Antisocial Personality Disorder in Bipolar Disorder: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Assessment of Study Quality
2.3. Selection Criteria
2.4. Data Collection and Extraction
3. Results
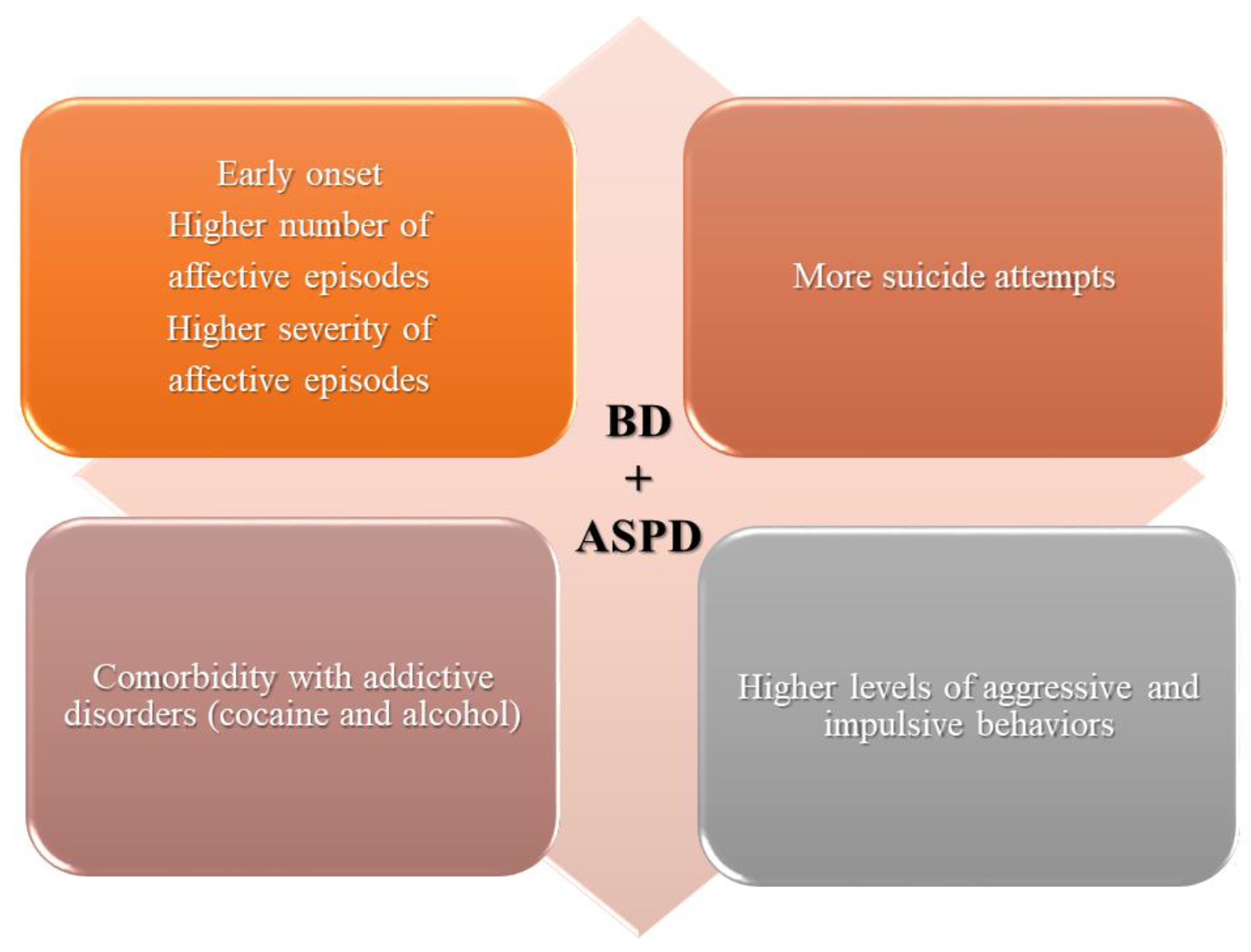
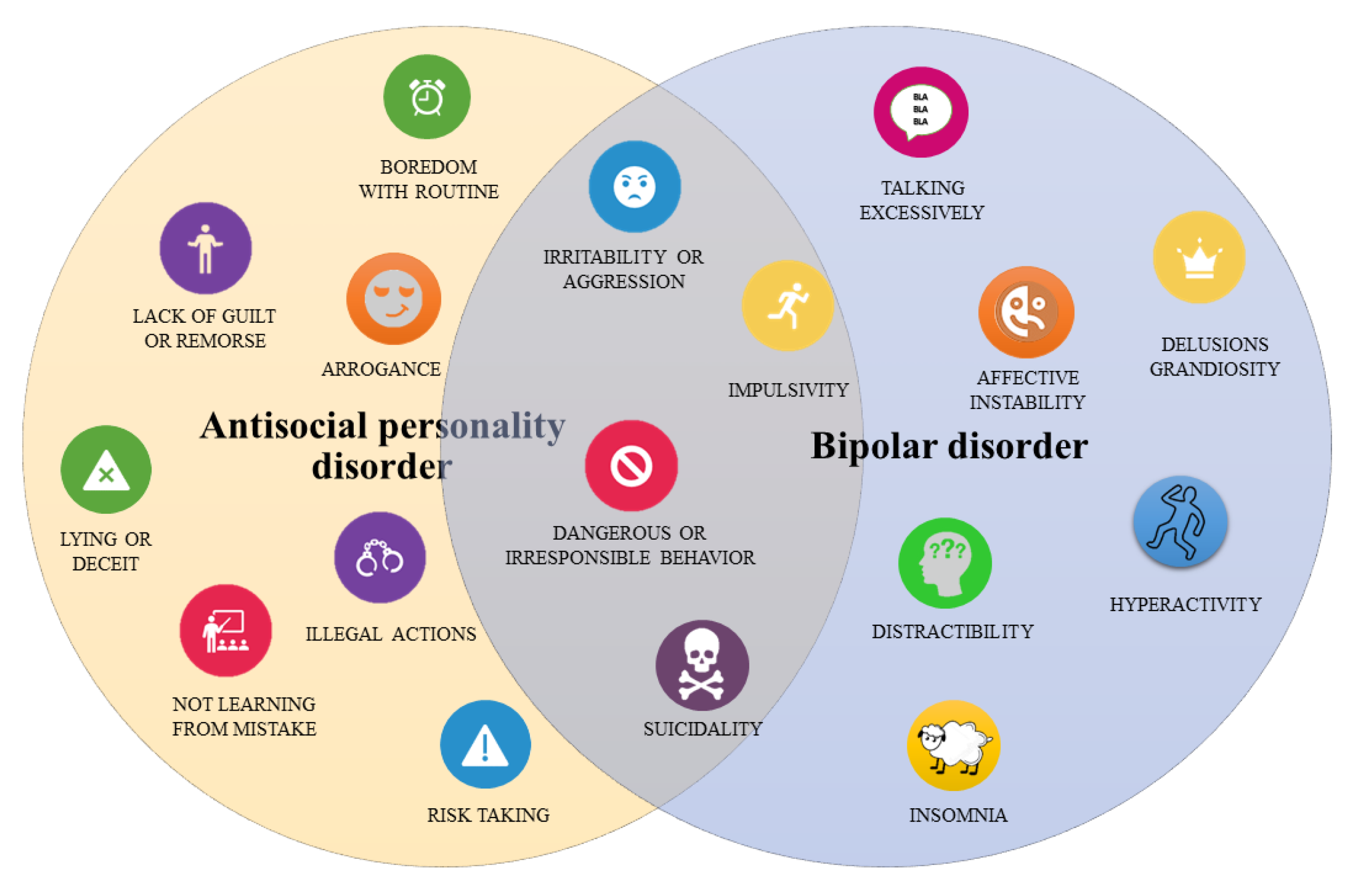
4. Discussion
Limits and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grande, I.; Berk, M.; Birmaher, B.; Vieta, E. Bipolar disorder. Lancet 2016, 387, 1561–1572. [Google Scholar] [CrossRef]
- Jann, M.W. Diagnosis and treatment of bipolar disorders in adults: A review of the evidence on pharmacologic treatments. Am. Health Drug Benefits 2014, 7, 489–499. [Google Scholar] [PubMed]
- Merikangas, K.R.; Jin, R.; He, J.-P.; Kessler, R.C.; Lee, S.; Sampson, N.A.; Viana, M.C.; Andrade, L.H.; Hu, C.; Karam, E.G.; et al. Prevalence and Correlates of Bipolar Spectrum Disorder in the World Mental Health Survey Initiative. Arch. Gen. Psychiatry 2011, 68, 241. [Google Scholar] [CrossRef] [PubMed]
- Koirala, P.; Hu, B.; Altinay, M.; Li, M.; DiVita, A.L.; Bryant, K.A.; Karne, H.S.; Fiedorowicz, J.G.; Anand, A. Sub-threshold bipolar disorder in medication-free young subjects with major depression: Clinical characteristics and antidepressant treatment response. J. Psychiatr. Res. 2019, 110, 1–8. [Google Scholar] [CrossRef]
- Sinha, A.; Shariq, A.; Said, K.; Sharma, A.; Jeffrey Newport, D.; Salloum, I.M. Medical Comorbidities in Bipolar Disorder. Curr. Psychiatry Rep. 2018, 20, 36. [Google Scholar] [CrossRef] [PubMed]
- Judd, L.L.; Akiskal, H.S.; Schettler, P.J.; Endicott, J.; Maser, J.; Solomon, D.A.; Leon, A.C.; Rice, J.A.; Keller, M.B. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch. Gen. Psychiatry 2002, 59, 530–537. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Fitzgerald, H.M.; Madera, J.J.; Tohen, M. Functional outcome assessment in bipolar disorder: A systematic literature review. Bipolar Disord. 2019, 21, 194–214. [Google Scholar] [CrossRef] [PubMed]
- Amerio, A.; Odone, A.; Tonna, M.; Stubbs, B.; Ghaemi, S.N. Bipolar disorder and its comorbidities between Feinstein and the Diagnostic and Statistical Manual of Mental Disorders. Aust. N. Z. J. Psychiatry 2015, 49, 1073. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Di Florio, A.; Craddock, N.; van den Bree, M. Alcohol misuse in bipolar disorder. A systematic review and meta-analysis of comorbidity rates. Eur. Psychiatry 2014, 29, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Hunt, G.E.; Malhi, G.S.; Cleary, M.; Lai, H.M.X.; Sitharthan, T. Prevalence of comorbid bipolar and substance use disorders in clinical settings, 1990-2015: Systematic review and meta-analysis. J. Affect. Disord. 2016, 206, 331–349. [Google Scholar] [CrossRef] [PubMed]
- Hunt, G.E.; Malhi, G.S.; Cleary, M.; Lai, H.M.X.; Sitharthan, T. Comorbidity of bipolar and substance use disorders in national surveys of general populations, 1990–2015: Systematic review and meta-analysis. J. Affect. Disord. 2016, 206, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Nabavi, B.; Mitchell, A.J.; Nutt, D. A Lifetime Prevalence of Comorbidity Between Bipolar Affective Disorder and Anxiety Disorders: A Meta-analysis of 52 Interview-based Studies of Psychiatric Population. EBioMedicine 2015, 2, 1405–1419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pavlova, B.; Perlis, R.H.; Mantere, O.; Sellgren, C.M.; Isometsä, E.; Mitchell, P.B.; Alda, M.; Uher, R. Prevalence of current anxiety disorders in people with bipolar disorder during euthymia: A meta-analysis. Psychol. Med. 2017, 47, 1107–1115. [Google Scholar] [CrossRef] [PubMed]
