Effects of the Proprioceptive Neuromuscular Facilitation Technique on Scapula Function in Office Workers with Scapula Dyskinesis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Approval
2.2. Participants
2.3. Procedures
2.4. Interventions
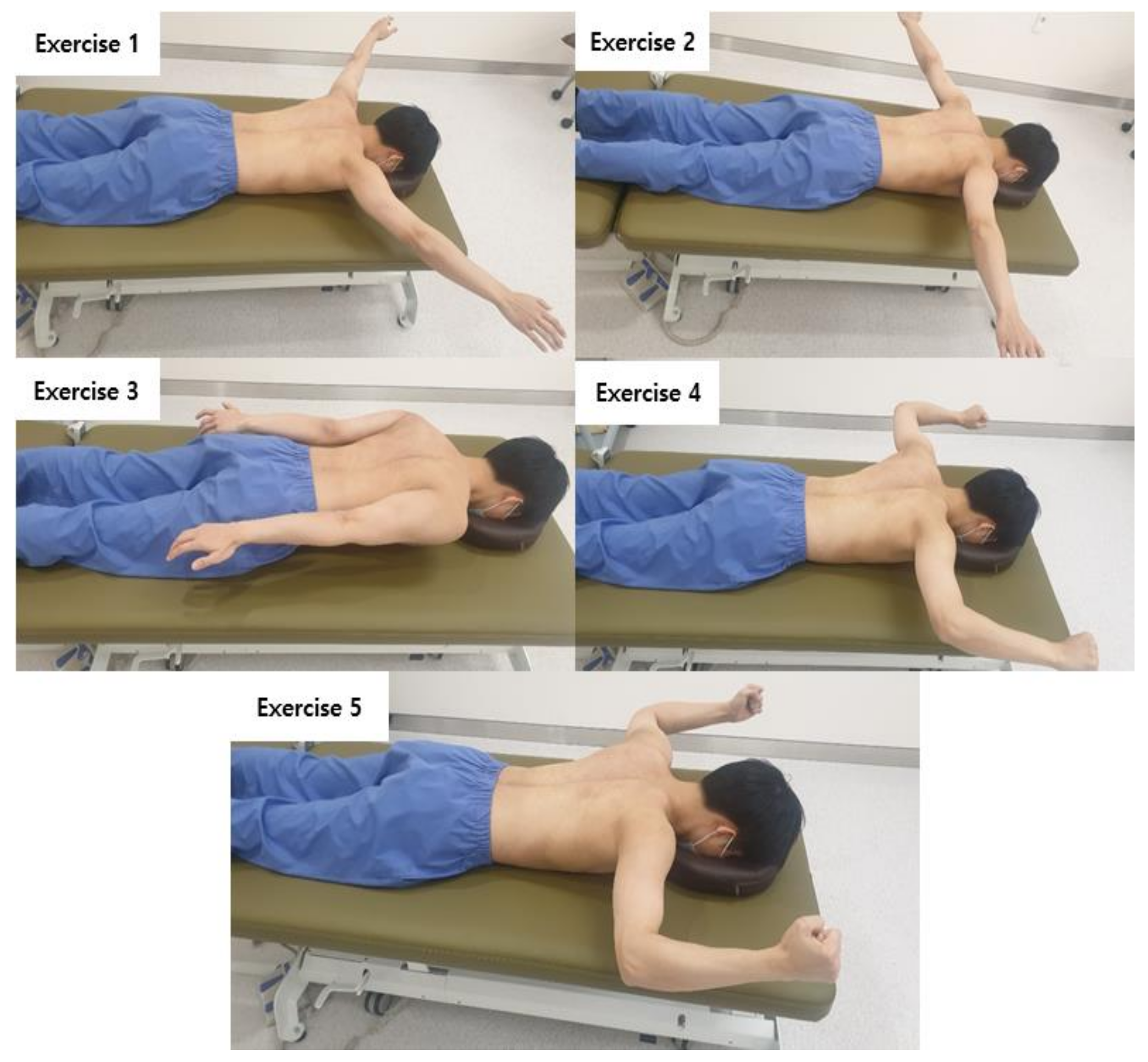
2.4.1. Muscle Strengthening Exercise
