1. Introduction
Frostbite is an injury caused by freezing of the skin and underlying tissues. Severe frostbite is a relatively uncommon event that can lead to early arthritis, tissue loss, or amputation. Frostbite comprises on average 2% of mountain emergencies in the western Alps [
1]. Frostbite takes place in three phases: pre-freeze/freezing, thawing/rewarming, and mummification.
Pre/freeze is an acute ischemia with peripheral vasoconstriction. During freezing, cell death is triggered by intracellular dehydration and direct damage to cell membrane by ice microcrystals. Thawing is best accomplished by the immersion of frozen limbs in warm water. After blood flow is restored, cyanotic lesions can occur. During rewarming, there is a vascular stasis with a prothrombotic environment (hypoxia and acidosis), interstitial edema, and ischemia–reperfusion injuries. It leads to the destruction of microcirculation and cell death [
2,
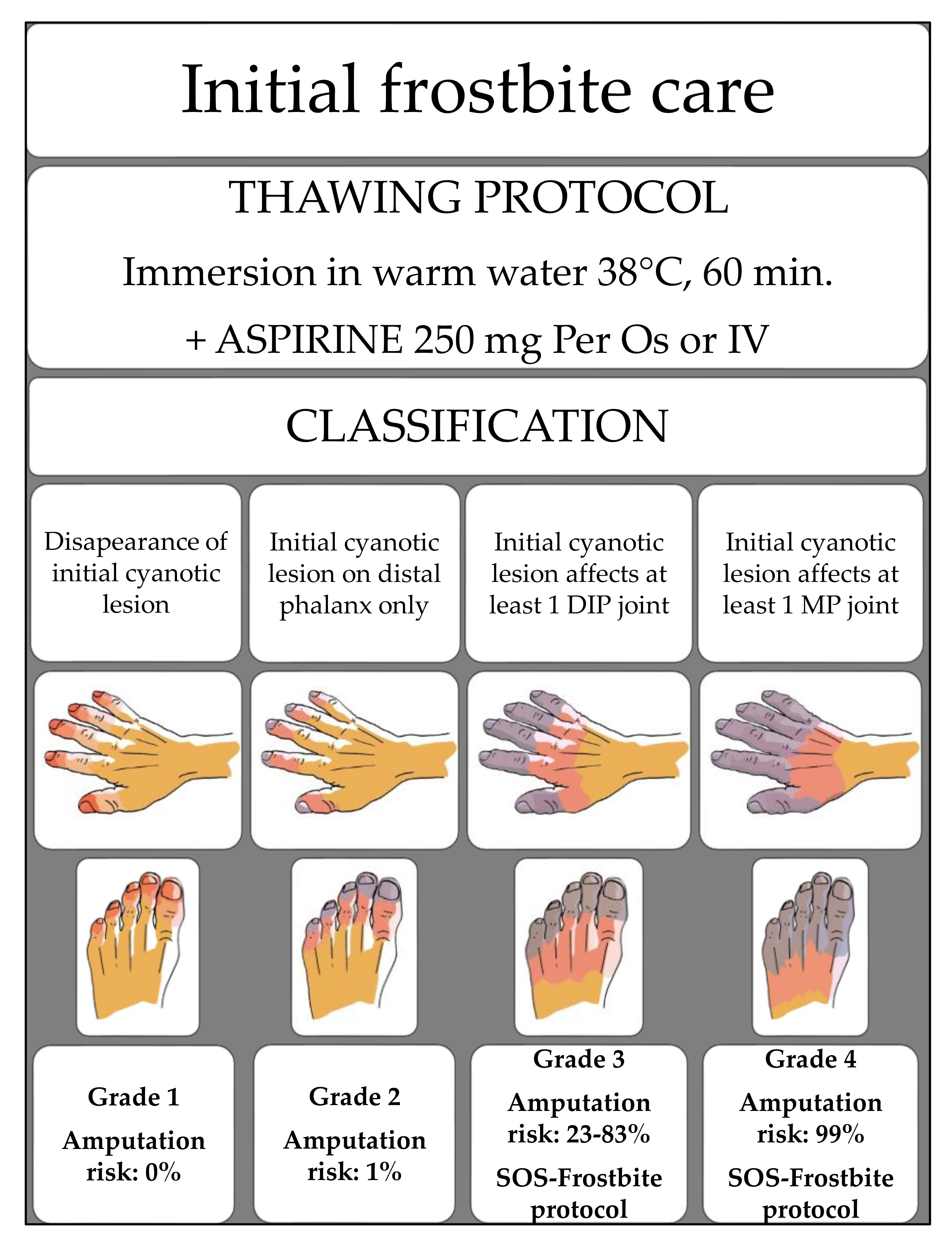
3]. Frostbite outcome is related to the initial cyanotic lesion. The Cauchy classification defines four grades that predict the amputation risk after rapid thawing in warm water when there is no targeted frostbite care [
3]. It is based on the extent of the initial cyanotic lesion. Frostbite is classified as grade 1 if cyanosis disappears, grade 2 if only distal phalanges are cyanotic (amputation risk below 1%), grade 3 if cyanosis involves the intermediate or proximal phalanges (amputation risk: 30–83% greater in the hands than feet), and grade 4 if cyanosis involves the metacarpals or metatarsals (amputation risk: 99%) [
3] (
Figure 1).
The goal of treatment is to limit tissue damage from hypoxia and acidosis, mitigate the subsequent prothrombotic cascade, reduce edema and the inflammatory response, and minimize the impact of the ischemic–reperfusion syndrome. Prior studies have demonstrated the efficacy of thrombolytics such as recombinant tissue plasminogen activator (rt-PA) [
4] and vasodilator such as iloprost [
5,
6,
7] in improving outcome [
8]; medical care must be initiated within 24 h for rt-PA [
9,
