Perioperative Management of Chronic Antithrombotic Agents in Elective Hip and Knee Arthroplasty
Abstract
1. Introduction
2. Overview of Thromboembolism and Bleeding Events after TJA (Total Joint Arthroplasty)
3. Summary of Guidelines for Perioperative Management of Chronic Antithrombotic Agents
3.1. Classifying Surgical and Patient Bleeding and Thromboembolism Risk
3.2. Warfarin Management and Bridging
3.3. Direct Oral Anticoagulants
3.4. Anti-Platelet Medications
4. Recent Studies of Perioperative Antithrombotic Agent Management
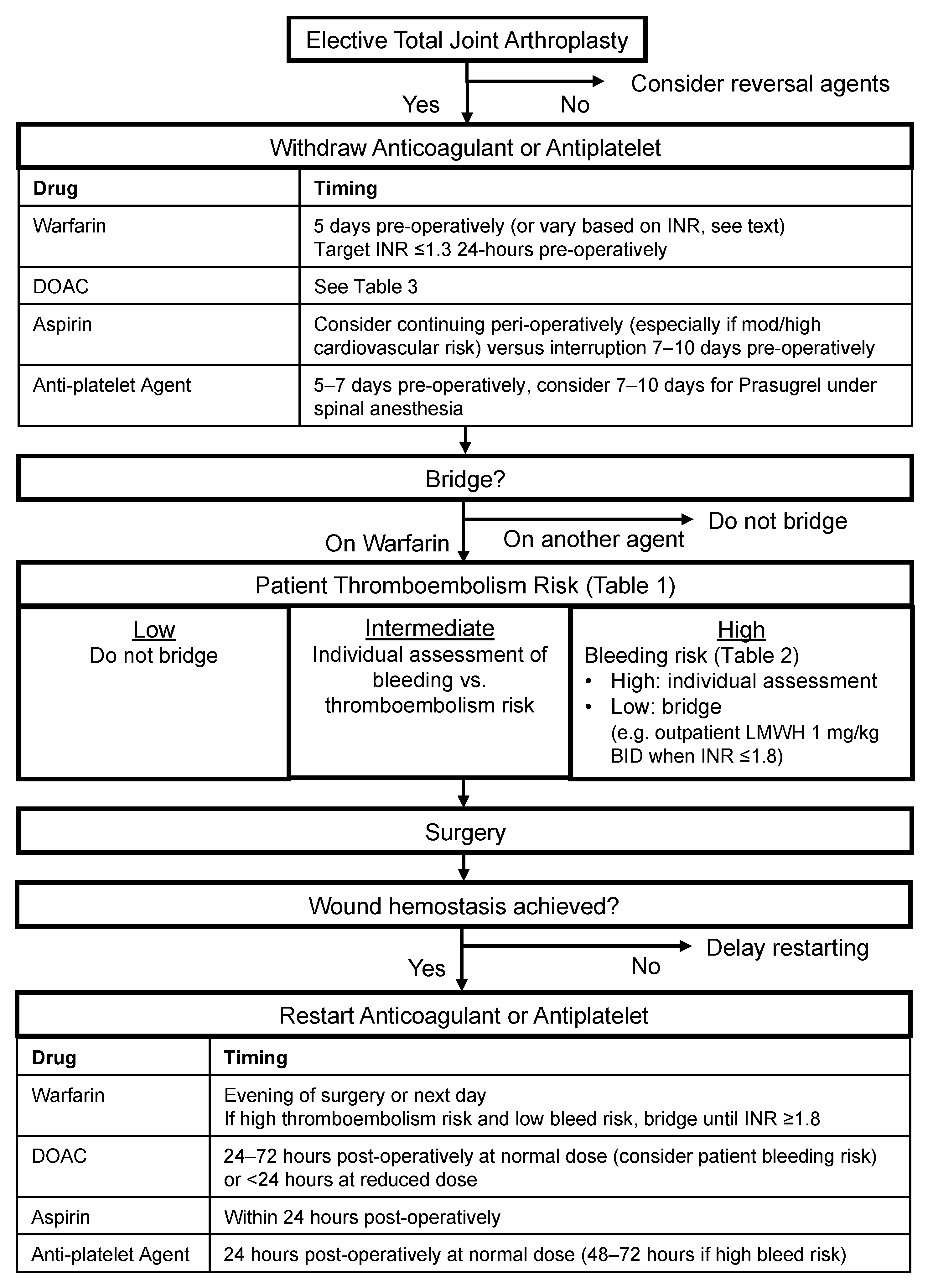
5. Proposed Algorithm for Perioperative Management of Antithrombotic Agents
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barnes, G.D.; Lucas, E.; Alexander, G.C.; Goldberger, Z.D. National trends in ambulatory oral anticoagulant use. Am. J. Med. 2015, 128, 1300–1305.e2. [Google Scholar] [CrossRef]
- Wong, S.L.; Marshall, L.Z.; Lawson, K.A. Direct oral anticoagulant prescription trends, switching patterns, and adherence in Texas medicaid. Am. J. Manag. Care 2018, 24, SP309–SP314. [Google Scholar]
- Zhu, J.; Alexander, G.C.; Nazarian, S.; Segal, J.B.; Wu, A.W. Trends and Variation in Oral Anticoagulant Choice in Patients with Atrial Fibrillation, 2010–2017. Pharmacotherapy 2018, 38, 907–920. [Google Scholar] [CrossRef] [PubMed]
- Mega, J.L.; Simon, T. Pharmacology of antithrombotic drugs: An assessment of oral antiplatelet and anticoagulant treatments. Lancet 2015, 386, 281–291. [Google Scholar] [CrossRef]
- Sloan, M.; Premkumar, A.; Sheth, N.P. Projected volume of primary total joint arthroplasty in the USA, 2014 to 2030. J. Bone Jt. Surg. Am. 2018, 100, 1455–1460. [Google Scholar] [CrossRef] [PubMed]
- Stulberg, B.N.; Insall, J.N.; Williams, G.W.; Ghelman, B. Deep-vein thrombosis following total knee replacement. An analysis of six hundred and thirty-eight arthroplasties. J. Bone Jt. Surg. Ser. A 1984, 66, 194–201. [Google Scholar] [CrossRef]
- Geerts, W.H.; Bergqvist, D.; Pineo, G.F.; Heit, J.A.; Samama, C.M.; Lassen, M.R.; Colwell, C.W. Prevention of venous thromboembolism: American College of Chest Physicians evidence-based clinical practice guidelines (8th edition). Chest 2008, 133, 381S–453S. [Google Scholar] [CrossRef]
- Shahi, A.; Chen, A.F.; Tan, T.L.; Maltenfort, M.G.; Kucukdurmaz, F.; Parvizi, J. The Incidence and Economic Burden of In-Hospital Venous Thromboembolism in the United States. J. Arthroplast. 2017, 32, 1063–1066. [Google Scholar] [CrossRef] [PubMed]
- Horlander, K.T.; Mannino, D.M.; Leeper, K.V. Pulmonary embolism mortality in the United States, 1979-1998: An analysis using multiple-cause mortality data. Arch. Intern. Med. 2003, 163, 1711–1717. [Google Scholar] [CrossRef]
