Ergonomics in Interventional Radiology: Awareness Is Mandatory
Abstract
:1. Introduction
2. Materials and Methods
3. Work-Related Musculoskeletal Disorders
3.1. Definition
3.2. Risk Factors
3.3. Consequences
4. Situations Encountered in Interventional Radiology and Existing Solutions
4.1. Ultrasound-Guided Procedures
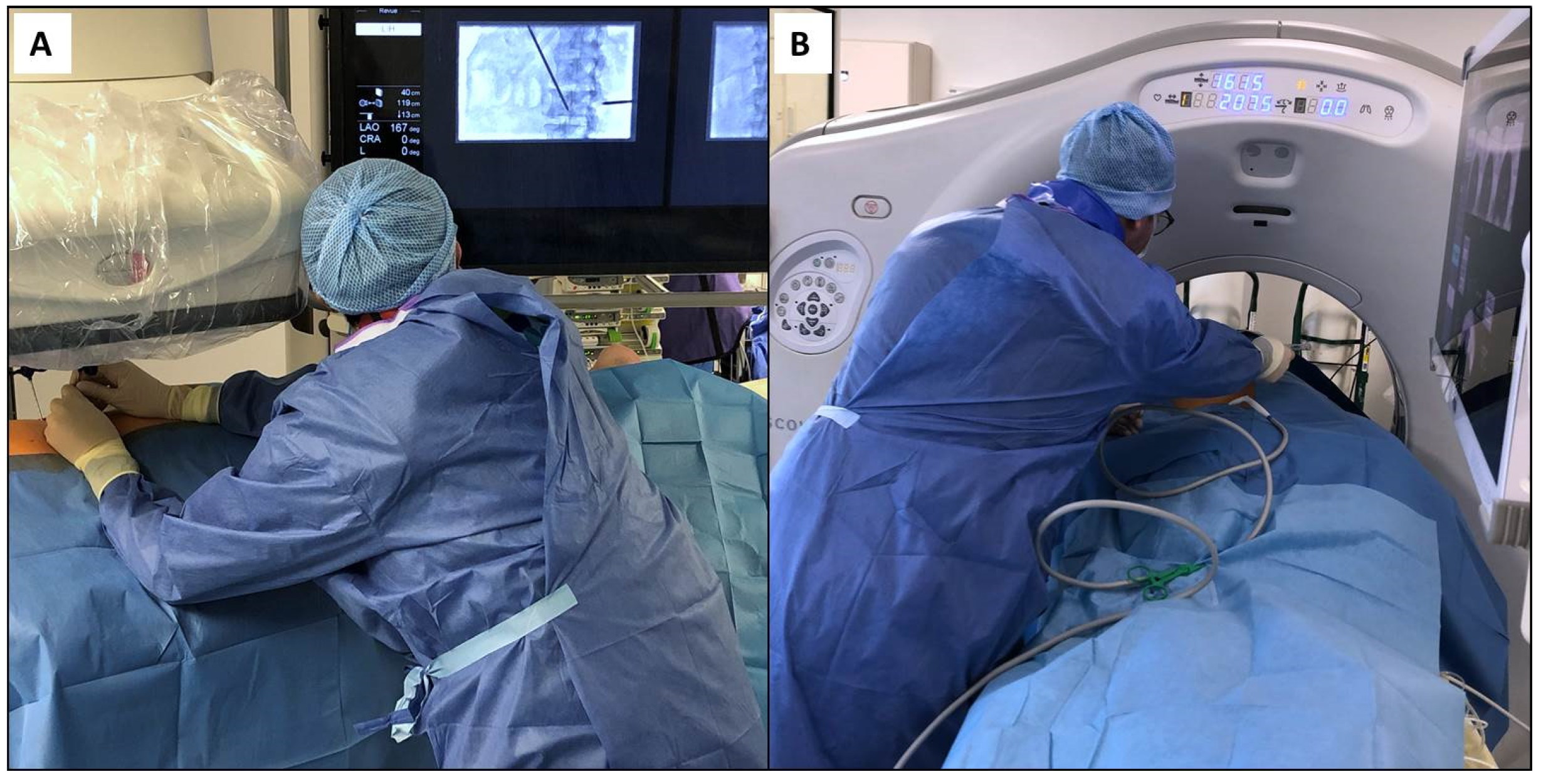
4.2. Procedures Performed under Angiography and Cone-Beam Computed Tomography
4.3. Procedures Performed under Computed Tomography and Positron Emission Tomography Scan
4.4. Magnetic Resonance Imaging Guided Interventions
5. Future Developments
5.1. Prevention and Physical Exercise
5.2. Training
5.3. Specialization and Design of Interventional Equipments
5.4. Robotics and New Technologies
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Filippiadis, D.; Tutton, S.; Kelekis, A. Pain management: The rising role of interventional oncology. Diagn. Interv. Imaging 2017, 98, 627–634. [Google Scholar] [CrossRef]
- Cornelis, F. The interventional oncologist: The fourth musketeer of cancer care. Diagn. Interv. Imaging 2017, 98, 579–581. [Google Scholar] [CrossRef] [PubMed]
- Vroomen, L.; Petre, E.; Cornelis, F.; Solomon, S.; Srimathveeravalli, G. Irreversible electroporation and thermal ablation of tumors in the liver, lung, kidney and bone: What are the differences? Diagn. Interv. Imaging 2017, 98, 609–617. [Google Scholar] [CrossRef]
- Cornelis, F.H.; Joly, Q.; Nouri-Neuville, M.; Ben-Ammar, M.; Kastler, B.; Kastler, A.; Amoretti, N.; Hauger, O. Innovative Spine Implants for Improved Augmentation and Stability in Neoplastic Vertebral Compression Fracture. Medicina 2019, 55, 426. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cornelis, F.H.; Tutton, S.; Filippiadis, D.; Kelekis, A. Metastatic Osseous Pain Control: Bone Ablation and Cementoplasty. Semin. Interv. Radiol. 2017, 34, 328–336. [Google Scholar] [CrossRef]
- Klein, L.W.; Miller, D.L.; Balter, S.; Laskey, W.; Haines, D.; Norbash, A.; Mauro, M.A.; Goldstein, J.A. Joint Inter-Society Task Force on Occupational Hazards in the Interventional Laboratory. Occupational Health Hazards in the Interventional Laboratory: Time for a Safer Environment. J. Vasc. Interv. Radiol. 2009, 20, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Dalager, T.; Søgaard, K.; Boyle, E.; Jensen, P.T.; Mogensen, O. Surgery Is Physically Demanding and Associated with Multisite Musculoskeletal Pain: A Cross-Sectional Study. J. Surg. Res. 2019, 240, 30–39. [Google Scholar] [CrossRef] [Green Version]
- Dixon, R.G.; Khiatani, V.; Statler, J.D.; Walser, E.M.; Midia, M.; Miller, D.L.; Bartal, G.; Collins, J.D.; Gross, K.A.; Stecker, M.S.; et al. Society of Interventional Radiology: Occupational Back and Neck Pain and the Interventional Radiologist. J. Vasc. Interv. Radiol. 2017, 28, 195–199. [Google Scholar] [CrossRef] [Green Version]