10] and 48 h for iloprost [
11]. Currently, the Wilderness Medical Society guidelines do not recommend HBO treatment for frostbite [
8]. However, HBO may improve frostbite outcome by increasing the cellular oxygen availability to the damaged tissues. This may help to mitigate the negative impact of the inflammatory cascade and the ischaemia–reperfusion syndrome [
12]
. Few case reports suggest that HBO might improve frostbite injury outcome [
13,
14,
15,
16,
17,
18,
19,
20,
21,
22,
23]. There are no randomized controlled trials (RCT) with HBO conducted so far. It is arduous to carry out a double-blinded RCT for HBO because frostbite is uncommon, and blinding subjects to HBO or not HBO could be difficult.
We implemented a cross-border European program (INTERREG-IV FRANCE-SUISSE) to foster and coordinate the care management of patients who suffer frostbite in the French and Swiss Alps.
2. Materials and Methods
2.1. Study Oversight
The SOS-Frostbite research program was a multicenter prospective, non-randomized study from 2013 to 2019. The study was conducted by the hyperbaric centers of Geneva and Lyon, and the Mont-Blanc hospitals in Chamonix and Sallanches. The statistical analysis was performed independently by the unit of methodological support from the CTU of Geneva University Hospital. The study aim was to assess whether the early addition of HBO to standard care with iloprost (prospective group) was associated with better frostbite outcomes compared to standard care alone (retrospective group).
2.2. Setting and Participants
Patients were eligible for the SOS-Frostbite protocol after screening determined no contraindication to aspirin, iloprost, or HBO. The inclusion criteria for both groups were grade 3 or 4 frostbite according to the Cauchy classification [
3] and start of medical care within 72 h from frostbite injury, which was defined previously in the historical cohort as the onset of frostbite. Physicians involved in the study systematically searched for the onset of loss of sensitivity in the fingers or toes through the medical history to determine this time period.