- Forty, L.; Ulanova, A.; Jones, L.; Jones, I.; Gordon-Smith, K.; Fraser, C.; Farmer, A.; McGuffin, P.; Lewis, C.M.; Hosang, G.M.; et al. Comorbid medical illness in bipolar disorder. Br. J. Psychiatry 2014, 205, 465–472. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McElroy, S.L.; Altshuler, L.L.; Suppes, T.; Keck, P.E.; Frye, M.A.; Denicoff, K.D.; Nolen, W.A.; Kupka, R.W.; Leverich, G.S.; Rochussen, J.R.; et al. Axis I psychiatric comorbidity and its relationship to historical illness variables in 288 patients with bipolar disorder. Am. J. Psychiatry 2001, 158, 420–426. [Google Scholar] [CrossRef] [PubMed]
- Preti, A.; Vrublevska, J.; Veroniki, A.A.; Huedo-Medina, T.B.; Kyriazis, O.; Fountoulakis, K.N. Prevalence and treatment of panic disorder in bipolar disorder: Systematic review and meta-analysis. Evid. Based. Ment. Health 2018, 21, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, R.B.; Compton, W.M.; Grant, B.F. Antisocial Behavioral Syndromes and Additional Psychiatric Comorbidity in Posttraumatic Stress Disorder Among U.S. Adults: Results From Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J. Am. Psychiatr. Nurses Assoc. 2010, 16, 145–165. [Google Scholar] [CrossRef]
- Hossain, S.; Mainali, P.; Bhimanadham, N.N.; Imran, S.; Ahmad, N.; Patel, R.S. Medical and Psychiatric Comorbidities in Bipolar Disorder: Insights from National Inpatient Population-based Study. Cureus 2019, 11, e5636. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maina, G.; Albert, U.; Pessina, E.; Bogetto, F. Bipolar obsessive-compulsive disorder and personality disorders. Bipolar Disord. 2007, 9, 722–729. [Google Scholar] [CrossRef] [PubMed]
- Simon, N.M.; Otto, M.W.; Wisniewski, S.R.; Fossey, M.; Sagduyu, K.; Frank, E.; Sachs, G.S.; Nierenberg, A.A.; Thase, M.E.; Pollack, M.H. Anxiety disorder comorbidity in bipolar disorder patients: Data from the first 500 participants in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Am. J. Psychiatry 2004, 161, 2222–2229. [Google Scholar] [CrossRef] [PubMed]
- Thiebaut, S.; Godart, N.; Radon, L.; Courtet, P.; Guillaume, S. Crossed prevalence results between subtypes of eating disorder and bipolar disorder: A systematic review of the literature. Encephale 2019, 45, 60–73. [Google Scholar] [CrossRef] [PubMed]
- Pinna, M.; Visioli, C.; Rago, C.M.; Manchia, M.; Tondo, L.; Baldessarini, R.J. Attention deficit-hyperactivity disorder in adult bipolar disorder patients. J. Affect. Disord. 2019, 243, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Cerimele, J.M.; Bauer, A.M.; Fortney, J.C.; Bauer, M.S. Patients with co-occurring bipolar disorder and posttraumatic stress disorder: A rapid review of the literature. J. Clin. Psychiatry 2017, 78, e506–e514. [Google Scholar] [CrossRef] [PubMed]
- Bezerra-Filho, S.; Almeida, A.G.; Studart, P.; Rocha, M.V.; Lopes, F.L.; Miranda-Scippa, Â. Personality disorders in euthymic bipolar patients: A systematic review. Rev. Bras. Psiquiatr. 2015, 37, 162–167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fan, A.H.; Hassell, J. Bipolar disorder and comorbid personality psychopathology: A review of the literature. J. Clin. Psychiatry 2008, 69, 1794–1803. [Google Scholar] [CrossRef] [PubMed]
- Harnic, D.; Catalano, V.; Mazza, M.; Janiri, L.; Bria, P. An observational study evaluating comorbidity between bipolar disorder and personality disorders. Clin. Ter. 2010, 161, 51–54. [Google Scholar] [PubMed]
- Friborg, O.; Martinsen, E.W.; Martinussen, M.; Kaiser, S.; Øvergård, K.T.; Rosenvinge, J.H. Comorbidity of personality disorders in mood disorders: A meta-analytic review of 122 studies from 1988 to 2010. J. Affect. Disord. 2014, 152–154, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Fowler, J.C.; Madan, A.; Allen, J.G.; Oldham, J.M.; Frueh, B.C. Differentiating bipolar disorder from borderline personality disorder: Diagnostic accuracy of the difficulty in emotion regulation scale and personality inventory for DSM-5. J. Affect. Disord. 2019, 245, 856–860. [Google Scholar] [CrossRef] [PubMed]
