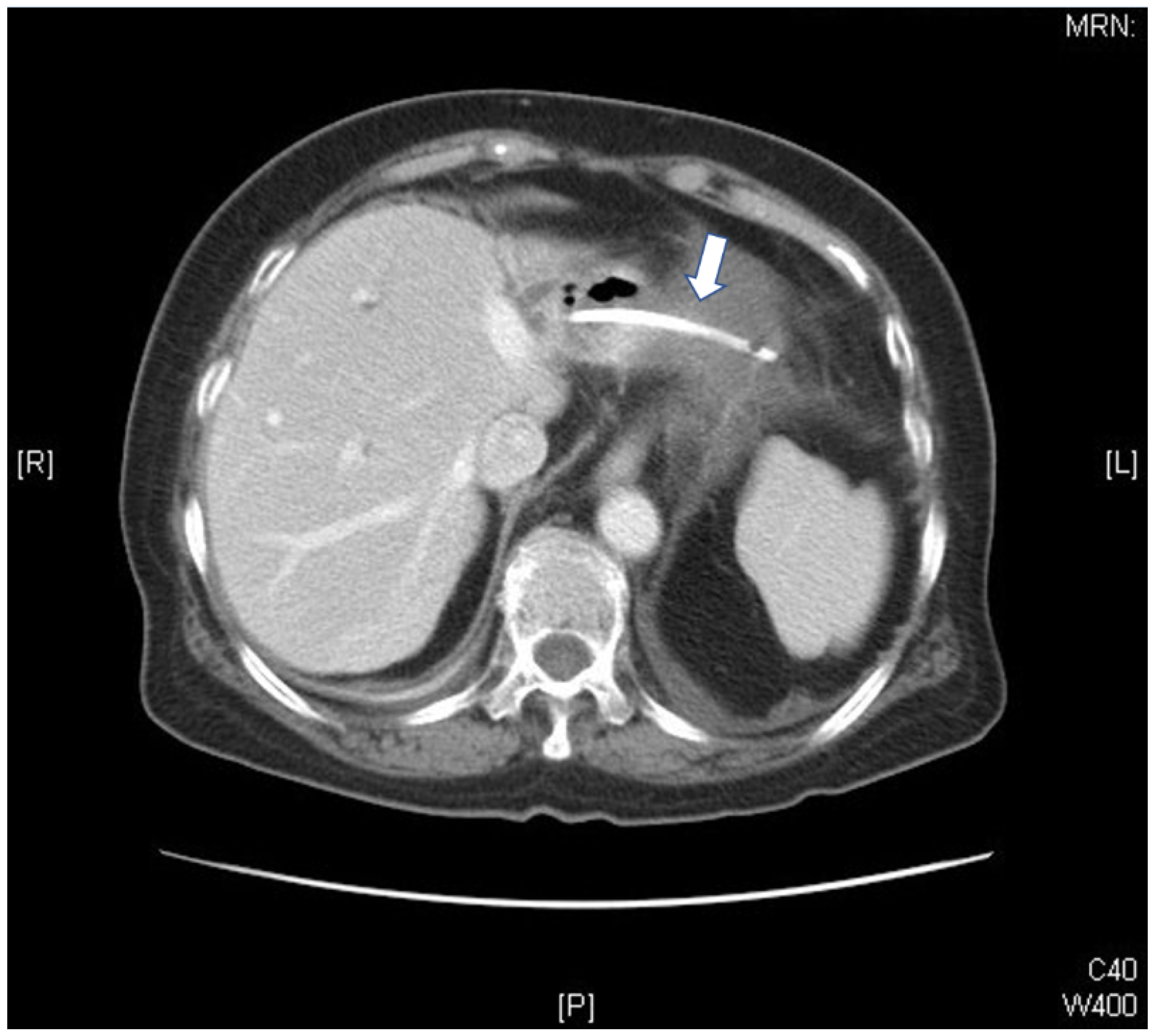
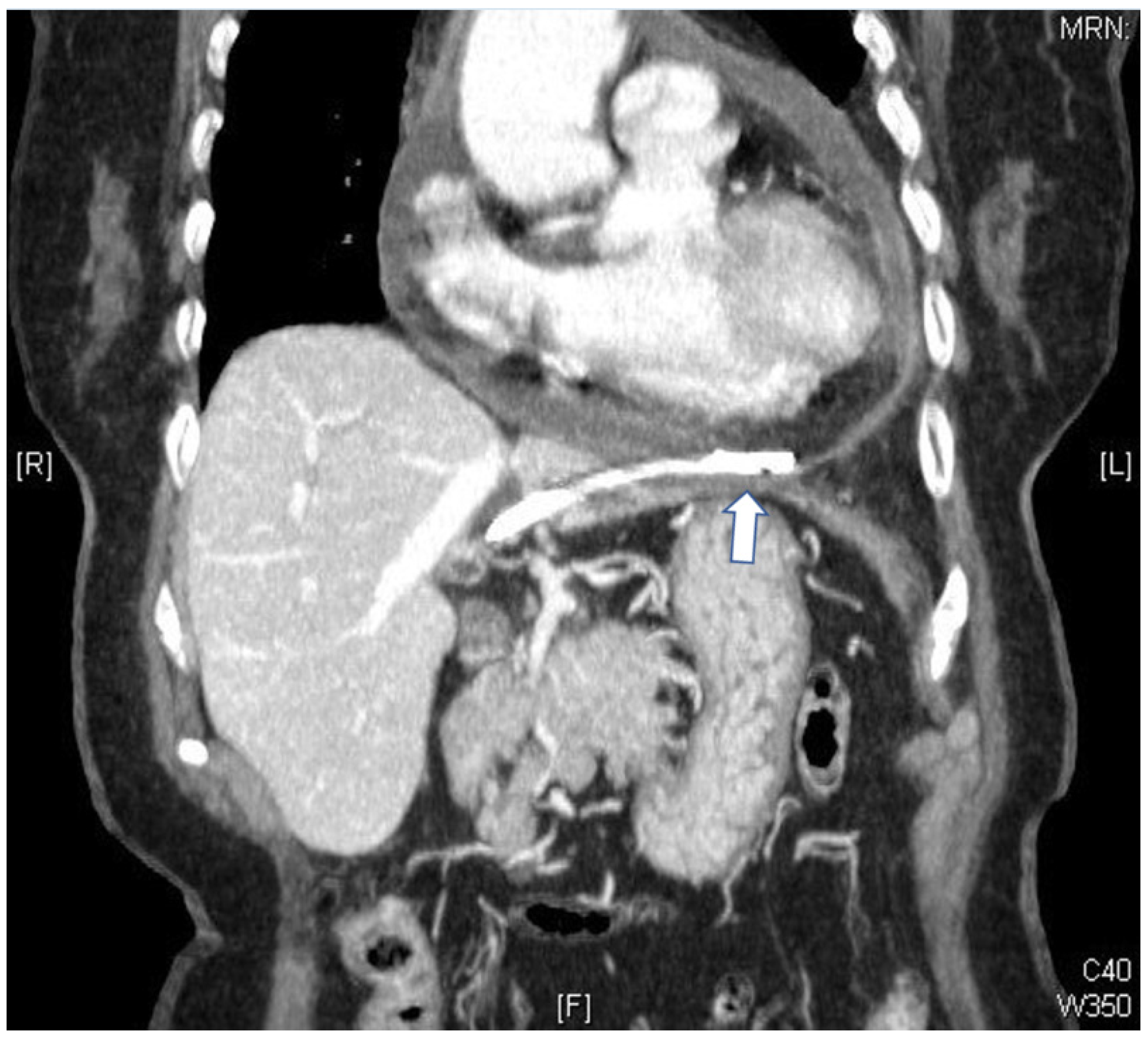
Bacterial Pericarditis Caused by Penetration of a Migrated Biliary Stent from the Lateral Segment of the Liver: A Case Report
Abstract
:1. Introduction
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dumonceau, J.M.; Tringali, A.; Blero, D.; Deviere, J.; Laugiers, R.; Heresbach, D.; Costamagna, G.; European Society of Gastrointestinal Endoscopy. Biliary stenting: Indications, choice of stents and results: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy 2012, 44, 277–298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trejo-Avila, M.; Valenzuela-Salazar, C.; Herrera-Esquivel, J.J. Biliary stent-induced duodenal perforation. Rev. Gastroenterol. Mex. 2020, 85, 358–359. [Google Scholar] [CrossRef] [PubMed]
- Arhan, M.; Odemiş, B.; Parlak, E.; Ertuğrul, I.; Başar, O. Migration of biliary plastic stents: Experience of a tertiary center. Surg. Endosc. 2009, 23, 769–775. [Google Scholar] [CrossRef]
- Katsinelos, P.; Kountouras, J.; Paroutoglou, G.; Chatzimavroudis, G.; Paikos, D.; Zavos, C.; Karakousis, K.; Gelas, G.; Tzilves, D. Migration of plastic biliary stents and endoscopic retrieval: An experience of three referral centers. Surg. Laparosc. Endosc. Percutan. Tech. 2009, 19, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Namdar, T.; Raffel, A.M.; Topp, S.A.; Namdar, L.; Alldinger, I.; Schmitt, M.; Knoefel, W.T.; Eisenberger, C.F. Complications and treatment of migrated biliary endoprostheses: A review of the literature. World J. Gastroenterol. 2007, 13, 5397–5399. [Google Scholar] [CrossRef] [Green Version]
- Soto-Avila, J.J.; Gómez-Wong, M.E.; Preciado-Hernández, F. Colovesical fistula secondary to the migration of a biliary stent. Case report. Cir. Cir. 2006, 74, 473–475. [Google Scholar]