To identify the historical cohort, we retrospectively collected data of all frostbite medical files treated at the Mont-Blanc hospital from 2000 to 2012. Before 2000, as the Cauchy classification had not yet been established, no patients could be included. All eligible patients who met the inclusion criteria from the retrospective analysis were included in the historical cohort. They were all grade 3 or 4 frostbitten patients who received a standardized protocol including iloprost, which was initiated no longer than 72 h from frostbite injury.
The standardized frostbite treatment: frostbitten extremities were rewarmed by immersion in warm water (38 °C) for 60 min, and patients were given aspirin 250 mg orally. During the hour following the rewarming, the frostbite classification was determined. Grade 3 or 4 frostbite patients received the first iloprost infusion immediately (by infusion pump, 8–10 mcg/h for 6 h, 48–60 mcg/day). Patients were hospitalized for 7 days to continue daily iloprost (by infusion pump, 8 to 10 mcg/h for 6 h, 48–60 mcg/day), aspirin (250 mg/day; orally), antibiotics (amoxicillin/clavulanate: 1 g/125 mg 3 times daily, orally for 7 days), and daily wound care with topical hyaluronic acid.
To identify the SOS-Frostbite group, data were prospectively collected from patients satisfying inclusion criteria who received the same standardized frostbite treatment protocol plus early HBO from 2013 to 2019.
The SOS Frostbite protocol: The SOS-Frostbite protocol was initiated upon hospital arrival. Patients were treated with the same standardized protocol as the historical cohort with the addition of HBO. The first HBO (150 min at 2.5ATA) session was done as soon as possible after the first iloprost infusion (from 1 to 6 h after the end of the iloprost infusion, as some patients were transferred from other hospitals to the Geneva or Lyon hyperbaric chamber for HBO). Then, patients were hospitalized for 7 days and received the same treatment protocol as in the historical cohort plus HBO sessions (150 min, 2.5 ATA, 1 daily) (
Appendix A,
Figure A1). After hospital discharge, the patient completed daily HBO sessions for 7 additional days (14 HBO session in total). Hyperbaric chambers involved in the study used multiplace chambers and patients breathed oxygen via a mask or a hood.
2.3. The Follow-Up
A Technecium 99 (Tc99) bone scan was performed at day 3 and day 7 (control group and prospective cohort). Results were considered pathological when the bone scan demonstrated absent or markedly decreased uptake of the Tc99 tracer in the bone tissue (severe bone ischemia). An additional Tc 99 bone scan was conducted at the end of the HBO sessions if radiological improvement (recovery of bone activity) was identified on the day 7 Tc99 bone scan compared to the day 3 Tc99 bone scan. All patients had a clinical examination at 6 months, 1 year. Patients enrolled in the first 4 years of the study also had a follow-up at 2 years and 3 years to evaluate early and delayed sequelae such as arthritis.
2.4. Outcomes
The study’s primary outcome was the number of preserved segments at 12 months, which was defined as the difference between the number of segments with frostbite after rewarming and lost segments. Each phalanx and each metacarpal or metatarsal is defined as a segment; 4 segments comprise a ray (3 segments for the thumb or the hallux), and 3 out 4 segments make a digit (2 out 3 segments make the digit for the thumb or the hallux). To align with the eligibility criteria regarding frostbite severity (grade 3 or 4), we only considered rays with at least 2 segments damaged. The secondary outcomes were the number of amputated segments at 12 months and the ratio of the number of amputated segments at 12 months divided by the number of segments with initial frostbite injury.
2.5. Data Collection
All data from the prospective and the historical cohorts were collected on site using a standardized case report form. All observations were coded to preserve patient anonymity and data confidentiality.
2.6. Statistical Analysis
There was no preliminary estimation of study sample size; we used all available data on 31 December 2019 and obtained a fixed sample size of 58 patients. In the control group, we described 6 (mean ± SD, 5.3) preserved segments at 12 months post-treatment. We had 80% power to detect a two-fold increase in the number of preserved segments (+6) in the standard care plus HBO group, considering a larger variability of the difference of number of preserved segments (±10).
