Compression Stockings Improve Cardiac Output and Cerebral Blood Flow during Tilt Testing in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) Patients: A Randomized Crossover Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cerebral Blood Flow (CBF) Measurements: Acquisition and Analysis
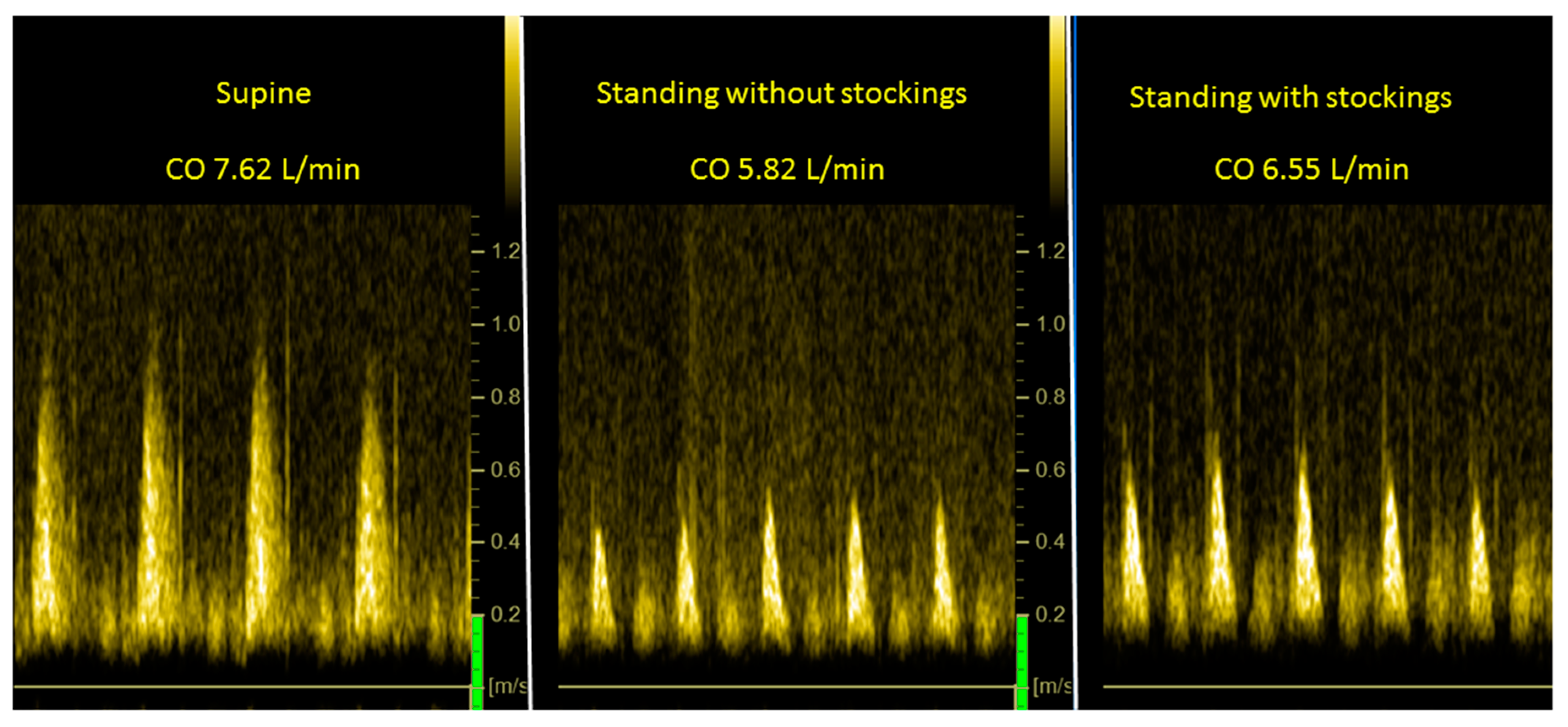
2.2. Doppler Measurements for Cardiac Output (CO) Determination: Acquisition and Analysis
2.3. Statistical Analysis
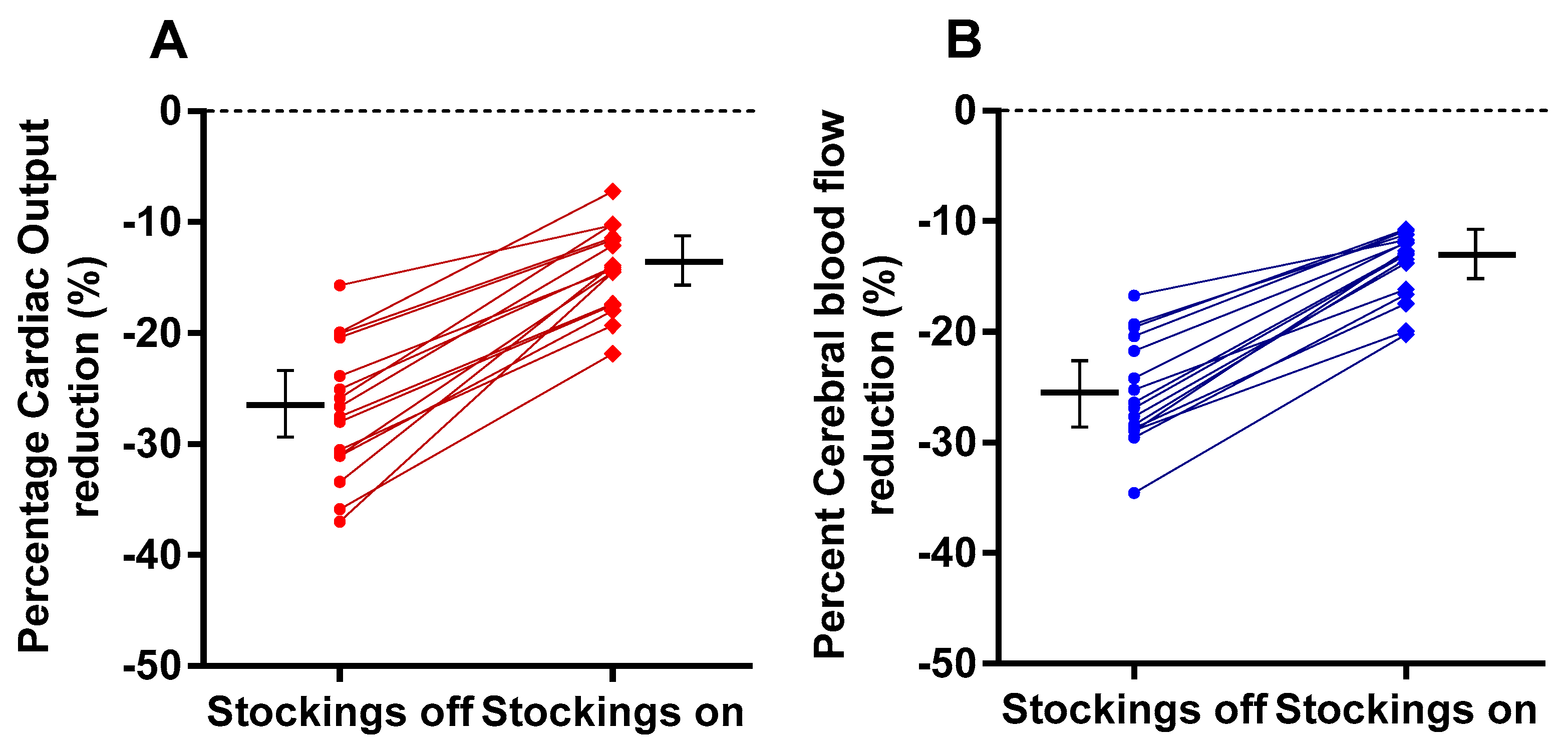
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Institute Of Medicine (IOM) (Ed.) Beyond Mayalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness; The National Academies Press: Washington, DC, USA, 2015. [Google Scholar]
- Jason, L.A.; Evans, M.; So, S.; Scott, J.; Brown, A. Problems in Defining Post-Exertional Malaise. J. Prev. Interv. Community 2015, 43, 20–31. [Google Scholar] [CrossRef] [Green Version]
- Loy, B.D.; O’Connor, P.J.; Dishman, R.K. Effect of Acute Exercise on Fatigue in People with ME/CFS/SEID: A Meta-analysis. Med. Sci. Sports Exerc. 2016, 48, 2003–2012. [Google Scholar] [CrossRef] [Green Version]
- Freeman, R.; Wieling, W.; Axelrod, F.B.; Benditt, D.G.; Benarroch, E.; Biaggioni, I.; Cheshire, W.; Chelimsky, T.; Cortelli, P.; Gibbons, C.H.; et al. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Auton. Neurosci. 2011, 161, 46–48. [Google Scholar] [CrossRef] [PubMed]
- Low, P.A.; Sandroni, P.; Joyner, M.; Shen, W.K. Postural tachycardia syndrome (POTS). J. Cardiovasc. Electrophysiol. 2009, 20, 352–358. [Google Scholar] [CrossRef] [Green Version]
- Van Campen, C.L.M.; Verheugt, F.W.; Rowe, P.C.; Visser, F.C. Cerebral blood flow is reduced in ME/CFS during head-up tilt testing even in the absence of hypotension or tachycardia: A quantitative, controlled study using Doppler echography. Clin. Neurophysiol. Pract. 2020, 5, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Bou-Holaigah, I.; Rowe, P.C.; Kan, J.; Calkins, H. The relationship between neurally mediated hypotension and the chronic fatigue syndrome. JAMA 1995, 274, 961–967. [Google Scholar] [CrossRef]