- Poultsides, L.A.; Gonzalez Della Valle, A.; Memtsoudis, S.G.; Ma, Y.; Roberts, T.; Sharrock, N.; Salvati, E. Meta-analysis of cause of death following total joint replacement using different thromboprophylaxis regimens. J. Bone Jt. Surg. Br. 2012, 94, 113–121. [Google Scholar] [CrossRef]
- Zusmanovich, M.; Kester, B.S.; Schwarzkopf, R. Postoperative Complications of Total Joint Arthroplasty in Obese Patients Stratified by BMI. J. Arthroplast. 2018, 33, 856–864. [Google Scholar] [CrossRef]
- Olson, J.J.; Schwab, P.-E.; Jackson, J.; Lange, J.K.; Bedair, H.S.; Abdeen, A. HIV-Positive Patients Are at Increased Risk of Venous Thromboembolism After Total Joint Replacement. J. Am. Acad. Orthop. Surg. 2020. Publish Ahead of Print. [Google Scholar] [CrossRef] [PubMed]
- Parvizi, J.; Huang, R.; Rezapoor, M.; Bagheri, B.; Maltenfort, M.G. Individualized Risk Model for Venous Thromboembolism after Total Joint Arthroplasty. J. Arthroplast. 2016, 31, 180–186. [Google Scholar] [CrossRef] [PubMed]
- Morris, G.K.; Henry, A.P.J.; Preston, B.J. Prevention of Deep-Vein Thrombosis by Low-Dose Heparin in Patients Undergoing Total Hip Replacement. Lancet 1974, 304, 797–800. [Google Scholar] [CrossRef]
- Januel, J.M.; Chen, G.; Ruffieux, C.; Quan, H.; Douketis, J.D.; Crowther, M.A.; Colin, C.; Ghali, W.A.; Burnand, B. Symptomatic in-hospital deep vein thrombosis and pulmonary embolism following hip and knee arthroplasty among patients receiving recommended prophylaxis: A systematic review. JAMA 2012, 307, 294–303. [Google Scholar] [CrossRef]
- Cote, M.P.; Chen, A.; Jiang, Y.; Cheng, V.; Lieberman, J.R. Persistent Pulmonary Embolism Rates Following Total Knee Arthroplasty Even With Prophylactic Anticoagulants. J. Arthroplast. 2017, 32, 3833–3839. [Google Scholar] [CrossRef]
- Lu, Q.; Peng, H.; Zhou, G.J.; Yin, D. Perioperative Blood Management Strategies for Total Knee Arthroplasty. Orthop. Surg. 2018, 10, 8–16. [Google Scholar] [CrossRef]
- Merkow, R.P.; Ju, M.H.; Chung, J.W.; Hall, B.L.; Cohen, M.E.; Williams, M.V.; Tsai, T.C.; Ko, C.Y.; Bilimoria, K.Y. Underlying reasons associated with hospital readmission following surgery in the United States. JAMA 2015, 313, 483–495. [Google Scholar] [CrossRef] [PubMed]
- Clifford, L.; Jia, Q.; Yadav, H.; Subramanian, A.; Wilson, G.A.; Murphy, S.P.; Pathak, J.; Schroeder, D.R.; Ereth, M.H.; Kor, D.J. Characterizing the epidemiology of perioperative transfusion-associated circulatory overload. Anesthesiology 2015, 122, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Jenny, J.-Y.; Bulaid, Y.; Boisrenoult, P.; Bonin, N.; Henky, P.; Tracol, P.; Chouteau, J.; Courtin, C.; Henry, M.-P.; Schwartz, C.; et al. Risques thrombotique et hémorragique de la prophylaxie antithrombotique conventionnelle après prothèse totale de hanche et de genou incluses dans une procédure de récupération accélérée. Rev. Chir. Orthopédique Traumatol. 2020, 106, 971–977. [Google Scholar] [CrossRef]