Continuous variables were reported as mean ± SD, median, and interquartile range. Categorical variables are reported as frequencies and percentages. We compared two cohorts of patients: those included between 2000 and 2012 (historical cohort) and those included after 2013 (prospective cohort). We compared continuous variables between the two cohorts of patients with the use of nonparametric Mann–Whitney test, as we anticipated that continuous variables are non-normally distributed and do not respect the assumptions for using Student’s t-test; we compared categorical variables between the two cohorts with the use of chi-square or Fisher’s exact tests, depending on assumptions, and p-values of less than 0.05 were considered to indicate statistical significance. Since the main outcome (number of preserved segments) was an ordinal variable (0, 1, 2, 3, and 4 preserved segments) and because one patient could have several data points for the main outcome (repeated measurements), we performed mixed ordinal logistic regressions with the patient identifier as a random factor. We compared the main outcome between the two cohorts of patients (HBO plus standard care vs. standard care alone). We adjusted the analysis for patient age, delay between signs of freezing and medical treatment received (<6 h, 6–12 h, 12–24 h, 24–48 h, and 48–72 h). For secondary outcome, we also performed mixed ordinal logistic regressions models as the number of amputations was also ordinal (3–4, 2, 1, 0 amputation), and we also adjusted the analysis for patient age and the delay between signs of freezing and medical treatment received. All analyses were performed with the use of STATA 16 IC (StatCorp, College Station, TX, USA).
3. Results
3.1. Description
3.1.1. Patients
The prospective cohort: Thirty-nine patients with grade 3 or 4 frostbite were treated from 2013 to 2019 with the SOS-Frostbite protocol; 11 patients were excluded because medical care delay was over 72 h from frostbite injury or the treatment protocol was interrupted or changed. For statistical analysis, 28 patients were prospectively included in the SOS-Frostbite group. None of the patients from the prospective cohort suffered from HBO side effects.
The retrospective cohort (control group): After reviewing all frostbite medical files in the Mont-Blanc hospitals (168 medical files), 30 patients met the inclusion criteria (standardized frostbite treatment with iloprost, grade 3 or 4 frostbite and medical care initiated within 72 h from frostbite injury) (
Figure 2).
The SOS-Frostbite group and the historical control group both consisted of a similar number of patients with identical inclusion criteria.
The comparison of patient characteristics is presented in
Table 1. Percentages of patients with delays of 12 to 24 h or 24 to 48 h were more frequent in the prospective cohort compared to the historical cohort. Patients were significantly older in the prospective than in the historical cohort. A higher proportion of patients with three or four segments with frostbite were observed in the prospective cohort compared to the control group (
p < 0.001).
3.1.2. Outcomes
A significantly higher mean number of preserved segments per patient was observed in the prospective SOS-Frostbite group (13 SD ± 10) compared to the historical control group (6 SD ± 5) (
p = 0.006). In the prospective cohort, 57% of patients had three to four preserved segments (respectively 43% for three segments and 14% for four segments) compared to 13% in the control group (respectively 13% for three segments and 0% for four segments). (
p < 0.001,
Table 2). At baseline, a higher but not statistically significant number of frostbitten segments was observed in the prospective than in the control group. However, a significantly higher number of frostbitten amputated segments was observed in the control than in the prospective group (
p = 0.014,
Table 2).
The odds ratio of the number of preserved segments was significantly higher by 20-fold (95%CI: 4-101,
p < 0.001) in the prospective group who received standard care plus HBO compared to the control group (
Table 3, model 1). This association remained after adjustment for patient age and delay between signs of freezing and medical treatment start (
Table 3, model 2).
The association between the treatment received (cohort group) and a lower number of amputated segments was assessed. The odds of fewer amputated segments were significantly higher in the prospective group with standard care plus HBO compared to the control group with standard care alone (odds ratio 0.015; 95% CI: 0.0009; 0.25, p = 0.003). This association was reinforced after adjustment for patient age and delay between signs of freezing and onset of medical treatment, but due to very small numbers, the imprecision of the estimates was very large (odds ratio 0.0004; 95% CI: 0.00003; 0.06, p = 0.002).
