1. Introduction
Periapical lesions of the jaws are most commonly of endodontic origin and are related to pulp infection [
1,
2]. Most lesions of endodontic origin can be classified as either periapical granuloma or radicular cyst. The reported prevalence of radicular cysts within periapical lesions varies between 6–55% [
2,
3]. In an analysis of 2030 cystic lesions of the jaws, the prevalence of radicular cysts was 42% and the most common diagnosis of cysts of the jaws [
4].
In the 2017 edition of the World Health Organization (WHO) classification of odontogenic lesions, radicular cysts were included in the inflammatory cyst group. A subclassification of this category includes radicular cyst (apical and periodontal cysts) and inflammatory collateral cysts (paradental cyst, buccal bifurcation cyst) [
5].
Radicular cysts are a sequel of a chronically inflamed granulation tissue (the periapical granuloma) located adjacent to the apex of either endodontically or non-endodontically treated teeth with an infected root canal system [
2,
6,
7]. However, the effects of a previous root canal treatment on the clinical presentation of these cysts, such as the size of the lesion size and the clinical symptoms, are still unclear.
It has been reported that radicular cysts are more frequently found in the maxilla [
8], occurring almost ten times more frequently than in the mandible [
9]. Most radicular cysts range in size from 5 to 15 mm. However, in the maxilla, a cyst may enlarge more than 15 mm [
10,
11,
12,
13]).
Thus, the development of these large maxillary cysts, and the effect of a previous root canal treatment on the clinical presentation is of a particular interest.
In this study, we retrospectively collected all cases of maxillary radicular cysts referred to a Oral and Maxillofacial Surgery Department of a large tertiary public hospital (Rabin Medical Center, Petach Tikva, Israel), over a period of 6 years, in order to evaluate the effect of a previous root canal treatment on the clinical presentation of large maxillary radicular cysts.
2. Materials and Methods
A retrospective review of all the radicular cysts treated at the Oral Maxillofacial Surgery Department of Rabin Medical Center, Petach Tikva, Israel for a period of 6 years (November 2012–November 2018). The study was approved by the institutional review board of authors’ hospital (00-88-19RMC).
The search was done based on pathological diagnostic code (Radicular Cyst) and according to the WHO classification of odontogenic lesions, subclassification radicular cyst, our search did not include other inflammatory collateral cysts such as paradental and buccal bifurcation cysts. Data was classified by the main investigator and the following characteristics were collected: age at diagnosis, gender, history of previous root canal treatment (yes/no), presence of swelling or expansion (yes/no), tooth location (divided to: central\lateral incisor; Canine; 1st\2nd premolar\molar teeth), largest dimension, presence of periapical lesions in other teeth, involvement of nasal floor and treatment performed (endodontic treatment/apicoectomy/enucleation/extraction/decompression/combination of treatments).
The cysts were measured by the main investigator on panoramic radiographs or cone bean computerized tomography (CBCT). The size of the periapical lesions was recorded at their widest horizontal or vertical diameters and the presence or absence of a radiopaque lamina of the periapical lesions was recorded.
Biopsy procedure was either incisional or excisional depending on the size of the lesion. The specimens were fixed in 4% neutral-buffered formaldehyde and processed for paraffin embedding. Specimens were sectioned and stained with hematoxylin and eosin using standard techniques. All the samples were analyzed by the same oral pathologist.
Radicular cysts were diagnosed histologically by demonstrating a lumen at least partially lined by stratified squamous epithelium and a connective tissue wall with various amounts of chronic and acute inflammatory cells [
7].
Patients were divided in two groups. The first group included patients with a radicular cyst from a tooth with previous endodontic treatment (study group). The second group included patients with a radicular cyst without a previous endodontic treatment (comparison group).
Data analysis was perform using the Statistical Analysis System software (SAS©, Cary, NC, USA). T-test and Fisher’s exact test were used for grouped variables.
3. Results
Demographic Data and Clinical Characteristics
A total of 211 inflammatory cysts were treated over a period of 6 years. Of these patients, 57 were diagnosed with inflammatory cysts of the maxilla (3 residual and 54 radicular cysts). According to the WHO classification of odontogenic lesions, residual and radicular cyst are included in the same subclassification, t. Residual cysts were excluded from this point because it was not clear which teeth caused the initial infection.