- Wang, Z.; Anderson, F.A.; Ward, M.; Bhattacharyya, T. Surgical site infections and other postoperative complications following prophylactic anticoagulation in total joint arthroplasty. PLoS ONE 2014, 9, e91755. [Google Scholar] [CrossRef]
- Quintero, J.I.; Cárdenas, L.L.; Navas, M.; Bautista, M.P.; Bonilla, G.A.; Llinás, A.M. Primary Joint Arthroplasty Surgery: Is the Risk of Major Bleeding Higher in Elderly Patients? A Retrospective Cohort Study. J. Arthroplast. 2016, 31, 2264–2268. [Google Scholar] [CrossRef]
- Slover, J.; Lavery, J.A.; Schwarzkopf, R.; Iorio, R.; Bosco, J.; Gold, H.T. Incidence and Risk Factors for Blood Transfusion in Total Joint Arthroplasty: Analysis of a Statewide Database. J. Arthroplast. 2017, 32, 2684–2687.e1. [Google Scholar] [CrossRef]
- Hart, A.; Khalil, J.A.; Carli, A.; Huk, O.; Zukor, D.; Antoniou, J. Blood transfusion in primary total hip and knee arthroplasty. Incidence, risk factors, and thirty-day complication rates. J. Bone Jt. Surg. Am. 2014, 96, 1945–1951. [Google Scholar] [CrossRef] [PubMed]
- Lindquist, D.E.; Stewart, D.W.; Brewster, A.; Waldroup, C.; Odle, B.L.; Burchette, J.E.; El-Bazouni, H. Comparison of Postoperative Bleeding in Total Hip and Knee Arthroplasty Patients Receiving Rivaroxaban, Enoxaparin, or Aspirin for Thromboprophylaxis. Clin. Appl. Thromb. 2018, 24, 1315–1321. [Google Scholar] [CrossRef] [PubMed]
- Ricket, A.L.; Stewart, D.W.; Wood, R.C.; Cornett, L.; Odle, B.; Cluck, D.; Freshour, J.; El-Bazouni, H. Comparison of Postoperative Bleeding in Total Hip and Knee Arthroplasty Patients Receiving Rivaroxaban or Enoxaparin. Ann. Pharmacother. 2016, 50, 270–275. [Google Scholar] [CrossRef] [PubMed]
- Klemen, N.D.; Feingold, P.L.; Hashimoto, B.; Wang, M.; Kleyman, S.; Brackett, A.; Gross, C.P.; Pei, K.Y. Mortality risk associated with venous thromboembolism: A systematic review and Bayesian meta-analysis. Lancet Haematol. 2020, 7, e583–e593. [Google Scholar] [CrossRef]
- Murray, D.W.; Britton, A.R.; Bulstrode, C.J. Thromboprophylaxis and death after total hip replacement. J. Bone Jt. Surg. Br. 1996, 78, 863–870. [Google Scholar] [CrossRef]
- Thakur, N.A.; Czerwein, J.K.; Butera, J.N.; Palumbo, M.A. Perioperative management of chronic anticoagulation in orthopaedic surgery. J. Am. Acad. Orthop. Surg. 2010, 18, 729–738. [Google Scholar] [CrossRef]
- American Academy of Orthopaedic Surgeons. Preventing venous thromboembolic disease in patients undergoing elective hip and knee arthroplasty: Evidence-based guideline and evidence report. J. Am. Acad. Orthop. Surg. 2011, 19, 768–776. [Google Scholar] [CrossRef]