- Aaron, K.A.; Vaughan, J.; Gupta, R.; Ali, N.-E.-S.; Beth, A.H.; Moore, J.M.; Ma, Y.; Ahmad, I.; Jackler, R.K.; Vaisbuch, Y. The risk of ergonomic injury across surgical specialties. PLoS ONE 2021, 16, e0244868. [Google Scholar] [CrossRef]
- Benjamin, J.L.; Meisinger, Q.C. Ergonomics in the Development and Prevention of Musculoskeletal Injury in Interventional Radiologists. Tech. Vasc. Interv. Radiol. 2018, 21, 16–20. [Google Scholar] [CrossRef]
- Knuttinen, M.-G.; Zurcher, K.S.; Wallace, A.; Doe, C.; Naidu, S.G.; Money, S.R.; Rochon, P.J. Ergonomics in IR. J. Vasc. Interv. Radiol. 2021, 32, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Baethge, C.; Goldbeck-Wood, S.; Mertens, S. SANRA—a scale for the quality assessment of narrative review articles. Res. Integr. Peer Rev. 2019, 4, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Machan, L. Risks of Back Injury. J. Vasc. Interv. Radiol. 2002, 13, P130–P131. [Google Scholar] [CrossRef]
- Epstein, S.; Sparer, E.H.; Tran, B.N.; Ruan, Q.Z.; Dennerlein, J.T.; Singhal, D.; Lee, B.T. Prevalence of Work-Related Musculoskeletal Disorders Among Surgeons and Interventionalists: A Systematic Review and Meta-analysis. JAMA Surg. 2018, 153, e174947. [Google Scholar] [CrossRef]
- Wells, A.C.; Kjellman, M.; Harper, S.J.F.; Forsman, M.; Hallbeck, M.S. Operating hurts: A study of EAES surgeons. Surg. Endosc. 2019, 33, 933–940. [Google Scholar] [CrossRef] [Green Version]
- McDonald, M.E.; Ramirez, P.T.; Munsell, M.F.; Greer, M.; Burke, W.M.; Naumann, W.T.; Frumovitz, M. Physician pain and discomfort during minimally invasive gynecologic cancer surgery. Gynecol. Oncol. 2014, 134, 243–247. [Google Scholar] [CrossRef] [Green Version]
- Adams, S.R.; Hacker, M.R.; McKinney, J.L.; Elkadry, E.A.; Rosenblatt, P.L. Musculoskeletal Pain in Gynecologic Surgeons. J. Minim. Invasive Gynecol. 2013, 20, 656–660. [Google Scholar] [CrossRef] [Green Version]
- Alleblas, C.C.J.; de Man, A.M.; Haak, L.V.D.; Vierhout, M.E.; Jansen, F.W.; Nieboer, T.E. Prevalence of Musculoskeletal Disorders Among Surgeons Performing Minimally Invasive Surgery. Ann. Surg. 2017, 266, 905–920. [Google Scholar] [CrossRef]
- Monaco, M.G.L.; Carta, A.; Tamhid, T.; Porru, S. Anti-X Apron Wearing and Musculoskeletal Problems Among Healthcare Workers: A Systematic Scoping Review. Int. J. Environ. Res. Public Health 2020, 17, 5877. [Google Scholar] [CrossRef]
- Moore, B.; Vansonnenberg, E.; Casola, G.; Novelline, R.A. The relationship between back pain and lead apron use in radiologists. Am. J. Roentgenol. 1992, 158, 191–193. [Google Scholar] [CrossRef]
- Goldstein, J.A.; Balter, S.; Cowley, M.; Hodgson, J.; Klein, L.W. Occupational hazards of interventional cardiologists: Prevalence of orthopedic health problems in contemporary practice. Catheter. Cardiovasc. Interv. 2004, 63, 407–411. [Google Scholar] [CrossRef] [PubMed]