- Quanbeck, C.D.; Stone, D.C.; Scott, C.L.; McDermott, B.E.; Altshuler, L.L.; Frye, M.A. Clinical and legal correlates of inmates with bipolar disorder at time of criminal arrest. J. Clin. Psychiatry 2004, 65, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Yen, S.; Frazier, E.; Hower, H.; Weinstock, L.M.; Topor, D.R.; Hunt, J.; Goldstein, T.R.; Goldstein, B.I.; Gill, M.K.; Ryan, N.D.; et al. Borderline personality disorder in transition age youth with bipolar disorder. Acta Psychiatr. Scand. 2015, 132, 270–280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Post, R.M.; McElroy, S.; Kupka, R.; Suppes, T.; Hellemann, G.; Nolen, W.; Frye, M.; Keck, P.; Grunze, H.; Rowe, M. Axis II personality disorders are linked to an adverse course of bipolar disorder. J. Nerv. Ment. Dis. 2018, 206, 469–472. [Google Scholar] [CrossRef] [PubMed]
- Latalova, K.; Prasko, J.; Kamaradova, D.; Sedlackova, J.; Ociskova, M. Comorbidity bipolar disorder and personality disorders. Neuro Endocrinol. Lett. 2013, 34, 1–8. [Google Scholar]
- Fazel, S.; Lichtenstein, P.; Grann, M.; Goodwin, G.M.; Långström, N. Bipolar disorder and violent crime: New evidence from population-based longitudinal studies and systematic review. Arch. Gen. Psychiatry 2010, 67, 931–938. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Apfelbaum, S.; Regalado, P.; Herman, L.; Teitelbaum, J.; Gagliesi, P. Comorbidity between Bipolar Disorder and Cluster B Personality Disorders as indicator of affective dysregulation and clinical severity. Actas Esp. Psiquiatr. 2013, 41, 269–278. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. DSM-5, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Samuels, J.; Eaton, W.W.; Bienvenu, O.J.; Brown, C.H.; Costa, P.T.; Nestadt, G. Prevalence and correlates of personality disorders in a community sample. Br. J. Psychiatry 2002, 180, 536–542. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lenzenweger, M.F. Current status of the scientific study of the personality disorders: An overview of epidemiological, longitudinal, experimental psychopathology, and neurobehavioral perspectives. J. Am. Psychoanal. Assoc. 2010, 58, 741–778. [Google Scholar] [CrossRef] [PubMed]
- Etain, B.; Mathieu, F.; Liquet, S.; Raust, A.; Cochet, B.; Richard, J.R.; Gard, S.; Zanouy, L.; Kahn, J.P.; Cohen, R.F.; et al. Clinical features associated with trait-impulsiveness in euthymic bipolar disorder patients. J. Affect. Disord. 2013, 144, 240–247. [Google Scholar] [CrossRef] [PubMed]
- Turner, D.; Sebastian, A.; Tüscher, O. Impulsivity and Cluster B Personality Disorders. Curr. Psychiatry Rep. 2017, 19, 15. [Google Scholar] [CrossRef] [PubMed]
- Helle, A.C.; Watts, A.L.; Trull, T.J.; Sher, K.J. Alcohol use disorder and antisocial and borderline personality disorders. Alcohol Res. Curr. Rev. 2019, 40, e1–e16. [Google Scholar] [CrossRef] [PubMed]
- González, E.; Arias, F.; Szerman, N.; Vega, P.; Mesias, B.; Basurte, I. Coexistence between personality disorders and substance use disorder. Madrid study about prevalence of dual pathology. Actas Esp. Psiquiatr. 2019, 47, 218–228. [Google Scholar]
- Messer, T.; Lammers, G.; Müller-Siecheneder, F.; Schmidt, R.F.; Latifi, S. Substance abuse in patients with bipolar disorder: A systematic review and meta-analysis. Psychiatry Res. 2017, 253, 338–350. [Google Scholar] [CrossRef]
- Fovet, T.; Geoffroy, P.A.; Vaiva, G.; Adins, C.; Thomas, P.; Amad, A. Individuals with bipolar disorder and their relationship with the criminal justice system: A critical review. Psychiatr. Serv. 2015, 66, 348–353. [Google Scholar] [CrossRef] [PubMed]
- Spaans, M.; Barendregt, M.; Haan, B.; Nijman, H.; de Beurs, E. Diagnosis of antisocial personality disorder and criminal responsibility. Int. J. Law Psychiatry 2011, 34, 374–378. [Google Scholar] [CrossRef] [PubMed]
- Icick, R.; Melle, I.; Etain, B.; Ringen, P.A.; Aminoff, S.R.; Leboyer, M.; Aas, M.; Henry, C.; Bjella, T.D.; Andreassen, O.A.; et al. Tobacco smoking and other substance use disorders associated with recurrent suicide attempts in bipolar disorder. J. Affect. Disord. 2019, 256, 348–357. [Google Scholar] [CrossRef] [PubMed]