If we consider the ratio of segment amputation to all injured segments, a higher proportion of patients with one-third, half, two-thirds, or the total of segments amputated in the control group were observed compared to the standard care plus HBO group after 1-year follow-up (
Table 2).
4. Discussion
This observational study is the first published prospective study reporting data on severe frostbite treated by early HBO.
In this study, HBO is a positive adjunct to treatment with iloprost. When started within 48 h from injury, iloprost can increase the segment salvage rate up to 78% in severe frostbite [
24]. Iloprost has the highest recommendation level in frostbite treatment [
8] and should be considered on grade 3 or 4 frostbites when rt-PA is contraindicated or is used in the field. Frostbite treatment with iloprost is strongly recommended, as it decreases the risk of amputation; HBO further improves segment salvage even if initiated after 48 h from frostbite injury.
This study did not compare the combined effect of thrombolytics and HBO. Thrombolytics are another recommended treatment that can lower the amputation rate from 41% to 10% when done within 24 h from frostbite injury [
4]; a risk–benefit analysis should always be performed regarding bleeding risk and all contraindication to the treatment.
HBO is a non-invasive treatment; side effects are self-limiting and can mostly be avoided with appropriate screening [
25]. In appropriate indications, the benefits of HBO frequently outweigh the risks. The US Food and Drug administration approved HBO for the treatment of acute ischemia, whereas iloprost has not yet been approved for such treatment. It can be performed on some people with contraindication to rt-PA due to the bleeding risk or in children. When available, HBO may be considered as an alternative treatment when there are contraindications to iloprost or thrombolytics. In our study, we showed that HBO plus standard care including iloprost significantly reduced the amputation risk even over 48h from frostbite injury.
The physiological mechanism of HBO action is well known [
12,
13,
14,
15,
16,
17,
18,
19,
20,
21,
22,
23], but there are no previous randomized controlled trials conducted to evaluate the added value of HBO on frostbite injury outcomes. Regarding frostbite physiopathology, there are good reasons as to why HBO could improve frostbite injury outcomes. HBO has a direct action on tissue ischemia, increasing dissolved oxygen and improving oxygen transportation in the blood. The HBO decreases blood viscosity and minimizes the inflammatory cascade. There is a hyperoxic vasoconstriction in the micro vascularization of healthy tissues, inducing a redistribution of blood to hypoxic territories. Those effects of HBO on vasoconstriction decrease edema and the incidence of compartment syndrome. There is a reduction of the deleterious influences of ischemia–reperfusion [
12,
26,
27] besides diminishing damages due to the thaw–rewarming phase; HBO has an anti-infective activity due to its bactericidal effect on anaerobic germs and bacteriostatic action on aerobic germs so it can prevent infection during the mummification phase [
12,
28]. Finally, when repeated every day, HBO sessions induce vascular endothelium growth factor activation, fibroblast and collagen production, and thus the progression toward the resolution of tissue damage. HBO promotes the formation of the healing sulcus between necrotic and healthy tissues [
12,
28]. These clinical effects were described in recent retrospective studies [
13].
Regarding the longer delay for medical care in the prospective cohort, the second aim of this INTERREG project was to set up a network for severe frostbite management. A SOS-Frostbite call center has been created. Some patients have been repatriated from far away to benefit from this research protocol, which could explain the longer delay for medical care from frostbite injury in the SOS-Frostbite group. Despite the longer delay for medical care in the SOS-Frostbite group, segment salvage was still significantly improved.
5. Conclusions
The SOS-Frostbite program is the first controlled prospective study that evaluates the effect of early HBO additive to iloprost on severe frostbite. Results show more favorable outcome in terms of the functionality and quality of life in patients treated by HBO: HBO added to the standard care with iloprost might improve frostbite injury outcomes by doubling the chance to preserve the number of injured segments from amputation.