The patients age ranged between 19 years to 70 years, with a mean age of 43.3 years.
Regarding gender distribution of the 54 patients, 24 were male and 30 were female.
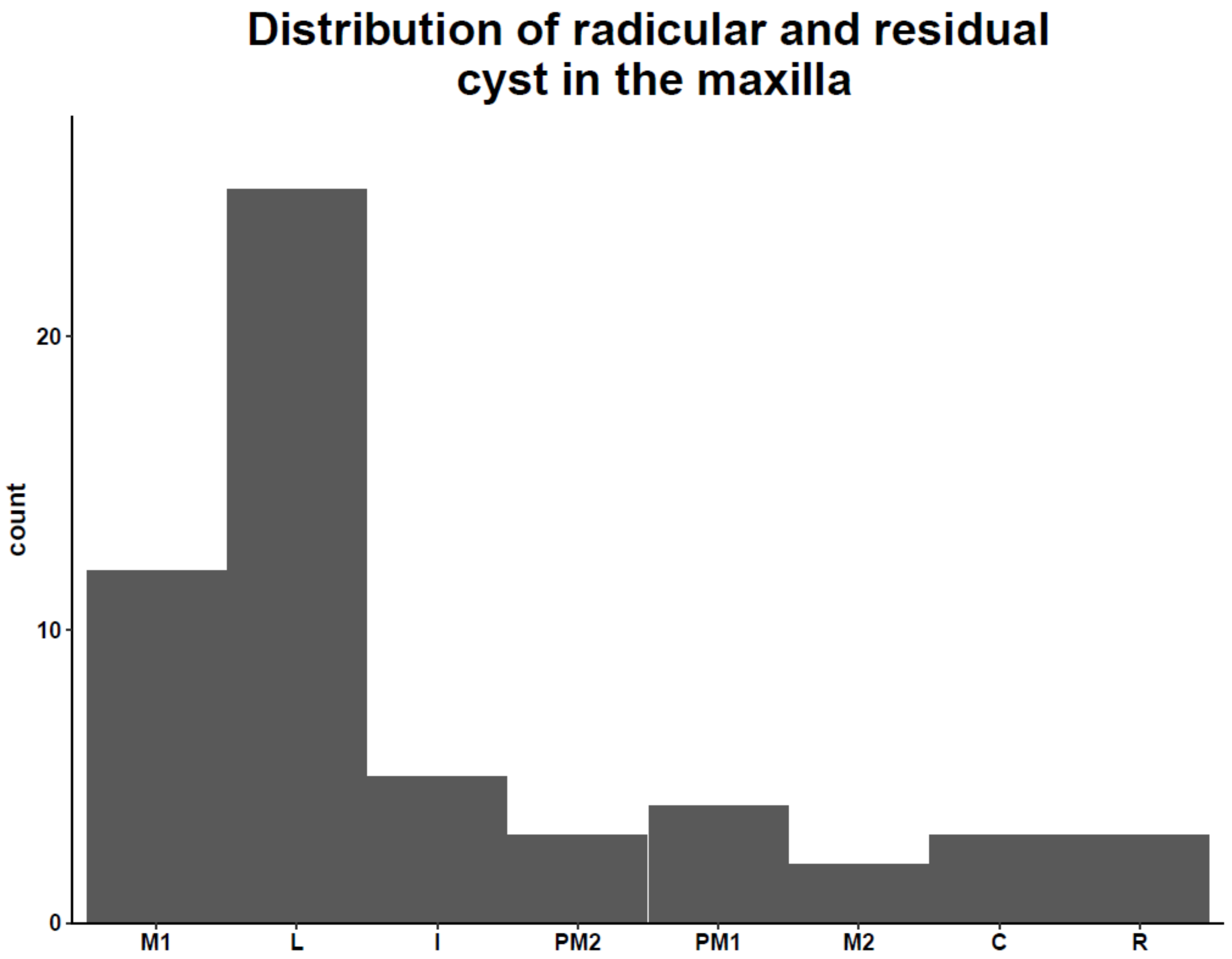
The lateral incisor was the most common tooth affected in the maxilla in 25 of the 54 cases (46.3%), first molar 12 of 54 cases (22.2%) and central incisor and first premolar equally involved in 5 cases (9.2%), the distribution between the affected teeth is presented in
Figure 1. In 20 cases, other periapical lesions were diagnosed in different teeth, and in 4 cases, bilateral lesions were found.