- De Lorenzo, F.; Hargreaves, J.; Kakkar, V.V. Pathogenesis and management of delayed orthostatic hypotension in patients with chronic fatigue syndrome. Clin. Auton. Res. 1997, 7, 185–190. [Google Scholar] [CrossRef]
- Kawamura, Y.; Kihara, M.; Nishimoto, K.; Taki, M. Efficacy of a half dose of oral pyridostigmine in the treatment of chronic fatigue syndrome: Three case reports. Pathophysiology 2003, 9, 189–194. [Google Scholar] [CrossRef]
- Naschitz, J.; Dreyfuss, D.; Yeshurun, D.; Rosner, I. Midodrine treatment for chronic fatigue syndrome. Postgrad. Med. J. 2004, 80, 230–232. [Google Scholar] [CrossRef] [PubMed]
- Blockmans, D.; Persoons, P.; Van, H.B.; Lejeune, M.; Bobbaers, H. Combination therapy with hydrocortisone and fludrocortisone does not improve symptoms in chronic fatigue syndrome: A randomized, placebo-controlled, double-blind, crossover study. Am. J. Med. 2003, 114, 736–741. [Google Scholar] [CrossRef]
- Peterson, P.K.; Pheley, A.; Schroeppel, J.; Schenck, C.; Marshall, P.; Kind, A.; Haugland, J.M.; Lambrecht, L.J.; Swan, S.; Goldsmith, S. A Preliminary Placebo-Controlled Crossover Trial of Fludrocortisone for Chronic Fatigue Syndrome. Arch. Intern. Med. 1998, 158, 908–914. [Google Scholar] [CrossRef] [PubMed]
- Rowe, P.C.; Calkins, H.; DeBusk, K.; McKenzie, R.; Anand, R.; Sharma, G.; Cuccherini, B.A.; Soto, N.; Hohman, P.; Snader, S.; et al. Fludrocortisone acetate to treat neurally mediated hypotension in chronic fatigue syndrome: A randomized controlled trial. JAMA 2001, 285, 52–59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Campen, C.L.M.C.; Verheugt, F.W.A.; Visser, F.C. Quantification of the beneficial effects of compression stockings on symptoms of exercise and orthostatic intolerance in chronic fatigue/myalgic encephalomyelitis patients. Int. J. Clin. Med. 2018, 9, 367–376. [Google Scholar] [CrossRef] [Green Version]
- Van Campen, C.L.M.C.; Rowe, P.C.; Visser, F.C. Cerebral Blood Flow Is Reduced in Severe Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Patients During Mild Orthostatic Stress Testing: An Exploratory Study at 20 Degrees of Head-Up Tilt Testing. Healthcare 2020, 8, 169. [Google Scholar] [CrossRef]