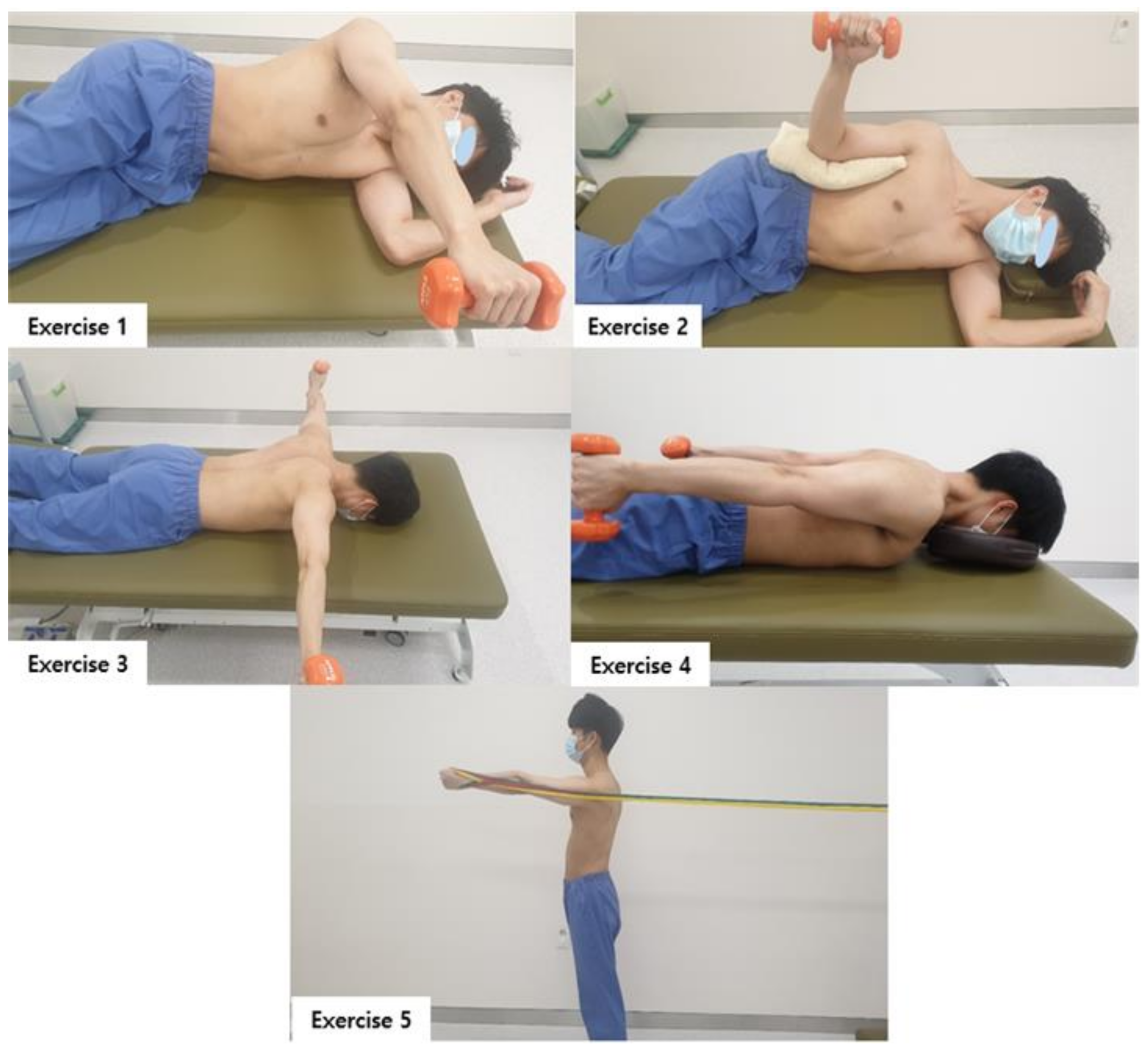
2.4.2. Muscle Balance Exercise
2.4.3. Movement Control Exercise
2.5. Outcome Measurements
2.5.1. Scapula Position
2.5.2. Scapula Movement
2.5.3. Disability of the Arm, Shoulder, and Hand Outcome Questionnaire
where N is the number of questions answered.