Moreover, the benefits of HBO frequently outweigh the risks as contraindications and side effects are limited, in comparison to standard treatments such as rt-PA and iloprost. Transferring the patient suffering from severe frostbite to a hyperbaric center could be considered even if it implies delayed HBO, as it still improves frostbite outcomes after 48 h. Our findings should be tested in a randomized controlled trial before concluding that HBO should be added to standard care of severe frostbite in patients receiving iloprost.
6. Patents
The decision to design a prospective single arm study instead of two-arm randomized study was made because severe frostbite is an infrequent event [
1,
2]. We collected data on a small sample of 28 patients prospectively and compared the prospective cohort with data from a retrospective cohort from a previous double blinded RCT [
5]. In both series, patients were mostly healthy, had little comorbidity, and had good access to medical care. Frostbite also occurs secondary to occupational exposure and in the homeless and migrant populations. The prognosis and outcome of frostbite for members of socially disadvantaged groups is likely much more severe. The fact our patients were healthy was an advantage, as frostbite was the only injury studied, inducing less bias from other pathologies. The Lyon hyperbaric site was more focused on the treatment of occupational accidents and injuries sustained by homeless patients. These patients were often hospitalized on medical services to treat comorbid conditions with an unfortunate delay in frostbite treatment. These patients were excluded if frostbite treatment was not initiated with 72 h.
Our study was not a randomized controlled trial. We tried to minimize selection and information biases using strict eligibility criteria. The allocation of the treatment group was not at random in our study, but we prespecified a list of criteria to select patients with very similar characteristics in this observational study in order to allow an unbiased comparison of treatment effects between the two treatment groups.
The two groups have a comparable number of patients, but those from the prospective group were older, had more severe frostbite, and the medical care delay was longer in comparison with the control group.
Another hypothesis is that HBO might prevent other side effects such as early arthritis by augmenting the healing process. It is still too early to present data, and it will not be possible to compare data with the historical cohort as there was no long-term follow up over 12 months.
Author Contributions
Conceptualization M.-A.M., R.P. and F.C.; methodology M.-A.M., R.P., P.L. and F.C.; software: C.L.; validation, M.-A.M., A.G.-A., P.L., F.C., T.J., C.L. and R.P.; formal analysis, A.G.-A.; investigation M.-A.M., P.L., F.C. and T.J.; data curation R.P. and M.-A.M.; writing—original draft preparation M.-A.M. and A.G.-A.; writing—review and editing, M.-A.M., A.G.-A., P.L. and R.P.; visualization M.-A.M., R.P. and P.L.; supervision M.-A.M. and R.P.; project administration: M.-A.M.; funding acquisition M.-A.M., R.P. and F.C. All authors have read and agreed to the published version of the manuscript.
Funding
The SOS-Frostbite program had financial support by the Interreg IV France-Switzerland and the Swiss Confederation. The Interreg committee and the Swiss Confederation had no influence on the design and the conduct of the trial and were not involved in data collection or analysis in writing of or submitting the manuscript. There was no commercial support for this study.
Institutional Review Board Statement
This trial was conducted according to the guidelines of the Declaration of Helsinki and was approved by the institutional review board at the University of Geneva and the French Committee on the Protection of the Persons in Biomedical Research (CCPPRB) approved the study protocol (protocol code 14-053 on 14 October 2015).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study and written informed consent form has been obtained from the patient(s) to publish this paper. Each patient received oral and written information about the treatment and signed a written consent form.
Data Availability Statement
All data from the prospective and the historical cohorts were collected on site using a standardized case report form in the international frostbite registry. All observations were coded to preserve patient anonymity and data confidentiality.
Acknowledgments
We honor the memory of Emmanuel Cauchy, who unfortunately died in an avalanche in 2018. He was a medical doctor specialized in mountain medicine and a mountain guide. He initiated the SOS-Frostbite program in 2013. We thank the INTERREG France-Suisse IV program and the Swiss Confederation for its financial support.
Conflicts of Interest
The authors declare no conflict of interest. The Interreg committee and the Swiss Confederation had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Appendix A
Figure A1.
