Delayed Onset Bilateral Papilledema in a Young Boy’s Eyes after Trauma
Abstract
:1. Introduction
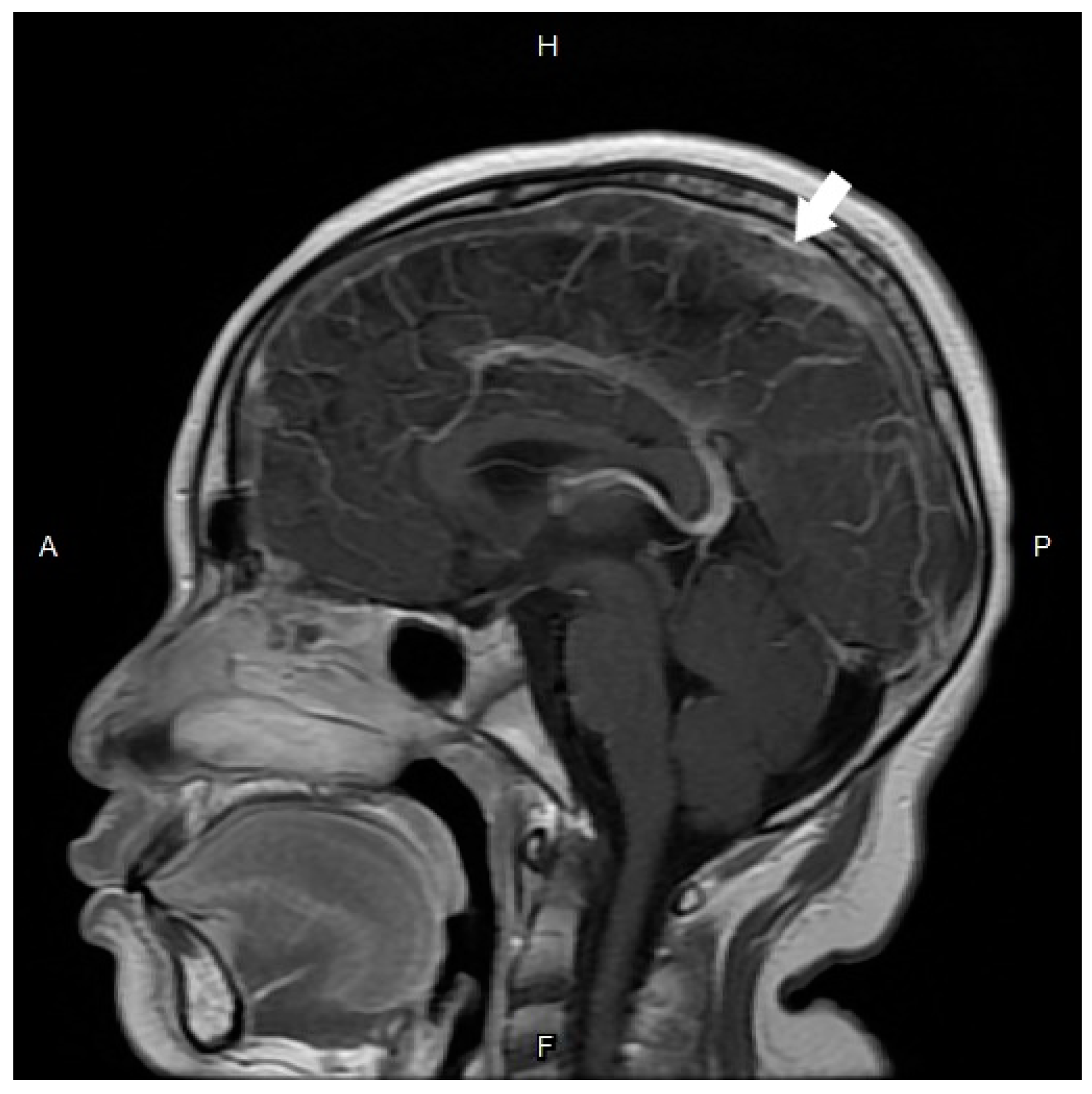
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Maali, L.; Khan, S.; Qeadan, F.; Ismail, M.; Ramaswamy, D.; Hedna, V.S. Cerebral venous thrombosis: Continental disparities. Neurol. Sci. 2017, 38, 1963–1968. [Google Scholar] [CrossRef] [PubMed]
- Capecchi, M.; Abbattista, M.; Martinelli, I. Cerebral venous sinus thrombosis. J. Thromb. Haemost. 2018, 16, 1918–1931. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agrawal, K.; Burger, K.; Rothrock, J.F. Cerebral Sinus Thrombosis. Headache 2016, 56, 1380–1389. [Google Scholar] [CrossRef] [PubMed]
- Ferro, J.M.; Canhão, P.; Stam, J.; Bousser, M.G.; Barinagarrementeria, F. Prognosis of cerebral vein and dural sinus thrombosis: Results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke 2004, 35, 664–670. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dlamini, N.; Billinghurst, L.; Kirkham, F.J. Cerebral venous sinus (sinovenous) thrombosis in children. Neurosurg. Clin. N. Am. 2010, 21, 511–527. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Rourke, T.L.; Slagle, W.S.; Elkins, M.; Eckermann, D.; Musick, A. Papilloedema associated with dural venous sinus thrombosis. Clin. Exp. Optom. 2014, 97, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.C.; Bhatti, M.T.; Chen, J.J.; Fairbanks, A.M.; Foroozan, R.; McClelland, C.M.; Lee, M.S.; Satija, C.E.; Francis, C.E.; Wildes, M.T.; et al. Presentation and Progression of Papilledema in Cerebral Venous Sinus Thrombosis. Am. J. Ophthalmol. 2020, 213, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Crassard, I.; Soria, C.; Tzourio, C.; Woimant, F.; Drouet, L.; Ducros, A.; Bousser, M.G. A negative D-dimer assay does not rule out cerebral venous thrombosis: A series of seventy-three patients. Stroke 2005, 36, 1716–1719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Damus, P.S.; Wallace, G.A. Immunologic measurement of antithrombin III-heparin cofactor and alpha2 macroglobulin in disseminated intravascular coagulation and hepatic failure coagulopathy. Thromb. Res. 1975, 6, 27–38. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, T.-Y.; Chien, K.-H. Delayed Onset Bilateral Papilledema in a Young Boy’s Eyes after Trauma. Medicina 2022, 58, 140. https://doi.org/10.3390/medicina58010140
Lin T-Y, Chien K-H. Delayed Onset Bilateral Papilledema in a Young Boy’s Eyes after Trauma. Medicina. 2022; 58(1):140. https://doi.org/10.3390/medicina58010140
Chicago/Turabian StyleLin, Ting-Yi, and Ke-Hung Chien. 2022. "Delayed Onset Bilateral Papilledema in a Young Boy’s Eyes after Trauma" Medicina 58, no. 1: 140. https://doi.org/10.3390/medicina58010140
APA StyleLin, T. -Y., & Chien, K. -H. (2022). Delayed Onset Bilateral Papilledema in a Young Boy’s Eyes after Trauma. Medicina, 58(1), 140. https://doi.org/10.3390/medicina58010140