- Douketis, J.D.; Spyropoulos, A.C.; Spencer, F.A.; Mayr, M.; Jaffer, A.K.; Eckman, M.H.; Dunn, A.S.; Kunz, R. Perioperative management of antithrombotic therapy. Antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2012, 141, e326S–e350S. [Google Scholar] [CrossRef]
- Falck-Ytter, Y.; Francis, C.W.; Johanson, N.A.; Curley, C.; Dahl, O.E.; Schulman, S.; Ortel, T.L.; Pauker, S.G.; Colwell, C.W. Prevention of VTE in orthopedic surgery patients. Antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2012, 141, e278S–e325S. [Google Scholar] [CrossRef]
- Kearon, C.; Akl, E.A.; Ornelas, J.; Blaivas, A.; Jimenez, D.; Bounameaux, H.; Huisman, M.; King, C.S.; Morris, T.A.; Sood, N.; et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 2016, 149, 315–352. [Google Scholar] [CrossRef] [PubMed]
- Doherty, J.U.; Gluckman, T.J.; Hucker, W.J.; Januzzi, J.L.; Ortel, T.L.; Saxonhouse, S.J.; Spinler, S.A. 2017 ACC Expert Consensus Decision Pathway for Periprocedural Management of Anticoagulation in Patients With Nonvalvular Atrial Fibrillation: A Report of the American College of Cardiology Clinical Expert Consensus Document Task Force. J. Am. Coll. Cardiol. 2017, 69, 871–898. [Google Scholar] [CrossRef]
- Hornor, M.A.; Duane, T.M.; Ehlers, A.P.; Jensen, E.H.; Brown, P.S.; Pohl, D.; da Costa, P.M.; Ko, C.Y.; Laronga, C. American College of Surgeons’ Guidelines for the Perioperative Management of Antithrombotic Medication. J. Am. Coll. Surg. 2018, 227, 521–536.e1. [Google Scholar] [CrossRef] [PubMed]
- Horlocker, T.T.; Vandermeuelen, E.; Kopp, S.L.; Gogarten, W.; Leffert, L.R.; Benzon, H.T. Regional Anesthesia in the Patient Receiving Antithrombotic or Thrombolytic Therapy: American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines (Fourth Edition). Reg. Anesth. Pain Med. 2018, 43, 263–309. [Google Scholar] [CrossRef]
- Anderson, D.R.; Morgano, G.P.; Bennett, C.; Dentali, F.; Francis, C.W.; Garcia, D.A.; Kahn, S.R.; Rahman, M.; Rajasekhar, A.; Rogers, F.B.; et al. American Society of Hematology 2019 guidelines for management of venous thromboembolism: Prevention of venous thromboembolism in surgical hospitalized patients. Blood Adv. 2019, 3, 3898–3944. [Google Scholar] [CrossRef] [PubMed]
- Keeling, D.; Tait, R.C.; Watson, H.; British Committee of Standards for Haematology. Peri-operative management of anticoagulation and antiplatelet therapy. Br. J. Haematol. 2016, 175, 602–613. [Google Scholar] [CrossRef] [PubMed]
- Vivas, D.; Roldán, I.; Ferrandis, R.; Marín, F.; Roldán, V.; Tello-Montoliu, A.; Ruiz-Nodar, J.M.; Gómez-Doblas, J.J.; Martín, A.; Llau, J.V.; et al. Perioperative and Periprocedural Management of Antithrombotic Therapy: Consensus Document of SEC, SEDAR, SEACV, SECTCV, AEC, SECPRE, SEPD, SEGO, SEHH, SETH, SEMERGEN, SEMFYC, SEMG, SEMICYUC, SEMI, SEMES, SEPAR, SENEC, SEO, SEPA, SERVEI, SECOT and AEU. Rev. Española Cardiol. 2018, 71, 553–564. [Google Scholar] [CrossRef]