- Van Campen, C.L.M.C.; Rowe, P.C.; Visser, F.C. Reductions in Cerebral Blood Flow Can Be Provoked by Sitting in Severe My-algic Encephalomyelitis/Chronic Fatigue Syndrome Patients. Healthcare 2020, 8, 394. [Google Scholar] [CrossRef]
- Sheldon, R.S.; Grubb, B.P., 2nd; Olshansky, B.; Shen, W.K.; Calkins, H.; Brignole, M.; Raj, S.R.; Krahn, A.D.; Morillo, C.A.; Stewart, J.M.; et al. 2015 heart rhythm society expert consensus statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm 2015, 12, e41–e63. [Google Scholar] [CrossRef] [Green Version]
- Shen, W.K.; Sheldon, R.S.; Benditt, D.G.; Cohen, M.I.; Forman, D.E.; Goldberger, Z.D.; Grubb, B.P.; Hamdan, M.H.; Krahn, A.D.; Link, M.S.; et al. 2017 ACC/AHA/HRS Guideline for the Evaluation and Management of Patients with Syncope: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J. Am. Coll. Cardiol. 2017, 70, 620–663. [Google Scholar] [CrossRef]
- Martina, J.R.; Westerhof, B.E.; van Goudoever, J.; de Beaumont, E.M.H.; Truijen, J.; Kim, Y.S.; Immink, R.V.; Jöbsis, D.A.; Hollmann, M.W.; Lahpor, J.R.; et al. Noninvasive continuous arterial blood pressure monitoring with Nexfin(R). Anesthesiology 2012, 116, 1092–1103. [Google Scholar] [CrossRef] [Green Version]
- Van Campen, C.L.M.C.; Verheugt, F.W.A.; Visser, F.C. Cerebral blood flow changes during tilt table testing in healthy volunteers, as assessed by Doppler imaging of the carotid and vertebral arteries. Clin. Neurophysiol. Pract. 2018, 3, 91–95. [Google Scholar] [CrossRef]
- Van Campen, C.L.M.C.; Visser, F.C. The abnormal Cardiac Index and Stroke Volume Index changes during a normal Tilt Table Test in ME/CFS patients compared to healthy volunteers, are not related to deconditioning. J. Thromb. Circ. 2018, 2, 1–8. [Google Scholar]
- Van Campen, C.L.M.C.; Visser, F.C. Validation of Stroke volume measured with suprasternal aortic Doppler imaging: Com-parison to transthoracic Stroke Volume measurements. J. Thromb. Circ. 2018, 2, 1–5. [Google Scholar]
- Van Campen, C.L.M.C.; Visser, F.C.; de Cock, C.C.; Vos, H.S.; Kamp, O.; Visser, C.A. Comparison of the haemodynamics of dif-ferent pacing sites in patients undergoing resynchronisation treatment: Need for individualisation of lead localisation. Heart 2006, 92, 1795–1800. [Google Scholar] [CrossRef]
