Trochanteric Femur Fractures: Application of Skeletal Traction during Surgery Does Not Alter Soft-Tissue Microcirculation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
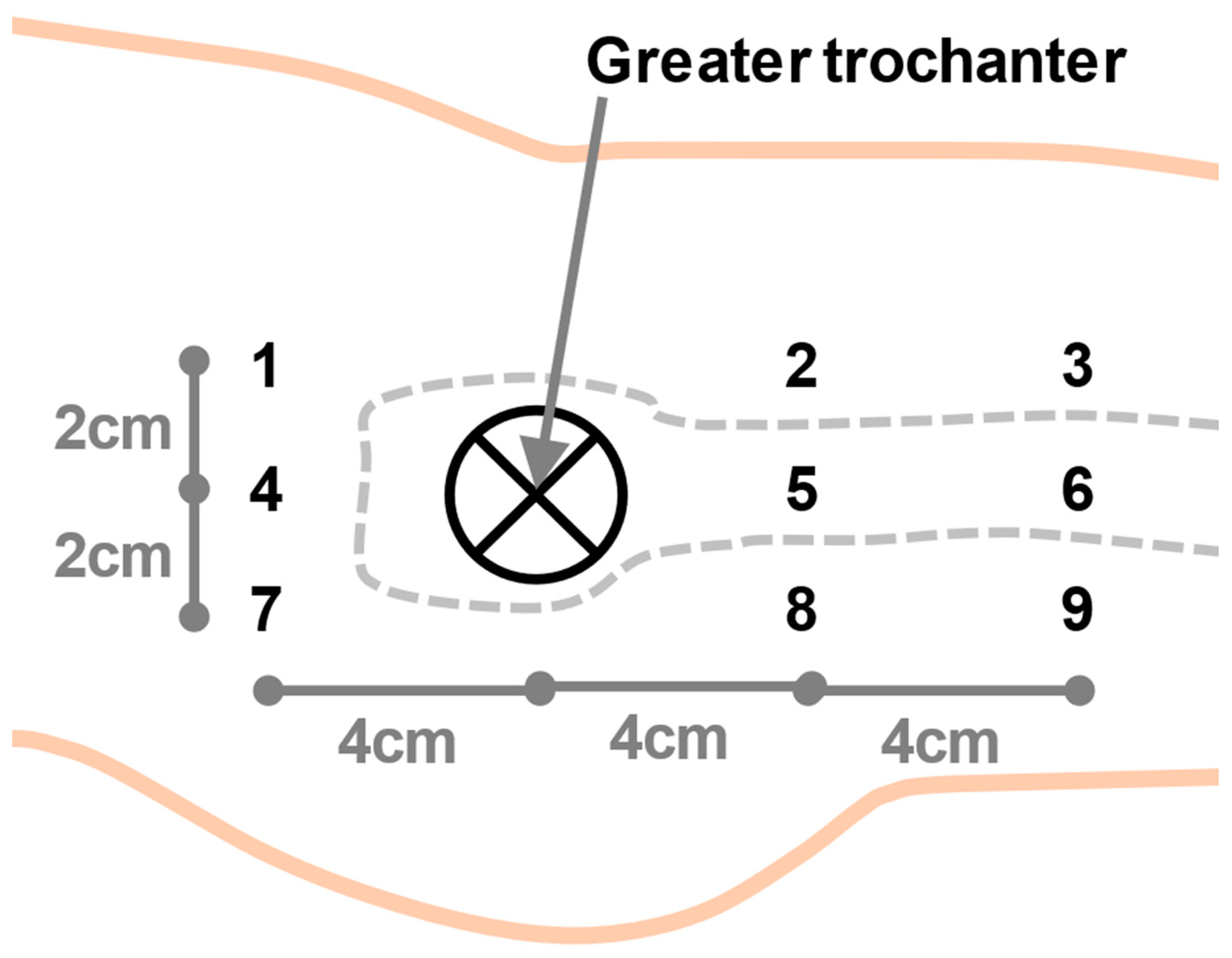
2.2. Measurements
2.3. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Knobe, M.; Siebert, C.H. Hip fractures in the elderly: Osteosynthesis versus joint replacement. Orthopade 2014, 43, 314–324. [Google Scholar] [CrossRef] [PubMed]
- Hagino, T.; Ochiai, S.; Wako, M.; Sato, E.; Maekawa, S.; Hamada, Y. Comparison of the prognosis among different age groups in elderly patients with hip fracture. Indian J. Orthop. 2008, 42, 29–32. [Google Scholar] [CrossRef]
- Blomfeldt, R.; Törnkvist, H.; Ponzer, S.; Söderqvist, A.; Tidermark, J. Internal fixation versus hemiarthroplasty for displaced fractures of the femoral neck in elderly patients with severe cognitive impairment. J. Bone Jt. Surg. Br. 2005, 87, 523–529. [Google Scholar] [CrossRef] [PubMed]
- Tidermark, J. Quality of life and femoral neck fractures. Acta Orthop. Scand. Suppl. 2003, 74, 1–42. [Google Scholar] [CrossRef] [PubMed]
- Knobe, M.; Drescher, W.; Heussen, N.; Sellei, R.M.; Pape, H.C. Is helical blade nailing superior to locked minimally invasive plating in unstable pertrochanteric fractures? Clin. Orthop. Relat. Res. 2012, 470, 2302–2312. [Google Scholar] [CrossRef] [Green Version]
- Handoll, H.H.; Parker, M.J. Conservative versus operative treatment for hip fractures in adults. Cochrane Database Syst. Rev. 2008, 4, CD000337. [Google Scholar] [CrossRef]
- Marottoli, R.A.; Berkman, L.F.; Cooney, L.M., Jr. Decline in physical function following hip fracture. J. Am. Geriatr. Soc. 1992, 40, 861–866. [Google Scholar] [CrossRef] [PubMed]
- Hornby, R.; Evans, J.G.; Vardon, V. Operative or conservative treatment for trochanteric fractures of the femur. A randomised epidemiological trial in elderly patients. J. Bone Jt. Surg. Br. 1989, 71, 619–623. [Google Scholar] [CrossRef]
- Parker, M.J.; Handoll, H.H. Pre-operative traction for fractures of the proximal femur in adults. Cochrane Database Syst. Rev. 2006, 3, CD000168. [Google Scholar] [CrossRef] [Green Version]
- Biz, C.; Fantoni, I.; Crepaldi, N.; Zonta, F.; Buffon, L.; Corradin, M.; Lissandron, A.; Ruggieri, P. Clinical practice and nursing management of pre-operative skin or skeletal traction for hip fractures in elderly patients: A cross-sectional three-institution study. Int. J. Orthop. Trauma Nurs. 2019, 32, 32–40. [Google Scholar] [CrossRef]