- Godier, A.; Garrigue, D.; Lasne, D.; Fontana, P.; Bonhomme, F.; Collet, J.P.; de Maistre, E.; Ickx, B.; Gruel, Y.; Mazighi, M.; et al. Management of antiplatelet therapy for non elective invasive procedures of bleeding complications: Proposals from the French working group on perioperative haemostasis (GIHP), in collaboration with the French Society of Anaesthesia and Intensive Care Medi. Anaesth. Crit. Care Pain Med. 2019, 38, 289–302. [Google Scholar] [CrossRef]
- Yassa, R.; Khalfaoui, M.Y.; Hujazi, I.; Sevenoaks, H.; Dunkow, P. Management of anticoagulation in hip fractures: A pragmatic approach. EFORT Open Rev. 2017, 2, 394–402. [Google Scholar] [CrossRef] [PubMed]
- Gage, B.F.; Van Walraven, C.; Pearce, L.; Hart, R.G.; Koudstaal, P.J.; Boode, B.S.P.; Petersen, P. Selecting patients with atrial fibrillation for anticoagulation: Stroke risk stratification in patients taking aspirin. Circulation 2004, 110, 2287–2292. [Google Scholar] [CrossRef]
- Lip, G.Y.H.; Nieuwlaat, R.; Pisters, R.; Lane, D.A.; Crijns, H.J.G.M.; Andresen, D.; Camm, A.J.; Davies, W.; Capucci, A.; Olsson, B.; et al. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: The Euro Heart Survey on atrial fibrillation. Chest 2010, 137, 263–272. [Google Scholar] [CrossRef]
- Pisters, R.; Lane, D.A.; Nieuwlaat, R.; De Vos, C.B.; Crijns, H.J.G.M.; Lip, G.Y.H.; Andresen, D.; Camm, A.J.; Davies, W.; Capucci, A.; et al. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: The euro heart survey. Chest 2010, 138, 1093–1100. [Google Scholar] [CrossRef] [PubMed]
- Douketis, J.D.; Spyropoulos, A.C.; Kaatz, S.; Becker, R.C.; Caprini, J.A.; Dunn, A.S.; Garcia, D.A.; Jacobson, A.; Jaffer, A.K.; Kong, D.F.; et al. Perioperative Bridging Anticoagulation in Patients with Atrial Fibrillation. N. Engl. J. Med. 2015, 373, 823–833. [Google Scholar] [CrossRef]
- Barlow, B.T.; Hannon, M.T.; Waldron, J.E. Preoperative Management of Antithrombotics in Arthroplasty. J. Am. Acad. Orthop. Surg. 2019, 27, 878–886. [Google Scholar] [CrossRef]
- Mussa, M.; Chikkalur, P.; Isbister, J.; Deshpande, S.; Isbister, E. Interruption of long-term warfarin is not necessary in patients undergoing total hip arthroplasty. J. Orthop. 2020, 17, 139–143. [Google Scholar] [CrossRef]
- Phillips, A.; Dan, M.; Schaefer, N.; Randle, R. Warfarin cessation is non-essential in patients undergoing total knee arthroplasty-a case-control study. J. Orthop. Surg. Res. 2015, 10, 11. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Leijtens, B.; Kremers Van De Hei, K.; Jansen, J.; Koëter, S. High complication rate after total knee and hip replacement due to perioperative bridging of anticoagulant therapy based on the 2012 ACCP guideline. Arch. Orthop. Trauma Surg. 2014, 134, 1335–1341. [Google Scholar] [CrossRef]