- Kusumoto, F.; Venet, T.; Schiller, N.B.; Sebastian, A.; Foster, E. Measurement of aortic blood flow by Doppler echocardiography: Temporal, technician, and reader variability in normal subjects and the application of generalizability theory in clinical research. J. Am. Soc. Echocardiogr. 1995, 8 Pt 1, 647–653. [Google Scholar] [CrossRef]
- Critchley, L.A.H.; Critchley, J.A.J.H. A Meta-Analysis of Studies Using Bias and Precision Statistics to Compare Cardiac Output Measurement Techniques. J. Clin. Monit. Comput. 1999, 15, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Orbach, E.J. Compression therapy of vein and lymph vessel diseases of the lower extremities: A present day overview. Angiology 1979, 30, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Rabe, E.; Partsch, H.; Hafner, J.; Lattimer, C.; Mosti, G.; Neumann, M.; Urbanek, T.; Huebner, M.; Gaillard, S.; Carpentier, P. Indications for medical compression stockings in venous and lymphatic disorders: An evidence-based consensus statement. Phlebology 2018, 33, 163–184. [Google Scholar] [CrossRef] [Green Version]
- Newton, J.L.; Frith, J. The efficacy of nonpharmacologic intervention for orthostatic hypotension associated with aging. Neurology 2018, 91, e652–e656. [Google Scholar] [CrossRef] [Green Version]
- Frith, J.; Newton, J.L. Combination non-pharmacologic intervention for orthostatic hypotension in older people: A phase 2 study. Age Ageing 2020, 49, 253–257. [Google Scholar] [CrossRef] [Green Version]
- Robinson, L.J.; Pearce, R.M.; Frith, J. Acceptability of non-drug therapies in older people with orthostatic hypotension: A qualitative study. BMC Geriatr. 2018, 18, 315. [Google Scholar] [CrossRef] [PubMed]
- Logan, I.C.; Witham, M. Efficacy of treatments for orthostatic hypotension: A systematic review. Age Ageing 2012, 41, 587–594. [Google Scholar] [CrossRef] [Green Version]
- Subbarayan, S.; Myint, P.K.; Martin, K.R.; Abraha, I.; Devkota, S.; O’Mahony, D. Nonpharmacologic Management of Orthostatic Hypotension in Older People: A Systematic Review. The SENATOR ONTOP Series. J. Am. Med. Dir. Assoc. 2019, 20, 1065–1073.e3. [Google Scholar] [CrossRef]