- Links, P.S.; Gould, B.; Ratnayake, R. Assessing suicidal youth with antisocial, borderline, or narcissistic personality disorder. Can. J. Psychiatry 2003, 48, 301–310. [Google Scholar] [CrossRef] [PubMed]
- Swann, A.C.; Lijffijt, M.; Lane, S.D.; Steinberg, J.L.; Moeller, F.G. Interactions between bipolar disorder and antisocial personality disorder in trait impulsivity and severity of illness. Acta Psychiatr. Scand. 2010, 121, 453–461. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, J.D.; Brown, E.S.; Rush, A.J. Comorbid disorders in patients with bipolar disorder and concomitant substance dependence. J. Affect. Disord. 2007, 102, 281–287. [Google Scholar] [CrossRef] [Green Version]
- Lev-Ran, S.; Le Foll, B.; McKenzie, K.; George, T.P.; Rehm, J. Bipolar disorder and co-occurring cannabis use disorders: Characteristics, co-morbidities and clinical correlates. Psychiatry Res. 2013, 209, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Glenn, A.L.; Johnson, A.K.; Raine, A. Antisocial Personality Disorder: A Current Review. Curr. Psychiatry Rep. 2013, 15, 427. [Google Scholar] [CrossRef] [PubMed]
- Fridell, M.; Hesse, M.; Jæger, M.M.; Kühlhorn, E. Antisocial personality disorder as a predictor of criminal behaviour in a longitudinal study of a cohort of abusers of several classes of drugs: Relation to type of substance and type of crime. Addict. Behav. 2008, 33, 799–811. [Google Scholar] [CrossRef] [PubMed]
- Swann, A.C. Antisocial personality and bipolar disorder: Interactions in impulsivity and course of illness. Neuropsychiatry (London) 2011, 1, 599–610. [Google Scholar] [CrossRef] [Green Version]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. Br. Med. J. 2009, 339, b2700. [Google Scholar] [CrossRef] [Green Version]
- Pluye, P.; Gagnon, M.P.; Griffiths, F.; Johnson-Lafleur, J. A scoring system for appraising mixed methods research, and concomitantly appraising qualitative, quantitative and mixed methods primary studies in Mixed Studies Reviews. Int. J. Nurs. Stud. 2009, 46, 529–546. [Google Scholar] [CrossRef]
- Hong, Q.N.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.P.; Griffiths, F.; Nicolau, B.; O’Cathain, A.; et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ. Inf. 2018, 34, 285–291. [Google Scholar] [CrossRef] [Green Version]
- Turley, B.; Bates, G.W.; Edwards, J.; Jackson, H.J. MCMI-II personality disorders in recent-onset bipolar disorders. J. Clin. Psychol. 1992, 48, 320–329. [Google Scholar] [CrossRef]
- Goldstein, R.B.; Chou, S.P.; Saha, T.D.; Smith, S.M.; Jung, J.; Zhang, H.; Pickering, R.P.; Ruan, W.J.; Huang, B.; Grant, B.F. The Epidemiology of Antisocial Behavioral Syndromes in Adulthood. J. Clin. Psychiatry 2017, 78, 90–98. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Swann, A.C.; Lijffijt, M.; Lane, S.D.; Steinberg, J.L.; Moeller, F.G. Antisocial personality disorder and borderline symptoms are differentially related to impulsivity and course of illness in bipolar disorder. J. Affect. Disord. 2013, 148, 384–390. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mueser, K.T.; Gottlieb, J.D.; Cather, C.; Glynn, S.M.; Zarate, R.; Smith, M.F.; Clark, R.E.; Wolfe, R. Antisocial personality disorder in people with co-occurring severe mental illness and substance use disorders: Clinical, functional, and family relationship correlates. Psychosis 2012, 4, 52–62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garno, J.L.; Gunawardane, N.; Goldberg, J.F. Predictors of trait aggression in bipolar disorder. Bipolar Disord. 2008, 10, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Swann, A.C.; Lijffijt, M.; Lane, S.D.; Steinberg, J.L.; Moeller, F.G. Interacting mechanisms of impulsivity in bipolar disorder and antisocial personality disorder. J. Psychiatr. Res. 2011, 45, 1477–1482. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perugi, G.; Toni, C.; Maremmani, I.; Tusini, G.; Ramacciotti, S.; Madia, A.; Fornaro, M.; Akiskal, H.S. The influence of affective temperaments and psychopathological traits on the definition of bipolar disorder subtypes: A study on Bipolar I Italian National sample. J. Affect. Disord. 2012, 136, e41–e49. [Google Scholar] [CrossRef] [PubMed]