- Orme, N.M.; Rihal, C.S.; Gulati, R.; Holmes, D.R.; Lennon, R.J.; Lewis, B.R.; McPhail, I.R.; Thielen, K.R.; Pislaru, S.V.; Sandhu, G.S.; et al. Occupational Health Hazards of Working in the Interventional Laboratory. J. Am. Coll. Cardiol. 2015, 65, 820–826. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sutton, E.; Irvin, M.; Zeigler, C.; Lee, G.; Park, A. The ergonomics of women in surgery. Surg. Endosc. 2014, 28, 1051–1055. [Google Scholar] [CrossRef] [PubMed]
- Hemal, A.; Srinivas, M.; Charles, A. Ergonomic Problems Associated with Laparoscopy. J. Endourol. 2001, 15, 499–503. [Google Scholar] [CrossRef] [PubMed]
- Wong, K.; Grundfast, K.M.; Levi, J.R. Assessing work-related musculoskeletal symptoms among otolaryngology residents. Am. J. Otolaryngol. 2017, 38, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Davis, W.T.; Fletcher, S.A.; Guillamondegui, O.D. Musculoskeletal occupational injury among surgeons: Effects for patients, providers, and institutions. J. Surg. Res. 2014, 189, 207–212.e6. [Google Scholar] [CrossRef]
- Sergesketter, A.R.; Lubkin, D.T.; Shammas, R.L.; Krucoff, K.B.; Peskoe, S.B.; Risoli, T.; Endres, K.; Hollenbeck, S.T. The Impact of Ergonomics on Recruitment to Surgical Fields: A Multi-Institutional Survey Study. J. Surg. Res. 2019, 236, 238–246. [Google Scholar] [CrossRef]
- Rotenstein, L.S.; Torre, M.; Ramos, M.A.; Rosales, R.C.; Guille, C.; Sen, S.; Mata, D.A. Prevalence of Burnout Among Physicians: A Systematic Review. JAMA 2018, 320, 1131–1150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Hert, S. Burnout in Healthcare Workers: Prevalence, Impact and Preventative Strategies. Local Reg. Anesth. 2020, 13, 171–183. [Google Scholar] [CrossRef]
- Davila, V.J.; Meltzer, A.J.; Hallbeck, M.S.; Stone, W.M.; Money, S.R. Physical discomfort, professional satisfaction, and burnout in vascular surgeons. J. Vasc. Surg. 2019, 70, 913–920.e2. [Google Scholar] [CrossRef]
- Stucky, C.-C.H.; Cromwell, K.D.; Voss, R.K.; Chiang, Y.-J.; Woodman, K.; Lee, J.E.; Cormier, J.N. Surgeon symptoms, strain, and selections: Systematic review and meta-analysis of surgical ergonomics. Ann. Med. Surg. 2018, 27, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Goyal, N.; Jain, N.; Rachapalli, V. Ergonomics in radiology. Clin. Radiol. 2009, 64, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.C.; Wolf, J.G.; Xie, G.-Y.; Smith, M.D. Musculoskeletal pain in cardiac ultrasonographers: Results of a random survey. J. Am. Soc. Echocardiogr. 1997, 10, 357–362. [Google Scholar] [CrossRef]
- Barros-Gomes, S.; Orme, N.; Nhola, L.F.; Scott, C.; Helfinstine, K.; Pislaru, S.V.; Kane, G.C.; Singh, M.; Pellikka, P.A. Characteristics and Consequences of Work-Related Musculoskeletal Pain among Cardiac Sonographers Compared with Peer Employees: A Multisite Cross-Sectional Study. J. Am. Soc. Echocardiogr. 2019, 32, 1138–1146. [Google Scholar] [CrossRef]
- Magnavita, N.; Bevilacqua, L.; Mirk, P.; Fileni, A.; Castellino, N. Work-Related Musculoskeletal Complaints in Sonologists. J. Occup. Environ. Med. 1999, 41, 981–988. [Google Scholar] [CrossRef] [PubMed]