- Heyer, G.L. Abdominal and Lower-Extremity Compression Decreases Symptoms of Postural Tachycardia Syndrome in Youth during Tilt Table Testing. J. Pediatr. 2014, 165, 395–397. [Google Scholar] [CrossRef] [PubMed]
- Kelly, K.L.; Johnson, C.P.; Dunne, L.E.; Holschuh, B.; Joyner, M.; Johnson, B.D. Active compression garment prevents tilt-induced orthostatic tachycardia in humans. Physiol. Rep. 2019, 7, e14050. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bourne, K.M.; Sheldon, R.S.; Hall, J.; Lloyd, M.; Kogut, K.; Sheikh, N.; Jorge, J.; Ng, J.; Exner, D.V.; Tyberg, J.V.; et al. Compression Garment Reduces Orthostatic Tachycardia and Symptoms in Patients with Postural Orthostatic Tachycardia Syndrome. J. Am. Coll. Cardiol. 2021, 77, 285–296. [Google Scholar] [CrossRef] [PubMed]
- Benditt, D.G.; Sutton, R. Improved Acute Orthostatic Tolerance in POTS by Lower Body Compression: Both Beneficial and Sufficient? J. Am. Coll. Cardiol. 2021, 77, 297–299. [Google Scholar] [CrossRef]
- SANTOS, R.Q.D.; Smidt, L.; Suzigan, B.H.; De Souza, L.V.; Barbisan, J.N. Efficacy of lower limb compression in the management of vasovagal syncope-randomized, crossover study. Pacing Clin. Electrophysiol. 2013, 36, 451–455. [Google Scholar] [CrossRef]
- Platts, S.H.; Tuxhorn, J.A.; Ribeiro, L.C.; Stenger, M.B.; Lee, S.; Meck, J.V. Compression garments as countermeasures to orthostatic intolerance. Aviat. Space Environ. Med. 2009, 80, 437–442. [Google Scholar] [CrossRef]
- Stenger, M.B.; Brown, A.K.; Lee, S.M.C.; Locke, J.P.; Platts, S.H. Gradient compression garments as a countermeasure to post-spaceflight orthostatic intolerance. Aviat. Space Environ. Med. 2010, 81, 883–887. [Google Scholar] [CrossRef]
- Kamiya, A.; Michikami, D.; Fu, Q.; Iwase, S.; Hayano, J.; Kawada, T.; Mano, T.; Sunagawa, K. Pathophysiology of orthostatic hypotension after bed rest: Paradoxical sympathetic withdrawal. Am. J. Physiol. Circ. Physiol. 2003, 285, H1158–H1167. [Google Scholar] [CrossRef] [Green Version]
- Dani, M.; Dirksen, A.; Taraborrelli, P.; Torocastro, M.; Panagopoulos, D.; Sutton, R.; Lim, P.B. Autonomic dysfunction in ‘long COVID’: Rationale, physiology and management strategies. Clin. Med. 2021, 21, e63–e67. [Google Scholar] [CrossRef]