- Garno, J.L.; Goldberg, J.F.; Ramirez, P.M.; Ritzler, B.A. Bipolar disorder with comorbid cluster B personality disorder features: Impact on suicidality. J. Clin. Psychiatry 2005, 66, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Mueser, K.T.; Crocker, A.G.; Frisman, L.B.; Drake, R.E.; Covell, N.H.; Essock, S.M. Conduct disorder and antisocial personality disorder in persons with severe psychiatric and substance use disorders. Schizophr. Bull. 2006, 32, 626–636. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mueser, K.T.; Rosenberg, S.D.; Drake, R.E.; Miles, K.M.; Wolford, G.; Vidaver, R.; Carrieri, K. Conduct disorder, antisocial personality disorder and substance use disorders in schizophrenia and major affective disorders. J. Stud. Alcohol. 1999, 60, 278–284. [Google Scholar] [CrossRef] [PubMed]
- Jackson, H.J.; Pica, S. An investigation into the internal structure of DSM-III antisocial personality disorder. Psychol. Rep. 1993, 72, 355–367. [Google Scholar] [CrossRef] [PubMed]
- Pica, S.; Edwards, J.; Jackson, H.J.; Bell, R.C.; Bates, G.W.; Rudd, R.P. Personality disorders in recent-onset bipolar disorder. Compr. Psychiatry 1990, 31, 499–510. [Google Scholar] [CrossRef]
- Mantere, O.; Melartin, T.K.; Suominen, K.; Rytsälä, H.J.; Valtonen, H.M.; Arvilommi, P.; Leppämäki, S.; Isometsä, E.T. Differences in Axis I and II comorbidity between bipolar I and II disorders and major depressive disorder. J. Clin. Psychiatry 2006, 67, 584–593. [Google Scholar] [CrossRef] [PubMed]
- Berk, M.; Dodd, S. Bipolar II disorder: A review. Bipolar Disord. 2005, 7, 11–21. [Google Scholar] [CrossRef]
- Ravizza, L.; Barzega, G.; Bellino, S.; Bogetto, F.; Maina, G. Predictors of drug treatment response in obsessive-compulsive disorder. J. Clin. Psychiatry 1995, 56, 368–373. [Google Scholar] [PubMed]
- Crawford, T.N.; Cohen, P.; First, M.B.; Skodol, A.E.; Johnson, J.G.; Kasen, S. Comorbid Axis I and Axis II disorders in early adolescence: Outcomes 20 years later. Arch. Gen. Psychiatry 2008, 65, 641–648. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Post, R.M.; Leverich, G.S.; McElroy, S.; Kupka, R.; Suppes, T.; Altshuler, L.; Nolen, W.; Frye, M.; Keck, P.; Grunze, H.; et al. Prevalence of axis II comorbidities in bipolar disorder: Relationship to mood state. Bipolar Disord. 2018, 20, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Dunayevich, E.; Sax, K.W.; Keck, P.E.; McElroy, S.L.; Sorter, M.T.; McConville, B.J.; Strakowski, S.M. Twelve-month outcome in bipolar patients with and without personality disorders. J. Clin. Psychiatry 2000, 61, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Leverich, G.S.; Altshuler, L.L.; Frye, M.A.; Suppes, T.; Keck, P.E.; McElroy, S.L.; Denicoff, K.D.; Obrocea, G.; Nolen, W.A.; Kupka, R.; et al. Factors associated with suicide attempts in 648 patients with bipolar disorder in the Stanley Foundation Bipolar Network. J. Clin. Psychiatry 2003, 64, 506–515. [Google Scholar] [CrossRef] [PubMed]
- Kay, J.H.; Altshuler, L.L.; Ventura, J.; Mintz, J. Impact of axis II comorbidity on the course of bipolar illness in men: A retrospective chart review. Bipolar Disord. 2002, 4, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Lembke, A.; Miklowitz, D.J.; Otto, M.W.; Zhang, H.; Wisniewski, S.R.; Sachs, G.S.; Thase, M.E.; Ketter, T.A.; STEP-BD Investigators. Psychosocial service utilization by patients with bipolar disorders: Data from the first 500 participants in the Systematic Treatment Enhancement Program. J. Psychiatr. Pract. 2004, 10, 81–87. [Google Scholar] [CrossRef]