2.6. Sample Size Estimation
2.7. Statistical Analysis
3. Results
3.1. Scapula Position
Scapula Index (SI)
3.2. Scapulohumeral Movements (Scapula Upward Rotation at Humeral Abduction)
Scapula Upward Rotation at 0°–180° Humeral Abduction
3.3. DASH Outcome Questionnaire
3.3.1. Pain and Performing Ability
3.3.2. Work Ability
3.3.3. Sports & Art Activity Ability
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Huegel, J.; Williams, A.A.; Soslowsky, L.J. Rotator Cuff Biology and Biomechanics: A Review of Normal and Pathological Conditions. Curr. Rheumatol. Rep. 2015, 17, 476. [Google Scholar] [CrossRef]
- Lippert, L.S.; Minor, M.A.D. Laboratory Manual for Clinical Kinesiology and Anatomy; FA Davis: Duxbury, VT, USA, 2017. [Google Scholar]
- De Oliveira, A.S.; de Morais Carvalho, M.; de Brum, D.P.C. Activation of the shoulder and arm muscles during axial load exercises on a stable base of support and on a medicine ball. J. Electromyogr. Kinesiol. 2008, 18, 472–479. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Gill, S.; Mohammad, F.; Kumar, S.; Kumar, D.; Kumar, S. Prevalence of shoulder disorders in tertiary care centre. Int. J. Res. Med. Sci. 2015, 3, 917–920. [Google Scholar] [CrossRef] [Green Version]
- Laudner, K.G.; Stanek, J.M.; Meister, K. Differences in Scapular Upward Rotation between Baseball Pitchers and Position Players. Am. J. Sports Med. 2007, 35, 2091–2095. [Google Scholar] [CrossRef]
- Mottram, S. Dynamic stability of the scapula. Man. Ther. 1997, 2, 123–131. [Google Scholar] [CrossRef]
- Neumann, D.A.; Camargo, P.R. Kinesiologic considerations for targeting activation of scapulothoracic muscles—Part 1: Serratus anterior. Braz. J. Phys. Ther. 2019, 23, 459–466. [Google Scholar] [CrossRef]
- Camargo, P.R.; Neumann, D.A. Kinesiologic considerations for targeting activation of scapulothoracic muscles—Part 2: Trapezius. Braz. J. Phys. Ther. 2019, 23, 467–475. [Google Scholar] [CrossRef]
- Smith, J.; Dietrich, C.T.; Kotajarvi, B.R.; Kaufman, K.R. The effect of scapular protraction on isometric shoulder rotation strength in normal subjects. J. Shoulder Elb. Surg. 2006, 15, 339–343. [Google Scholar] [CrossRef] [PubMed]
- Voight, M.L.; Thomson, B.C. The role of the scapula in the rehabilitation of shoulder injuries. J. Athl. Train. 2000, 35, 364. [Google Scholar]
- Burkhart, S.S.; Morgan, C.D.; Kibler, W.B. The disabled throwing shoulder: Spectrum of pathology part III: The SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy 2003, 19, 641–661. [Google Scholar] [CrossRef]
- Kibler, W.B.; Ludewig, P.M.; McClure, P.; Uhl, T.L.; Sciascia, A. Scapular Summit 2009: Introduction. July 16, 2009, Lexington, Kentucky. J. Orthop. Sports Phys. Ther. 2009, 39, A1–A13. [Google Scholar] [CrossRef] [PubMed]
- Uhl, T.L.; Kibler, W.B.; Gecewich, B.; Tripp, B.L. Evaluation of Clinical Assessment Methods for Scapular Dyskinesis. Arthrosc. J. Arthrosc. Relat. Surg. 2009, 25, 1240–1248. [Google Scholar] [CrossRef] [PubMed]