- Jørgensen, C.C.; Kehlet, H.; Søballe, K.; Hansen, T.B.; Husted, H.; Laursen, M.B.; Hansen, L.T.; Kjærsgaard-Andersen, P.; Solgaard, S.; Jorn, L.P. Thromboembolic and major bleeding events in relation to perioperative bridging of vitamin K antagonists in 649 fast-track total hip and knee arthroplasties. Acta Orthop. 2017, 88, 55–61. [Google Scholar] [CrossRef]
- Tsukada, S.; Kurosaka, K.; Nishino, M.; Maeda, T.; Hirasawa, N. A Strategy of Continued Antiplatelet Agents, Vitamin K Antagonists, and Direct Oral Anticoagulants throughout the Perioperative Period of Total Knee Arthroplasty in Patients Receiving Chronic Antithrombotic Therapy. JBJS Open Access 2019, 4, e0057. [Google Scholar] [CrossRef]
- Ashkenazi, I.; Schermann, H.; Gold, A.; Gurel, R.; Chechik, O.; Warschawski, Y.; Schwarzkopf, R.; Snir, N. Is continuation of anti-platelet treatment safe for elective total hip arthroplasty patients? Arch. Orthop. Trauma Surg. 2020, 140, 2101–2107. [Google Scholar] [CrossRef] [PubMed]
- Meier, R.; Marthy, R.; Saely, C.H.; Kuster, M.S.; Giesinger, K.; Rickli, H. Comparison of preoperative continuation and discontinuation of aspirin in patients undergoing total hip or knee arthroplasty. Eur. J. Orthop. Surg. Traumatol. 2016, 26, 921–928. [Google Scholar] [CrossRef] [PubMed]
- Jacob, A.K.; Hurley, S.P.; Loughran, S.M.; Wetsch, T.M.; Trousdale, R.T. Continuing clopidogrel during elective total hip and knee arthroplasty: Assessment of bleeding risk and adverse outcomes. J. Arthroplast. 2014, 29, 325–328. [Google Scholar] [CrossRef]
- Tsukada, S.; Wakui, M. Continuing versus discontinuing antiplatelet drugs, vasodilators, and/or cerebral ameliorators on perioperative total blood loss in total knee arthroplasty without pneumatic tourniquet. Arthroplast. Today 2018, 4, 89–93. [Google Scholar] [CrossRef] [PubMed]
| Thromboembolism Risk | CHADS2 Score *,** | CHA2DS2-VASc Score *** | Mechanical Heart Valve **,**** | VTE History *,** | Medical Risk Factors *,** |
|---|---|---|---|---|---|
| High | 5 or 6 | ≥7 | Any mitral valve | VTE within 3 months | Stroke or transient ischemic attack within 3 months |
| Any caged ball or tilting disc aortic valve | ≥2 idiopathic VTE events | Rheumatic valvular heart disease | |||
| Mechanical valve within 3 months | Severe thrombophilia/hypercoagulable state | ||||
| Active malignancy | |||||
| Intermediate | 3 or 4 | 5 to 6 | Bileaflet aortic valve with atrial fibrillation or stroke risk factors | VTE within 3–12 months | Non-severe thrombophilia |
| Recurrent VTE | |||||
| Low | 1 or 2 | 1 to 4 | Bileaflet aortic valve without atrial fibrillation and no other stroke risk factors | Previous VTE > 12 months | No history of stroke or TIA |