- Flierl, M.A.; Stahel, P.F.; Hak, D.J.; Morgan, S.J.; Smith, W.R. Traction table-related complications in orthopaedic surgery. J. Am. Acad. Orthop. Surg. 2010, 18, 668–675. [Google Scholar] [CrossRef]
- Şahin, E.; Songür, M.; Kalem, M.; Zehir, S.; Aksekili, M.A.; Keser, S.; Bayar, A. Traction table versus manual traction in the intramedullary nailing of unstable intertrochanteric fractures: A prospective randomized trial. Injury 2016, 47, 1547–1554. [Google Scholar] [CrossRef] [PubMed]
- Ganse, B.; Böhle, F.; Pastor, T.; Gueorguiev, B.; Altgassen, S.; Gradl, G.; Kim, B.S.; Modabber, A.; Nebelung, S.; Hildebrand, F.; et al. Microcirculation After Trochanteric Femur Fractures: A Prospective Cohort Study Using Non-invasive Laser-Doppler Spectrophotometry. Front. Physiol. 2019, 10, 236. [Google Scholar] [CrossRef] [Green Version]
- Bentov, I.; Reed, M.J. Anesthesia, microcirculation, and wound repair in aging. Anesthesiology 2014, 120, 760–772. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soneja, A.; Drews, M.; Malinski, T. Role of nitric oxide, nitroxidative and oxidative stress in wound healing. Pharmacol. Rep. 2005, 57, 108–119. [Google Scholar] [PubMed]
- Forst, T.; Hohberg, C.; Tarakci, E.; Forst, S.; Kann, P.; Pfützner, A. Reliability of lightguide spectrophotometry (O2C) for the investigation of skin tissue microvascular blood flow and tissue oxygen supply in diabetic and nondiabetic subjects. J. Diabetes Sci. Technol. 2008, 2, 1151–1156. [Google Scholar] [CrossRef] [PubMed]
- Ganse, B.; Pishnamaz, M.; Kobbe, P.; Herren, C.; Gradl-Dietsch, G.; Böhle, F.; Johannes, B.; Kim, B.-S.; Horst, K.; Knobe, M. Microcirculation in open vs. minimally invasive dorsal stabilization of thoracolumbar fractures. PLoS ONE 2017, 12, e0188115. [Google Scholar] [CrossRef] [Green Version]
- Bläsius, F.M.; Link, B.C.; Beeres, F.J.P.; Iselin, L.D.; Leu, B.M.; Gueorguiev, B.; Klos, K.; Ganse, B.; Nebelung, S.; Modabber, A.; et al. Impact of surgical procedures on soft tissue microcirculation in calcaneal fractures: A prospective longitudinal cohort study. Injury 2019, 50, 2332–2338. [Google Scholar] [CrossRef]
- Ljung, P.; Bornmyr, S.; Svensson, H. Wound healing after total elbow replacement in rheumatoid arthritis. Wound complications in 50 cases and laser-Doppler imaging of skin microcirculation. Acta Orthop. Scand. 1995, 66, 59–63. [Google Scholar] [CrossRef]