- Myers, J.B.; Oyama, S.; Hibberd, E.E. Scapular dysfunction in high school baseball players sustaining throwing-related upper extremity injury: A prospective study. J. Shoulder Elb. Surg. 2013, 22, 1154–1159. [Google Scholar] [CrossRef] [PubMed]
- Jayesh, P.N.; Muragod, A.R.; Motimath, B. Open kinematic chain exercises for SICK scapula in competitive asymptomatic overhead athletes for 3 weeks. Int. J. Physiother. Res. 2014, 2, 608–615. [Google Scholar]
- Ben Kibler, W. The Role of the Scapula in Athletic Shoulder Function. Am. J. Sports Med. 1998, 26, 325–337. [Google Scholar] [CrossRef]
- Geronimo, S.M.; Baracho, W.F.; da Silva Triani, F. Effects of Strength Training on Scapular Dyskinesia: A Systematic Review. J. Health Sci. 2019, 21, 409–413. [Google Scholar] [CrossRef]
- Moghadam, A.N.; Rahnama, L.; Dehkordi, S.N.; Abdollahi, S. Exercise therapy may affect scapular position and motion in individuals with scapular dyskinesis: A systematic review of clinical trials. J. Shoulder Elb. Surg. 2020, 29, e29–e36. [Google Scholar] [CrossRef] [Green Version]
- Warner, J.J.; Micheli, L.J.; Arslanian, L.E.; Kennedy, J.; Kennedy, R. Scapulothoracic motion in normal shoulders and shoulders with glenohumeral instability and impingement syndrome. A study using Moiré topographic analysis. Clin. Orthop. Relat. Res. 1992, 191–199. [Google Scholar]
- Blackburn, T. EMG analysis of posterior rotator cuff exercises. J. Athl. Train. 1990, 25, 40–45. [Google Scholar]
- Johnson, M.P.; McClure, P.W.; Karduna, A.R. New Method to Assess Scapular Upward Rotation in Subjects with Shoulder Pathology. J. Orthop. Sports Phys. Ther. 2001, 31, 81–89. [Google Scholar] [CrossRef]
- Struyf, F.; Nijs, J.; Mottram, S.; Roussel, N.A.; Cools, A.M.; Meeusen, R. Clinical assessment of the scapula: A review of the literature. Br. J. Sports Med. 2014, 48, 883–890. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sree, S.D. To Evaluate Scapulohumeral Rhythm in Scapular Dyskinesia in Software Professionals with Neck Pain. Indian J. Physiother. Occup. Ther. 2020, 13. [Google Scholar] [CrossRef]
- De Mey, K.; Danneels, L.; Cagnie, B.; Cools, A.M. Scapular muscle rehabilitation exercises in overhead athletes with impingement symptoms: Effect of a 6-week training program on muscle recruitment and functional outcome. Am. J. Sports Med. 2012, 40, 1906–1915. [Google Scholar] [CrossRef] [PubMed]
- Peteraitis, T.; Smedes, F. Scapula motor control training with Proprioceptive Neuromuscular Facilitation in chronic subacromial impingement syndrome: A case report. J. Bodyw. Mov. Ther. 2020, 24, 165–171. [Google Scholar] [CrossRef]
- Borstad, J.D. Resting Position Variables at the Shoulder: Evidence to Support a Posture-Impairment Association. Phys. Ther. 2006, 86, 549–557. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, L.A.; Aquino, C.F.; Souza, T.R.; Anjos, M.T.S.; Lima, D.B.; Fonseca, S.T. Clinical Measures Related to Forward Shoulder Posture: A Reliability and Correlational Study. J. Manip. Physiol. Ther. 2019, 42, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Watson, L.; Balster, S.; Finch, C.; Dalziel, R. Measurement of scapula upward rotation: A reliable clinical procedure. Br. J. Sports Med. 2005, 39, 599–603. [Google Scholar] [CrossRef] [Green Version]