- Christenssen, W.D. Stretch Exercises. J. Diagn. Med. Sonogr. 2001, 17, 123–140. [Google Scholar] [CrossRef]
- Mirowski, M.M. New-old methods of reducing and monitoring X-ray exposure in the interventional radiology environment. Med. Pract. 2020, 72, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Tetteh, E.; Sarker, P.; Radley, C.; Hallbeck, M.S.; Mirka, G.A. Effect of surgical radiation personal protective equipment on EMG-based measures of back and shoulder muscle fatigue: A laboratory study of novices. Appl. Ergon. 2020, 84, 103029. [Google Scholar] [CrossRef]
- Ross, A.M.; Segal, J.; Borenstein, D.; Jenkins, E.; Cho, S. Prevalence of Spinal Disc Disease Among Interventional Cardiologists. Am. J. Cardiol. 1997, 79, 68–70. [Google Scholar] [CrossRef]
- Miller, D.L.; Vañó, E.; Bartal, G.; Balter, S.; Dixon, R.; Padovani, R.; Schueler, B.; Cardella, J.F.; De Baère, T. Occupational Radiation Protection in Interventional Radiology: A Joint Guideline of the Cardiovascular and Interventional Radiology Society of Europe and the Society of Interventional Radiology. Cardiovasc. Interv. Radiol. 2009, 33, 230–239. [Google Scholar] [CrossRef] [Green Version]
- Marichal, D.A.; Anwar, T.; Kirsch, D.; Clements, J.; Carlson, L.; Savage, C.; Rees, C.R. Comparison of a Suspended Radiation Protection System versus Standard Lead Apron for Radiation Exposure of a Simulated Interventionalist. J. Vasc. Interv. Radiol. 2011, 22, 437–442. [Google Scholar] [CrossRef]
- Sikkink, C.; Reijnen, M.; Zeebregts, C. The Creation of the Optimal Dedicated Endovascular Suite. Eur. J. Vasc. Endovasc. Surg. 2008, 35, 198–204. [Google Scholar] [CrossRef] [Green Version]
- Harisinghani, M.G.; Blake, M.A.; Saksena, M.; Hahn, P.F.; Gervais, D.; Zalis, M.; Fernandes, L.D.S.D.; Mueller, P.R. Importance and Effects of Altered Workplace Ergonomics in Modern Radiology Suites1. Radiography 2004, 24, 615–627. [Google Scholar] [CrossRef] [PubMed]
- Barral, M.; Gardavaud, F.; Lassalle, L.; Ben Ammar, M.; Najdawi, M.; Razakamanantsoa, L.; Renard-Penna, R.; Cussenot, O.; Cornelis, F.H. Limiting radiation exposure during prostatic arteries embolization: Influence of patient characteristics, anatomical conditions, and technical factors. Eur. Radiol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Van Veelen, M.; Kazemier, G.; Koopman, J.; Goossens, R.; Meijer, D. Assessment of the Ergonomically Optimal Operating Surface Height for Laparoscopic Surgery. J. Laparoendosc. Adv. Surg. Tech. 2002, 12, 47–52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- King, P.M. A comparison of the effects of floor mats and shoe in-soles on standing fatigue. Appl. Ergon. 2002, 33, 477–484. [Google Scholar] [CrossRef]
- Leng, S.; Christner, J.A.; Carlson, S.K.; Jacobsen, M.; Vrieze, T.J.; Atwell, T.D.; McCollough, C.H. Radiation Dose Levels for Interventional CT Procedures. Am. J. Roentgenol. 2011, 197, W97–W103. [Google Scholar] [CrossRef] [PubMed]