- Liebich-Bartholain, L.; Kleinau, U.; Elsbernd, H.; Buchsel, R. Biliary pneumonitis after proximal stent migration. Gastrointest. Endosc. 2001, 54, 382–384. [Google Scholar] [CrossRef]
- Shah, O.J.; Khan, F.A.; Robanni, I.; Wani, N.A. Hepatic perforation: A complication of proximal biliary stent migration. Endoscopy 2004, 36, 1040. [Google Scholar] [CrossRef] [Green Version]
- Mangiavillano, B.; Pagano, N.; Baron, T.H.; Luigiano, C. Outcome of stenting in biliary and pancreatic benign and malignant diseases: A comprehensive review. World J. Gastroenterol. 2015, 21, 9038–9054. [Google Scholar] [CrossRef]
- Wurbs, D. The development of biliary drainage and stenting. Endoscopy 1998, 30, A 202–A 206. [Google Scholar] [CrossRef]
- Deviere, J.; Baize, M.; de Toeuf, J.; Cremer, M. Long-term follow-up of patients with hilar malignant stricture treated by endoscopic internal biliary drainage. Gastrointest. Endosc. 1988, 34, 95–101. [Google Scholar] [CrossRef]
- Lahoti, S.; Catalano, M.F.; Geenen, J.E.; Schmalz, M.J. Endoscopic retrieval of proximally migrated biliary and pancreatic stents: Experience of a large referral center. Gastrointest. Endosc. 1998, 47, 486–491. [Google Scholar] [CrossRef]
- Johanson, J.F.; Schmalz, M.J.; Geenen, J.E. Incidence and risk factors for biliary and pancreatic stent migration. Gastrointest. Endosc. 1992, 38, 341–346. [Google Scholar] [CrossRef]
- Emara, M.H.; Ahmed, M.H.; Mohammed, A.S.; Radwan, M.I.; Mahros, A.M. Biliary stent migration: Why, how, and what? Eur. J. Gastroenterol. Hepatol. 2021, 33, 967–973. [Google Scholar] [CrossRef] [PubMed]
- Malgras, B.; Pierret, C.; Tourtier, J.P.; Olagui, G.; Nizou, C.; Duverger, V. Double Sigmoid colon perforation due to migration of a biliary stent. J. Visc. Surg. 2011, 148, e397–e399. [Google Scholar] [CrossRef] [PubMed]