The SOS-Frostbite protocol during hospitalization at university hospitals of Geneva.
Figure A1.
The SOS-Frostbite protocol during hospitalization at university hospitals of Geneva.
References
- Brustia, R.; Enrione, G.; Catuzzo, B.; Cavoretto, L.; Campagnoni, M.P.; Visetti, E.; Cauchy, E.; Ziegler, S.; Giardini, G.; on behalf of RESAMONT 2 Project Group. Results of a Prospective Observational Study on Mountaineering Emergencies in Western Alps: Mind Your Head. High Alt. Med. Biol. 2016, 17, 116–121. [Google Scholar] [CrossRef]
- Hallam, M.-J.; Cubison, T.; Dheansa, B.; Imray, C. Managing frostbite. BMJ 2010, 341, c5864. [Google Scholar] [CrossRef] [PubMed]
- Cauchy, E.; Chetaille, E.; Marchand, V.; Marsigny, B. Retrospective study of 70 cases of severe frostbite lesions: A proposed new classification scheme. Wilderness Environ. Med. 2001, 12, 248–255. [Google Scholar] [CrossRef] [Green Version]
- Bruen, K.J. Reduction of the Incidence of Amputation in Frostbite Injury with Thrombolytic Therapy. Arch. Surg. 2007, 142, 546–553. [Google Scholar] [CrossRef] [Green Version]
- Cauchy, E.; Cheguillaume, B.; Chetaille, E. A Controlled Trial of a Prostacyclin and rt-PA in the Treatment of Severe Frostbite. N. Engl. J. Med. 2011, 364, 189–190. [Google Scholar] [CrossRef] [Green Version]
- Irarrázaval, S.; Besa, P.; Cauchy, E.; Pandey, P.; Vergara, J. Case Report of Frostbite with Delay in Evacuation: Field Use of Iloprost Might Have Improved the Outcome. High Alt. Med. Biol. 2018, 19, 382–387. [Google Scholar] [CrossRef]
- Cauchy, E.; Davis, C.B.; Pasquier, M.; Meyer, E.F.; Hackett, P.H. A New Proposal for Management of Severe Frostbite in the Austere Environment. Wilderness Environ. Med. 2016, 27, 92–99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McIntosh, S.E.; Freer, L.; Grissom, C.K.; Auerbach, P.S.; Rodway, G.W.; Cochran, A.; Giesbrecht, G.G.; McDevitt, M.; Imray, C.H.; Johnson, E.L.; et al. Wilderness Medical Society Practice Guidelines for the prevention and treatment of Frostbite: 2019 up-date. Wilderness Environ. Med. 2019, 30, S19–S32. [Google Scholar] [CrossRef] [Green Version]
- Millet, J.D.; Brown, R.K.J.; Levi, B.; Kraft, C.T.; Jacobson, J.A.; Gross, M.D.; Wong, K.K. Frostbite: Spectrum of Imaging Findings and Guidelines for Management. Radiographics 2016, 36, 2154–2169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonzaga, T.; Jenabzadeh, K.; Anderson, C.P.; Mohr, W.J.; Endorf, F.W.; Ahrenholz, D.H. Use of Intra-arterial Thrombolytic Therapy for Acute Treatment of Frostbite in 62 Patients with Review of Thrombolytic Therapy in Frostbite. J. Burn. Care Res. 2016, 37, e323–e334. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Poole, A.; Gauthier, J. Treatment of severe frostbite with iloprost in northern Canada. Can. Med Assoc. J. 2016, 188, 1255–1258. [Google Scholar] [CrossRef] [Green Version]
- Camporoso, E.; Bosco, G. Mechanisms of action of hyperbaric oxygen therapy. Undersea Hyperb. Med. 2014, 41, 247–252. [Google Scholar] [PubMed]