- Jylhä, P.; Rosenström, T.; Mantere, O.; Suominen, K.; Melartin, T.; Vuorilehto, M.; Holma, M.; Riihimäki, K.; Oquendo, M.A.; Keltikangas-Järvinen, L.; et al. Personality disorders and suicide attempts in unipolar and bipolar mood disorders. J. Affect. Disord. 2016, 190, 632–639. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johansson, P.; Kerr, M.; Andershed, H. Linking adult psychopathy with childhood hyperactivity-impulsivity-attention problems and conduct problems through retrospective self-reports. J. Pers. Disord. 2005, 19, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Black, D.W. The natural history of antisocial personality disorder. Can. J. Psychiatry 2015, 60, 309–314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Connor, D.F.; Ford, J.D.; Pearson, G.S.; Scranton, V.L.; Dusad, A. Early-Onset Bipolar Disorder: Characteristics and Outcomes in the Clinic. J. Child Adolesc. Psychopharmacol. 2017, 27, 875–883. [Google Scholar] [CrossRef]
- Croarkin, P.E.; Luby, J.L.; Cercy, K.; Geske, J.R.; Veldic, M.; Simonson, M.; Joshi, P.T.; Wagner, K.D.; Walkup, J.T.; Nassan, M.M.; et al. Genetic risk score analysis in early-onset bipolar disorder. J. Clin. Psychiatry 2017, 78, 1337–1343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferguson, C.J. Genetic contributions to antisocial personality and behavior: A meta-analytic review from an evolutionary perspective. J. Soc. Psychol. 2010, 150, 160–180. [Google Scholar] [CrossRef] [PubMed]
- Shi, Z.; Bureau, J.F.; Easterbrooks, M.A.; Zhao, X.; Lyons-Ruth, K. Childhood maltreatment and prospectively observed quality of early care as predictors of antisocial personality disorder features. Infant Ment. Health J. 2012, 33, 55–69. [Google Scholar] [CrossRef]
- Agnew-Blais, J.; Danese, A. Childhood maltreatment and unfavourable clinical outcomes in bipolar disorder: A systematic review and meta-analysis. Lancet Psychiatry 2016, 3, 342–349. [Google Scholar] [CrossRef]
- Sparding, T.; Pålsson, E.; Joas, E.; Hansen, S.; Landén, M. Personality traits in bipolar disorder and influence on outcome. BMC Psychiatry 2017, 17, 159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fulwiler, C.; Grossman, H.; Forbes, C.; Ruthazer, R. Early-onset substance abuse and community violence by outpatients with chronic mental illness. Psychiatr. Serv. 1997, 48, 1181–1185. [Google Scholar] [PubMed] [Green Version]

| Authors, Years | Sample | Measurements | Results | Comments | MMAT |
|---|---|---|---|---|---|
| Goldstein et al., 2017 [57] | N = 36,309 | AUDADIS-5; SF-12 | Lifetime prevalence: ASPD + BD1: 11.8% AABS + BD1: 4.8% OR (C.I.) lifetime of BD 1 comorbidity: ASPD 2.9 (1.93–4.28) AABS 1.9 (1.43–2.50) | Comorbidity is higher in the ASPD than in the AABS. Patients with ASPD has a 3 times fold risk of BD, while it is 2 times greater if it has AABS | ***** |
| Lev-Ran et al., 2013 [49] | N = 43,093 | AUDADIS-IV; SF-12 | 12-month prevalence: BD + CUD + ASPD: 49.9% BD + No CUD + ASPD: 18.2% OR (C.I.): 2.75 (1.63–4.64) | The bipolar patient with CUD is almost 3 times more likely to have ASPD than the bipolar patient without CUD | ***** |
| Swann et al., 2013 [58] | N = 55 4 BD II 51 BD I 14 = no Axis II disorder (8 men and 6 women) 35 ASPD (20 men and 15 women) 23 Borderline 8 men and 15 women 17 (7 men and 10 women) both disorders | Diagnosis was made by Structured Clinical Interview for DSM-IV SCID-II Schedule for Affective Disorders and Schizophrenia (SADS-C) Barratt Impulsiveness Scale (BIS-11) | Prevalence: 35 ASPD of 55 BD:63% 17 ASPD + Borderline of 55: 30.9%. Number of episodes: ASPD symptoms predicted a history of many depressive and manic episodes (but not either type alone) and a early onset. BIS-11 score: Total, motor, and attentional BIS-11 scores were predicted significantly by borderline symptom scores with no significant contribution from ASPD scores. Suicide attempts: Impulsivity in ASPD + BD did not contribute significantly to history of suicide attempt SUD Comorbidity: ASPD symptoms predicted history of alcohol, other substance-abuse disorder, and smoking. | ASPD symptoms were more strongly related to course of illness (i.e., early age at onset, frequency of affective episodes, suicide attempts and substance-related disorders) but not to impulsivity. | **** |