- Solomon, S.B.; Cornelis, F.H. Interventional Molecular Imaging. J. Nucl. Med. 2016, 57, 493–496. [Google Scholar] [CrossRef] [Green Version]
- Bogoni, M.; Cerci, J.J.; Cornelis, F.H.; Nanni, C.; Tabacchi, E.; Schöder, H.; Shyn, P.B.; Sofocleous, C.T.; Solomon, S.B.; Kirov, A.S. Practice and prospects for PET/CT guided interventions. Q. J. Nucl. Med. Mol. Imaging 2021, 65, 20–31. [Google Scholar] [CrossRef] [PubMed]
- Meyer, B.C.; Peter, O.; Nagel, M.; Hoheisel, M.; Frericks, B.B.; Wolf, K.-J.; Wacker, F.K. Electromagnetic field-based navigation for percutaneous punctures on C-arm CT: Experimental evaluation and clinical application. Eur. Radiol. 2008, 18, 2855–2864. [Google Scholar] [CrossRef] [PubMed]
- Abi-Jaoudeh, N.; Kruecker, J.; Kadoury, S.; Kobeiter, H.; Venkatesan, A.M.; Levy, E.; Wood, B.J. Multimodality Image Fusion–Guided Procedures: Technique, Accuracy, and Applications. Cardiovasc. Interv. Radiol. 2012, 35, 986–998. [Google Scholar] [CrossRef] [Green Version]
- Ahrar, K.; Ahrar, J.U.; Javadi, S.; Pan, L.; Milton, D.R.; Wood, C.G.; Matin, S.F.; Stafford, R.J. Real-Time Magnetic Resonance Imaging–Guided Cryoablation of Small Renal Tumors at 1.5 T. Investig. Radiol. 2013, 48, 437–444. [Google Scholar] [CrossRef] [Green Version]
- Pickup, L.; Nugent, B.; Bowie, P. A preliminary ergonomic analysis of the MRI work system environment: Implications and recommendations for safety and design. Radiography 2019, 25, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Bock, M.; Wacker, F.K. MR-guided intravascular interventions: Techniques and applications. J. Magn. Reson. Imaging 2008, 27, 326–338. [Google Scholar] [CrossRef] [PubMed]
- Sjøgaard, G.; Christensen, J.R.; Justesen, J.B.; Murray, M.; Dalager, T.; Fredslund, G.H.; Søgaard, K. Exercise is more than medicine: The working age population’s well-being and productivity. J. Sport Health Sci. 2016, 5, 159–165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robertson, M.M.; O’Neill, M.J. Reducing Musculoskeletal Discomfort: Effects of an Office Ergonomics Workplace and Training Intervention. Int. J. Occup. Saf. Ergon. 2003, 9, 491–502. [Google Scholar] [CrossRef]
- Hallbeck, M.; Lowndes, B.; Bingener, J.; Abdelrahman, A.; Yu, D.; Bartley, A.; Park, A. The impact of intraoperative microbreaks with exercises on surgeons: A multi-center cohort study. Appl. Ergon. 2017, 60, 334–341. [Google Scholar] [CrossRef]
- Cornelis, F.H.; Najdawi, M.; Ben Ammar, M.; Nouri-Neuville, M.; Lombart, B.; Lotz, J.-P.; Cadranel, J.; Barral, M. Integrative Medicine in Interventional Oncology: A Virtuous Alliance. Medicina 2020, 56, 35. [Google Scholar] [CrossRef] [Green Version]
- Cornelis, F.-H.; Solomon, S.-B. Image guidance in interventional radiology: Back to the future? Diagn. Interv. Imaging 2020, 101, 429–430. [Google Scholar] [CrossRef]