- Culnan, D.M.; Cicuto, B.J.; Singh, H.; Cherry, R.A. Percutaneous retrieval of a biliary stent after migration and ileal perforation. World J. Emerg. Surg. 2009, 4, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karim, A.; Orbell, J.H.; Bhatti, K.; Chaudhary, B.; Parvaiz, A. Biliary stent migration presenting as a recurrent abdominal wall abscess with underlying enterocutaneous fistula. Gastrointest. Endosc. 2006, 63, 874–876. [Google Scholar] [CrossRef]
- Basile, A.; Macri, A.; Lamberto, S.; Caloggero, S.; Versaci, A.; Famulari, C. Duodenoscrotal fistula secondary to retroperitoneal migration of an endoscopically placed plastic biliary stent. Gastrointest. Endosc. 2003, 57, 136–138. [Google Scholar] [CrossRef]
- Katz, R.; Meretyk, S.; Gimmon, Z. Abdominal compartment syndrome due to delayed identification of a ureteral perforation following abdomino-perineal resection for rectal carcinoma. Int. J. Urol. 1997, 4, 615–617. [Google Scholar] [CrossRef]
- Dumonceau, J.M.; Tringali, A.; Papanikolaou, I.S.; Blero, D.; Mangiavillano, B.; Schmidt, A.; Vanbiervliet, G.; Costamagna, G.; Devière, J.; García-Cano, J.; et al. Endoscopic biliary stenting: Indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline-Updated October 2017. Endoscopy 2018, 50, 910–930. [Google Scholar] [CrossRef] [Green Version]
- Williams, E.; Beckingham, I.; El Sayed, G.; Gurusamy, K.; Sturgess, R.; Webster, G.; Young, T. Updated guideline on the management of common bile duct stones (CBDS). Gut 2017, 66, 765–782. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yuan, X.L.; Ye, L.S.; Liu, Q.; Wu, C.C.; Liu, W.; Zeng, X.H.; Zhang, Y.H.; Guo, L.J.; Zhang, Y.Y.; Li, Y.; et al. Risk factors for distal migration of biliary plastic stents and related duodenal injury. Surg. Endosc. 2020, 34, 1722–1728. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kendall, B.J.; Jutabha, R.; So, L.; Jamidar, P.A. Determining required stent length in endoscopic retrograde biliary stenting. Gastrointest. Endosc. 1995, 41, 242–243. [Google Scholar] [CrossRef]