- Petracek, L.S.; Suskauer, S.J.; Vickers, R.F.; Patel, N.R.; Violand, R.L.; Swope, R.L.; Rowe, P.C. Adolescent and Young Adult ME/CFS After Confirmed or Probable COVID-19. Front. Med. 2021, 8, 668944. [Google Scholar] [CrossRef]
- Skarin, M.U.; Rice, D.A.; McNair, P.J.; Kluger, M.T. Orthostatic intolerance following hip arthroplasty: Incidence, risk factors and effect on length of stay: A prospective cohort study. Eur. J. Anaesthesiol. 2019, 36, 123–129. [Google Scholar] [CrossRef]
- Bundgaard-Nielsen, M.; Jørgensen, C.; Jørgensen, T.; Ruhnau, B.; Secher, N.; Kehlet, H. Orthostatic intolerance and the cardiovascular response to early postoperative mobilization. Br. J. Anaesth. 2009, 102, 756–762. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tanaka, K.; Tokumiya, S.; Ishihara, Y.; Kohira, Y.; Katafuchi, T. Compression Stocking Length Effects on Arterial Blood Pressure and Heart Rate Following Head-Up Tilt in Healthy Volunteers. Nurs. Res. 2014, 63, 435–438. [Google Scholar] [CrossRef]
- Podoleanu, C.; Maggi, R.; Brignole, M.; Croci, F.; Incze, A.; Solano, A.; Puggioni, E.; Carasca, E. Lower Limb and Abdominal Compression Bandages Prevent Progressive Orthostatic Hypotension in Elderly Persons: A Randomized Single-Blind Controlled Study. J. Am. Coll. Cardiol. 2006, 48, 1425–1432. [Google Scholar] [CrossRef] [Green Version]
- Novak, P. Orthostatic Cerebral Hypoperfusion Syndrome. Front. Aging Neurosci. 2016, 8, 22. [Google Scholar] [CrossRef] [Green Version]
- Toska, K.; Walloe, L. Dynamic time course of hemodynamic responses after passive head-up tilt and tilt back to supine position. J. Appl. Physiol. 2002, 92, 1671–1676. [Google Scholar] [CrossRef] [Green Version]
- Alskaf, E.; Kardos, A. The mystery of defining aortic valve area: What have we learnt from three-dimensional imaging modalities? J. Echocardiogr. 2018, 16, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Castle-Kirszbaum, M.; Parkin, W.G.; Goldschlager, T.; Lewis, P.M. Cardiac Output and Cerebral Blood Flow: A Systematic Review of Cardio-Cerebral Coupling. J. Neurosurg. Anesthesiol. 2021. [Google Scholar] [CrossRef]