- Kösters, A.K.; Ganse, B.; Gueorguiev, B.; Klos, K.; Modabber, A.; Nebelung, S.; Kim, B.S.; Knobe, M. Effects of low-intensity pulsed ultrasound on soft tissue micro-circulation in the foot. Int. Orthop. 2017, 41, 2067–2074. [Google Scholar] [CrossRef]
- Bosutti, A.; Egginton, S.; Barnouin, Y.; Ganse, B.; Rittweger, J.; Degens, H. Local capillary supply in muscle is not determined by local oxidative capacity. J. Exp. Biol. 2015, 218, 3377–3380. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Braverman, I.M. The cutaneous microcirculation. J. Investig. Dermatol. Symp. Proc. 2000, 5, 3–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yvonne-Tee, G.B.; Rasool, A.H.G.; Halim, A.S.; Rahman, A.R.A. Reproducibility of different laser Doppler fluximetry parameters of postocclusive reactive hyperemia in human forearm skin. J. Pharmacol. Toxicol. Methods 2005, 52, 286–292. [Google Scholar] [CrossRef] [PubMed]


| Depth (mm) | t0 (AU) | t1 (AU) | p-Value | |
|---|---|---|---|---|
| SO2 | 2 | 13.33 ± 17.37 | 13.33 ± 16.62 | p = 0.751 |
| 8 | 65.00 ± 14.24 | 71.00 ± 17.24 | p = 0.308 | |
| 15 | 64.67 ± 10.89 | 63.67 ± 12.05 | p = 0.955 | |
| Hb | 2 | 36.00 ± 9.95 | 34.67 ± 9.88 | p = 0.651 |
| 8 | 30.67 ± 8.47 | 29.33 ± 10.45 | p = 0.928 | |
| 15 | 27.67 ± 7.55 | 28.83 ± 4.63 | p = 0.926 | |
| Flow | 2 | 11.83 ± 11.11 | 11.33 ± 10.85 | p = 0.829 |
| 8 | 96.00 ± 42.27 | 97.00 ± 46.95 | p = 0.866 | |
| 15 | 173.00 ± 198.06 | 138.33 ± 64.93 | p = 0.411 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van Knegsel, K.P.; Ganse, B.; Haefeli, P.C.; Migliorini, F.; Scaglioni, M.F.; van de Wall, B.J.M.; Kim, B.-S.; Link, B.-C.; Beeres, F.J.P.; Nebelung, S.; et al. Trochanteric Femur Fractures: Application of Skeletal Traction during Surgery Does Not Alter Soft-Tissue Microcirculation. Medicina 2021, 57, 884. https://doi.org/10.3390/medicina57090884
van Knegsel KP, Ganse B, Haefeli PC, Migliorini F, Scaglioni MF, van de Wall BJM, Kim B-S, Link B-C, Beeres FJP, Nebelung S, et al. Trochanteric Femur Fractures: Application of Skeletal Traction during Surgery Does Not Alter Soft-Tissue Microcirculation. Medicina. 2021; 57(9):884. https://doi.org/10.3390/medicina57090884
Chicago/Turabian Stylevan Knegsel, Kenneth P., Bergita Ganse, Pascal C. Haefeli, Filippo Migliorini, Mario F. Scaglioni, Bryan J. M. van de Wall, Bong-Sung Kim, Björn-Christian Link, Frank J. P. Beeres, Sven Nebelung, and et al. 2021. "Trochanteric Femur Fractures: Application of Skeletal Traction during Surgery Does Not Alter Soft-Tissue Microcirculation" Medicina 57, no. 9: 884. https://doi.org/10.3390/medicina57090884








