021). Non-IgE Mediated Hypersensitivity to Food Products or Food Intolerance—Problems of Appropriate Diagnostics. Medicina, 57(11), 1245. https://doi.org/10.3390/medicina57111245