- Franchignoni, F.; Vercelli, S.; Giordano, A.; Sartorio, F.; Bravini, E.; Ferriero, G. Minimal Clinically Important Difference of the Disabilities of the Arm, Shoulder and Hand Outcome Measure (DASH) and Its Shortened Version (QuickDASH). J. Orthop. Sports Phys. Ther. 2014, 44, 30–39. [Google Scholar] [CrossRef] [Green Version]
- Ludewig, P.M.; Cook, T.M. Alterations in Shoulder Kinematics and Associated Muscle Activity in People with Symptoms of Shoulder Impingement. Phys. Ther. 2000, 80, 276–291. [Google Scholar] [CrossRef]
- Townsend, H.; Jobe, F.W.; Pink, M.; Perry, J. Electromyographic analysis of the glenohumeral muscles during a baseball rehabilitation program. Am. J. Sports Med. 1991, 19, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Maenhout, A.; Van Praet, K.; Pizzi, L.; Van Herzeele, M.; Cools, A. Electromyographic analysis of knee push up plus variations: What is the influence of the kinetic chain on scapular muscle activity? Br. J. Sports Med. 2010, 44, 1010–1015. [Google Scholar] [CrossRef] [PubMed]
- Holtermann, A.; Mork, P.; Andersen, L.; Olsen, H.B.; Søgaard, K. The use of EMG biofeedback for learning of selective activation of intra-muscular parts within the serratus anterior muscle: A novel approach for rehabilitation of scapular muscle imbalance. J. Electromyogr. Kinesiol. 2010, 20, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, A.B.; Jørgensen, U. Secondary impingement in the shoulder: An improved terminology in impingement. Scand. J. Med. Sci. Sports Rev. Artic. 2000, 10, 266–278. [Google Scholar] [CrossRef] [PubMed]
- Roy, J.-S.; Moffet, H.; McFadyen, B.J.; Lirette, R. Impact of movement training on upper limb motor strategies in persons with shoulder impingement syndrome. BMC Sports Sci. Med. Rehabil. 2009, 1, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Day, J.M.; Bush, H.; Nitz, A.J.; Uhl, T.L. Scapular Muscle Performance in Individuals with Lateral Epicondylalgia. J. Orthop. Sports Phys. Ther. 2015, 45, 414–424. [Google Scholar] [CrossRef] [PubMed]
| MSG (n = 14) | MBG (n = 14) | MCG (n = 14) | p | |
|---|---|---|---|---|
| Sex (male/female), n (%) | 4/9 (35.7%/64.3%) | 4/10 (40.0%/60.0%) | 8/6 (57.1%/42.9%) | 0.292 |
| Affected side (left/right), n | 7/7 | 9/5 | 7/7 | 0.697 |
| Age (years) | 32.86 ± 6.49 | 32.01 ± 5.87 | 32.14 ± 6.66 | 0.930 |
| Height (cm) | 166.05 ± 9.46 | 165.42 ± 8.92 | 168.29 ± 9.02 | 0.685 |
| Weight (kg) | 61.83 ± 12.74 | 62.67 ± 13.97 | 67.28 ± 13.26 | 0.514 |
| BMI (kg/m2) | 22.17 ± 2.45 | 22.65 ± 3.03 | 23.61 ± 3.43 | 0.443 |
| Scapula Position | MSG (n = 14) | MBG (n = 14) | MCG (n = 14) | p | E(η2) | |
|---|---|---|---|---|---|---|
| Scapula index (score) | Pre | 68.84 ± 7.66 | 63.89 ± 5.99 | 63.86 ± 6.91 | ||
| Post | 68.72 ± 7.45 | 67.40 ± 5.43 | 72.58 ± 4.83 | |||
| DIFF | 0.11 ± 7.79 †† | 3.50 ± 5.12 | 8.71 ± 4.79 | 0.002 | 0.279 | |
| p | 0.956 | 0.024 * | 0.000 *** |
| Humeral Abduction | MSG (n = 14) | MBG (n = 14) | MCG (n = 14) | p | E(η2) | |