- Hoiland, R.L.; Fisher, J.A.; Ainslie, P.N. Regulation of the Cerebral Circulation by Arterial Carbon Dioxide. Compr. Physiol. 2019, 9, 1101–1154. [Google Scholar] [CrossRef] [PubMed]
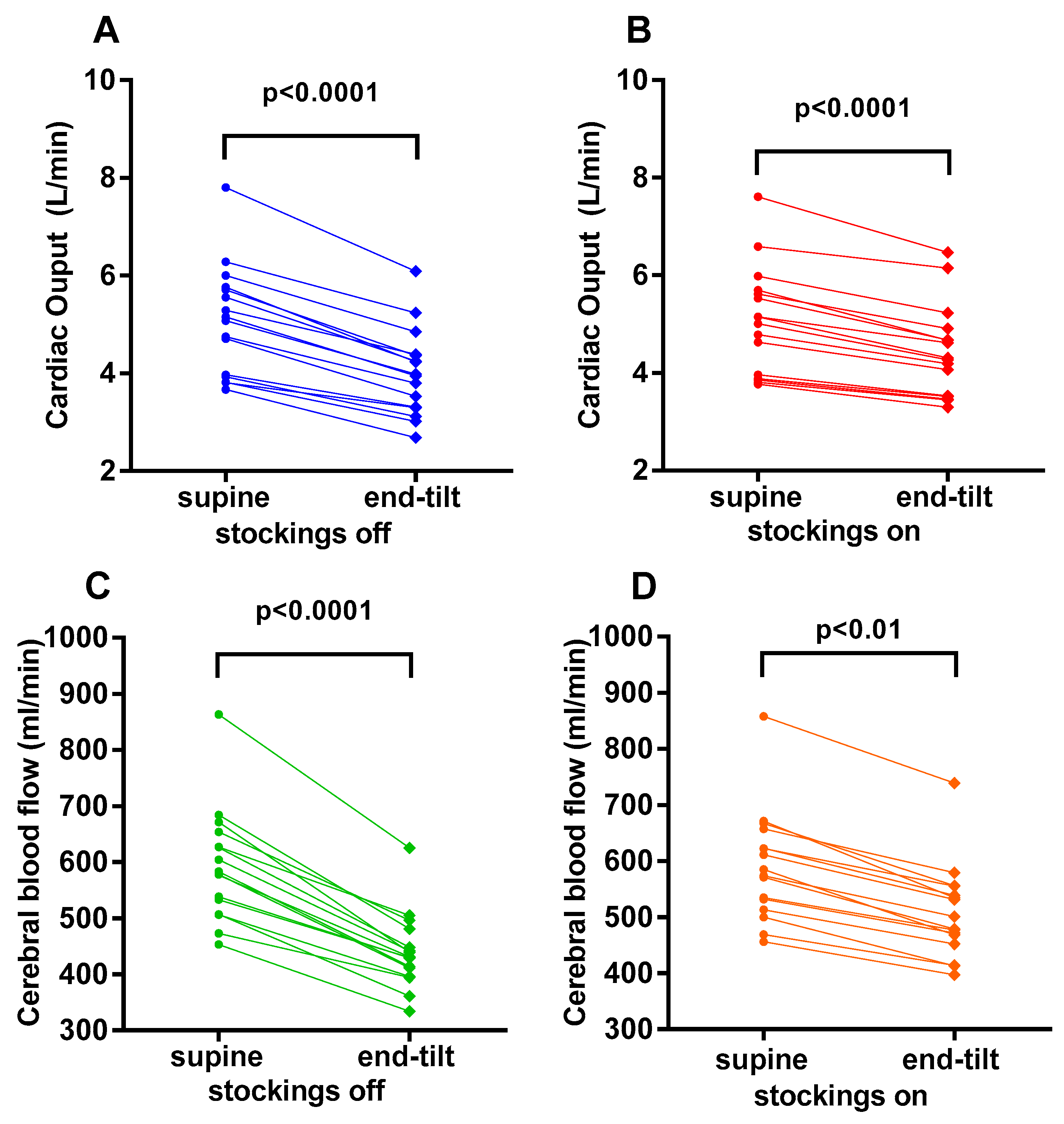


| Compression Stockings OFF (n = 16) | Compression Stockings ON (n = 16) | p-Value | |
|---|---|---|---|
| Heart rate supine (bpm) | 71 (10) | 71 (10) | ns |
| Heart rate upright (bpm) | 83 (13) | 85 (12) | ns |
| SBP supine (mmHg) | 131 (21) | 129 (16) | ns |
| SBP upright (mmHg) | 133 (22) | 131 (21) | ns |
| DBP supine (mmHg) | 77 (10) | 76 (8) | ns |
| DBP upright (mmHg) | 84 (11) | 83 (11) | ns |
| CO supine (L/min) | 5.08 (1.12) | 5.06 (1.10) | ns |
| CO upright (L/min) | 4.01 (0.89) | 4.43 (0.94) | <0.0001 |
| CBF supine (mL) | 580 (513–647) | 580 (518–649) | ns |
| CBF upright (mL) | 431 (400–473) | 490 (456–551) | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van Campen, C.M.C.; Rowe, P.C.; Visser, F.C. Compression Stockings Improve Cardiac Output and Cerebral Blood Flow during Tilt Testing in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) Patients: A Randomized Crossover Trial. Medicina 2022, 58, 51. https://doi.org/10.3390/medicina58010051
van Campen CMC, Rowe PC, Visser FC. Compression Stockings Improve Cardiac Output and Cerebral Blood Flow during Tilt Testing in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) Patients: A Randomized Crossover Trial. Medicina. 2022; 58(1):51. https://doi.org/10.3390/medicina58010051
Chicago/Turabian Stylevan Campen, C. (Linda) M. C., Peter C. Rowe, and Frans C. Visser. 2022. "Compression Stockings Improve Cardiac Output and Cerebral Blood Flow during Tilt Testing in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) Patients: A Randomized Crossover Trial" Medicina 58, no. 1: 51. https://doi.org/10.3390/medicina58010051
APA Stylevan Campen, C. M. C., Rowe, P. C., & Visser, F. C. (2022). Compression Stockings Improve Cardiac Output and Cerebral Blood Flow during Tilt Testing in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) Patients: A Randomized Crossover Trial. Medicina, 58(1), 51. https://doi.org/10.3390/medicina58010051