- Katsinelos, P.; Lazaraki, G.; Gkagkalis, S.; Chatzimavroudis, G.; Anastasiadou, K.; Georgakis, N.; Giouleme, O.; Zavos, C.; Kountouras, J. A fully covered self-expandable metal stent anchored by a 10-Fr double pigtail plastic stent: An effective anti-migration technique. Ann. Gastroenterol. 2017, 30, 114–117. [Google Scholar] [CrossRef]
- Weigt, J.; Kandulski, A.; Malfertheiner, P. Anatomy-shaped design of a fully-covered, biliary, self-expandable metal stent for treatment of benign distal biliary strictures. Endosc. Int. Open. 2016, 4, E79–E82. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chao, H.-Y.; Li, C.-H.; Chen, S.-Y. Bacterial Pericarditis Caused by Penetration of a Migrated Biliary Stent from the Lateral Segment of the Liver: A Case Report. Medicina 2022, 58, 132. https://doi.org/10.3390/medicina58010132
Chao H-Y, Li C-H, Chen S-Y. Bacterial Pericarditis Caused by Penetration of a Migrated Biliary Stent from the Lateral Segment of the Liver: A Case Report. Medicina. 2022; 58(1):132. https://doi.org/10.3390/medicina58010132
Chicago/Turabian StyleChao, Hsiao-Yun, Chih-Huang Li, and Shou-Yen Chen. 2022. "Bacterial Pericarditis Caused by Penetration of a Migrated Biliary Stent from the Lateral Segment of the Liver: A Case Report" Medicina 58, no. 1: 132. https://doi.org/10.3390/medicina58010132
APA StyleChao, H. -Y., Li, C. -H., & Chen, S. -Y. (2022). Bacterial Pericarditis Caused by Penetration of a Migrated Biliary Stent from the Lateral Segment of the Liver: A Case Report. Medicina, 58(1), 132. https://doi.org/10.3390/medicina58010132