|---|---|---|---|---|---|---|
| 0° | Pre | −6.29 ± 3.66 | −3.43 ± 5.34 | −2.57 ± 3.56 | ||
| Post | −5.64 ± 3.47 | −0.14 ± 4.72 | 1.43 ± 3.79 | |||
| DIFF | −0.64 ± 1.15 † | 3.28 ± 4.53 ††† | 4.00 ± 1.30 | 0.013 | 0.201 | |
| p | 0.057 | 0.018 * | 0.000 *** | |||
| 45° | Pre | 5.87 ± 3.37 | 5.21 ± 6.78 | 4.93 ± 3.14 | ||
| Post | 6.50 ± 2.87 | 5.14 ± 5.48 | 6.75 ± 3.77 | |||
| DIFF | 0.63 ± 1.72 | 0.07 ± 6.15 † | 3.42 ± 1.01 | 0.043 | 0.149 | |
| p | 0.196 | 0.966 | 0.000 *** | |||
| 90° | Pre | 14.57 ± 3.75 | 17.29 ± 8.10 | 18.09 ± 5.11 | ||
| Post | 15.21 ± 3.64 | 19.07 ± 6.83 | 19.07 ± 5.63 | |||
| DIFF | −0.64 ± 2.46 | −1.78 ± 9.79 | 0.97 ± 4.54 | 0.718 | 0.017 | |
| p | 0.370 | 0.199 | 0.435 | |||
| 135° | Pre | 34.89 ± 7.82 | 33.35 ± 13.58 | 32.70 ± 8.99 | ||
| Post | 31.74 ± 9.24 | 34.78 ± 11.76 | 34.57 ± 6.61 | |||
| DIFF | 3.17 ± 13.58 | 1.42 ± 12.58 | 1.87 ± 8.14 | 0.473 | 0.038 | |
| p | 0.397 | 0.678 | 0.405 | |||
| 180° | Pre | 43.63 ± 8.38 | 43.28 ± 15.77 | 43.40 ± 7.60 | ||
| Post | 41.64 ± 11.38 | 46.57 ± 12.85 | 44.93 ± 5.58 | |||
| DIFF | 1.99 ± 14.56 | 3.28 ± 15.51 | 1.52 ± 7.16 | 0.553 | 0.030 | |
| p | 0.617 | 0.442 | 0.441 |
| DASH | MSG (n = 14) | MBG (n = 14) | MCG (n = 14) | p | E(η2) | |
|---|---|---|---|---|---|---|
| Pain & performing ability (score) | Pre | 25.94 ± 16.57 | 21.08 ± 9.90 | 27.25 ± 14.40 | ||
| Post | 21.73 ± 14.88 | 20.00 ± 9.95 | 9.92 ± 8.11 | |||
| DIFF | −4.21 ± 7.80 †† | −1.08 ± 1.90 ††† | −17.32 ± 12.28 | 0.000 | 0.452 | |
| p | 0.65 | 0.55 | 0.000 *** | |||
| Work ability (score) | Pre | 22.76 ± 16.73 | 15.62 ± 9.09 | 21.42 ± 21.31 | ||
| Post | 21.42 ± 15.25 | 14.28 ± 9.31 | 10.71 ± 11.15 | |||
| DIFF | −1.34 ± 2.66 ††† | −1.33 ± 3.61 ††† | −10.71 ± 8.98 | 0.000 | 0.388 | |
| p | 0.082 | 0.189 | 0.001 *** | |||
| Sports & art activities (score) | Pre | 29.01 ± 18.44 | 27.23 ± 7.19 | 24.10 ± 16.04 | ||
| Post | 27.67 ± 16.57 | 24.55 ± 7.13 | 15.16 ± 14.23 | |||
| DIFF | −1.33 ± 2.66 † | −2.67 ± 6.35 | −8.94 ± 10.61 | 0.027 | 0.168 | |
| p | 0.082 | 0.139 | 0.008 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hwang, M.; Lee, S.; Lim, C. Effects of the Proprioceptive Neuromuscular Facilitation Technique on Scapula Function in Office Workers with Scapula Dyskinesis. Medicina 2021, 57, 332. https://doi.org/10.3390/medicina57040332
Hwang M, Lee S, Lim C. Effects of the Proprioceptive Neuromuscular Facilitation Technique on Scapula Function in Office Workers with Scapula Dyskinesis. Medicina. 2021; 57(4):332. https://doi.org/10.3390/medicina57040332
Chicago/Turabian StyleHwang, Myeungsik, Sangbin Lee, and Chaegil Lim. 2021. "Effects of the Proprioceptive Neuromuscular Facilitation Technique on Scapula Function in Office Workers with Scapula Dyskinesis" Medicina 57, no. 4: 332. https://doi.org/10.3390/medicina57040332
APA StyleHwang, M., Lee, S., & Lim, C. (2021). Effects of the Proprioceptive Neuromuscular Facilitation Technique on Scapula Function in Office Workers with Scapula Dyskinesis. Medicina, 57(4), 332. https://doi.org/10.3390/medicina57040332