Having a history of root canal treatment was a major characteristic found in 45 of 54 patients (83.8%),
Figure 2. This finding was statistically significant in both women and men of all ages,
p-value for Char (Fisher) 0.286 Group 2, without endodontic treatment presented clinically with fewer acute symptoms at diagnosis in comparison to Group 1. A representation of all patients clinical and radiological findings can be seen in a
Figure 3, and the most common finding was endodontically treated teeth.
4. Treatment
All the patients underwent biopsy for histological diagnosis. Treatment modalities included: endodontic treatment with decompression, extraction and decompression, apicoectomy and enucleation, extraction and enucleation, extraction enucleation and bone graft. The treatment selection was based on dental status, size of the cyst and nasal floor or sinus involvement. In 2 cases in which the size of the cyst was 35 mm and 25 mm, oro-nasal fistula presented as a minor complication that was treated surgically in a second stage.
5. Discussion
This retrospective study focused on the effect of previous root canal treatment on the clinical presentation of large maxillary radicular cysts that were diagnosed and surgically treated in over period of six years in one medical center. The radicular cyst is the most common cyst of the jaws and probably one of the most common lesions in the jaws. Tamiolakis et al. recently reported that 57% of 5294 jaw cysts diagnosed in a single Oral Pathology Department during a 38-year period were radicular cysts [
6].
In most cases of radicular cysts of the maxilla, the involved tooth had been previously treated endodontically; however, from the results of the present study, it is impossible to determine the role of the root canal treatment on the etiology of the radicular cyst. Radicular cysts are formed in association with a tooth with infected root canal system [
3,
7,
14,
15,
16,
17,
18,
19,
20,
21,
22,
23,
24,
25]. These root canal infections may be divided into primary and secondary infections (Primary infections develop after an initial bacterial invasion into the pulp of non-endodontically treated teeth, while secondary infections occur following a previous root canal treatment (i.e., in endodontically treated teeth)) [
26]. The bacterial flora found in endodontically treated teeth completely differs in its phenotype and characteristics and is much more resistant and able to survive harsh conditions compared to the flora found in non-endodontically treated teeth [
27]. However, the effect of the type of root canal infection on the development of radicular cysts, and on their clinical presentation remain unclear.
The different composition of the endodontic flora and the interaction between different species is a subject of study in the literature and is believed to be responsible for the immunological host response and progression from apical granuloma to radicular cyst [
8,
9,
10].
Mortensen et al., 1970 [
12], indicated that lesions larger than 15–20 mm can be safely classified as cysts. However, various studies have indicated that basing diagnoses on radiographic analysis is not sufficient [
28]. Matsuda et al. [
29] concluded that it is not possible to confirm the diagnosis of lesions only through clinical and radiographic examination. In the current study, all cysts were confirmed histologically.
We have not included data about the frequency of all apical periodontitis lesions because most apical granulomas and sometimes radicular cyst are treated with conventional endodontic therapy without the need for biopsy [
30], so this did not match our inclusion criteria.
The results of our study confirm the results of other studies in which the anterior part of the maxilla is more commonly affected [
6]. No significant difference was found between females and males. Neither significant difference was found in age or size of the lesion between the two groups. The average age of diagnosis of radicular cyst was 43.4 years, this result is comparable to the results of Lo Muzio with a mean age of 38.4 [
4]. The lateral incisor was the most frequent tooth overall.
6. Conclusions
In our study, 83.8% of all large maxillary radicular cysts were diagnosed from a tooth with previous endodontic treatment, this finding was not reported in the literature. Moreover, the group with radicular cysts with previous endodontic treatment was prone to chronic infection and swelling in more cases than the group without endodontic treatment. The common profile that was identified in the current study was of a large radicular cyst associated with a symptomatic anterior lateral root canal treated tooth. New studies on the possible effects of the microbiology of endodontically and non-endodontically treated teeth are needed.