- Feinberg, N.; Funaki, B.; Hieromnimon, M.; Guajardo, S.; Navuluri, R.; Zangan, S.; Lorenz, J.; Ahmed, O. Improved Utilization Following Conversion of a Fluoroscopy Suite to Hybrid CT/Angiography System. J. Vasc. Interv. Radiol. 2020, 31, 1857–1863. [Google Scholar] [CrossRef]
- Cornelis, F.H.; Takaki, H.; Laskhmanan, M.; Durack, J.C.; Erinjeri, J.P.; Getrajdman, G.I.; Maybody, M.; Sofocleous, C.T.; Solomon, S.B.; Srimathveeravalli, G. Comparison of CT Fluoroscopy-Guided Manual and CT-Guided Robotic Positioning System for In Vivo Needle Placements in Swine Liver. Cardiovasc. Interv. Radiol. 2014, 38, 1252–1260. [Google Scholar] [CrossRef] [Green Version]
- Franasiak, J.; Craven, R.; Mosaly, P.; Gehrig, P.A. Feasibility and Acceptance of a Robotic Surgery Ergonomic Training Program. JSLS J. Soc. Laparoendosc. Surg. 2014, 18, 00166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santos, J.S.; Uusi-Simola, J.; Kaasalainen, T.; Aho, P.; Venermo, M. Radiation Doses to Staff in a Hybrid Operating Room: An Anthropomorphic Phantom Study with Active Electronic Dosimeters. Eur. J. Vasc. Endovasc. Surg. 2020, 59, 654–660. [Google Scholar] [CrossRef] [PubMed]
- De Vries, A.W.; Krause, F.; De Looze, M.P. The effectivity of a passive arm support exoskeleton in reducing muscle activation and perceived exertion during plastering activities. Ergonomics 2021, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Park, B.J.; Hunt, S.J.; Martin, C.; Nadolski, G.J.; Wood, B.J.; Gade, T.P. Augmented and Mixed Reality: Technologies for Enhancing the Future of IR. J. Vasc. Interv. Radiol. 2020, 31, 1074–1082. [Google Scholar] [CrossRef] [PubMed]
- Bin Helayel, H.; Al-Mazidi, S.; Al Akeely, A. Can the Three-Dimensional Heads-Up Display Improve Ergonomics, Surgical Performance, and Ophthalmology Training Compared to Conventional Microscopy? Clin. Ophthalmol. 2021, 15, 679–686. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cornelis, F.H.; Razakamanantsoa, L.; Ben Ammar, M.; Lehrer, R.; Haffaf, I.; El-Mouhadi, S.; Gardavaud, F.; Najdawi, M.; Barral, M. Ergonomics in Interventional Radiology: Awareness Is Mandatory. Medicina 2021, 57, 500. https://doi.org/10.3390/medicina57050500
Cornelis FH, Razakamanantsoa L, Ben Ammar M, Lehrer R, Haffaf I, El-Mouhadi S, Gardavaud F, Najdawi M, Barral M. Ergonomics in Interventional Radiology: Awareness Is Mandatory. Medicina. 2021; 57(5):500. https://doi.org/10.3390/medicina57050500
Chicago/Turabian StyleCornelis, Francois H., Leo Razakamanantsoa, Mohamed Ben Ammar, Raphael Lehrer, Idriss Haffaf, Sanaa El-Mouhadi, Francois Gardavaud, Milan Najdawi, and Matthias Barral. 2021. "Ergonomics in Interventional Radiology: Awareness Is Mandatory" Medicina 57, no. 5: 500. https://doi.org/10.3390/medicina57050500
APA StyleCornelis, F. H., Razakamanantsoa, L., Ben Ammar, M., Lehrer, R., Haffaf, I., El-Mouhadi, S., Gardavaud, F., Najdawi, M., & Barral, M. (2021). Ergonomics in Interventional Radiology: Awareness Is Mandatory. Medicina, 57(5), 500. https://doi.org/10.3390/medicina57050500