| Mueser et al., 2012 [59] | N = 103 | SCID-II; Time-line Follow-back Calendar; AUS; DUS; SATS; BPRS; GAS; Knowledge Test; SPSI; FAS; SF-12; FEIS | Prevalence: 21 ASPD of which 11 BD: 52% | Over half of the antisocial patients are also bipolar | ***** |
| Perugi et al., 2012 [62] | N = 106 | CGI-BP; TEMPS-A; SAS; IPSM; SIMD-R | Prevalence: BD I + ASPD: 8.49% | The authors evaluated the impact of the affective phase of BD1 on axis II diagnosis, concluding that ASPD is more represented among hyperthymic than cyclothymic, depressive or euthymic patients and affective temperaments may influence both clinical features and axis I and II comorbidities. | **** |
| Swann et al., 2011 [61] | N = 133 46 HC 21 BD without personality disorders 50ASPD without BD 16BD + ASPD | Immediate Memory Task (IMT) Two Choice Impulsivity Paradigm (TCIP) | Prevalence: 16 ASPD of 37 BD: 43.24% Impulsivity: Impulsivity was increased in the combined disorders compared to both disorders alone. Outcome: In combined ASPD and BD increased reaction speed, impulsive response bias, and reward- delay impulsivity occurred. It was independent of substance-use disorder history. | The combination of ASPD and BD was associated with more impulsive TCIP performance compared to HC. Compensatory mechanisms for impulsivity in uncomplicated ASPD or BD appear to be compromised or lost when the disorders are in comorbidity. | **** |
| Goldstein et al., 2010 [17] | N = 2442 | AUDADIS-IV | Prevalence: BD1 + ASPD: 45.1% (p < 0.0001) BD2 + ASPD: 8.2% (p < 0.0122)BD1 + AABS: 32.4% BD2 + AABS: 5.8% | In subjects with PTSD and ASPD, comorbidity with DB 1 is the strongest evidence, that with DB 2, although lower, however, is statistically significant. | ***** |
| Swann et al., 2010 [47] | N = 197 78 HC 34 ASPD 61 BD 24 BD + ASPD | SCID-II; SADS-C; BIS-11 | Prevalence: 12.4% of total sampleSADS-C score: Higher scores of depression and psychosis BIS-11 score: higher subscale and total score Suicide attempts: BD + ASPD: 65.4% BD: 34.9%SUD Comorbidity: BD + ASPD: 91.3% BD: 66.7%Number of episodes: Higher number of manic and depressive episodes | Comorbidity is associated with a greater tendency to depression and psychosis, an increased number of depressive and manic episodes, greater impulsivity, greater risk of SUD and suicide. | **** |
| Garno et al., 2008 [60] | N = 100 73 BD1 27 BD2 | SCID-I; SCID-II; HDRS; YMRS; CTQ; BGA | Prevalence DB + ASPD: 6.25% Comorbidity and BGA: Higher BGA total score (p 0.008) | Bipolar patients with ASPD have more aggressive traits | **** |
| Mitchell et al., 2007 [48] | N = 166 | MINI | Prevalence ASPD in BD + SUD%; OR (C.I.): BD + COCA: 52.8%; 1.86 (0.81–4.26) BD + COCA + ALCOL:60%; 2.50 (1.23–5.08) | ASPD is more associated with the bipolar group with cocaine dependence (almost twice the risk) or cocaine plus alcohol (twice and a half risk) | **** |
| Maina et al., 2007 [19] | N = 204 BD = 21 BD I = 4; BD II = 17 BD + ASPD = 6 | Yale-Brown Obsessive-Compulsive Scale (Y-BOCS); SCID-I; SCID-II; | Prevalence DB + ASPD: 6% SUD Comorbidity: SUD + BD: 28.6%. Comorbidity: prevalence of antisocial personality disorders + BD: 28.6% | Clinically relevant effects of comorbid BD on the personality features of OCD patients. A higher rate of narcissistic and ASPD in BD/OCD patients. | **** |
| Mueser et al., 2006 [64] | N = 178 | SCID-I; SCID- II; BPRS; GAS; TLFB; ASI; AUS; DUS; SATS | Prevalence BD + AABS: 21.2% Prevalence BD + ASPD: 21.1% | The prevalence of AABS and ASPD in the DB is superimposable | **** |