Author Contributions
Conceptualization, R.S.C., T.G., E.R.; methodology, G.C., R.S.C.; validation, T.G., E.R.; formal analysis, R.S.C., G.C.; investigation, R.S.C.; resources, G.C.; data curation, T.G., E.R., I.M.; writing—original draft preparation, R.S.C., G.C., G.A.; writing—review and editing, T.G., E.R, I.T., I.M., G.A; visualization, R.S.C., T.G., E.R.; supervision G.C, R.S.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was approved by the institutional review board of Rabin Medical Center, Petach Tikva, Israel (Approval No. 00-88-19RMC). Date of approval 05/03/2019.
Informed Consent Statement
Since this is a retrospective study, formal consent is not required.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kuc, I.; Peters, E.; Pan, J. Comparison of clinical and histologic diagnoses in periapical lesions. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2000, 89, 333–337. [Google Scholar] [CrossRef]
- Tsesis, I.; Krepel, G.; Koren, T.; Rosen, E.; Kfir, A. Accuracy for diagnosis of periapical cystic lesions. Sci. Rep. 2020, 10, 14155. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.V.; Craig, G.T.; Franklin, C.D. Range and demographics of odontogenic cysts diagnosed in a UK population over a 30-year period. J. Oral Pathol. Med. 2006, 35, 500–507. [Google Scholar] [CrossRef]
- Muzio, L.L.; Mascitti, M.; Santarelli, A.; Rubini, C.; Bambini, F.; Procaccini, M.; Bertossi, D.; Albanese, M.; Bondì, V.; Nocini, P.F. Cystic lesions of the jaws: A retrospective clinicopathologic study of 2030 cases. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2017, 124, 128–138. [Google Scholar] [CrossRef]
- Soluk-tekkesin, M.; Wright, J.M. The world health organization classification of odontogenic lesions: A summary of the changes of the 2017 (4th) edition. Turkish J. Pathol. 2013, 34, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Tamiolakis, P.; Thermos, G.; Tosios, K.I.; Sklavounou-Andrikopoulou, A. Demographic and Clinical Characteristics of 5294 Jaw Cysts: A Retrospective Study of 38 Years. Head Neck Pathol. 2019, 13, 587–596. [Google Scholar] [CrossRef]
- Tsesis, I.; Rosen, E.; Dubinsky, L.; Buchner, A.; Vered, M. Metaplastic changes in the epithelium of radicular cysts: A series of 711 cases. J. Clin. Exp. Dent. 2016, 8, e529–e533. [Google Scholar] [CrossRef] [PubMed]
- Joshi, N.S.; Sujan, S.G.; Rachappa, M.M. An unusual case report of bilateral mandibular radicular cysts. Contemp. Clin. Dent. 2011, 2, 59. [Google Scholar] [CrossRef]
- Bhaskar, S.N. Oral surgery-oral pathology conference no. 17, Walter Reed Army Medical Center. Periapical lesions-Types, incidence, and clinical features. Oral Surg. Oral Med. Oral Pathol. 1966, 21, 657–671. [Google Scholar] [CrossRef]
- Marx, R.E.; Stern, D. Oral and Maxillofacial Pathology: A Rationale for Diagnosis and Treatment; Quintessence Publishing: Chicago, IL, USA, 2012; p. 980. [Google Scholar]
- Çalışkan, M.K.; Kaval, M.E.; Tekin, U.; Ünal, T. Radiographic and histological evaluation of persistent periapical lesions associated with endodontic failures after apical microsurgery. Int. Endod. J. 2016, 49, 1011–1019. [Google Scholar] [CrossRef]
- Mortensen, H.; Winther, J.E.; Birn, H. Periapical granulomas and cysts: An investigation of 1,600 cases. Eur. J. Oral Sci. 1970, 78, 241–250. [Google Scholar] [CrossRef]
- Koju, S.; Chaurasia, N.; Marla, V.; Niroula, D.; Poudel, P. Radicular cyst of the anterior maxilla: An insight into the most common inflammatory cyst of the jaws. J. Dent. Res. Rev. 2019, 6, 26. [Google Scholar] [CrossRef]