| HAS-BLED Score [44] | Additional Risk Factors * |
|---|---|
| +1 Hypertension (systolic > 160 mmHg) | Prior bleeding event within 3 months |
| +1 Abnormal renal function (chronic dialysis, transplant, or SCr ≥ 200 µmol/L) | Platelet abnormality |
| +1 Abnormal liver function (cirrhosis or significant biochemical derangement) | Supratherapeutic INR |
| +1 Prior stroke | Prior bleeding from bridge therapy |
| +1 History of anemia or predisposition to major bleeding | Prior bleeding from similar procedure |
| +1 Labile INR (<60% of time therapeutic) | |
| +1 >65 years old | |
| +1 On antiplatelet agent or NSAID | |
| +1 Significant alcohol or drug use history (≥8 per week) | |
| HAS-BLED ≥ 3 is predictive of bleeding events |
| DOAC | Half Life-Normal Renal Function *** | TJA Interruption Interval-Therapeutic Dosing **** | Spinal Anesthesia Interruption Interval-Therapeutic Dosing ‡ | |||
|---|---|---|---|---|---|---|
| CrCl (mL/min) | Interval | CrCl (mL/min) | Interval | |||
| Direct Thrombin Inhibitor | Dabigatran (Pradaxa) | 12–17 h | <15 | No data * | <15 | Spinal not recommended |
| 15–29 | ≥5 days | 15–29 | ||||
| 30–49 | ≥4 days | 30–49 | ≥5 days | |||
| 50–79 | ≥3 days | 50–79 | ≥4 days | |||
| ≥80 | ≥2 days | ≥80 | ≥3 days | |||
| Factor Xa Inhibitor | Apixaban (Eliquis) | 12 h | ≥30 ** | ≥2 days | ≥30 | ≥3 days |
| Edoxaban (Savaysa) | 10–14 h | ≥30 ** | ≥2 days | ≥30 | ≥3 days | |
| Rivaroxaban (Xarelto) | 5–13 h | ≥30 ** | ≥2 days | ≥30 | ≥3 days | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santana, D.C.; Hadad, M.J.; Emara, A.; Klika, A.K.; Barsoum, W.; Molloy, R.M.; Krebs, V.E.; Bloomfield, M.R.; Piuzzi, N.S. Perioperative Management of Chronic Antithrombotic Agents in Elective Hip and Knee Arthroplasty. Medicina 2021, 57, 188. https://doi.org/10.3390/medicina57020188
Santana DC, Hadad MJ, Emara A, Klika AK, Barsoum W, Molloy RM, Krebs VE, Bloomfield MR, Piuzzi NS. Perioperative Management of Chronic Antithrombotic Agents in Elective Hip and Knee Arthroplasty. Medicina. 2021; 57(2):188. https://doi.org/10.3390/medicina57020188
Chicago/Turabian StyleSantana, Daniel C., Matthew J. Hadad, Ahmed Emara, Alison K. Klika, Wael Barsoum, Robert M. Molloy, Viktor E. Krebs, Michael R. Bloomfield, and Nicolas S. Piuzzi. 2021. "Perioperative Management of Chronic Antithrombotic Agents in Elective Hip and Knee Arthroplasty" Medicina 57, no. 2: 188. https://doi.org/10.3390/medicina57020188
APA StyleSantana, D. C., Hadad, M. J., Emara, A., Klika, A. K., Barsoum, W., Molloy, R. M., Krebs, V. E., Bloomfield, M. R., & Piuzzi, N. S. (2021). Perioperative Management of Chronic Antithrombotic Agents in Elective Hip and Knee Arthroplasty. Medicina, 57(2), 188. https://doi.org/10.3390/medicina57020188