| Garno et al., 2005 [63] | N = 100 73 BD1 27 BD2 | SCID-I; SCID-II; CTQ; YMRS; HAM-D; SADS-C | Prevalence BD + ASPD: 6% | There is no statistically significant correlation between YMRS and HAM-D scores with ASPD. | **** |
| Mueser et al., 1999 [65] | No ASPD/CD = 293 CD Only = 293 Adult ASPD Only = 293 Full ASPD = 293 Schizophrenia (28%), schizoaffective disorder (24%), bipolar disorder (22%), major depression. (19%) and other (7%) | SCID; MMS; CRS; MAST; DAST; CAGE; TACE; TWEAK; ACI; AUDIT. | Prevalence BD + Adult ASPD Only: 24% Prevalence BD + Full ASPD: 22% SUD Comorbidity: Full ASPD group had the highest rate of substance use disorder, followed by either the CD Only or Adult ASPD Only groups, with the No ASPD/CD group lowest | Childhood CD and adult ASPD represent independently significant risk factors for substance use disorders in patients with schizophrenia- spectrum and major affective disorders. | **** |
| Jackson & Pica, 1993 [66] | 112 psychiatric inpatients 11 antisocial personality disorder, 65 had other forms of personality disorders, 36 no personality disorder. 35 recent-onset schizophrenic patients (27 men, 6 women), 26 recent-onset bipolar disorder patients (14 men, 12 women), 30 unipolar affective disorder patients (14 men, 16 women), and 21 (11 men, 10 women) with mixed disorders (e.g., anorexia nervosa, substance abuse, somatoform disorders) | SCID, Royal Park Multidiagnostic Instrument for Psychoses, SAPS, SANS, BDI BRMS | Prevalence: 4 patients of 11 antisocial are affected by BD. | Patients with ASPD were younger, with lower level of education and higher levels of many dysfunctional behaviors, as delinquency, sexual intercourse, drink/drugs abuse, thefts, vandalism, inconsistent work, irritability/aggressive, impulsivity, recklessness, continual antisocial behavior than patients with other or none PDs. | **** |
| Turley et al., 1992 [56] | 21 recent onset BD (12 man and 9 women) | MCMI-II); SIDP; BDI; SAPS; BRMS; SCID-P | The overall ratio of personality disorders identified was virtually equivalent for the MCMI- I1 and the SIDP. However, the MCMI-I1 was far more likely to make multiple diagnoses than the SIDP. The MCMI-I1 identified a total of 52 personality disorders compared with 30 for the SIDP. | Narcissistic and Antisocial personality disorders were the most prevalent disorders in this sample of Bipolar disordered patients, followed by Histrionic and Passive-Aggressive disorders | **** |
| Pica et al., 1990 [67] | N = 26 16 BD 10 Schizoaffective Disorder | SIDP; SCID-P; RPMIP; BDI; BRMS; SAPS; SANS | Prevalence BD + ASPD: 15.39% | Patients with BD showed a high frequency of PDs. | **** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carbone, E.A.; de Filippis, R.; Caroleo, M.; Calabrò, G.; Staltari, F.A.; Destefano, L.; Gaetano, R.; Steardo, L., Jr.; De Fazio, P. Antisocial Personality Disorder in Bipolar Disorder: A Systematic Review. Medicina 2021, 57, 183. https://doi.org/10.3390/medicina57020183
Carbone EA, de Filippis R, Caroleo M, Calabrò G, Staltari FA, Destefano L, Gaetano R, Steardo L Jr., De Fazio P. Antisocial Personality Disorder in Bipolar Disorder: A Systematic Review. Medicina. 2021; 57(2):183. https://doi.org/10.3390/medicina57020183
Chicago/Turabian StyleCarbone, Elvira Anna, Renato de Filippis, Mariarita Caroleo, Giuseppina Calabrò, Filippo Antonio Staltari, Laura Destefano, Raffaele Gaetano, Luca Steardo, Jr., and Pasquale De Fazio. 2021. "Antisocial Personality Disorder in Bipolar Disorder: A Systematic Review" Medicina 57, no. 2: 183. https://doi.org/10.3390/medicina57020183
APA StyleCarbone, E. A., de Filippis, R., Caroleo, M., Calabrò, G., Staltari, F. A., Destefano, L., Gaetano, R., Steardo, L., Jr., & De Fazio, P. (2021). Antisocial Personality Disorder in Bipolar Disorder: A Systematic Review. Medicina, 57(2), 183. https://doi.org/10.3390/medicina57020183