- Nair, P.N.R.; Pajarola, G.; Schroeder, H.E. Types and incidence of human periapical lesions obtained with extracted teeth. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1996, 81, 93–102. [Google Scholar] [CrossRef]
- Reeve, C.M.; Wentz, F.M. The prevalence, morphology, and distribution of epithelial rests in the human periodontal ligament. Oral Surg. Oral Med. Oral Pathol. 1962, 15, 785–793. [Google Scholar] [CrossRef]
- Seltzer, S.; Soltanoff, W.; Bender, I.B. Epithelial proliferation in periapical lesions. Oral Surg. Oral Med. Oral Pathol. 1969, 27, 111–121. [Google Scholar] [CrossRef]
- Shear, M.; Speight, P. Cysts of the Oral and Maxillofacial Regions, 4th ed.; Blackwell Munksgaard: Oxford, UK, 2007. [Google Scholar]
- Bergenholtz, G.; Lekholm, U.; Liljenberg, B.; Lindhe, J. Morphometric analysis of chronic inflammatory periapical lesions in root-filled teeth. Oral Surg. Oral Med. Oral Pathol. 1983, 55, 295–301. [Google Scholar] [CrossRef]
- Grossmann, S.M.; Machado, V.C.; Xavier, G.M.; Moura, M.D.; Gomez, R.S.; Aguiar, M.C.F.; Mesquita, R.A. Demographic profile of odontogenic and selected nonodontogenic cysts in a Brazilian population. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2007, 104. [Google Scholar] [CrossRef]
- Kreidler, J.F.; Raubenheimer, E.J.; van Heerden, W.F.P. A retrospective analysis of 367 cystic lesions of the jaw-the Ulm experience. J. Cranio-Maxillofac. Surg. 1993, 21, 339–341. [Google Scholar] [CrossRef]
- Kronfeld, R. Histopathology of the Teeth and Their Surrounding Structures; Lea & Febiger: Philadelphia, PA, USA, 1939. [Google Scholar]
- Langeland, K.; Conn, F.; Block, R.M.; Va, R.; Grossman, L.I. A histopathologic and histobacteriologic study of 35 periapical endodontic surgical specimens. J. Endod. 1977, 3, 8–23. [Google Scholar] [CrossRef]
- Lin, L.M.; Huang, G.T.J.; Rosenberg, P.A. Proliferation of Epithelial Cell Rests, Formation of Apical Cysts, and Regression of Apical Cysts after Periapical Wound Healing. J. Endod. 2007, 33, 908–916. [Google Scholar] [CrossRef] [PubMed]
- Nair, P.N.R. Review New perspectives on radicular cysts: Do they heal? Int. Endod. J. 1998, 179, 155–160. [Google Scholar]
- Nair, P.N.R. Pathways of the Pulp, 8th ed.; Cohen, S., Burns, R.C., Eds.; Mosby: St Louis, MO, USA, 2002; pp. 458–459. [Google Scholar]
- Siqueira, J.; Rôças, I. Diversity of endodontic microbiota revisited. J. Dent. Res. 2009, 88, 969–981. [Google Scholar] [CrossRef]
- Neelakantan, P.; Romero, M.; Vera, J.; Daood, U.; Khan, A.U.; Yan, A.; Cheung, G.S.P. Biofilms in Endodontics—Current status and future directions. Int. J. Mol. Sci. 2017, 18, 1748. [Google Scholar] [CrossRef] [PubMed]
- Ricucci, D.; Mannocci, F.; Pitt Ford, T.R. A study of periapical lesions correlating the presence of a radiopaque lamina with histological findings. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2006, 101, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, V.; Kadowaki, A.C.N.; Kataoka, S.H.H.; Caldeira, C.L. A comparison of clinical, histological and radiographic findings in periapical radiolucid lesions. Dent. Press Endod. 2011, 1, 17–21. [Google Scholar]
- Kvist, T.; Reit, C. Results of endodontic retreatment: A randomized clinical study comparing surgical and nonsurgical procedures. J. Endod. 1999, 25, 814–817. [Google Scholar] [CrossRef]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).