- Ghumman, A.; Denis-Katz, H.S.; Ashton, R.; Wherrett, C.; Malic, C. Treatment of Frostbite With Hyperbaric Oxygen Therapy: A Single Center’s Experience of 22 Cases. Wounds 2019, 31, 322–325. [Google Scholar] [PubMed]
- Gage, A.A.; Ishikawa, H.; Winter, P.M. Experimental frostbite. The effect of hyperbaric oxygenation on tissue survival. Cryo Biol. 1970, 7, 1–8. [Google Scholar] [CrossRef]
- Okuboye, A.J.; Ferguson, C.C. The use of hyperbaric oxygen in the treatment of experimental frostbite. Can. J. Surg. 1968, 11, 78–84. [Google Scholar] [PubMed]
- Higdon, B.; Youngman, L.; Regehr, M.; Chiou, A. Deep Frostbite Treated With Hyperbaric Oxygen and Thrombolytic Thera-pies. Wounds 2015, 27, 215–223. [Google Scholar] [PubMed]
- Singhal, S.; Dwivedi, D.A.; Alasinga, S.; Malhotra, V.K.; Kotwal, A. Successful treatment of frostbite with hyperbaric oxygen treatment. Indian J. Occup. Environ. Med. 2015, 19, 121–122. [Google Scholar] [CrossRef] [Green Version]
- Lansdorp, A.C.; Roukema, G.R.; Boonstra, O.; Dokter, J.; Van Der Vlies, C.H. Delayed treatment of frostbite with hyperbaric oxygen: A report of two cases. Undersea Hyperb. Med. 2017, 44, 365–369. [Google Scholar] [CrossRef]
- Kemper, T.C.P.M.; De Jong, V.M.; Anema, A.H.; Brink, A.V.D.; Van Hulst, A.R. Frostbite of both first digits of the foot treated with delayed hyperbaric oxygen:a case report and review of literature. Undersea Hyperb. Med. 2014, 41, 65–70. [Google Scholar]
- Finderle, Z.; Cankar, K. Delayed treatment of frostbite injury with hyperbaric oxygen therapy: A case report. Aviat. Space Environ. Med. 2002, 73, 392–394. [Google Scholar]
- Robins, M. Early treatment of frostbite with hyperbaric oxygen and pentoxifylline: A case report. Undresea Hyperb. Med. 2019, 46, 521–526. [Google Scholar]
- Robins, M.; Cooper, J.S. Hyperbaric Management of Frostbite; StatPearls (Internet); StatPearls: Treasure Island, FL, USA, 2019. [Google Scholar]
- Cauchy, E.; Leal, S.; Magnan, M.-A.; Nespoulet, H. Portable Hyperbaric Chamber and Management of Hypothermia and Frostbite: An Evident Utilization. High Alt. Med. Biol. 2014, 15, 95–96. [Google Scholar] [CrossRef] [PubMed]
- Lindford, A.; Valtonen, J.; Hult, M.; Kavola, H.; Lappalainen, K.; Lassila, R.; Aho, P.; Vuola, J. The evolution of the Helsinki frostbite management protocol. Burn 2017, 43, 1455–1463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heyboer, M.; Sharma, D.; Santiago, W.; McCulloch, N. Hyperbaric Oxygen Therpay/Side Effects Defined and Quantified. Adv. Wound Care 2017, 6, 210–224. [Google Scholar] [CrossRef] [Green Version]
- Haapaniemi, T.; Nylander, G.; Sirsjö, A.; Larsson, J. Hyperbaric Oxygen Reduces Ischemia-Induced Skeletal Muscle Injury. Plast. Reconstr. Surg. 1996, 97, 602–607. [Google Scholar] [CrossRef]
- Hentia, C.; Rizzato, A.; Camporesi, E.; Yang, Z.; Muntean, D.M.; Săndesc, D.; Bosco, G. An overview of protective strategies against ischemia/reperfusion injury: The role of hyperbaric oxygen preconditioning. Brain Behav. 2018, 8, e00959. [Google Scholar] [CrossRef]
- Mark, W.J.; Jeffrey, S.C. Hyperbaric Therapy for Wound Healing; Statpearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).